Introduction
Pediatric palliative care (PPC) adopts a comprehensive perspective, being dynamic throughout the course of the illness. It is essential to assess and address all physical, psychosocial, and spiritual needs that arise from the child and their family, treating them as a unit of care (Ministerio de Sanidad. Estrategia de Cuidados Paliativos 2014). Understanding life-limiting illness from the perspective of families facing such situations is crucial to improving quality and guiding the development of care for these patients. Qualitative research, focusing on the human experience, has gained prominence in this field, aiming to comprehend and interpret the reality, meanings, and actions of individuals in their context (Arantzamendi et al. Reference Arantzamendi, López-Dicastillo and Robinson2017). In essence, it seeks to explain how individuals attribute meaning to phenomena through their subjective experiences. Therefore, this research methodology, applied to the field of palliative care, aims to better understand patients and their families, professionals, and the contexts in which these health services are provided to enhance the quality of care.
One of the primary agents involved in the care of children with life-limiting conditions is their caregivers (informal or non-professional caregivers), including family or community members who do not receive payment for their activity (Beydoun et al. Reference Beydoun, Nasrallah and Sabrah2019). This situation entails a high level of stress, loss of self-esteem, decreased quality of life, and restructuring of family dynamics (Nightingale et al. Reference Nightingale, Friedl and Swalow2015; Woodgate et al. Reference Woodgate, Edwards and Ripat2015). In recent years, health-care professionals have become increasingly aware of the need to understand the perspectives of caregivers and families of these patients to establish care structures that meet their real needs (Hays et al. Reference Hays, Valentine and Haynes2006; Nightingale et al. Reference Nightingale, Friedl and Swalow2015; Stevenson et al. Reference Stevenson, Achille and Lugasi2013; Verbene et al. Reference Verbene, Kars and Schouten-van Meeteren2017; Verben el al Reference Verbene, Kars and Schouten-van Meeteren2019; Winger et al. Reference Winger, Kvarme and Loyland2020).
The PPC program at our tertiary university hospital, operating within the public health-care system, provides specialized and compassionate care to children and adolescents with life-threatening conditions. Serving the local community, particularly the 45,000 patients under 18 years old in its health area, the program ensures equitable access to high-quality palliative care services regardless of socioeconomic status. With an interdisciplinary approach and evidence-based practices, it offers symptom management, pain relief, psychosocial support, counseling, care coordination, advance care planning, and bereavement services. By integrating palliative care principles, the program aims to enhance patients’ and families’ quality of life, promoting dignity, comfort, and holistic well-being while respecting their values and preferences.
The rationale behind the PPC program lies in recognizing the complexities of caring for children with life-limiting illnesses. Unlike adult palliative care, PPC necessitates a family-centered approach, addressing both the child’s and caregivers’ developmental and emotional needs. Through interdisciplinary support and partnerships, the program empowers families, enhances coping strategies, and fosters resilience.
Moreover, the program emphasizes continuity of care and offers home-based palliative care to minimize disruptions to family life, promote normalcy, and strengthen connections within the community.
Therefore, our PPC program embodies a holistic and compassionate approach to PPC, guided by principles of equity, dignity, and respect for each child and family’s uniqueness. While essential, PPC’s specific impacts on families warrant further exploration. This study aims to illuminate families’ experiences within the PPC program, emphasizing the need for a clearer understanding of its context and objectives within the broader landscape of PPC.
This research aims to explore the experiences of families of children and adolescents enrolled in the PPC program regarding the care received and their perception of the impact it has had on their quality of life. Additionally, the specific objectives are to
– Explore the perceived impact on the physical, emotional, social, and spiritual spheres for families and children included in the PPC program.
– Explore their experiences and feelings regarding the care received before inclusion in the PPC program.
– Explore the limitations and possible areas for improvement perceived in the program based on their experience.
Materials and methods
Study design and characteristics
This is a qualitative descriptive study with a phenomenological approach. A total of 7 eligible patients were identified, and all their primary caregivers agreed to participate. In 1 case, it was not possible to conduct the interview within the specified timeframe due to the unavailability of the primary caregiver, resulting in 6 interviews (Table 1).
Table 1. Semi-structured interview
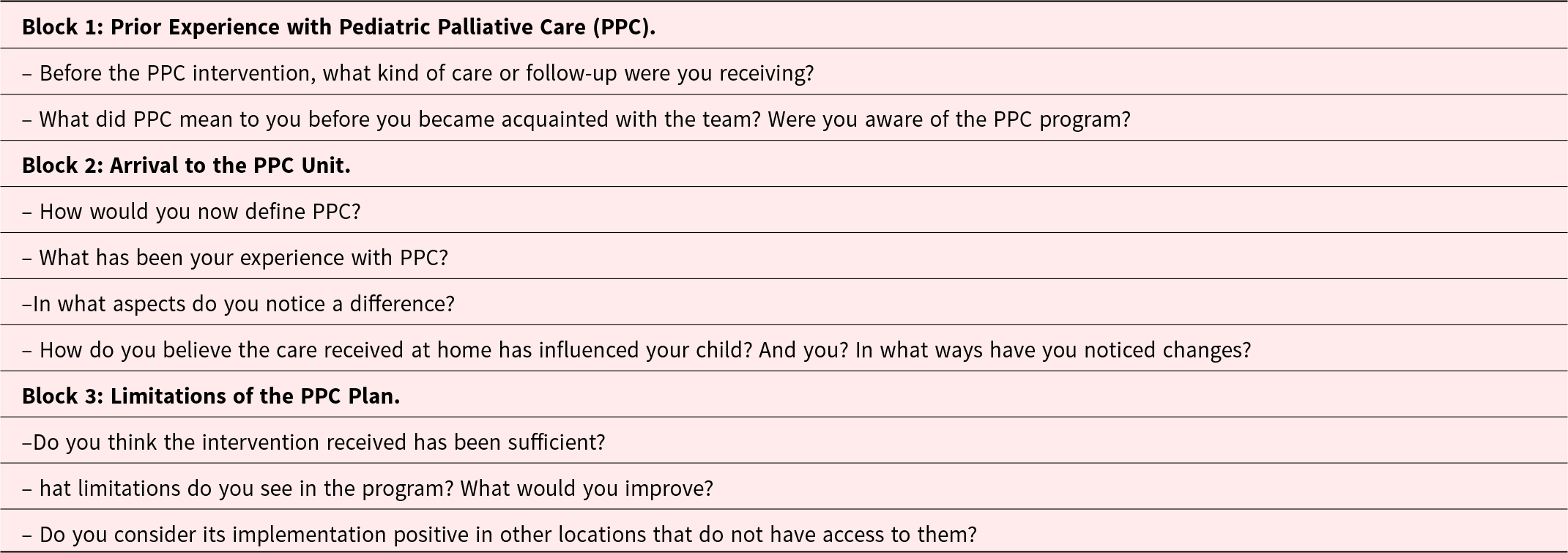
PPC: Pediatric Palliative Care.
