Context
Traditionally, health-care philanthropy has focused on giving to individual patients, hospitals, and volunteering opportunities. This chapter aims to demonstrate how strategic philanthropy in health care can play an important role in purposefully driving giving to improve health outcomes.
The Constitution of India obliges the government to ensure the ‘right to health’ for all and requires each state to provide free universal access to health-care services. Unfortunately, the health sector in India has been highly fragmented, not just in terms of financing and provision of health care, but also in terms of the continuum of care and quality standards. While government hospitals offer free health services, these facilities tend to be inadequately equipped, understaffed, and based predominantly in urban areas. Many medical services are, therefore, provided by private institutions and 65 per cent of medical expenditures in India are paid out of pocket by patients.Footnote 1
This chapter outlines how Cipla’s (India’s third-largest pharmaceutical company) philanthropy and corporate social responsibility (CSR) arms have, since the late 1990s, in tandem, been supporting the development of palliative care in India. In a fragmented health system, palliative care can potentially serve as the glue anchoring the patient at the centre of care by recognising that the challenges faced by a person with a serious illness are not just confined to the disease alone. Palliative care acknowledges that illness may cause pain and other symptoms related to the physical, social, and spiritual needs of both the patients and their families and that these should be holistically addressed. The palliative care team thus coordinates the care plan for each patient, seeking to connect a multidisciplinary team to provide all-round care to patients. Unfortunately, palliative care – though essential for quality patient care – is not a revenue source for the health-care industry and hence has been systematically neglected.
In 1997, Cipla’s promoter family decided to invest their philanthropic efforts in setting up a palliative centre in Pune, despite being aware that they were not experts on this type of treatment. However, they believed that palliative care is essential to improving the quality of life of patients, and stepped forward to bridge this gap in the Indian health-care space. The single-minded clarity and focus of the family’s vision – making palliative care accessible to all – has guided them develop a strategic model and has driven their philanthropic journey thus far.
Cipla’s unique approach initially focused on providing direct patient support through palliative care in one Indian city, which then grew into a wider philanthropic strategy when the company mandated Cipla Foundation, its CSR arm to expand palliative care programmes across the country. Thus, the strategy for creating a palliative care ecosystem was informed by the practice and challenges of delivering care at the Cipla Palliative Care and Training Centre (CPC) in Pune. Simultaneously, through the expansion process came learnings from partners across the country, which informed the services at the palliative care centres and ensured they were strengthened over time. Wearing multiple hats as a funder, funder and implementer, has broadened Cipla’s philanthropic scope and perspective of palliative care.
This chapter highlights how palliative care emerged as part of the philanthropy agenda, and how philanthropy was directed to set up a ‘proof of concept’ and lay the foundation to before being used strategically create access to care across the country. In doing so, the chapter also outlines the lessons the team learned and how it responded to challenges along the journey.
It is important to share this story as the Cipla team believes that philanthropy, when used strategically, can play an important role in creating a ripple effect, especially for issues such as palliative care that are neglected by market forces.
Cipla’s Philanthropy and Palliative Care: The Roots
Palliative care is a niche area in India – one that has found little support on the list of health causes popular with philanthropic funders despite being a gaping unmet need. Only 4 per cent of patients in India with a serious illness receive access to pain relief – the majority live and eventually die in discomfort with their caregivers suffering alongside them.Footnote 2 As people live longer with serious and complex illnesses owing to general advancements in medical care, the gap in access to palliative care is only widening in India’s fractured and under-resourced health-care system.
In 1997, it was commonly perceived that palliative care equalled hospice care; hence, palliative care was likened to end-of-life care. Therefore, the few available services in the late 1990s only offered this care to patients when curative treatment had ended.
Given that palliative was not clearly understood, from the start Cipla’s CPC focused on the importance of using the term palliative care to emphasise addressing ‘total patient pain’ – whether physical, social, emotional, or spiritual. The vision also held that in order for palliative care to make a real difference to patients and families, it needed to be introduced close to the time of diagnosis. This would allow for the Cipla team to integrate with the physician to provide a holistic care plan supporting both patients and their caregivers.
