Recruitment is the dialogue which takes place between an investigator and a potential participant prior to the initiation of the consent process. It begins with the identification, targeting and enlistment of participants (volunteer patients or controls) for a research study. It involves providing information to the potential participants and generating their interest in the proposed study. There are two main goals of recruitment:
-
• to recruit a sample that adequately represents the target population;
-
• to recruit sufficient participants to meet the sample size and power requirements of the study (Reference Hulley, Cimmings and BrownerHulley et al, 2001; Reference KeithKeith, 2001).
Problems with recruitment can disrupt the timetable for a research project, preoccupy staff, reduce the ability of a therapeutic study to detect treatment differences and, ultimately, result in a trial being abandoned (Reference Ashery and McAuliffeAshery & McAuliffe, 1992).
During recruitment, the sampling process can suffer from associated problems of non-response and the resultant selection bias. The proportion of eligible participants who agree to enter the study (the response rate) influences the validity of the inference that the sample represents the population of interest (Reference Woods, Ziedonis and SernyakWoods et al, 2000; Reference Hulley, Cimmings and BrownerHulley et al, 2001). People who are difficult to reach and those who refuse to participate once they have been contacted tend to be different from people who do not enrol. A summary of participant characteristics often associated with poor response is provided in Box 1 (see Reference Armstrong, White and SaracciArmstrong et al, 1992).
Box 1 Main factors adversely affecting response rates
Greater age
Male gender
Non-White race
Urban residence
Low educational status
Unemployed or low occupational status
Low family income
Smoker
Recent illness or poor present health
High use of medical care
Retention of participants is a related and important aspect of recruitment. Poor retention is costly both financially and in terms of time. Early retention techniques should be incorporated into recruitment strategies during the planning phase of the study (Reference NishimotoNishimoto, 1998). Retention also involves building relationships with participants to encourage their continuing participation.
Recruitment is perhaps the most challenging part of a clinical research study. It is often left for junior and inexperienced researchers to undertake and it is not often reported adequately in the literature (Reference Dowling and WienerDowling & Wiener, 1997). Participant recruitment is also dependent on the type of study undertaken, collaboration with the clinician, characteristics and preferences of the participants and the recruitment strategies employed. The aim of this article is to inform clinicians about these key issues for research on clinical diseases and treatment methods in psychiatry.
Design issues
Factors that need to be taken into consideration when recruiting participants include: sample size requirements; ethical principles; the type of study design; and the data collection methods (questionnaire, interview techniques) to be used. The main types of study design are shown in Fig. 1.
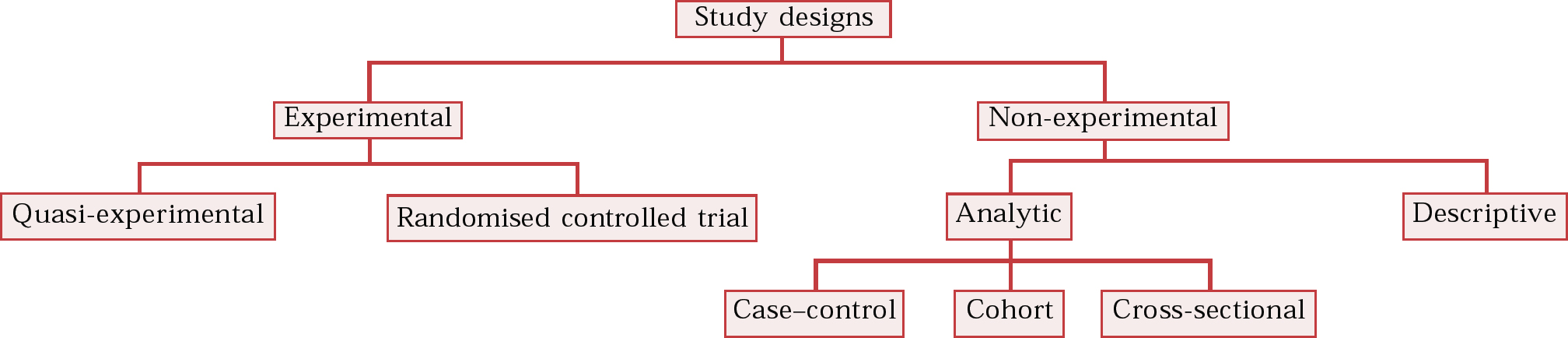
Fig. 1 Classification of study designs.
