Article contents
Facteurs prédisposants à la survenue d'une pathologie dépressive au cours du post-partum
Published online by Cambridge University Press: 28 April 2020
Résumé
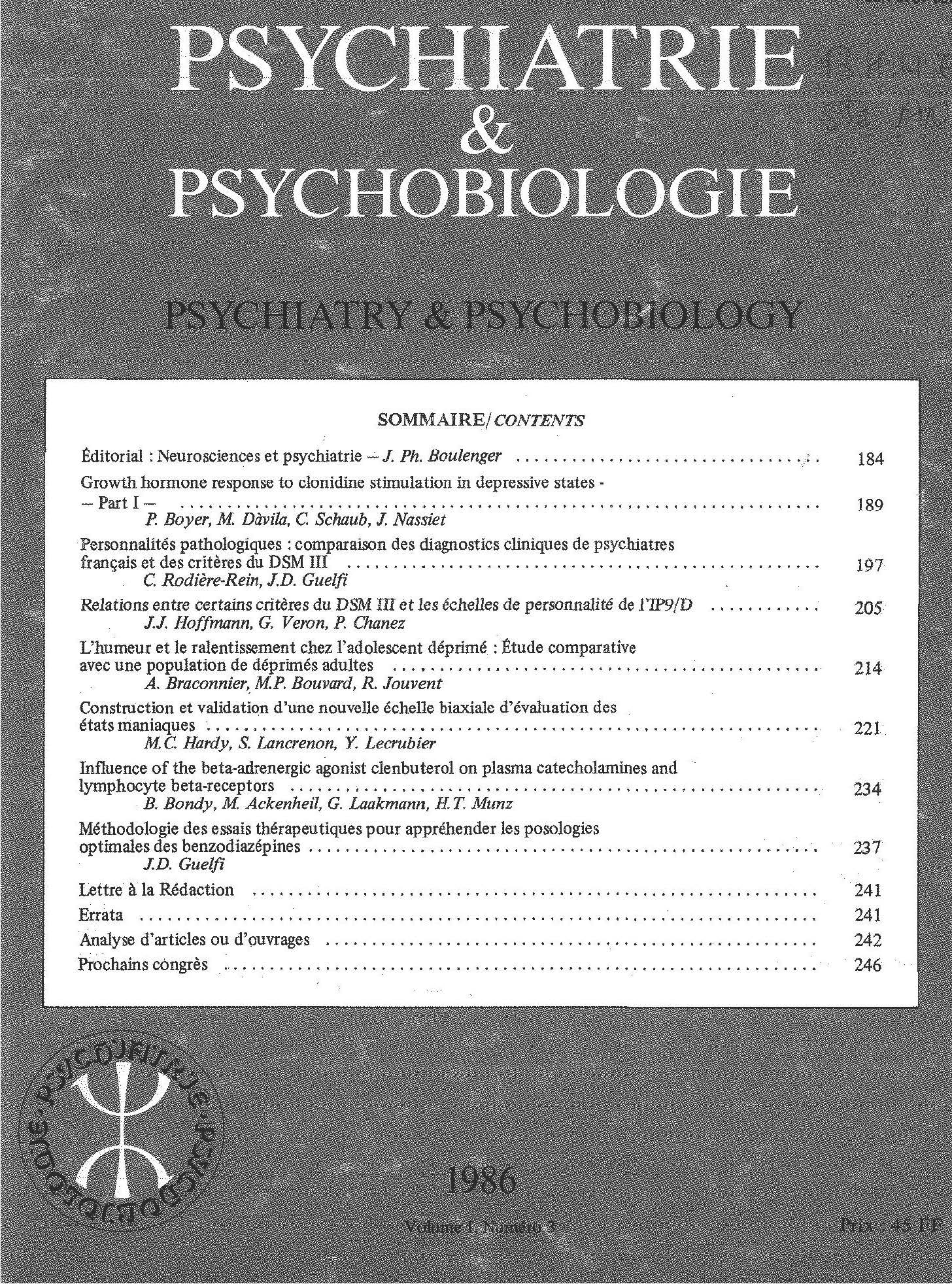
Cet article présente brièvement les résultats d’une étude épidémiologique unicentrique standardisée avec seulement deux cotateurs entraînés, de l’incidence et des facteurs de morbidité des épisodes dépressifs non psychotiques de la puerpéralité à partir de 483 dossiers standardisés de jeunes accouchées constituant un échantillon au tiers parmi les 1232 accouchements survenus durant une année à la maternité du CHRU de Saint-Etienne. Ce travail a permis de diagnostiquer au moyen d’évaluations psychométriques quantifiées 35 cas de “post partum blues” (incidence 6.6 %). Le dépouillement des réponses aux 35 items (Tableau 1) a permis d’isoler par segmentation non arborescente (figure 1) deux groupes: un de femmes non-à-risque et un de femmes à haut risque de pathologie dépressive post puerpérale défini par la présence de quatre facteurs prédisposants: la présence d’antécédants psychopathologiques personnels dépressifs, la survenue de manifestations anxiodépressives et de traumatismes psychologiques durant la grossesse, la séparation précoce d’avec l’enfant après l’accouchement. Quant aux “post partum blues”, seule la primiparité apparaît avec une plus grande fréquence. Néanmoins leur faible incidence dans notre échantillon peut conduire à s’interroger sur la définition des critères de morbidité de cette pathologie.