The impetus to provide palliative care services in India first came to Cipla in the early 1990s when Dr Lucito D’Souza, a leading cancer surgeon and the founder of Mumbai’s first hospice Shanti Avedna Sadan, spoke to Cipla’s promoter family about manufacturing morphine sulphate tablets for terminal patients admitted to his facility. Cipla not only supplied the morphine tablets, but the family also visited the hospice in Mumbai to understand pain management for patients with serious illnesses. Upon further study, the family found an abysmal lack of professional palliative care services in India and felt that in such a scenario, simply manufacturing medicines to alleviate the suffering of patients would not be enough.
The second turning point came when the family attended a programme organised by Macmillan Cancer Support, a London-based charity. Macmillan had launched a project to train Indian doctors and nurses in specialist palliative care. The family realised the need for bringing such care to patients in India and the seed for Cipla’s Palliative Care Centre was sown. In 1993, when palliative care was still relatively unknown in India, the family acquired a five-acre plot in a quiet suburb of Pune. To translate the vision into action in 1997, the Macmillan nurses in Britain were invited to Pune to demonstrate what a world-class palliative centre should look like and how it should function. This vision has continued to guide the work of Cipla palliative care since the late 1990s, allowing its services to reach over 22,500 patients and caregivers.
Using Philanthropy to Establish a Proof of Concept
From the outset, it was clear that the Cipla Centre (CPC) would not be a hospital, neither would it be a hospice for end-of-life patients. It was envisaged that Cipla’s CPC would care for a person with cancer at any stage of the illness. A dedicated team of doctors, nursing staff, social workers, specialists, and volunteers would work together to provide the highest level of care to patients and their loved ones, completely free of cost.
After four years of planning and designing the service, on 1 May 1997, CPC welcomed its first patient, and over 20,000 patients and their families have been served ever since. Since 1997, several additions have been made to CPC’s services driven by the goal of making quality palliative care accessible to patients and families.
The fifty-bed centre is designed to provide personalised care and exudes an atmosphere of peace and serenity. It is built around the concept of an aangan, an open courtyard, to foster a sense of community. The wards are named after flowers and patients are known by their names, not their bed numbers. Furthermore, the thoughtful architectural design of CPC allows even those patients who are confined to their beds who cannot even sit in wheel chairs, to be wheeled outside, on their beds, to enjoy the beautiful surroundings.
The service deeply embeds itself in the Indian ethos of family and community, where patients and caregivers are equally cared for at the Centre, at their home, or in an outpatient department. This model aims to equip family members by giving them the confidence and skills needed to care for their loved ones. Family members also receive ongoing emotional and psychological support, including much-needed grief and bereavement counselling. Box 1 illustrates an example of the difference palliative care can make to both the patient and their family.
Over the course of this process, the Centre’s team has learned that to make philanthropy more strategic, they must listen and respond to the voices of all stakeholders to work towards providing quality care.
From patients and caregivers the team learned that they required services suited to their unique needs and phase of illness. From 2004, CPC therefore started home care teams to visit patients and provide services of equal quality in their homes. In 2007, the Centre began outpatient clinics so that palliative care support could be closer to patients when they met their treating physicians and continued to expand home care and outpatient clinics over the subsequent years. In 2020, as COVID-19 struck, CPC responded to patients by strengthening its telephonic and video consultations so that patients could continue to receive care. It also began a patient support programme to provide financial assistance to those seeking treatment.
In services like palliative care, Cipla has learned that the teams delivering the care are agents of change and their insights from practice become instrumental in developing a particular service. Through documenting CPC’s interventions on a hospital management system, Cipla has used data and reflections from the team to make changes including: improving patient care through sharper assessment tools, embedding feedback mechanisms to better understand expectations from patients and caregivers, and strengthening our services by understanding the referral sources of patients and strategies to expand referrals from health-care professionals to palliative care.
Doctors helped Cipla understand the gap in communication between physicians and palliative care professionals, along with missed opportunities for information-sharing about pain-relief protocols. CPC responded by finding avenues for enhanced collaboration between these groups through exchange visits, workshops, and training sessions.