Sample size and ethical principles
Estimating the required sample size is one of the most important aspects of the recruitment process. Before a study is designed, it is important (if not mandatory) to calculate the sample size necessary to show a clinically important result. A sample size too small to detect differences could lead to studies which are unethical or wasteful. Furthermore, it can produce misleading results. For example, the results may show that there is no difference between groups or association between variables, when in fact there is a difference or an association (a Type II error). In contrast, a sample size that is too large leads to unnecessary expenditure of time, effort and finance. To minimise the probability of such errors, a power calculation is usually undertaken at the design stage. (Power can be defined as the probability of correctly concluding that there is a difference, given the sample size.) For these reasons researchers must make allowances in terms of time and money for the recruitment of a desired sample size (Reference StreinerStreiner, 1990; Reference Hulley, Cimmings and BrownerHulley et al, 2001).
As ethical principles must be adhered to and allowance made for potential participants who decline to take part, the required sample size needs to be adjusted to reflect the refusal rate. Ethical principles are based on the respect of the researcher for all potential participants and thus require the researcher to (i) obtain informed consent, (ii) protect participants with impaired decision-making capacity and (iii) maintain confidentiality (Reference Hulley, Cimmings and BrownerHulley et al, 2001). Informed consent is the process by which a fully informed individual voluntarily decides whether or not to take part as a research participant. The discussion between the recruiting researcher and potential participant should include the following: the nature of the procedure; reasonable alternatives to any proposed intervention; the relevant risk; benefits and uncertainties relating to each alternative; assessment of the potential participant's understanding; and the participant's acceptance of the intervention (see Box 2). The language used in the process should be pitched at a level that can be understood by the potential participants. For informed consent to be valid, the person concerned must be competent to make a decision and the consent must be voluntary (Reference Beauchamp, Cook and FayerweatherBeauchamp et al, 1991; Reference CarpenterCarpenter, 1999; Reference MichelsMichels, 1999). To avoid any suggestion of coercion, which can easily occur in clinical situations, adequate time must be allowed for the patient to comprehend and give feedback (i.e. between the initiation and completion of the consent process). An information sheet and a consent form are required and the latter is signed by the participant and the researcher at the end of process.
Box 2 Content of participant information sheet and consent form
Names of the investigators
Purpose of the research
Description of procedures
Estimate of time required
Potential benefits and risks of the procedures
Procedures to maintain confidentiality/anonymity
A statement that potential participants can refuse to participate or withdraw from the study at any time without prejudicing their care/interests (the right to refuse/withdraw)
An explicit offer to answer questions or provide further information, and whom to contact
Cross-sectional design
In a cross-sectional study, all the measurements of risk factors, outcome and confounding variables are made at a single point in time or over a short, specified period with no requirement for a follow-up period. For example, cross-sectional studies can provide data on the disease prevalence and distribution of the aforementioned variables. Recruitment for a cross-sectional study is generally less difficult than that for cohort studies and randomised controlled trials, because it involves one-off data collection with no commitment to follow-up.
Case–control design
In a case–control study, individuals with a particular condition or disease (the cases) are compared with a series of individuals in whom the condition is absent (the controls). Retrospective comparison between the two groups can then show differences in predictor variables (using assessments/measurements) that might explain why the cases developed the disease but the controls did not. Case–control studies are susceptible to a sampling bias by the recruiting researchers. Separate sampling of cases and controls, and the retrospective measurement of predictor variables, can bias the results and the conclusions drawn from them. This can be minimised by careful attention to the recruitment of a representative sample of cases and selection of appropriate controls.