Sample size adequacy was evaluated taking into account contextual factors, including the distinctiveness of the study population and the comprehensive nature of the information gathered from each participant.
A predetermined meeting point was established between the principal investigator and the participant (home or hospital). Before the interview, the purpose and characteristics of the study were explained again, and informed consent was obtained. Participants were asked for permission to record the interview in audio format using a mobile device to maintain the natural flow of communication between the researcher and participant. Subsequently, a literal transcription of the interview was carried out, forming the basis for data analysis documents along with the field diary maintained throughout the research process.
To understand the sample’s characteristics, theoretical convenience sampling was employed. The sample was based on a predefined conceptual framework defining the typologies or profiles of the sampling units (Duque and Aristizábal Díaz-Granados Reference Duque and Aristizábal Díaz-Granados2019). The principal investigator’s role in the PPC Unit during this phase of the research allowed direct access to the sample due to the therapeutic relationship with the participants, eliminating the need for intermediaries in the participant recruitment process. The primary caregivers of patients meeting the predefined characteristics were contacted by phone, and after explaining the study’s purpose and characteristics, a face-to-face appointment with the participant was arranged.
Participants and selection criteria
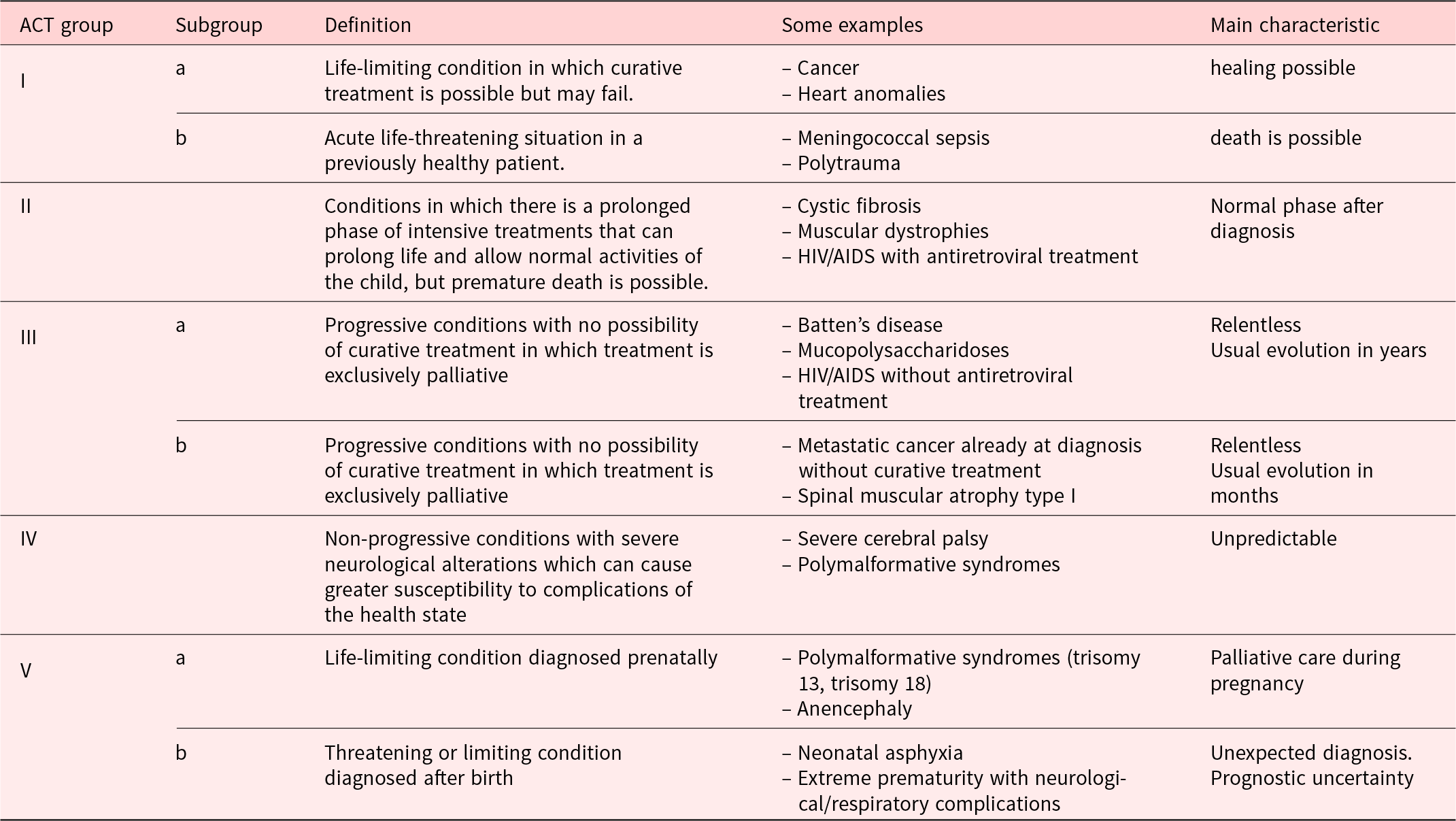
In this study, we focused on primary caregivers of patients enrolled in the PPC program, specifically those receiving home hospitalization. Home hospitalization refers to the provision of palliative care services within the patient’s home environment, aimed at enhancing comfort and quality of life while minimizing hospital visits. Caregivers of patients belonging to the Association for Children with Life Threatening or Terminal Conditions and their Families (Association for Children with Life-threatening or Terminal Conditions and Their Families 1997) (ACT) groups (Table 2), with a history of health-care needs before inclusion in the PPC program of at least 1 year, were selected. Inclusion criteria were voluntary participation in the study, correct completion of the informed consent, current role as the primary caregiver of a child or adolescent included in the PPC program (Table 2), inclusion in the program for at least 1 year, and a need for health care before inclusion in the PPC program as the primary caregiver for at least 1 year. Exclusion criteria were inability to communicate effectively in Spanish, the impossibility of conducting the interview within the specified timeframe for data collection and, patients in the end-of-life according to the identification of the inflection point (a period in the patient’s life where a change in the clinical trajectory of their illness is identified, manifested as an acceleration in clinical deterioration, decreased symptom-free intervals, increased hospital admissions, lack of response to treatment escalation, or repeated relapse of their baseline condition) (Martino Reference Martino2017).
Table 2. Patients entitled to palliative care according to the classification of the Association for Children with Life Threatening or Terminal Conditions and their Families (ACT), modified by R. Martino
Data analysis
Data collection utilized a semi-structured interview (Table 1) conducted in person with the primary caregiver of the child or adolescent included in the PPC program. Three supports were used to document contexts, ideas, and elements that emerged during the research: the research diary, field notes, and memoranda. These were unified in an electronic support safeguarded by the principal investigator under a code called the field notebook (Gibbs Reference Gibbs2012). For data analysis, literal transcription of interview audios was performed, assigning an alphanumeric code to each interview. Patient or health-care professional names were not reflected in the transcriptions. Atlas.ti 8.0® software was used to support the analysis of obtained data, including interview transcriptions and the field notebook.