Case Study: Early Integration
First Meeting with Pushpa
The team first met Pushpa and her daughter-in-law when they were referred to the CPC by a relative in February 2013. They had been told that CPC doctors are ‘different from other hospitals’ and ‘you don’t have be afraid to talk to them’. Pushpa had had a biopsy done three days earlier at a government hospital but was too afraid to collect her reports; she wanted to know if the CPC team could ease her pain. The social worker and the palliative care physician talked with Pushpa to find out more about her journey so far, her fears and expectations. Pushpa and her daughter-in-law also had the opportunity to tour the Centre. At the end of the visit, she agreed to collect the biopsy report but was still unsure of the benefits from any medical interventions. She agreed to have the palliative care team visit her at home to discuss further. After her visit to CPC, she collected the reports that confirmed her cancer diagnosis. Pushpa felt shame, anger, and guilt as a result of this diagnosis and resolved not to undergo any curative treatment.
Supporting Pushpa in Seeking Curative Treatment
Two days after her first visit to the Centre, the CPC home care team paid Pushpa a visit, went through her reports that she had just collected, and talked to her about the symptoms she was experiencing. They gave her information about the biopsy procedure, what the results indicated, and how they could be addressed. The CPC team also provided her with a prescription for present symptoms, including hypertension and breathlessness. At the time, Pushpa was not ready for further curative treatment. The home care team told her they would come back in two days to check on her symptoms. When the team visited again, the patient reported that she had some symptomatic relief and again spoke about her fear of cancer and the stigma around being a cancer patient. The home care social workers spoke to her about these fears, discussed her strengths and her methods for coping in the past, and the support that could be available through the CPC. After two more counselling sessions, Pushpa said she was ready to go ahead with curative treatment. The team explained the surgery and what to expect in the aftermath, and identified a local general practitioner whom the team could also contact if necessary.
Managing the Effects of Surgery
Pushpa underwent surgery in April 2013 and after discharge she agreed to be admitted at CPC for post-surgery and wound management. Looking back on her two-week stay at CPC, Pushpa describes this experience as one of the most life-changing and peaceful times in her life, where she learnt about caring for herself. The clinical team of doctors, nurses, physiotherapists, and social workers helped prepare and implement a care plan for Pushpa till after her wounds had healed well, she was no longer in pain and felt ready to go back home. She said she was more confident now to face her life ahead and more positive about facing any problems. The home care team assured her that she could call at any time and also briefed the local GP on Pushpa’s condition.
Establishing a Home Care Routine
The CPC home care team visited Pushpa two days after she left the Centre and advised her to see her oncologist as well for a check-up. They also went through her medications, diet, and exercise routine. At this visit, she explained her worries about the ill health of her youngest son, who was seeking treatment but did not seem to be getting better. Before the next visit scheduled for the following week, Pushpa called the home care team with news that her son had passed away – she was feeling guilty that due to her illness, she had neglected her son’s health. The home care team spent time with Pushpa to listen to her worries and reminded her of all the support she had provided as a mother. The team continued to support Pushpa in addressing her guilt, and after a month she said she had now accepted the situation. The home care team began visiting once a month from that point forward.
Continuing Care for Pushpa
The home care journey continued for Pushpa over the next several years. In September 2015, Pushpa mentioned on a call that she felt some pain in her left hand. The team asked her to come to the Centre and realised that she was developing mild lymphedema; she visited CPC regularly for physiotherapy and in two weeks was completely cured. The routine home visits and telephone calls continued – the home care team continues to be part of Pushpa’s life and joins in during family wedding and birthday celebrations, as well as difficult times for the family.
Pushpa’s case exemplifies a successful story of early support where the CPC team built trust and rapport with a patient, allowing for the establishment of a longer-term palliative care arrangement. There are many more patients like Pushpa who require support and CPC hopes to reach as many of them as possible in the years ahead.
Why Palliative Care Continues to be Nurtured and Strengthened
In 2016, when Cipla Foundation – the CSR arm of Cipla – began to engage strategically in palliative care, there was a strong conviction that palliative care had the power to transform the health-care system. This conviction stemmed from the positive health outcomes the Pune Centre achieved despite facing challenges. In striving to overcome difficulties at CPC, the below critical concerns emerged:
Need for greater awareness, understanding and acceptance about the benefits of palliative care: Many misconceptions remain among health-care providers and patients about the concept of palliative care as being ‘end-of-life’ care rather than ‘complementary’ care that should run alongside curative treatment protocols. Doctors and patient family members, who may be focused on curing an illness until the very end, misunderstand palliative care as a failure to adequately treat and help patients.Footnote 3 In addition, the use of opioids for pain relief, which are used in palliative care, are shrouded in misapprehensions as addictive drugs that can result in legal risks and misuse. This results in a double-edged challenge for health-care providers, who may not refer patients to palliative care facilities, and for patients, who may not demand palliative care in time.