Cohort studies and randomised controlled trials
In a cohort study, individuals are identified and grouped according to whether or not they possess a risk factor that is of interest (prospectively). The participants are then followed up over time and the incidence of the outcome (disease) is compared between the two groups (according to their risk factor status).
In a randomised controlled trial, participants are randomly allocated to one of two or more different groups, which are then treated in different ways (prospectively). The groups are followed up over time and measures of outcome (disease) are compared at the end of the study.
It is difficult to recruit participants for these studies because they often require a commitment to long-term follow-up. Both types of study usually require large sample sizes. Difficulties may arise with recruitment for cohort studies when participants do not see the point of the research because they have not yet developed the disease being studied. Recruitment for a randomised controlled trial is usually more difficult than that for an observational study because the participants must be willing to be assigned randomly and to take or accept treatments to which they may have been blinded. The possibility of receiving a placebo treatment is often a source of concern (Reference Hulley, Cimmings and BrownerHulley et al, 2001).
Data collection
The two most common methods of data collection in psychiatric clinical research are questionnaires and interviews. Questionnaires are usually self-report instruments, whereas interviews are administered verbally by the researcher. Each approach has costs and benefits and implications, therefore, for participant recruitment. Questionnaires are commonly used with cross-sectional survey designs. They are generally a more efficient, uniform and cheaper way to administer simple questions. It is usually better to use interviews to collect answers to complicated questions that require explanation or guidance. Research interviewers can ensure that the instruments are answered completely, probing when the responses being volunteered fall short of what is required. Interviews may be necessary when participants have different levels of reading ability and might find it difficult to understand the questions. However, interviews are more costly and time-consuming and the responses may be influenced by the relationship between the interviewer and the respondent (Reference Polgar and ThomasPolgar & Thomas, 2000; Reference Hulley, Cimmings and BrownerHulley et al, 2001). For example, interviewers can increase the magnitude of the error if, by their appearance, manner, method of administration of the interview or method of recording of the responses, they exert a qualitative influence on participants’ responses (Reference Armstrong, White and SaracciArmstrong et al, 1992). Newer and alternative methods of data collection include computer-assisted telephone interviewing and internet-based (online) questionnaires (Reference Smith and SeniorSmith & Senior, 2001).
The choice of data collection method is often dictated by practical considerations such as costs and logistics. When two methods are feasible, the choice involves trade-offs between cost-effectiveness, complexity of the questions to be answered and the required response rate. Sometimes a combination of administration methods is used. Within a single assessment, the number of instruments used should be minimised to prevent excessive participant burden. With repeat assessments over a period of time (i.e. follow-up studies), use of numerous instruments will increase investigator burden and will also contribute to poor recruitment. A cardinal rule is that it is usually not necessary to administer all instruments at every assessment.
Choosing the participant group
Before beginning the recruitment process, it is critical that the essential inclusion and exclusion criteria are decided for the study population. These are partially defined by the research question and hypotheses.
Generalisability
The generalisability of the research findings is dependent on the group that is targeted. If conclusions are to be generalise to the whole country, participants should ideally be drawn from different centres (urban and rural) across the whole geographical area. It must also be considered whether the study population should include patients in hospitals, community clinics and primary care or be from the nation at large. Considerable variation is therefore required in the recruitment strategies used to find participants, and which range from attending ward rounds to knocking on people's front doors.
Representative sample
Once the study population has been determined, the next step is to consider how to obtain a representative sample of that population. Failure to do so will result in poor generalisability of the results, even for the geographical area under investigation. Specific attention may be required for the adequate recruitment of participants from ethnic minority, non-English speaking, elderly, cognitively impaired or homeless groups. These groups may require different approaches, with the initial emphasis being on building trust and aligning the research goals with those of the minority community (Reference Levkoff, Levy and WeitzmanLevkoff et al, 2000; Reference McNeilly, Musick and EflandMcNeilly et al, 2000). To achieve this, bilingual or same-culture staff can be hired to target community leaders from religious centres, day centres and action groups. Patients detained in hospital are another important group that is often inadequately represented in research. In some cases, more extreme clinical presentations make it difficult to conduct the lengthy assessments required for research. However, this is not a sufficient reason to exclude all such patients. Thus, careful consideration (and justification) must be given to the process of setting the inclusion and exclusion criteria in research as well as to the subsequent impact that this will have on the recruitment strategies used.
