Introduction
International and UK health policy have developed standards stating that people with diabetes should be empowered and supported to participate in decision-making and self-management to optimise the control of blood glucose, blood pressure, and other risk factors for developing the complications of diabetes (Department of Health, 2002; 2005; International Diabetes Federation, 2003). This marks a shift in the treatment of those with chronic diseases away from health-care professional management towards ensuring that patients are enabled to self-manage their health effectively and engage in active partnership with health professionals. One of the dominant concepts in the literature on supporting self-management is that of self-efficacy (Day et al., Reference Day, Bodmer and Dunn1997; Norris et al., Reference Norris, Engelgau and Venkat Narayan2001; Guevara et al., Reference Guevara, Wolf, Grum and Clark2003).
Perceived self-efficacy is a reliable predictor of behaviour initiation (Bandura, Reference Bandura1977; Gillis, Reference Gillis1993). It demonstrates its value as the cornerstone of effective chronic disease self-management through its increasing use as a self-management research outcome measure (Lorig et al., Reference Lorig, Sobel, Stewart, Brown, Bandura, Ritter, Gonzalez, Laurent and Holman1999; Farmer et al., Reference Farmer, Wade, French, Goyder, Kinmonth and Neil2005; Sturt et al., Reference Sturt, Hearnshaw, Farmer, Dale and Eldridge2006a; Reference Sturt, Taylor, Docherty, Dale and Louise2006b; Davies et al., Reference Davies, Heller, Skinner, Campbell, Carey, Cradock, Dallosso, Daly, Doherty, Eaton, Fox, Oliver, Rantell, Rayman and Khunti2008). Perceived self-efficacy is defined as an individual’s perceptions or beliefs about their capabilities to undertake certain activities (Bandura, Reference Bandura1994). It influences how they think, feel, become motivated and behave. People with strong perceptions of their personal efficacy approach difficult tasks as challenges to be mastered; they set themselves challenging goals and maintain strong commitment to them. In the face of failure they increase their efforts and rapidly recover their self-efficacy after setbacks. This efficacious outlook produces personal accomplishments, reduces stress, and lowers vulnerability to depression. In contrast, people who doubt their capabilities avoid difficult tasks, they have low aspirations and weak commitment to their chosen goals. When faced with difficult tasks, they dwell on their personal deficiencies and on the obstacles and their efforts weaken in the face of these challenges. Individuals with low perceptions of efficacy are vulnerable to stress and depression (Bandura, Reference Bandura1994). Self-efficacy is often communicated to lay audiences, for example, in research measures, as ‘degree of confidence’ although this is not technically accurate and Bandura does describe important differences between confidence and self-efficacy in his web site (http://www.des.emory.edu/mfp/self-efficacy.html).
Self-efficacy is supported in four ways (in order of influence): personal mastery experiences, vicarious (or peer) experiences, emotional state, and verbal encouragement and it offers a framework for enabling health-care professionals to guide people towards experiences that will strengthen their self-efficacy (Bandura, Reference Bandura1977). Measurement of perceived self-efficacy is behaviour-specific and measurement predicts the likelihood that an individual will engage in a behaviour, the degree to which they will persist and overcome obstacles, and their ultimate success in maintaining behaviour in the longer term (Bandura, Reference Bandura1977; Sentcal et al., Reference Sentcal, Nouwen and White2000; Sniehotta et al., Reference Sniehotta, Scholzu and Schwarzer2005). However, measurement is complicated by the lack of generalisability of self-efficacy between types of behaviour, for example, stopping smoking and increasing physical activity. Attempts to develop measures across different behaviour types have limited usefulness (Bandura, Reference Bandura1997; Reference Bandura2006). Scales to measure perceived self-efficacy must, therefore, be highly specific to the behaviour or activity of interest, such as aspects of self-management in diabetes.
Diabetes is a complex metabolic condition requiring high levels of self-efficacy to perform the many facets of self-management required for blood glucose control, and hence prevention of complications. Diabetes self-efficacy measurement scales currently available provide good psychometric validity for the measurement of psychosocial aspects of living with diabetes, of self-management for people with type 1 diabetes, and for type 2 diabetes self-management for Dutch/US and Australian populations (Bijl et al., Reference Bijl, Poelgeest-Eeltink and Shortridge-Baggett1999; Anderson et al., Reference Anderson, Funnell, Fitzgerald and Marrero2000; Van Der Ven et al., Reference Van Der Ven, Weinger, Yi, Pouwer, Ader, Van Der Ploeg and Snoek2003; McDowell et al., Reference McDowell, Courtney, Edwards and Shortridge-Bagget2005). The Dutch/US scale assesses behavioural aspects of type 2 diabetes self-management and had the potential to offer a strongly aligned outcome measure for the type 2 diabetes patient education and self-management intervention studies that we were designing and which were strongly influenced by self-efficacy theory. Scale items assess self-efficacy for performing a range of self-management activities that will influence blood glucose control including managing healthy eating and monitoring skin integrity of the feet (Bijl et al., Reference Bijl, Poelgeest-Eeltink and Shortridge-Baggett1999). A scale for measuring perceived self-efficacy, validated for use with a UK population, focusing on diabetes-specific self-management activities would offer a tool for researchers and clinicians to evaluate progress towards meeting the UK Diabetes National Service Framework standards.