In accordance with contemporary standards for qualitative research, we employed a rigorous approach to ensure methodological and epistemological adequacy, relevance, validity, and reflexivity throughout the study. Building upon Calderón’s criteria (Calderón Reference Calderón2002), as well as insights from recent reviews on quality indicators in qualitative research (Johnson et al. Reference Johnson, Adkins and Chauvin2020), we implemented several strategies to uphold the integrity and trustworthiness of our findings.
To address these aspects comprehensively, we ensured methodological rigor through several key steps:
First, methodological and theoretical-epistemological adequacy: We adhered to established qualitative research methodologies, including semi-structured interviews and thematic analysis, to capture rich and nuanced data on caregiver experiences in the context of PPC. Our interview protocols were carefully designed to elicit detailed accounts from participants while allowing for flexibility and responsiveness to emerging themes. Given that this research aims to explore the experiences and feelings of the participants, qualitative research with a phenomenological approach is considered the most appropriate methodology for this purpose.
Second, relevance: prior to data collection, we conducted a thorough review of the literature to ensure the relevance of our research questions and to situate our study within the existing scholarly discourse on PPC. As previously justified, understanding the experiences and perspectives of patients and their families is considered to provide relevant information when evaluating the effectiveness of the PPC program and suggesting areas for improvement, always with the ultimate goal of maximizing benefits for patients and their families.
Third, reflexivity: throughout the data collection and analysis process, we maintained reflexivity by critically examining our own biases and preconceptions. In this case, special attention and care have been paid to this point, aiming to minimize interference with the neutrality of the principal investigator that could arise from being a worker in the Unit and having a therapeutic relationship with the study participants. This involved regularly engaging in reflexivity sessions within the research team to discuss and challenge our interpretations of the data, allowing for critical self-awareness and transparency in our methodological approach.
Additionally, validity: to enhance the validity of our findings, all original data sources are available (recordings, interview transcriptions, field notes, signed informed consents, etc.). Additionally, in presenting the results, numerous direct quotes from the participants during the interviews are included to ensure the transferability of the conclusions developed to the participants’ discourse.
For the conduct of this research, the Declaration of Helsinki with its updates and revisions was considered. Participation was voluntary, and it was considered essential for each participant to accept and sign the informed consent document before each interview. This study was approved by the local Research Ethics Committee.
Results
A total of 6 primary caregivers (C) of patients (n = 6) were included in the study. All interviewees were the mothers of the patients, and all patients belonged to ACT groups II, III, or IV, in a phase of relative stability of their illness. This approach aimed to avoid potential interference from emotions generated by acute or end-of-life processes in their perception of the PPC team’s activity. The main characteristics of the patients are presented in Table 3.