‘Normal’ control participants
Some studies require the selection and recruitment of an appropriate comparison group, and ‘normal’ healthy participants may be selected. A variety of recruitment strategies can be used, including advertising in job-centres and supermarkets. It is often very tempting for the researcher to recruit friends and colleagues and, in some cases, students are given course credits if they ‘volunteer’ to take part (Reference LyddyLyddy, 2002). Such a situation causes concern as participants should be able to volunteer freely. Furthermore, recruiting university-educated volunteers may not allow for an appropriate comparison with the patient participant group, both in terms of basic demographic factors (e.g. social class, level of education) and core personality traits. Perhaps in an attempt to overcome such difficulties, a Centralised Recruitment Program has been developed in New York. This maintains a pool of healthy participants who are interested in taking part in research (Reference Schechter, Strasser and SantangeloSchechter et al, 1994). Although initially these individuals are not directly recruited to a specific study, a participant self-selection bias is, none the less, still evident.
Response rates
The response rate is the proportion of those approached who eventually agree to participate in research. It is critically dependent on the selection of the sample of potential participants, the nature of the research and the recruitment strategies utilised. Overall response rates can be enhanced by using a multi-tiered strategy for all initial non-respondents (see ‘Assertive tracking’ below). Therefore, non-respondents are approached a second or even a third time, as required, until a response is achieved (even if it is a refusal to participate). However, researchers should note that the specific response rate will usually be highest for the first tier and will reduce by approximately half for each subsequent tier (Fig. 2). There is a general consensus that response rates of 70% and above are necessary to ensure that the obtained sample group is sufficiently representative of the target population from which its members are drawn. The assumption here is that the remaining non-respondents are unlikely to have markedly different views and presentations from those that have been successfully recruited into the sample. Low response rates are criticised on the basis of a non-response bias, i.e. the views of the non-responders may significantly differ from those identified in the recruited group. Attempts to overcome this include demonstrating the lack of significant differences in basic characteristics and demographics between the non-responders and responders.
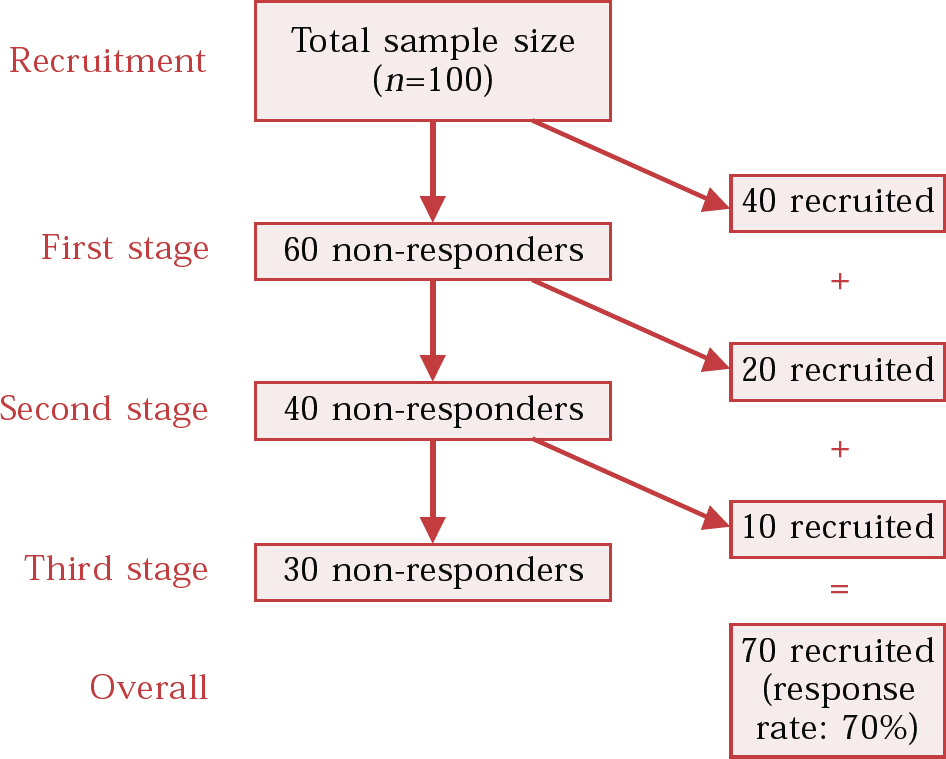
Fig. 2 Response rate decay over three stages.