Increasing access to holistic healing and total pain management: The CPC team observed that health-care providers focus primarily on physical pain relief. As a result, the vast majority of patients live a poor quality of life, especially just before death. Additionally, there is a lack of awareness about the use of opioids in pain relief.Footnote 4
Improving communication between health-care providers, patients, and families: In an overburdened health-care system patients with serious illnesses and their families often feel rushed, with inadequate support and information about their disease prognosis and care plans. This is further exacerbated by the lack of communication within the family due to the stigma of certain health conditions as well as fear of discussing the impact of the condition on the patient.
Enhancing palliative care skills amongst health-care providers: The Centre’s team realised that there is an acute shortage of trained palliative care professionals, including physicians, nurses, and social workers. They also learned about the lack of evidence-based palliative care training opportunities available for health-care providers to deepen their skills. The team’s on-ground experience of the difficulty in getting trained palliative care professionals for the Centre fuelled Cipla’s belief that training was an essential component of the strategy to scale up palliative care work in India.
Focusing on the needs of caregivers: Family members who visited the Centre in Pune told the team how their own physical, financial, emotional, and spiritual needs had been neglected, and described the support they required to cope with the relentless demands of caregiving. A key guiding principle in Cipla’s work therefore became ensuring that the patient’s family also receives ongoing emotional and psychosocial support, including much-needed bereavement counselling. Throughout the patient’s journey, the palliative care team assesses the needs of both the patient and the caregivers and has a care plan for both. This aspect of palliative care ensures that the focus remains on holistically observing how the illness impacts both the patient and caregiver.
Ensuring a continuum of care: The CPC team members learned that successful palliative care ensures that no patient with a serious illness suffers because of pain, whether in hospital or at home. In addition to inpatient care, they realised the immense scope and value of providing patients with the choice of providing quality services at outpatient clinics or at their homes. Patients and families told the Centre’s team that they often spend longer periods of time than needed at hospitals for fear of losing access to quality care back home. Cipla’s goal was therefore to achieve the same standard through home care services.
These key insights not only guided the philanthropic strategy in running the Palliative Care Centre in Pune, but further informed Cipla’s vision to strengthen palliative care access across the country. The aim of this type of strategic philanthropy centres on building an ecosystem where all health-care providers embody the essence of palliative care and adopt its responsive approach to meet patient needs, delivering care based on patient preferences.
Using Philanthropy Strategically to Create Access to Care
To take forward Cipla’s palliative care vision, Cipla Foundation’s (CF) strategy is to invest in direct services that will create greater health-care access for Indians. The Foundation supports this aim by partnering with organisations interested in developing palliative care services in their locations or with those seeking to consolidate and expand their existing palliative care work.