Table 3. Baseline characteristics of the patients
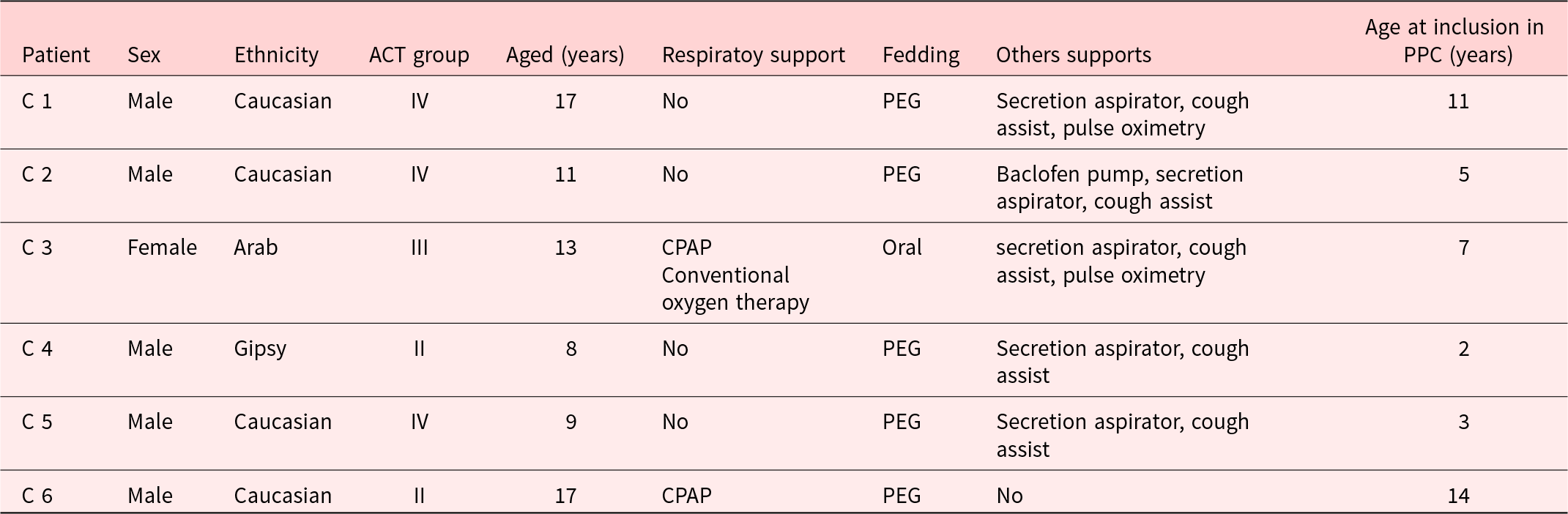
PPC: pediatric palliative care; CPAP: continuous positive airway pressure; PEG: percutaneous endoscopic gastrostomy. C: Caregiver. ACT group: Association for Children with Life Threatening or Terminal Conditions and their Families Classification.
Twelve codes were identified, grouped into 6 code families, and further categorized into three central themes. The obtained data are presented in Table 4.
Table 4. Results: central themes, code families and codes
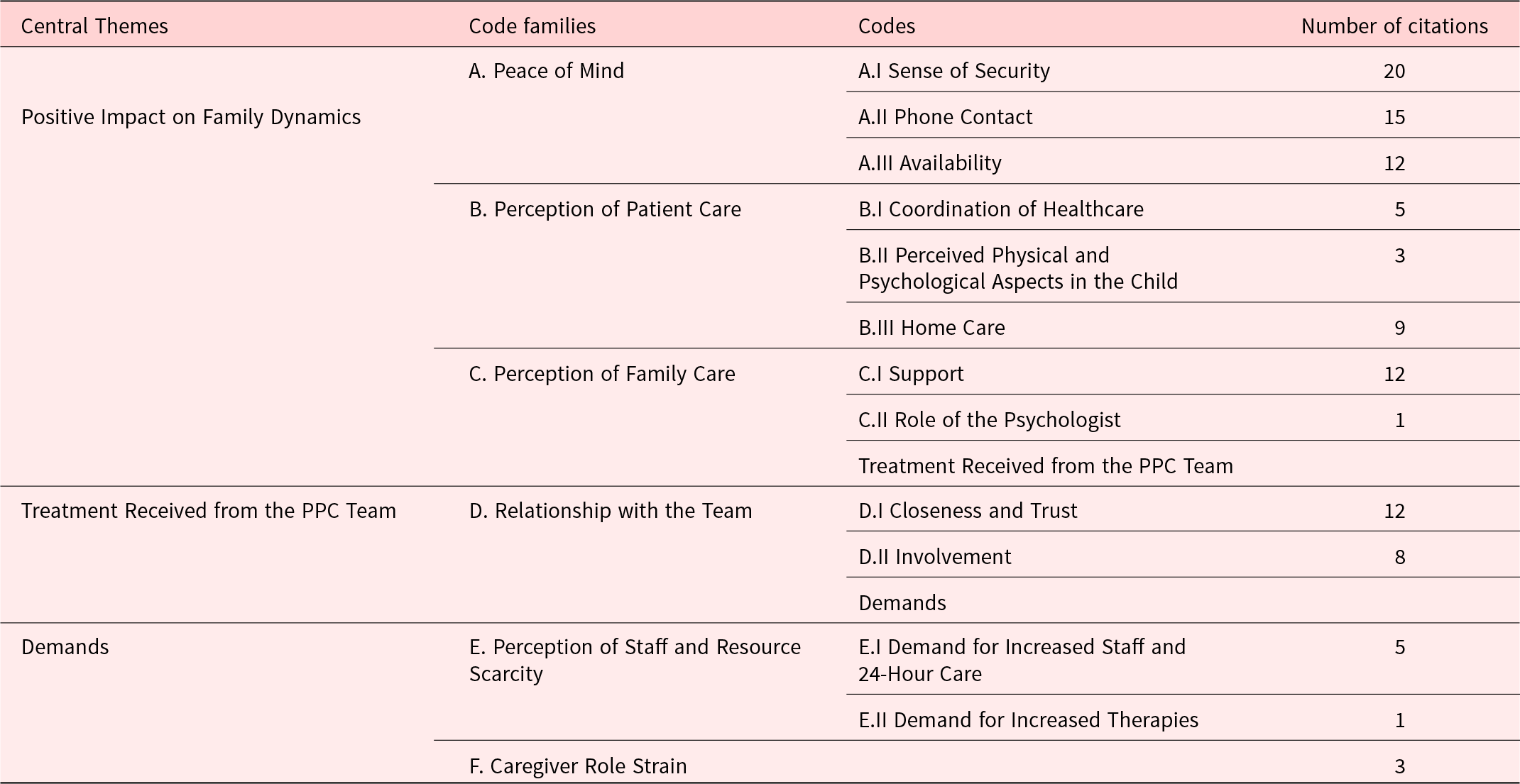
PPC: pediatric palliative care.