Working with other clinicians
Most research studies of human participants involve working with other mental health care professionals. Box 3 summarises the key points of collaboration, which are examined in greater detail below.
Box 3 Working with colleagues
Do not underestimate the importance of initial contact with staff from key recruitment sites
Provide adequate information using a variety of methods
Clarify roles, responsibilities and expectations of potential collaborators
Show appreciation for help received
Remember to give feedback
Establishing collaboration
Successful recruitment of participants (in the clinical setting) is critically dependent on initial contacts made with administrative and clinical staff from key recruitment sites. Attention should be paid to factors such as administrative support and the attitude of clinical staff, volume/turnover of patients and stability of the patient population. It is noteworthy that some health professionals advise their administrative staff to discourage calls that include the word ‘research’. Clinicians who are supportive of research should be identified at an early stage in the recruitment process. This will save time later on by avoiding unproductive visits to less-than-enthusiastic parties in the future. Attempts at understanding the motivational needs of clinicians can lead to a more accurate perception of how to reach willing collaborators (Reference Young and DombrowskiYoung & Dombrowski, 1989).
It is essential to seek permission at an early stage to carry out a study. Potential collaborators need to know exactly what they will be asked to do, how much time they will be expected to give and what use will be made of the information they provide. Health professionals, administrators, medical records personnel and ward clerks will have to be convinced of the researcher's integrity and the value of the research before they decide whether or not to cooperate (Reference BellBell, 1993; Reference Miller, Rosenstein and DeRenzoMiller et al, 1998). In this regard, it is helpful if the junior researcher has had a few years of clinical experience and if the principal investigator makes a high-profile appearance at the early stages of planning recruitment.
Methods of collaboration
Pre-study promotion is usually targeted at potential referrers. Various methods are used, including presentations, specially arranged meetings, forums and road shows. During this phase, clear procedures for recruitment should be established between the researcher and the referring clinicians. Mutually agreed procedures should be developed and clearly documented. Eligibility criteria should be clearly stated and recruitment materials (patient information sheets, consent forms) must be provided. For clinical trials, the role of the responsible medical officer must be clarified. Procedures during acute or emergency situations should be outlined and, ideally, rehearsed. Care must be taken not to make excessive demands on the time and effort of the community mental health team (CMHT) (Reference BellBell, 1993).
Maintaining collaboration
During the study, it is important to maintain frequent contact with a nominated member of the referring CMHT, both by telephone and by visits to the referring site. The researcher should make an effort to identify convenient opportunities to promote the study and to recruit participants. This can be achieved by volunteering to offer services such as clinical sessions, attending ward rounds and teaching. The question ‘What can I do for them [the collaborators] so that they will refer patients to the study?’ should constantly engage the researcher. Appreciation should be demonstrated in reciprocation for help given by collaborators. Lastly, regular feedback on results of the investigation and changes in mental state (for individual patients) should be provided to the CMHT as well as information about the overall findings of the research. This aspect is often overlooked and can have profound adverse consequences on future attempts to recruit participants in the local region.
Recruitment techniques
Techniques to enhance recruitment include addressing the participant's willingness to take part, the investigator's personal performance and utilisation of appropriate methods (Box 4).