By October 2023, CF was supporting thirty partner organisations across twenty-four Indian cities, as illustrated in Figure 8.1. The Foundation’s budgets over the past five years have also grown to reflect the commitment to palliative care, from 12 crore rupees (£1,255,000) in 2019–1920 to 16 crore rupees (£1,675,000) in 2021–2022.Footnote 5 From April 2021 to March 2022 alone, Cipla CPC and its partners offered palliative care services to over 10,000 patients.Footnote 6
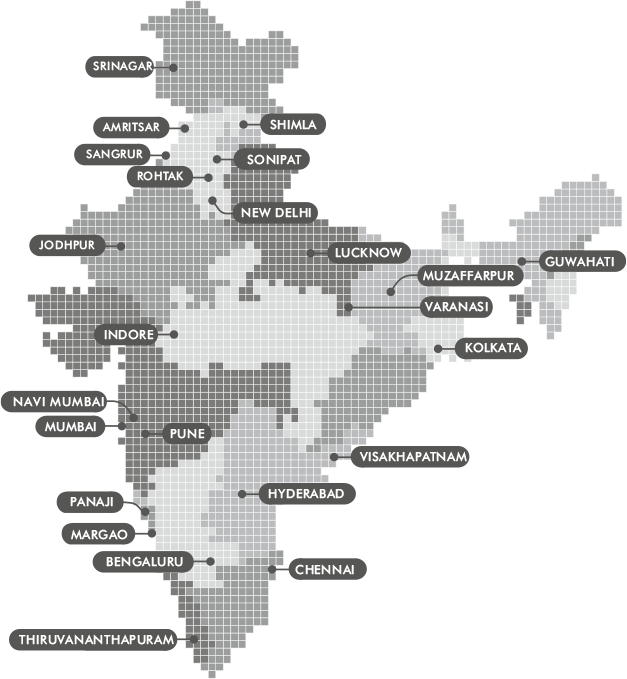
Figure 8.1 Palliative care services supported by the Cipla Foundation
The strategy of CF, whilst creating access, has been to partner with like-minded organisations already working in this space and find champions willing to take on palliative care in their geographies. Further focus on training and building a cadre of health-care professionals with a palliative care approach has supported strong collaborations at a national level to take forward changes in policy and resource allocation to palliative care.
Identifying and Supporting Champions
A key process for the Foundation has been identifying champions for palliative care and supporting them in strengthening services. In doing so, CF has focused on a variety of service models in palliative care, examined how palliative care can move beyond oncology, and demonstrated that partnerships with the government are important to scaling up the work and making it accessible.
Strengthening existing palliative care providers: Initially, the Foundation began partnerships with partners that enabled cross-sharing of work between teams. CF recognised innovative work being implemented by other organisations and supported these partners to strengthen their service delivery. For example, many partners have existing inpatient facilities but lacked home care services. The Foundation’s support enabled them to provide a continuum of care to patients ensuring that health facilities are accessible to the most vulnerable.
Setting up palliative care in new geographies: The Foundation also identified champions in locations that had no palliative care services available and supported their development of integrated outpatient clinics offering palliative care services, with the aim of having a more equitable distribution across the country.
Developing palliative care services beyond oncology: The Foundation supported the establishment of a novel inclusive inpatient palliative care facility in Mumbai. It has also partnered with India’s premier institute for neurology to set up an outpatient clinic for patients with neurological conditions in Bengaluru.
Demonstrating that palliative care is for children and adults of all ages: CF has partnered with champions in charitable and state hospitals to set up paediatric palliative care units, supporting six of these centres across the country to date.
Piloting community projects along with the state governments: To work towards integrating palliative care within the public health-care system, the Foundation has been supporting a project with the state government. Through this community-based project, it trains government health workers to use a checklist of symptoms to identify patients requiring palliative care and refer them accordingly. Additionally, CF trains doctors, nurses, and multipurpose workers to provide palliative care at primary health-care centres, subcentres, and rural hospitals. The project has now been scaled up to an entire district with the hope that this pilot will encourage an uptake at the state level.
Cascading Palliative Care through Trained Professionals
The need for training has been a consistent theme that emerged from Cipla’s experience at the Centre and through its partnerships. At the Foundation, the strategy uses an evidence-based curriculum, focuses on partnering with premier training institutes in the country, identifies key audiences for training, ensures the follow up of training activities, and allows for practical hands-on training.
The Foundation has forged partnerships with End-of-Life Nursing Education Curriculum (ELNEC) USA and Education in Palliative and End-of-Life Care (EPEC) USA to design training modules along with palliative care professionals in India to adapt this to local needs. CF’s support has enabled this face-to-face collaboration, ensuring that jointly the organisations developed and piloted modules to deepen knowledge and skills on palliative care. By supporting the ELNEC and EPEC programmes, Cipla trained 2,600+ nurses including 35 trainers, and over 120 physicians. Such training also includes a training-of-trainers component with a professional development workshop to create a cadre of lead trainers who cascade the training across the country.
CF has, further, trained professionals across the country by partnering with institutions that have a national presence in the Indian public health-care system, including the All India Institute of Medical Sciences (AIIMS), New Delhi, and the Tata Memorial Hospital. A key aspect of all these training programmes centres on providing a mentorship programme for participants that extends beyond the core training.