Positive impact on family dynamics
A consistent reference in all interviews was the general perception of a positive impact on the daily lives of families. Families reported a sense of tranquility, security, a perception of better patient care, and important support for caregivers. Despite being satisfied with the health care and treatment received before inclusion in the PPC program, families consistently reported a positive impact on their lives after enrollment. Sense of tranquility: Many references were made to the feeling of security provided by belonging to the PPC program. This feeling was largely attributed to the availability of direct contact through telephone communication in case of need.
– “Because you have a direct number at a given moment. If anything happens, it’s a relief and a rest to say, hey, this is happening. You come or you don’t come, it can be solved over the phone or whatever.” (C 1)
– “I am calm because, as I have the number, and maybe they don’t answer it at the moment, but I know that if the call comes, it’s okay.” (C 2)
– “I can call them and ask if anything happens to my child. I don’t call other doctors. I call them, and they answer or if they don’t answer, they see the call and call me to ask if I need anything.” (C 6)
– “You have a phone to call” (C 5).
Thus, thanks to this resource, but also simply by being part of the PPC program, families feel close to health-care professionals, as well as sheltered and with a sense of availability.
– “Maybe for you, it’s trivial, but I didn’t know what to do. Because I don’t have the same availability with my pediatrician.” (C 2)
– “I feel closer.” (C 3)
– “Now with the issue of the PEG that he has had recently, many doubts have arisen, many questions: if it is well placed, if the child is perfectly fed. You can’t wait three months for an appointment to solve it. These are doubts that arise in areas of your child’s illness that you have to solve, and you don’t know if you are managing them badly or managing them well.” (C 4)
– “They are always there.” (C 5)
– “Always be there.” (C 2)
In relation to these feelings generated in the families attended, 1 mother literally refers to how, for her, palliative care now means “quality of life”:
– “At first when they told me about palliative care, I felt like I was in the final phase, and it was difficult for me, you know? But then I saw that it was totally different, that it was the opposite.” “And now I tell you that for me it means quality of life, and to give the best possible life. That’s the feeling I have now; I’m not afraid of the name anymore.” to help you lead your life, not think about the other. I don’t even want to think about it. Just to lead life as normally and calmly as possible …”(C 2)
Better patient care: Families highlighted improvements in the care received, emphasizing the personalization and continuity of care as important aspects.
– “They are more involved, more aware. They know him better than anyone else.” (C 6)
– “Before he was admitted here, they were always worried. They were always on their toes, like, a thing happens to him, and they run to the hospital, and they don’t know what’s wrong. Here they are calmer. They know what he has, and they know what to do.” (C 1)
– “It’s different because they treat you very differently here. I think they personalize more. The ones from the health center, they’re not going to come and say, ‘I’m going to see what’s wrong with your child.” (C 3)
– “Being interconnected among different professionals, even though the palliative care doctors are the ones who act more directly with the child. But they can establish other lines with other specialists without also having to see the child. Like they plan things more and the intervention is more targeted.” (C 1)
– “They are attentive to everything, and you can ask anything; you don’t have to wait for an appointment in two months. With them, you have everything close by.” (C 3)
– “They manage what you need, they make everything easier for you..” (C 4)
– “I notice that the child is more controlled by them. In the end, there are more controls for him.” (C 4)
– “I see her very well, happier. She has a lot of confidence. For example, if she has a blood test, she says ‘with A (nurse) it’s better’. She has a lot of confidence with the team, and she is difficult, it is very difficult for her to gain confidence. If she doesn’t gain confidence, she is not happy, but with the whole team, she has a lot of confidence and is very happy. When they do something to her, she feels calmer.” (C 3)
– “The most positive thing is that I see the child happier, calmer. When they come to see him, after being with them, he feels better; I see him happier. He is fine, which is what matters to me.” (C 5)
Also included in this point are the benefits for the patient perceived by many families from home care, as it reduces the number of hospital trips, as well as provides closer monitoring and support in home care.