Box 4 Techniques
Consider the participant's perspective (costs and benefits)
Stress the relevance of the research
Enhance generic and personal skills and interpersonal communication skills
Establish adequate training and supervision, targets and investigator incentives
Implement assertive tracking procedures using various modes of communication
Box 5 The participant's perspective – costs and benefits
Costs
Undesired experimental design
Requirement of regular or costly travel to investigation site
Lengthy or frequent appointments required
Tedious, repetitive and lengthy questionnaires
Discontinuation of current treatment
Risk of adverse side-effects from starting new treatment
Risk of being randomised to a placebo group
Benefits
Increased enjoyable personal contact (with services)
Accessibility and affordability of therapy
Altruistic intent
Small financial incentives (to offset costs of time and travel)
Alternative incentives: food vouchers, T-shirts, mugs, book tokens, cards
The participant's perspective
Participants take part in research voluntarily, hoping that this will bring them direct therapeutic benefits or will ultimately improve treatment for future patients. Respect for participants (and their relatives and carers) can help to establish trust and rapport (Reference Miller, Rosenstein and DeRenzoMiller et al, 1998). Few participants will take part in research unless they can identify with and understand its validity and relevance. Consequently, an adequate, clear and concise explanation must be provided (this is also essential when obtaining informed consent).
Presumably, participants conduct a personal cost–benefit analysis when deciding whether or not to participate in research. Attention to these issues may gain the participant's confidence, with resultant successful recruitment (Box 5; Reference Sibbald, Addington-Hall and BrennemanSibbald et al, 1994; Reference Hough, Tarke and RenkerHough et al, 1996; Reference Ribisl, Walton and MowbrayRibisl et al, 1996; Reference Dowling and WienerDowling & Wiener, 1997; Reference BootsMiller, Ribisl and MowbrayBootsMiller et al, 1998; Reference Lindenberg, Solorzano and VilaroLindenberg et al, 2001). Time, travel, financial and incon-venience costs for participants can be minimised if researchers are accommodating and flexible. Financial incentives can be effective but are not significantly motivating for all participants. However, enclosing a gratuity with a postal survey can double the response rate compared with the situation when the incentive is promised contingent on survey completion and return.
The investigator
Certain personal attributes are an asset to any research investigator. These include being conscientious, having professional integrity and paying meticulous attention to detail. Good interpersonal skills should include the ability to be respectful, tolerant, tactful and approachable and to show a caring and compassionate attitude. Experience in health services and familiarity with the specialist field and the target population are desirable. Appropriate training and regular supervision are also essential prerequisites and these should cover: briefing on the objectives of the project; confidentiality procedures; personal safety; observation and practice sessions under supervision; learning from colleagues who have experience in the same area; and giving attention to the tracking of potential participants. Together with the junior investigator's high visibility at target outreach sites, these factors will help the investigator to build strong relationships with potential referrers and participants.
Although paying investigators on a piece rate basis may enhance recruitment, not all of them will be motivated by this. The associated personal financial insecurity can lead to rapid staff turnover, which is undesirable in the long run. A fixed salary or even a hybrid approach, using both a fixed salary and incentive bonuses for achieving targets, are preferred alternatives.
Methods
Methods and tools used to increase awareness of and accessibility to a study during the recruitment phase are shown in Box 6 (Reference Sibbald, Addington-Hall and BrennemanSibbald et al, 1994; Reference Desmond, Maddux and JohnsonDesmond et al, 1995; Reference Coen and PatrickCoen & Patrick, 1996; Reference Ribisl, Walton and MowbrayRibisl et al, 1996; Reference BootsMiller, Ribisl and MowbrayBootsMiller et al, 1998; Reference Fischer, Dornelas and GoetheFischer et al, 2001). Ideally, the chosen recruitment methods should fit the target population and sample size, although resources and costs may ultimately bias the choice.
