Introduction
Background
Trauma carries a significant risk of morbidity and mortality, frequently due to hemorrhage. Reference Britt, Weireter, Riblet, Asensio and Maull1,Reference Eastridge, Mabry and Seguin2 Early and accurate identification of those patients at risk for deterioration is among the greatest challenges facing clinicians managing this population. Prognostication is important not only to optimize care for each individual patient, but also to inform planning and resource utilization in the event of mass-casualty incidents. Reference Schauer, April, Simon, Maddry, Carter and Delorenzo3
Existing literature has attempted to correlate multiple patient factors or initial variables with trauma patient outcomes. Much of this literature focuses on injury patterns and severity as measured by the injury severity score (ISS). Reference Inci, Ozçelik, Taçyildiz, Nizam, Eren and Ozgen4,Reference Schauer, April and Naylor5 Another focus of these studies is the impact of medical interventions on patient survival. 6,Reference Schauer, Naylor and Chow7 Equally important is proactive identification of patients at increased risk of deterioration. Vital signs offer a readily obtainable physiologic tool for early prognostication.
Past studies have focused upon systolic blood pressure (SBP) and pulse as the ideal signs to provide prognostic information in trauma patients. Specifically, the conventional definition of hypotension in trauma patients has been 90mmHg, 8,Reference Bickell, Wall and Pepe9 a value which some physiologic studies find to correspond to the presence of a radial pulse. Reference Odagiri, Morita, Yamauchi, Imai, Tei and Inoue10 However, registry data suggest the SBP values at which a radial pulse is detectable are more variable. Reference Naylor, Fisher, April and Schauer11 Moreover, recent studies in both civilian and military settings indicate that SBP values associated with short-term mortality among trauma patients are higher than the traditional threshold, spanning from 100-110 mm Hg, Reference Eastridge, Salinas and McManus12,Reference Eastridge, Salinas, Wade and Blackbourne13 suggesting that the presence of a radial pulse does not obviate the need to measure vital signs. The shock index (SI) is a clinical calculation which incorporates both measures by dividing heart rate by SBP (SI) or mean arterial pressure (modified SI); SI values more than 0.9 and modified SI values less than 0.7 or greater than 1.3 are both associated with increased mortality. Reference Cannon, Braxton, Kling-Smith, Mahnken, Carlton and Moncure14,Reference Singh, Ali, Agarwal and Srivastava15
Goal of this Study
This goal of this study was to identify the vital sign thresholds associated with death among trauma patients using the Trauma Quality Improvement Program (TQIP) database. The intended output was to determine the optimal thresholds predictive of 24-hour mortality for SBP, heart rate, and SI. The secondary aim was to identify these thresholds for elderly patients (70 or greater years of age).
Methods
Study Design and Setting
This study utilized data from TQIP. The American College of Surgeons (ACS; Chicago, Illinois USA) has maintained TQIP since 2008. The database has mandatory data collection for Level 1 trauma centers and collects data from other centers that do not meet Level 1 criteria. Reference Blackmore, Leonard, Madayag and Bourg16 The goals of the program are to provide data to aid trauma centers, to standardize trauma care, to develop local and national quality improvement in trauma care, and to provide data needed for best trauma care practices guidelines. There are over 700 participating centers where trained registrars enter data for trauma visits that meet entry criteria. Reference Newgard, Fildes and Wu17 The Colorado Multiple Institutional Review Board (COMIRB; Aurora, Colorado USA) reviewed protocol COMIRB-2023-1732 and determined it met the definition of research not involving human subjects and therefore was exempt from IRB oversight.
Data Collection
This study comprised a retrospective review of the prospectively collected data from the TQIP registry. Only entries from 2019-2020 were included because TQIP stopped collecting Emergency Medical Service (EMS) vital sign data after 2020. Furthermore, only subjects with a documented age of ≥15 years were included. Patients who underwent interfacility transfers or had no signs of life on arrival (eg, vital sign was documented as zero) were excluded. Data collected included patient demographics including age and sex. Initial vital sign data from both EMS and emergency department (ED) settings were collected. Vital signs collected include SBP, pulse, respiratory rate, and SI (ratio of pulse to SBP). The primary outcome measure was 24-hour survival.
Data Analysis
Descriptive statistics were used to characterize the study population. Continuous variables were presented as means and 95% confidence intervals (95% CI) with t-test comparisons. Non-parametric continuous variables and ordinal variables were presented as medians and interquartile ranges (IQR) with Wilcoxon rank sum comparisons. Nominal variables were presented as percentages and numbers with chi square or Fisher’s exact tests depending on the expected cell count for comparison.