– “And then home care. In our case, as (child) has a hard time with travel, it is an advantage, no, more than an advantage. For us, it’s a lot.” (C 6)
– “A team that treats people as if they were in the hospital but at home. With a lot of experience. It is very good support for families.” (C 3)
– “When they placed the PEG, a granuloma appeared, and they came to heal it. These are things you don’t know, and by coming home, that has been resolved.” (C 4)
– “When they come, they are attentive to everything, that he is fine (child), that the machines he has work correctly at home, that those who come to change everything monitor them, that we are fine, how we feel, how we are..” (C 4)
Support for caregivers: Families consistently highlighted the support received by caregivers, emphasizing the psychological and emotional aspect of care.
– “What makes me happy is the treatment they give to my daughter (…) The one who comes is quite nice and has a great time with my daughter’s things her way.” (C 4)
– “Yes, a lot of help. They not only come to see him, but they also play with him, and they bring me things or come with a snack for him. They do their job and more. The truth is that they come to play with him. They always bring something, and they always leave a good mood.” (C 1)
– “Now we have this, you see the difference. One time I went to the hospital crying, and I was very overwhelmed. And a nurse told me that this happens, that it was normal, but I was not being treated at home. When you see them here, you say, ‘Wow, the hospital is there, and here I am at home.’ It’s the same, but it’s different. I’m more at ease. You’re more relaxed because you’re at home.” (C 3)
– “Psychologically, they have helped me a lot, much more than people think. And it is a very tough job for them, because to put yourself in the shoes of a mother.. they do it. For me, the group we have in our city does it, I don’t know about other cities, but here they get very involved.”(C 4)
– “There is a psychologist who supports us a lot. What we needed most was a psychologist. More for me, I needed it.” (C 5)
Impact on emotional well-being
Another prominent theme in the interviews was the impact on the emotional well-being of both the child and the family. Families consistently reported improvements in mood, decreased anxiety, and a sense of normalcy in the family environment.
Improvements in mood: Families frequently referred to positive changes in the emotional state of both the child and the family as a whole.
– “She’s happier. She’s more active. She was very still, very bored, and now she’s happier. She has more vitality.” (C 3)
– “You can tell the difference. Before, he was much more restless, more irritable, more… I don’t know how to explain it. More nervous, I guess.” (C 3)
– “It’s different. When you’re at home, you see it differently. If you go to the hospital, you see it differently. It’s like … being at home is more normal.” (C 3)
Decreased anxiety: Families consistently reported a reduction in anxiety levels, attributing this change to the support and accessibility provided by the PPC program.
– “The main advantage is tranquility. You’re not anxious because, if you need them, they’re there.” (C 2)
– “The difference is that you are calmer. Before, you’re with anxiety, with nerves, running to the hospital with the child, not knowing what’s happening to him. Now you’re calmer. You say, ‘Hey, something is happening to him. I call them, and they come.’”(C 1)
– “Here you can ask about anything. If there’s any doubt or anything happens, I can ask the doctor or the nurse who comes. At the health center, you can’t do that.” (C 3)
Sensation of normalcy: Families consistently highlighted the sense of normalcy achieved by the child and the family in the home environment.
– “The best thing is that he’s at home, that he’s calm, that he’s normal. It’s true that he’s much better at home.” (C 4)
– “Because when you have a child who is ill, you go to the hospital a lot, and your life changes. And this is different. Here, you have a somewhat normal life. You can say, ‘Let’s go to the cinema. Let’s go for a walk. Even if it’s only for a short time, you can do things you can’t do at the hospital. It changes your life a lot.” (C 3)
Treatment received by the PPC team
In several interviews, caregivers refer to the treatment provided by the PPC team. They feel that the team is like “a family” because of the close and friendly treatment received, as well as the high degree of involvement perceived by the families of the patients. These facts generate a mutual trust relationship between the team and the families, being one of the most mentioned and valued points by them.
– “It’s like we are family, or more than family. People with so much confidence, who you see are fighting, fighting for a patient, as if it were their daughter.” (C 3)
– “It’s not just the patient’s treatment with the doctor but also treatment at a personal level, like family. They get involved a lot, they are very attentive to you, and they give you a lot of encouragement. They leave the gown aside, as I say, and put themselves in the place of a human being. And that is very important for us. At least for me, I value it a lot, which nowadays is lacking.” (C 4)
– “They are more committed.” (C 5)
– “With all the doctors, I leave my daughter as if she were at home. If we are here, I am calm.” (C 3)
– “You trust someone who is going to come home.” (C 6)
Caregiver role strain
A point not directly mentioned but considered of great relevance due to its implications is the reference in three of the caregivers to the strain of exercising the caregiver role.
– “Because you go to bed thinking about what you have to do tomorrow, about how his meal is, about when he has to have physiotherapy, about his schedules, about making sure he sleeps his hours.. and that burns you out a lot psychologically and physically too, because I also have another child and I also have a partner.” (C 4)
– “Well, there is a psychologist who supports us a lot. What we needed most was a psychologist. More for me, I needed it.” (C 5)
In one case, a mother is identified as apparently on the verge of breakdown.
– “I am not well; I am having a very hard time; I am with him 24 hours; I am his mother.. I am here 24 hours; I don’t go out at all. The only day I go out is Wednesdays when someone from dependency comes, and I go grocery shopping. Look, I am alone. I have been separated since my son was 5 months old, he was a baby, and I have a 24-year-old daughter, who left to live with her boyfriend at 18 and has two children; and I am alone. I have no one. I am alone 24 hours, for everything. I am tired; I am exhausted.. Besides, it is my son, it is not someone I don’t care about, it is my son.” (C 6)
Challenges and areas for improvement
Despite the overall positive perceptions of families regarding the PPC program, some challenges and areas for improvement were identified.