Box 6 Methods and tools used to increase study awareness and accessibility
General
A project logo
Business cards
Freephone number and 24-hour answering machine
Websites
Mailshots (mass or targeted)
Fliers/posters in key locations (see below)
General public
Radio
Press releases to local and national newspapers
Key locations – public access buildings, including:
-
• community centres
-
• supermarkets
-
• cinemas
-
• libraries
-
• laundrettes
-
• religious buildings
-
• employment centres
Clinical groups
Announcements and presentations to potential referrers or participants by:
-
• arranged meetings
-
• forums (user-groups)
-
• road-shows
Key locations – specific buildings, including:
-
• accommodation facilities
-
• mental health community facilities
-
• clinics and hospitals
Assertive tracking
The first rule is to not give up after the first attempt to recruit a potential participant. Regardless of whether early attempts were initially successful, they should be followed up. Second, many researchers advocate the use of different methods of communication with participants, including letter, telephone, e-mail or face-to-face contact – the significance of personal contact should not be underestimated. Using a different method of communication on subsequent attempts to establish contact may yield new success and thus achieve good response rates (Reference Lindenberg, Solorzano and VilaroLindenberg et al, 2001; Reference Edwards, Roberts and ClarkeEdwards et al, 2002).
Locator details and collateral contacts
When a potential participant is first identified, contact should be established wherever possible. Confirm the contact details at each subsequent contact to avoid early attrition before recruitment is completed. Mobile telephone numbers and e-mail addresses may remain unchanged despite many changes of home address, so always ask for these details where appropriate. Also include contact details of collateral agencies (out-patient services, key workers), families and friends. Participants should be asked to sign release of information forms, allowing contact with these agencies and individuals in order to obtain updated details, if required. The participant's right to confidentiality is a key issue here and this principle should not be compromised (Reference Cohen, Mowbray and BybeeCohen et al, 1993; Reference BootsMiller, Ribisl and MowbrayBootsMiller et al, 1998; Reference NishimotoNishimoto, 1998).
Modes of communication
Letters and e-mails should adhere to the usual rules of written professional correspondence. Some participants (patients and health professionals) respond positively if a letterhead from a medical charity or university is used and personalised with an original signature or a handwritten note. Use of colour (ink, letter paper, enclosed fliers or even envelopes) has been shown to increase response rates. Including a stamped addressed reply envelope and not using a franking machine and computer-generated address labels are also beneficial (Reference Sloan, Kreiger and JamesSloan et al, 1997; Reference Edwards, Roberts and ClarkeEdwards et al, 2002). Establishing contact by telephone usually requires several attempts at different times and on different days. Where postal questionnaires have failed, telephone interviews can increase the response rate by a further 30%, although telephone responses are presumably more susceptible to a social desirability response bias and thus may introduce a mode error (Reference Sibbald, Addington-Hall and BrennemanSibbald et al, 1994; Reference Ribisl, Walton and MowbrayRibisl et al, 1996; Reference BootsMiller, Ribisl and MowbrayBootsMiller et al, 1998; Reference Fischer, Dornelas and GoetheFischer et al, 2001).
The researcher's personal perspective
Recruiting participants can be an emotionally turbulent and maturing experience for a junior researcher. More personal issues are considered below, together with potential solutions.
Team membership
Recruitment is seldom a solitary exercise. The researcher is usually part of a multi-disciplinary team of researchers headed by a principal investigator, who is generally the grant holder and may be a senior lecturer, professor or consultant. Other members of the team include junior doctors, psychologists, epidemiologists, sociologists and nurses. Differences in expertise, skills, expectations and working styles can affect the individual's role within the team, with varying consequences. However, the team may sometimes consist of only two members: the junior researcher responsible for recruitment and the principal investigator (Reference Young and DombrowskiYoung & Dombrowski, 1989).
Compromised autonomy and emotions
In a clinical trial, team members responsible for recruiting are often employed after the projected recruitment targets have been decided by the principal investigator or the trial sponsors. This prevents any negotiation by junior researchers. Often, it is not clear from the outset of the study which recruitment strategy is going to work. Together, these issues can leave the junior researcher feeling powerless and uncertain as to how to proceed. In multi-centre studies, where recruitment is competitive, comparison of rates of recruitment creates additional pressure on the team to perform better. When recruitment rates fall behind target, junior researchers should beware that some principal investigators use negative pressure to ‘enhance’ motivation.