The aim of this paper is to present the evaluation of aspects of the validity and reliability of an adapted version of the Dutch/US diabetes management self-efficacy scale (DMSES) as a measure of perceived self-efficacy in relation to the management of diabetes in patients with type 2 diabetes, in the UK population.
Methods
Adaptation of the Dutch/US DMSES
The 20-item Dutch/US DMSES measures the individual’s efficacy expectations for engaging in 20 type 2 diabetes self-management activities, for example, taking daily exercise, keeping to a healthy eating plan when away from home (Bijl et al., Reference Bijl, Poelgeest-Eeltink and Shortridge-Baggett1999). The scale is scored according to a 1–5 point numerical scale indicating the level of efficacy expectation the respondent has for each item with higher scores indicating greater levels of self-efficacy. The Dutch/US evaluation of the DMSES covered content and construct validity, internal consistency, and temporal stability. That process, involving a panel of experts within diabetes and self-efficacy, resulted in the reduction of an original 42-item scale to 20 items. The DMSES was translated from Dutch to US English as part of the scale development work. The construct validity of the scale was demonstrated through the findings of a positive relationship in a second, US-based study, testing the relationship between the self-efficacy scores of individuals living with diabetes and the self-efficacy scores of their significant other for supporting and assisting them in the 20 self-management activities, for example, ‘How confident are you that you could support and assist your significant other in choosing the correct foods’ (Shortridge-Bagget and van der Bijl, Reference Shortridge-Bagget and van der Bijl2002).
Assessing face validity
Face validation of a DMSES for the UK started by consulting with the Warwick Diabetes Research & Education User Group (WDREUG), a lay advisory group of 10–12 people living with diabetes, during two meetings over six months (Lindenmeyer et al., Reference Lindenmeyer, Hearnshaw and Sturt2007). The WDREUG provided advice to ensure appropriate use of vocabulary (eg, blood glucose monitoring) and concepts (eg, confidence), which resulted in changes made to items, for example, diabetic diet was replaced by healthy eating pattern. Following WDREUG consultation and with regard to the literature (Donaldson, Reference Donaldson2003) the stem phrase ‘I am confident that …’ was used to precede each item in the 20-item DMSES UK. The 20 UK items are described in Table 1.
Table 1 Initial version of the DMSES UK with 20 items
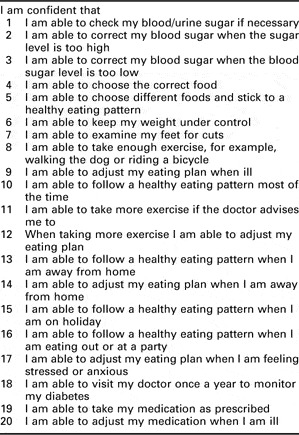
DMSES=diabetes management self-efficacy scale.
The five-point response scale used in the Dutch/US DMSES has a poorer predictive capacity than a 0 to 10-point scale (Pajares et al., Reference Pajares, Hartley and Valiante2001). The DMSES UK incorporated an 11-point 0–10 scale reflecting Bandura’s thesis (Bandura, Reference Bandura2006). The WDREUG advised on the anchor point terms used in the scale, which were as follows; 0–1 Cannot do at all, 4/5 Maybe yes maybe no, 9/10 Certain can do. The centre anchor point recommended by Bandura is moderately certain can do. The WDREUG felt this was ambiguous and using Maybe yes, maybe no enabled a responder to judge their certainty based on a collective experience of their perceived confidence for a particular behaviour, indicating that some days they might be more confident than others. The scale instructions were determined with reference to Bandura’s guidance on the construction of self-efficacy scales and with regard to the opinions of the users (Bandura, Reference Bandura1997). The scale was intended for self-completion, in private, so clear instructions were an important aspect of the scale. The Flesch reading ease score (tool available in Microsoft Office Word) for the DMSES UK was assessed as 82.9% or grade 2.6 equivalent to a reading age of seven to eight years, and therefore appropriate. This process of consultation in adapting the scale established high-face validity.
Assessing content validity
Once face validity was established we amended the DMSES and content validity was assessed with both people living with type 2 diabetes and with diabetes health-care professionals. Thirty individuals attending two lay diabetes events in 2003, volunteered to complete the 20-item DMSES UK with the available support of a researcher (JS/HH). During completion the volunteers with type 2 diabetes identified duplications and ambiguities in the scale, which were recorded in field notes. This process confirmed the views of the WDREUG.