Communication between health-care professionals: Families expressed the need for improved communication between different health-care professionals involved in the care of the child. Besides, caregivers had the perception of staff and resource shortages provided, mainly demanding more staff and extended hours of attention to nights and weekends.
– “Sometimes there is a lack of communication between the center, the hospital, and us. I think there should be more coordination. I go to the hospital, and the doctors don’t know what’s going on. And sometimes I say things here that they don’t know about either.” (C 3)
– “The one from the hospital comes (doctor), but sometimes I tell her things that I’ve already told the health center, and she doesn’t know. They don’t talk to each other. It’s like they don’t coordinate well. That’s what I miss.” (C 2)
– “In this case of personnel, I would like there to be a broader service. For example, also on weekends, to be able to locate them, but of course, for that, more doctors who specialize in palliative care and more professionals are needed, both doctors and A (nurse).” (C 1)
Limited availability of services: Families expressed a desire for more frequent and extended services, highlighting the positive impact on their lives.
– “It’s all very good, but I would like them to come more often. Sometimes they come, and then they take a step back, and then they come again. I would like them to come more regularly.” (C 1)
– “Sometimes, yes, I would like more. I can’t deny it. They help us a lot, but sometimes we need more support. Because sometimes, for example, we go to the hospital, and they see him, but then they don’t come home for a long time. And you say, ‘Hey, it’s been a long time. Why don’t they come?’ Because, if they don’t come, you go to the hospital.” (C 6)
– “Some palliative therapies also working together.” (C 5)
Perceived limitations in the home setting: Families acknowledged that, despite the positive impact, there were still limitations to care in the home environment.
– “Sometimes it is difficult to do some things at home. You don’t have everything you need, and sometimes, you would need more help. But, in general, the main thing is that we can be at home.” (C 1)
– “I would like them to have more resources. For example, physiotherapy. I would like them to have more resources, more professionals. Because, for example, my child needs physiotherapy, and there is a lot of delay.” (C 6)
Discussion
The analysis of the data obtained in this research reveals three central themes regarding the care provided by the CPP Unit.
Firstly, there is a highlighted positive impact perceived in family dynamics as in other studies (Hays et al. Reference Hays, Valentine and Haynes2006; Nightingale et al. Reference Nightingale, Friedl and Swalow2015; Stevenson et al. Reference Stevenson, Achille and Lugasi2013; Verbene et al. Reference Verbene, Kars and Schouten-van Meeteren2017; Winger et al. Reference Winger, Kvarme and Loyland2020). Caregivers express important changes in their subjective impression of improved family dynamics. They often mention feelings of tranquility, a sense of protection, and simplification of bureaucratic procedures related to the health care of their children. Families experience peace of mind and security, largely due to the team’s availability, manifested through telephone contact as a means of communication. Other noteworthy aspects include multiple references to the perception of the comprehensiveness of care, as well as attention to the entire family unit. Caregivers also feel important support from the team, even describing this overall impression using the term “quality of life.” Furthermore, the perception that the team is like a family to them and their strong involvement in the care of the child and family establish a mutual trust relationship, contributing to the feelings of tranquility and security.
Secondly, a recurring theme has been the experience of the treatment received from the CPP team. Despite having received adequate care previously, families identify the inclusion in the PPC program as an event that brought about a meaningful improvement in their lives. This underscores the holistic and family-centric approach of the PPC program, which goes beyond mere medical treatment to provide comprehensive support to families facing life-limiting illnesses.
Additionally, there was reflection on the fact that the questions asked in the interviews could potentially trigger or remind families of previous unpleasant experiences, such as the moment of diagnosis or past negative experiences related to patient care. In such a delicate moment as end-of-life care, where the primary goal is to focus on the present moment and provide support, it was recognized that evoking painful memories could have a negative effect on the family’s experience. Therefore, it was decided to avoid such questions that could potentially cause additional distress during such a crucial time.
For this reason, patients in the end-of-life stage were excluded upon identifying the inflection point. Therefore, considering that the team’s main approach is to ensure that patients spend as much time as possible with their loved ones and maintain as normal a routine as possible, it was deemed ethically inappropriate to disrupt family dynamics to make the interviews, which. Given the vulnerability of the situation, it was prioritized that visits during end-of-life care focus exclusively on clinical and supportive aspects.
A crucial point explored is related to the limitations and areas for improvement perceived by families. Despite being generally satisfied with the care received and showing reluctance to mention limitations, three of them express the need to address the strain of taking more comprehensively on the role of caregiver for these patients. This is particularly important due to the impact it can have on patient care and on the caregiver’s health and social functioning. In this regard, there is a proposal to promote support for families by psychologists, as well as to be attentive to symptoms of fatigue and potential caregiver burnout, suggesting resources such as family respites, which are currently not offered by our unit, to prevent their occurrence (Gérain and Zech Reference Gérain and Zech2021, Reference Gérain and Zech2018; Ministerio de Sanidad. Estrategia de Cuidados Paliativos 2014). This fact should make us reflect on possible areas for improvement in the assistance provided to patients and their families, aimed at avoiding the breakdown of caregivers of our patients.
Our findings reveal profound positive impacts on family dynamics, emotional well-being, and caregiver support within the PPC program. However, challenges such as communication gaps and limited-service availability underscore the need for program refinement.