Based on the existing services supported by the Foundation, oncologists and paediatricians were identified as key professionals to train in palliative care. It has therefore partnered with the SAARC Federation of Oncologists (SFO) as well as the Indian Academy of Paediatricians (IAP) to train their members. To date the Foundation has trained 450 oncologists and over 100 paediatricians in palliative care.
As palliative care becomes integrated into the health-care curriculum of doctors and nurses, the need to design a training programme for faculty in teaching hospitals has emerged. The Foundation will continue to intensify its efforts to support such programmes.
National Collaborations for Policy Change
Whilst the Foundation’s team does not directly lobby state and national governments, it supports and collaborates with its partners to advocate for better access to pain relief, training of doctors and nurses, and greater allocation of government resources for palliative care. CF supports training programmes and best-practice exchange, in addition to bringing members together on national, regional, and theme-based platforms to promote palliative care. It also supports partners in pressing the government for better allocation of resources to palliative care and adding this important service area to the agenda for the broader national health-care system.
The Foundation has thus been striving to work alongside its partners to create access to palliative care by generating a ripple effect through its support in direct services, training, and collaborations, so that access becomes a basic right for patients and caregivers.
Using Philanthropy as a Catalyst for Sustainable Change
When analysing the role of Cipla’s philanthropy and CSR in supporting sustainable change in palliative care, key themes that emerge are:
Integrated models of care in the public health system: Cipla Foundation’s work has focused on strengthening services in outpatient clinics in key government and charitable hospitals. Its support enables the overstretched public health-care system to recruit for an embedded palliative care team. This multidisciplinary team then works in close collaboration with the treating physician to coordinate care for the patient, and to answer questions from the patient and caregiver about their concerns, treatment options, and how the treatment is impacting them, thus reducing time required by the treating physician. This integrated clinic model further enables palliative care to be offered earlier on to patients and caregivers, given its availability within the hospital itself. Through these programmes, the CF demonstrates the value of housing a specialised team within a larger institution to deliver care, train other professionals, facilitate interdisciplinary working, and achieve better health outcomes. Once the value proposition of these interventions is felt within the hospital, it becomes easier to discuss further funding or co-funding partnerships with the hospital leadership team.
Bringing partners together to increase reach and impact: The Foundation upholds the belief that changing the health-care ecosystem requires a truly collaborative movement to embed and integrate palliative care. CF has taken every opportunity to join forces with committed, passionate individuals and organisations working in the palliative care space, strengthening its resolve to bring partners together, share knowledge and skills, and leverage best practices. The Foundation even attempted this during COVID-19 through the establishment of a national palliative care helpline – Saath Saath.
During the height of COVID-19, several palliative care services, and especially home care services, were interrupted. The extremely vulnerable subset of palliative care patients experienced difficulty accessing medical care in the event of increased symptom burden, obstacles in reaching hospitals during emergencies or at end of life, limited access to medication, and isolation due to social distancing regulations, all of which led to psychosocial impacts and a lack of bereavement support. The Foundation consulted with partners and experts internationally to draw up standard operating procedures that guided the care at Cipla’s Centre as well as at its partner organizations. This enabled palliative care to safely continue for both staff and patients. CF also facilitated regular discussions amongst partners to share experiences and learn how best to support patients especially through telemedicine services.
The value of reaching out to patients and caregivers through technology became apparent during COVID-19 and initiated the development of a national palliative care helpline.
The Foundation played a leading role in bringing together its partners to develop the helpline Saath Saath, a toll-free number for patients, caregivers, and professionals that launched in October 2021. This is the first national palliative care helpline in India, linking callers to their nearest palliative care service. Calls in the first 2 years (over 4,500 calls) demonstrate the value of having a single point of contact for patients, and further highlight the gaps in service provision which need to be addressed.
Aligning with government priorities: State governments have been developing their non-communicable disease (NCD) programmes in recent years, offering crucial opportunities to integrate palliative care. Cipla Foundation learned about this opportunity through supporting a community-based project with the National Health Mission. The community-based project supported by CF strategically aligned with the NCD so that prevention, promotion, palliation, treatment, and rehabilitation are all integrated into the care programme. This enabled the training of health-care workers and identifying patients with serious illnesses early in their disease trajectory. As a Foundation, Cipla will continuously review the latest government priorities and find relevant partners in order to dovetail palliative care within such programmes.