Logistic regression models were constructed with vital signs as the independent variables and death within 24 hours as the dependent variable. Youden’s index was used to determine the optimal vital sign threshold described in prior analyses along with the 90% sensitivity and 90% specificity bounds. Reference Schauer, April and Fisher18,Reference Moulton, Schauer and Borgman19 The area under the receiver operator curve (AUROC) was used for each of these thresholds. A planned sub-group analysis examined subjects 70 and older. All statistical analysis was performed using Microsoft Excel (version 365; Microsoft Corp.; Redmond, Washington USA) and JMP Statistical Discovery from SAS (version 17; SAS Institute; Cary, North Carolina USA).
Results
There were 1,439,221 subjects in the 2019-2020 datasets that met inclusion for this analysis with <0.1% (10,270) who died within 24 hours. Non-survivors were younger and more likely to be male than survivors. Non-survivors also had higher median ISS (24 versus 9; Table 1).
Table 1. Overall Subject Characteristics
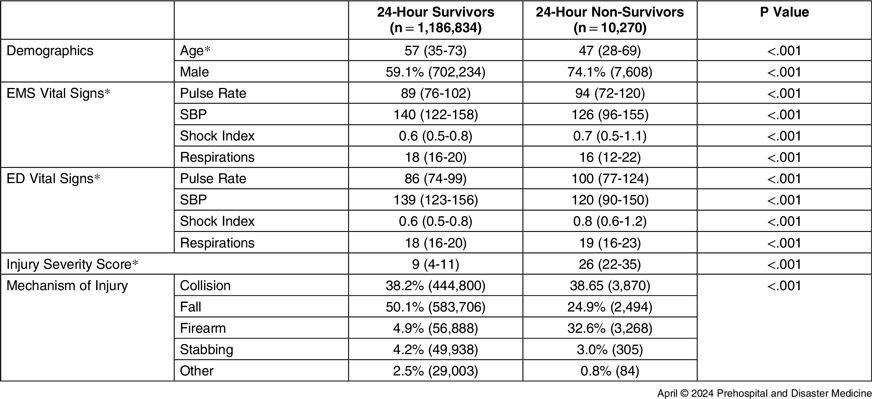
Abbreviations: EMS, Emergency Medical Services; ED, emergency department; SBP, systolic blood pressure.
* Presented as median and interquartile range, compared using Wilcoxon rank sum.
Systolic blood pressure was markedly lower among non-survivors as compared to survivors. Median EMS SBP was 126 (IQR 96-155) among non-survivors versus 140 (IQR 122-158) among survivors. Median ED SBP was 120 (IQR 90-150) mmHg among non-survivors versus 139 (IQR 123-156) mmHg among survivors (Table 1).
All vital signs assessed were only modestly predictive of 24-hour mortality. Among the EMS vital signs, the systolic pressure was most predictive with an optimal threshold of 110 and a 90% specificity of 104 with a 90% sensitivity of 182. Among the ED vital signs, SI was most predictive with an optimal threshold of 0.9 with a 90% specificity of 1.0 and a 90% sensitivity of 0.5 (Table 2).
Table 2. Vital Sign Thresholds and Characteristics

Abbreviations: AUROC, area under the receiver operator curves; EMS, Emergency Medical Services; SBP, systolic blood pressure; SI, shock index.
The results for the sub-analysis of patients ≥70 years of age was generally comparable in terms of predictive ability, though with slightly higher SBP and slightly lower pulse thresholds. Shock index was most predictive among both the EMS and ED vital signs (Table 3).
Table 3. Vital Sign Thresholds and Characteristics for Elderly Patients

Abbreviations: AUROC, area under the receiver operator curves; EMS, Emergency Medical Services; SBP, systolic blood pressure; SI, shock index.
Discussion
The objective of this study was to identify clear and readily obtainable prognostic indicators of poor outcomes among trauma patients. These TQIP data of EMS and ED vital signs offer thresholds predictive of mortality among trauma patients. The SBP thresholds ranged from 110-112mmHg among all patients and 116-121mmHg among elderly patients. The heart rate thresholds ranged from 107-110bpm among all patients and 95-100bpm for elderly patients. These findings suggest lower thresholds than those traditionally considered to indicate heightened risk of short-term mortality. That said, all these thresholds showed only a modest ability to predict mortality with AUROC values ranging from 54% to 69%. Early identification of patients at high risk of mortality may empower clinicians to optimize care in these situations. The intent of this analysis was to provide triggers for consideration of aggressive diagnostic and therapeutic interventions as early as possible to improve outcomes for these critically ill patients. However, all vital-sign-based measurements lacked robust sensitivity and specificity, suggesting that other modalities of assessing shock may be needed. Reference Schauer, April and Arana20,Reference Schauer, April, Arana, Long and Maddry21
The SBP thresholds identified by this study to be most predictive of mortality are markedly higher than the threshold of 90mmHg conventionally cited as associated with death in Advanced Trauma Life Support courses. 8 That said, multiple original research studies using civilian and military registry data report higher values associated with mortality. The work by Eastridge, et al using trauma registry data for military operations from 2002 to 2009 identified 100mmHg as the SBP threshold most predictive of mortality. Reference Eastridge, Salinas, Wade and Blackbourne13 Previous work using the Department of Defense Trauma Registry (DODTR; US Department of Defense; Washington, DC USA) found results even more closely aligned with the findings of the present analysis: a SBP threshold of 112mmHg was most predictive of short-term mortality. Similarly, a study of civilian trauma patients also by Eastridge, et al found a threshold predictive of short-term mortality of 110mmHg. Reference Eastridge, Salinas and McManus12 This study’s threshold may reflect a generally less critically injured patient population given its inclusion of data from a more contemporary time period which also encompassed the coronavirus disease 2019/COVID-19 pandemic during which there were reported reductions in the number of critically injured trauma patients in some hospitals. Reference April, Becker, Fisher, Naylor and Schauer22 These deviations from the traditional thresholds may be due to the underlying adrenaline surge that happens after trauma compared to other causes of shock.