One theoretical framework that may be particularly relevant is the Family Systems Theory, which posits that families operate as interconnected and interdependent systems, with each member influencing and being influenced by the others (Bowen Reference Bowen1978). Applying this framework to the study findings, we have could examine how the PPC program impacts not only the patient but also the entire family unit. For example, the sense of tranquility and support reported by caregivers may be indicative of the program’s ability to strengthen family resilience and cohesion in the face of adversity. The analogy of the health-care team as a family offers a valuable lens through which to investigate the interpersonal dynamics within PPC. This metaphor provides insight into the roles, interactions, and support mechanisms that characterize collaborative care in the PPC setting. By delving into this comparison, we could elucidate how health-care professionals are perceived by caregivers, examining instances where they may serve as surrogate family members, providing both medical expertise and emotional support. Additionally, exploring the implications of this familial dynamic could shed light on communication patterns, decision-making processes, and the provision of holistic care within the PPC program. Furthermore, reflecting on the concept of “care” within this familial context underscores the importance of cultivating authentic connections and mutual respect. Overall, further developing the analogy of the health-care team as a family offers an opportunity to deepen our understanding of the complex relationships and care dynamics in PPC, contributing to effective palliative care provision.
Furthermore, to explore the concept of anticipatory grief within the context of PPC is important. Anticipatory grief refers to the process of mourning and psychological preparation that occurs in advance of an expected loss (Maciejewski et al. Reference Maciejewski, Zhang and Block2007). By acknowledging and addressing anticipatory grief among families, health-care providers can offer targeted support and interventions to facilitate coping and adaptation to the challenges of caring for a child with a life-limiting illness.
Additionally, the transactional model of stress and coping (Lazarus and Folkman Reference Lazarus and Folkman1984) may offer insights into how families perceive and respond to stressors associated with PPC. By examining the appraisal processes and coping strategies employed by caregivers, we could elucidate the mechanisms through which the PPC program influences family well-being and adaptation.
We believe that incorporating these theoretical perspectives into the PPC program would enrich the interpretation of the study findings and provide a more comprehensive understanding of the experiences of families in PPC.
By engaging in a narrative exploration of the interview data, we have could uncover meaningful themes and patterns that elucidate the multifaceted nature of the families’ experiences in PPC. This approach we allowed for a more nuanced understanding of the challenges, coping strategies, and psychosocial dynamics that characterize the caregiving journey.
Furthermore, we strive to capture the diversity of experiences within the participant population, recognizing that families may have varying needs, preferences, and cultural contexts that shape their perceptions of palliative care. By amplifying the voices of marginalized or underrepresented groups, this study could contribute to a more inclusive and holistic understanding of PPC experiences.
Regarding study limitations (Smith Reference Smith2011), it is worth noting that being conducted by a single researcher does not allow for researcher triangulation. There was also no triangulation of methodologies and methods. Another possible limitation is the existence of a therapeutic relationship between the principal investigator and the participant, which could interfere with the participants’ complete honesty in pointing out areas for improvement or limitations in the care received. Although the study is limited to patients from a single center, this is not considered a limitation since the goal was to analyze the quality of care and potential areas for improvement in a specific PPC Unit.
Moreover, addressing the concern regarding the adequacy of the sample size, it is acknowledged that the inclusion of six interviews may raise questions about the comprehensiveness and generalizability of the study findings. However, the sample size in the qualitative research, the depth of data obtained from each interview, contextual factors, and the principle of data saturation, where in additional interviews may not yield substantially new insights according to other studies (Rico-Mena et al. Reference Rico-Mena, Palacios-Ceña and Martino-Alba2019; Somanadhan and Larkin Reference Somanadhan and Larkin2016). Therefore, contextual factors play a crucial role in determining the adequacy of sample size in PPC qualitative research. Considering the unique nature of the PPC study population, characterized by its specialization or hard-to-reach group due to the limited volume of pediatric cases compared to adult palliative care, a smaller sample size can still yield valuable insights.
However, the limitations imposed by the sample size should be acknowledged, and future research directions could be suggested to address this constraint.
Conclusions
In summary, our study highlights the important positive impact of the PPC program on the perceived quality of life of families with children and adolescents facing life-limiting illnesses. However, addressing communication gaps and expanding service provisions to support caregivers and prevent burnout are pressing needs.
Furthermore, while our findings contribute to understanding the benefits of the PPC program, there are broader implications and future directions for clinical practice and research. Situating our study within the broader health-care delivery and policy frameworks could emphasize the importance of PPC in addressing unmet needs and promoting equitable access to comprehensive care services. Additionally, discussing potential policy recommendations or advocacy initiatives arising from our findings could contribute to shaping systemic changes and enhancing support structures for families navigating PPC.
Reflecting on the methodological and conceptual contributions of our study to the broader field of palliative care research can foster ongoing debates and discussions within the academic community. By critically examining the strengths and limitations of our research approach and identifying areas for future inquiry, we can enhance scholarly rigor and contribute to continuous learning and improvement in PPC.
Finally, offering practical recommendations for health-care practitioners and policymakers based on our findings could empower stakeholders to enact meaningful change. Whether it involves enhancing caregiver support services, optimizing care coordination mechanisms, or integrating patient and family preferences into care planning processes, actionable insights can improve the quality of care for children with life-limiting conditions and their families.
In conclusion, our study provides a more comprehensive understanding of PPC by expanding broader societal implications, methodological contributions, and actionable recommendations. We aim to further enrich the PPC experience for families in need, inspiring meaningful action in practice and policy, ultimately improving outcomes for families facing life-limiting illnesses.
Funding
No funding received for the study.
Competing interest
The authors have no conflicts of interest to report.
Ethical approval
This study was reviewed and approved by our institution’s ethics committee.