Summary
This paper presents the results of an investigation into incidence and morbidity factors as regards non-psychotic depressive conditions during puerperium, and post-partum blues.
The investigation was conducted in a group of 483 females chosen at random from the 1232 maternity patients admitted to the Saint Etienne CHRU (University Regional Hospital Center) between June 1 1985 and May 31 1986. Post-partum blues was diagnosed as the presence of depression, in keeping with Feighner's criteria, for a period occurring between day 5 and day 15 and lasting less than 8 days. Persistence for these symptoms after day 15 was diagnosed as depression.
On days 5, 15 and 28 post partum, two trained raters carried out standard interviews and filled in Montgomery and Asberg's depression scale (M.A.D.R.S.), Widlôcher's depressive psychomotor retardation scle (E.R.D.), Covi's anxiety scale and a list of 35 items considered as being possibly pathogenic (see table 1). One of the following tests was chosen for statistical analysis for each case: analysis of variance, Student's t-test, X2 test, or the Kruskall and Wallis test. The non-arborescent segmentation method of analysis (SIPINA), developed by the Lyon Statistics Center, was used to classify patients as “normal” (group 1), “with post-partum blues” (group 2) or “depressed” (group 3). Average age was 28 ± 4 years. Items 1, 2, 3, 4, 5, 6, 9, 15, 21, 23, 26, 27 and 30 showed no difference for the three groups (table 1). Items 19, 20, 22, 32, 33, 34 and 35 (table 1) could not be rated because of the excessively low incidence of pathological response in groups 1 and 2. The incidence of post-partum depression (DPP) and post-partum blues (PPB) was respectively 6.6% and 7.2% (32 and 35 cases). The DPP group differed from the other two groups in terms of items 8, 10, 11, 17, 18, 24 and 26 (table 1); the PPB subjects differed from the two other groups only in terms of the incidence of primiparity (item 7). The normal, non arborescent segmentation method showed 27 of the 32 cases of depression to involve females who were separated from their babies early, and/or underwent traumatic experiences during pregnancy, and/or presented a previous history of psychopathological disorders. The other five cases of depression were observed in groups of females devoid of any of these factors.
Our study confirms the predisposing characteristics identified in the existing literature, and the relatively insignificant connection between depressive states and events occurring during pregnancy, with the exception of real or imagined losses. The limited incidence of DPP in our test group may constitute a specific phenomenon for this group or be related to our diagnostic criteria, despite their being clearly defined. The absence of response to items 15, 16, 32, 33, 34 and 35 is also found in the literature, in research carried out on difficult early mother-child relationships. We are not sure whether this factor is the result of random selection of our patients, whether these items “disappear” once the child is born but reappear subsequently, or whether they in fact develop at a later stage.
Finally, the DPP-related risk factors we have demonstrated indicate a more general psychobiological fragility.
Keywords
- Type
- Research Article
- Information
- Copyright
- Copyright © European Psychiatric Association 1987
References
- 1
- Cited by


Comments
No Comments have been published for this article.