More desirable motivating factors include the opportunity to acquire research skills and experience, to learn how to work in a team and promises of attendance at conferences and of having work published at the end of the study. These should be borne in mind not only at the beginning of the study but also during the difficult times when enthusiasm wanes. However, as time progresses, the initial enthusiasm for recruitment gradually fades. In the face of the harsh realities of research, such as slow recruitment, negative emotions often become dominant. Researchers may experience feelings of despair, self-blame, guilt, a sense of failure, worthlessness, loneliness, frustration and sub-clinical depression; sometimes even paranoia sets in.
Solutions
It is important to maintain a sense of proportion and objectivity in the face of adversity. This can be achieved by talking to supportive members of the research team as well as to senior colleagues or peers who can give objective advice based on their own research experience. During these sessions, it is important to identify your strengths and weaknesses. Failure to do this can lead to personal distress and have unknown effects on the validity of the research data. It can also contribute to increased costs resulting from burnout (Reference Cohen, Mowbray and BybeeCohen et al, 1993). You need to be flexible, proactive and creative in finding solutions to problems that had not been anticipated. For example, when working in a catchment area which is overresearched, you should be aware of competition from other researchers interested in the same participant group. Such colleagues may be hostile and should be dealt with diplomatically. The usual solution is to move to another hospital or catchment area where there is less competition and where staff are more receptive to research. Learning how to recruit participants is a significant milestone in anyone's career. If achieved, self-knowledge, enhanced skills and the ability to embrace uncertainty with courage are more than worthy rewards.
Summary
There are many aspects that the diligent researcher should consider when attempting to maximise participant recruitment and avoid subsequent attrition. These include the following.
Early considerations
Several aspects of the design and method (e.g. participant exclusion criteria and the required duration of active participation) are necessarily decided at an early stage in the research process. Remember that such decisions will affect actual participant recruitment.
The participant's perspective
Try to be amenable and accommodating with potential participants. Do not expect them to travel long distances to see you.
Close collaboration with colleagues
Optimise your working relationship with colleagues by regular face-to-face contact. Be approachable, easily contactable and amenable.
Generic skills
Do not underestimate the importance of personal generic skills. Assertive tracking of potential participants requires thorough, methodical and timely organisation. Similarly, it is essential to have a range of good interpersonal and communication skills, using a variety of different methods (e.g. the written word, the telephone and visual presentations).
Feedback
Lastly, we strongly advocate that researchers should always attempt to present their findings to all colleagues involved in the recruitment phase as well as to the participants. This aspect is often overlooked and can have profound adverse consequences on future attempts to recruit participants in the region.
Multiple choice questions
-
1 Recruitment strategies:
-
a aim to enlist a representative sample of the target population for a research study
-
b involve establishing communication between recruiting staff and potential participants
-
c are seldom used in psychiatric research
-
d aim to overcome selection bias
-
e are adequately reported in psychiatric research literature.
-
-
2 To enhance recruitment rates, the assessment should ideally be:
-
a repetitive
-
b relevant
-
c complicated
-
d lengthy
-
e valid.
-
-
3 Participants are more likely to participate in research as a result of:
-
a inconvenience
-
b boredom
-
c personal contact
-
d offered incentive
-
e altruistic intent.
-
-
4 For a successful recruitment strategy, recruiting staff should:
-
a have good interpersonal skills
-
b work on a voluntary basis
-
c be replaced every 2 months
-
d use only one method of communication
-
e receive appropriate training and regular supervision.
-
-
5 The following are associated with increasing recruitment rates for postal questionnaires:
-
a use of colour in correspondence
-
b computer-generated subject address labels
-
c providing a stamped addressed return envelope
-
d use of a franking machine
-
e assertive tracking.
-
MCQ answers
| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | T | a | F | a | F | a | T | a | T |
| b | T | b | T | b | F | b | F | b | F |
| c | F | c | F | c | T | c | F | c | T |
| d | T | d | F | d | T | d | F | d | F |
| e | F | e | T | e | T | e | T | e | T |





eLetters
No eLetters have been published for this article.