Attracting more philanthropists to the palliative care space: To broaden funding to palliative care services, Cipla has been engaging with funding agencies and philanthropists to deepen their support towards palliative care services. Of the twenty-three projects Cipla Foundation supported between 2021–2022, nearly one third of them were able to raise additional funds from donors for these projects.Footnote 7 Cipla recognizes that whilst government funding to palliative care may increase over time, there is an urgent need for more philanthropists and corporations to include palliative care projects within their scope of health-care work.
Challenges in Advancing Palliative Care
Notable challenges faced during implementation of the services work have included:
Changing the perception of palliative care: Misunderstandings around palliative care are a substantial barrier inhibiting all stakeholders, including patients, health-care professionals, and donors, from deeper involvement in this area. Shifting mindsets is extremely important for palliative care to truly become embedded in the health-care system. Cipla attempts to change this perception by avoiding certain terms such as ‘life limiting’, ‘threatening’, and ‘beyond cure’ whilst explaining palliative care. However, this requires a larger behavioural-change campaign to enable stakeholders to see the supportive nature of palliative care as well as the medical science of care in palliation.
Measuring impact: India lacks clear evidence of impact in palliative care. There have been some studies outside of India that demonstrated how early integration of palliative care leads to better health-related quality of life, improved communication, fewer emergency hospitalisations, less distress, and better satisfaction with care. However, there is a lack of India-specific research and data. Additionally, outcome tools in palliative care have been developed and standardised outside of India and need to be standardised based on the country’s national norms. Cipla, through its Foundation is now embarking on a research programme aiming to develop guidelines and standard operating principles for palliative care service provision.
Financing health care: Given that palliative care is not seen as part of the health-care continuum, funding is very limited in an already underfinanced broader system. This challenge forces the Cipla team to prioritise and strategise on how to achieve maximum reach. To ensure lack of funding does not limit newer initiatives, more philanthropists and donors need to co-fund palliative care projects, especially for home care services that reach patients most in need.
Supply of trained palliative care professionals: Related to the issues of awareness and funding, there is a dearth of health professionals opting to specialise in palliative medicine. This challenge requires deeper awareness in all medical, nursing, and social work colleges about palliative care as well as the development of specialised courses for professionals to further enhance their skills.
Whilst the Cipla team has attempted to mitigate some of these challenges in a limited way, it feels confident that now is the time for a concerted effort from all stakeholders to further advance the palliative care agenda. Cipla Foundation is committed to furthering this movement.
Conclusion
Through its philanthropy and CSR efforts, Cipla has worn multiple hats as a programme funder and implementer, broadening its scope and perspective on how to strategically shape the palliative care ecosystem. After twenty-five years working in this space, Cipla Foundation is now poised to move forward with its legacy. Whilst the Foundation hopes to continually be flexible in responding to emerging needs, the principles that guide its strategic focus will be based on a commitment to increasing access to palliative care, strengthening collaborations and partnerships, and collecting evidence to improve practice and policy.
Cipla Foundation believes that the pathway to achieving its goal requires collaborations at all levels. As it strengthens and forges new partnerships, it will continue to identify champions, work with the public health-care system, and ensure integrated models of care so that the needs of patients remain at the core of the service.
CF is further committed to facilitating platforms to increase dialogue and communication between stakeholders. It hopes this will lead to greater awareness about the key issues, attract more talent into the space, increase funding to palliative care, and develop more training opportunities and dissemination of information on palliative care.
Cipla’s work in service delivery through its Centre at Pune, has strengthened its conviction that palliative care, when understood as responsive care for patients with a serious illness, has the potential to transform the Indian health-care system to one that is more person-centred and can improve health-related outcomes. Cipla strives to make a difference with a strategy guided by keeping people, especially the most disadvantaged, at the heart of the health-care system. It hopes that this strategy of philanthropic commitment to palliative care that engages all stakeholders will create a ripple effect in the entire health-care ecosystem.