Historically, the prevailing thought has been that the physical examination finding of a missing radial pulse aligns with a SBP less than 90mmHg. Reference Odagiri, Morita, Yamauchi, Imai, Tei and Inoue10 Even if true, this study’s findings reinforce the emerging consensus that absence of a radial pulse is likely a late finding with inadequate sensitivity to effectively identify patients at risk of mortality as blood pressure levels portend heightened risk of mortality far before the radial pulse reliably vanishes. In fact, recent data evaluating paired radial pulse strength characterizations and SBP measurements within the DODTR demonstrate that radial pulse strength is not a reliable indicator of hypotension. Naylor, et al found that over 50% (n = 615) of casualties in the DODTR with an SBP <80 mm Hg had a strong radial pulse. Reference Naylor, Fisher, April and Schauer11 Pulse rate may also be particularly misleading among patients on medications such as beta blockers that can suppress patient ability to mount a tachycardic response. In the absence of plethysmography to precisely measure blood pressure in the prehospital setting, any perceived weakness or absence of the radial pulse should be considered cause for grave concern as this is likely a late finding and the patient is at high risk of death. Such patients should undergo aggressive diagnostic and therapeutic interventions.
Limited existing data speak to the heart rate and SI thresholds associated with death. Reference Eastridge, Owsley and Sebesta23,Reference Sorensen, April, Fisher and Schauer24 This study’s results indicate that while SI has broadly equivalent prognostic value compared to SBP, pulse has significantly less. Of course, pulse carries the advantage of generally requiring no equipment to measure. This makes it particularly valuable to EMS providers. Nevertheless, these personnel must understand the limited prognostic value of this information. In the elderly, SI has modestly higher accuracy as measured by sensitivity and specificity, compared to SBP or heart rate alone. This finding highlights the potential for this measure to provide added prognostic value in this vulnerable patient population. Moreover, the ability to calculate this from routinely used vital sign data makes it particular enticing until other novel methods for assessing shock are developed.
Limitations
This study has several limitations. It is a retrospective analysis of a registry. Such data can be inaccurate secondary to errors in data entry. Reference Nissley, Rodriguez, April, Schauer and Stevens25 Furthermore, the TQIP registry includes only patients with identified traumatic injuries, therefore these vital sign parameter risk factors for mortality may not apply to patients who receive trauma team activations for concern for possible traumatic injury but do not ultimately have significant traumatic injuries. Moreover, the modest accuracies for the clinical measurements studied bely the limited utility of using these data in isolation to drive trauma activation decisions. Additionally, this study lacks information on pediatric vital sign thresholds predictive of adverse outcomes. Relatively little work exists examining the correlation between prehospital and ED vital signs and injury patterns with pediatric trauma patient outcomes. Reference Cuenca, Borgman, April, Fisher and Schauer26,Reference Gale, Borgman, April and Schauer27 The literature would benefit from future studies specifically examining this patient population. Reference Naylor, April, Roper, Hill, Clark and Schauer28,Reference Schauer, Wheeler and April29 Strengths of this study include the size of the study population as well as the general relevance of results to the broader adult trauma patient population.
Conclusions
Of the vital signs examined, SBP and SI offered the best predictor of mortality among trauma patients. Patients with a SBP less than 110-112 mm Hg among all patients and between 116-121 mm Hg among patients ≥70 years are at high risk of mortality. These values are significantly higher than the traditional 90mmHg threshold. Moreover, the TQIP dataset highlights the need for better methods to guide resuscitation as vital sign measurements have limited accuracy in predicting subsequent mortality.
Conflicts of interest/disclaimer
The views expressed in this article are those of the authors and do not reflect the official policy or position of the US Army Medical Department, Department of the Army, Department of Defense, or the US Government. The authors declare no conflicts of interest.
Acknowledgments
The authors thank the Trauma Quality Improvement Program (TQIP) for making this research possible.