Health professionals undergoing continuing professional development in diabetes care at the Warwick Medical School were also consulted on the validity of the constructs. Group discussions were held with three cohorts of professionals, approximately 20 people per cohort. This revealed ambiguity around a number of items and some duplication. The professional and lay consultation led to the removal of five items from the DMSES UK. Two items were ambiguous (items 8,18) and three involved duplicate items or elements of items (items 5,14,15) (Table 2). The health professionals confirmed that the scale content was sufficiently broad to cover the salient and challenging aspects of self-managing type 2 diabetes giving high content validity. The face and content validity of the DMSES UK was determined to be of sufficient strength for the revised 15 item scale to undergo further psychometric evaluation.
Table 2 Redundant items from initial 20-item DMSES UK

DMSES=diabetes management self-efficacy scale.
Diabetes manual randomised controlled trial (RCT) and participants
Evaluation of the criterion and construct validity and the reliability of the DMSES UK was undertaken using data from the cluster randomised trial of the Diabetes Manual, a structured education programme for type 2 diabetes undertaken from 2005 to 2007 (Sturt et al., Reference Sturt, Hearnshaw, Farmer, Dale and Eldridge2006a; Reference Sturt, Taylor, Docherty, Dale and Louise2006b; Reference Sturt, Whitlock, Fox, Hearnshaw, Farmer, Wakelin, Eldridge, Griffiths and Dale2008). RCT participants were 245 people with type 2 diabetes resident across the West Midlands, UK. All participants were recruited from primary care and randomised to receive the diabetes manual intervention or a six-month deferred intervention. The diabetes manual is a self-management and structured education programme to be used by practice nurses and patients on a one to one basis. It consists of two-day facilitator training for the nurse, a patient workbook for recommended completion over three months, a frequently asked questions CD, a relaxation CD, and three nurse-delivered telephone support calls. The aim of the intervention is to strengthen the patient’s self-efficacy by developing skills and confidence in managing their diabetes, quickly, and progressively. The intervention is theoretically underpinned by self-efficacy theory (Bandura, Reference Bandura1977).
RCT outcome measures
Baseline data were collected from 245 participants before randomisation and consisted of HbA1c as the primary outcome and completion of a six-page questionnaire including the 15 item DMSES UK, the 20 item problem areas in diabetes (PAID) scale (Polonsky et al., Reference Polonsky, Anderson, Lohrer, Welch, Jacobson, Aponte and Schwartz1995), and 10 demographic questions. The PAID scale is a 20-item measure of diabetes-specific emotional distress; with a maximum score of 100 and higher scores indicting greater emotional distress. The maximum score on the DMSES UK is 150 with higher scores indicating higher self-efficacy. Since higher self-efficacy is related to lower emotional distress (Fisher et al., Reference Fisher, Thorpe, Devellis and Devellis2007) a strong correlation between low PAID scores (a gold standard), indicating low distress, and high scores on the DMSES UK, indicating high self-efficacy, would indicate criterion validity. Two hundred and thirty-two (95%) randomised participants completed some elements of the questionnaire, of whom 175 (71%) participants responded to all of the DMSES UK questions. These 175 participants form the sample used for this psychometric evaluation of the DMSES UK.
At the six-month follow-up for the trial, the six-page questionnaire was completed again by participants. Within four weeks of that, all control group patients were sent a repeat questionnaire. This group was chosen for the test-retest because they were awaiting the deferred intervention and could be expected to complete the repeat questionnaire. The repeat questionnaire was returned by 67 participants.
Results
Patient characteristics
The demographic and clinical characteristics of the participants who completed the DMSES UK questions at baseline are summarised in Table 3.
Table 3 Characteristics of participants

DMSES=diabetes management self-efficacy scale; PAID=problem areas in diabetes.
Principal component analysis
Principal components analysis was used to investigate whether DMSES should be considered as several subscales or as one general factor. The item coefficients for the first principal component varied from 0.38 to 0.80 demonstrating that it was indeed a weighted average of all questions, rather than being dominated by a small subset of questions. The first principal component accounted for 41% of the total variance. The second component accounted for only 11% of the variance and the third component accounted for 10%. The scree plot (Figure 1) indicates that one factor was important, confirmed as a weighted average, supporting the reporting of DMSES as one overall score.

Figure 1 Scree plot for baseline diabetes management self-efficacy scale (DMSES UK; n = 175)
Internal reliability and internal consistency
The correlation coefficients between item scores and total scores were all >0.30 (minimum = 0.34, maximum = 0.71). Internal consistency was demonstrated by a Cronbach’s alpha of 0.89 over all 15 items. Internal reliability of DMSES UK was therefore deemed to be acceptable.
Criterion validity
A Pearson’s correlation coefficient of −0.46, P < 0.0001 was found indicating a negative correlation between DMSES scores and PAID scores. This demonstrates the criterion validity of the DMSES, since the PAID is a well established and validated gold standard scale (Fisher et al., Reference Fisher, Thorpe, Devellis and Devellis2007).
Construct validity
A negative correlation between DMSES scores and HbA1c (Pearson’s correlation coefficient −0.21, P = 0.002) was found. Since higher self-efficacy should lead to greater self-care behaviours resulting in lower blood glucose levels and ultimately lower HbA1c levels (Fisher et al., Reference Fisher, Thorpe, Devellis and Devellis2007), this demonstrates the construct validity of the DMSES.
Test-retest reliability
Analysis of test-retest data from 67 participants, who completed the DMSES UK questionnaire twice within a four-week time period, produced an intra-class correlation of 0.77. This demonstrates the reliability over time of the DMSES UK.
Discussion
The results from this evaluation of aspects of the validity and reliability of DMSES UK, demonstrate that the scale has good internal reliability and high internal consistency. DMSES UK score was found to be negatively correlated with both PAID score and HbA1c. These findings demonstrate the criterion validity and the construct validity of DMSES UK. Acceptable test-retest reliability was demonstrated by an intra-class correlation coefficient of 0.77.
The data were drawn from an intervention study in which participants consented to a programme of self-management education with some burden attached. This may represent a different population from one who were just asked to complete a single questionnaire on two occasions. The trial participants were not found to differ from the eligible participants on any variable although the low 18.5% RCT response rate indicates that acceptance of burden may have been a distinguishing feature of our participants (Sturt et al., Reference Sturt, Whitlock, Fox, Hearnshaw, Farmer, Wakelin, Eldridge, Griffiths and Dale2008). Our participants also had a mean diabetes distress level of 21 as measured by the PAID scale at baseline. This compares slightly lower to typical diabetes out-patient populations in the USA and Germany where scores in the range of 20–30 were detected (Polonsky et al., Reference Polonsky, Anderson, Lohrer, Welch, Jacobson, Aponte and Schwartz1995; Welch et al., Reference Welch, Weinger, Anderson and Polonsky2003). These study sample factors may distort the validity of the findings were it used on a population not involved in an intervention trial. One further limitation may be the anchor points of ‘maybe yes, maybe no’ which may confound moderate efficacy with uncertainty. Given the observed inter-items and inter-scale correlations, we expect any such confounding to have been small.
A validation and psychometric evaluation of the 20 item DMSES in an Australian population also reported some probable redundancy (McDowell et al., Reference McDowell, Courtney, Edwards and Shortridge-Bagget2005). The authors identified inter-item correlations between items 2/3, 8/11, 13/14, 13/15, and 14/15, which map well onto the items found to be redundant in the DMSES UK. The DMSES UK is the first national validation and psychometric evaluation of the DMSES to have been used as an outcome measure in RCTs of self-management interventions (Sturt et al., Reference Sturt, Whitlock, Fox, Hearnshaw, Farmer, Wakelin, Eldridge, Griffiths and Dale2008; Dale et al., Reference Dale, Caramlau, Sturt, Friede and Walker2009). The DMSES UK has undergone face validation for use in audio-delivery and symbol self-completion for Bangladeshi and Pakistani populations’ resident within the UK whose main language has no written form (Lloyd et al., Reference Lloyd, Sturt, Johnson, Mughal, Collins and Barnett2008). The psychometric evaluation of the DMSES UK now enables confident use of the Sylheti and Mirpuri DMSES UK scales in diabetes self-management intervention studies for these South Asian populations vulnerable to diabetes and its consequences.
Conclusions
The DMSES UK is available as a measure of diabetes management self-efficacy for both clinical and research use. The predictive reliability of self-efficacy means that the DMSES UK can be used to enable more effective targeting of self-management interventions and clinical resources to the individual patient. It has strong face validity and is a reliable scale for use as an outcome measure in research studies. Future research could evaluate the predictive capacity of the DMSES UK, in particular sub-groups of people with type 2 diabetes.
Clinicians have a tool available, which has strong face validity, with both clinicians and patients, to help identify in which areas of diabetes self-management a patient’s self-efficacy is more or less secure. This will enable clinicians to coach the patients into goal choice areas, where new behavioural challenges are more likely to be successful. Early success in new behavioural challenges will lead to strengthening of self-efficacy in more challenging goals over time.
Acknowledgements
The authors would like to thank the WDREUG, the people with type 2 diabetes and the health care professionals who have participated in this study. Thanks are due to Professor Shortridge-Baggett and Dr van der Bijl for their collaborative engagement with this UK validation study. The study was funded by Diabetes UK and the UK Department of Health NCCRCD programme.






