Anaemia, a condition in which the number of erythrocytes is insufficient to meet physiological needs, is defined as Hb concentration levels lower than a specific threshold(1). Symptoms of anaemia include fatigue, weakness, reduced cognitive capacity and low productivity(Reference Brunner and Wuillemin2–4). Previous studies have suggested that Hb distribution varies with age, sex, lifestyle, ethnic origin, socio-economic status and region(Reference McLean, Cogswell and Egli5–7). Compelling evidence has suggested that anaemia is associated with major consequences for human health, as well as a significant social and economic burden(Reference Disease, Injury and Prevalence8,Reference Cappellini and Motta9) .
Currently, anaemia is a global public health problem affecting both developing and developed countries, with developing countries accounting for more than 89 % of the global burden of anaemia(Reference Adamu, Crampin and Kayuni10–Reference Halawi, Moukhadder and Taher12). It has serious health implications, causing both increasing morbidity and mortality due to the reduced oxygen-carrying capacity(Reference Culleton, Manns and Zhang13,Reference Zakai, Katz and Hirsch14) . Remarkably, anaemia affects 1·62 billion people globally, and specific subgroups are at higher risk of anaemia, such as reproductive-age women (29 % for anaemia and 1·1 % for severe anaemia)(Reference Kassebaum and Collaborators11,Reference Stevens, Finucane and De-Regil15,Reference Baig-Ansari, Badruddin and Karmaliani16) . Reproductive-age women who live in under-resourced environments are particularly vulnerable to anaemia, leaving themselves and their offspring ill-prepared to meet the increasing nutritional demand during pregnancy(Reference Lander, Hambidge and Westcott17). Anaemia during pregnancy has multiple long-term adverse effects on mother and offspring health. Moreover, anaemia is a leading cause of maternal deaths and adverse pregnancy outcomes in developing countries(Reference Lander, Hambidge and Westcott17). Several studies have demonstrated that severe anaemia has multiple causes, distinct from mild or moderate anaemia(Reference Yip18). Women with severe anaemia are far more liable to experience many health hazards, such as infections and heart failure, which may increase the risk of maternal and neonatal deaths during delivery(1,Reference Ma, Zhang and Liu19) . It has been estimated that many pregnant women are already anaemic at the time of conception in developing countries(Reference Baig-Ansari, Badruddin and Karmaliani16). Therefore, pre-pregnancy maternal anaemia is closely related to women’s health and future pregnancy outcomes.
At present, many studies have reported on the prevalence of anaemia among the general population or among pregnant women, but few have focused on prevalence among pre-pregnant women(Reference Stevens, Finucane and De-Regil15,Reference Herzog, Leikauf and Jakse20) . In addition, although some variables are already known to be associated with an increased risk for anaemia(Reference Chaparro and Suchdev6), ABO blood type, rhesus (Rh) blood type and menstruation status are not commonly analysed as risk factors. The association between blood type and anaemia status remains unknown in this population. To update current knowledge on the epidemiology of anaemia, we examined the prevalence of overall anaemia and anaemia by severity in a population of pre-pregnant women. Therefore, we focused on Chinese pre-pregnant women and used the data from the National Free Pre-conception Check-up Projects (NFPCP) to estimate the prevalence and identify correlated factors of anaemia by severity level, which was based on the most recent WHO cut-off values to categorise anaemia.
Materials and methods
Study population and study design
The NFPCP is supported by the Chinese government, aiming to provide free pre-conception health examinations for couples who planned to be pregnant within 6 months to reduce the incidence of adverse pregnancy outcomes throughout the country(Reference Zhou, Acharya and Zhang21,Reference Zhang, Wang and Shen22) . The project began in 2010 with 100 rural counties and has been further expanded to all urban and rural areas in mainland China. Detailed information about the protocols, study design, organisation and implementation has been described previously(Reference Liu, Zhang and Liu23–Reference Zhou, Zhang and Wang25).
Relying on the NFPCP database, we conducted a nationwide population-based cross-sectional study to obtain Hb concentration distributions and anaemia prevalence among pre-pregnant women in mainland China. Since the legal age for women to get married in China is 20 years, and 49 years is considered to be the upper age limit for reproductive-age women(Reference Kibret, Chojenta and D’Arcy26), we chose pre-pregnant women between 20 and 49 years old as the research object. A total of 5 830 265 Chinese women aged 20–49 years participated in the NFPCP from 1 January 2017 to 31 December 2017. The present study included 5 679 782 participants (150 483 were excluded due to their Hb concentration being unavailable) from thirty-one provinces in China who had completed both standardised questionnaires and laboratory examinations of Hb concentration.
Data collection and definitions of anaemia
Local health workers collected participants’ general information through a standardised questionnaire, including demographic characteristics (age, region, ethnic origin, educational level and occupation, self-reported pregnancy history), health status/lifestyles (self-reported meat and egg eating habits, smoking and alcohol consumption, and self-reported history of anaemia) and self-reported menstruation status (age at menarche (AAM), menstrual blood loss, menstrual period and menstrual cycle). Health professionals measured participants’ height and weight according to the NFPCP’s standard techniques and protocols. According to the National Clinical Laboratory Procedures of this project, blood samples were collected after at least 8 h of fasting using ethylenediamine tetraacetic acid vacuum tubes to examine participants’ Hb concentration (cyanmethemoglobin method), ABO blood type and Rh blood type(Reference Zhang, Wang and Shen22). The accuracy and stability of Hb measurement and other laboratory tests were ensured through establishment of a quality assurance system in the NFPCP(Reference Zhou, Acharya and Zhang21,Reference Zhang, Wang and Shen22) .
In our study, women were divided into six groups according to age (20–24, 25–29, 30–34, 35–39, 40–44 and 45–49 years). Region indicates the province where the inspection agency was located and was grouped as follows: ‘north’ (Beijing, Tianjin, Hebei, Shanxi and Inner Mongolia), ‘northeast’ (Liaoning, Jilin and Heilongjiang), ‘east’ (Shanghai, Jiangsu, Zhejiang, Anhui, Fujian, Jiangxi and Shandong), ‘south-central’ (Henan, Hubei, Hunan, Guangdong, Guangxi and Hainan), ‘southwest’ (Sichuan, Guizhou, Yunnan, Tibet and Chongqing) and ‘northwest’ (Shaanxi, Gansu, Qinghai, Ningxia and Xinjiang)(27). Other demographic characteristics were further categorised as follows: ethnic origin (Han or others), educational level (primary school or below, junior high school, senior high school, college and master or above), occupation (farmers, manual labourers, waitresses, merchants, housekeeping, teacher or civil servants and others), ABO blood type (O, A, B and AB), Rh blood type (positive and negative) and pregnancy history (no and yes). BMI was calculated using weight and height based on the following formula: BMI = weight/height2 (kg/m2). The classification of BMI was defined according to the criteria of the working group on obesity in China: underweight (BMI < 18·5 kg/m2), normal (18·5 ≤ BMI < 24·0 kg/m2), overweight (24·0 ≤ BMI < 28·0 kg/m2) and obesity (BMI ≥ 28·0 kg/m2)(Reference Zhou28). In the questionnaire, local health professionals asked the participants whether they ate meat and eggs in their daily life. If the answer was ‘yes’, they were considered meat and egg eaters. Smoking status was defined according to WHO guidelines(29) (Online Supplementary Table S2). Other healthy status/lifestyles characteristics were further categorised as follows: alcohol consumption (no and yes) and history of anaemia (no and yes).
A regular menstrual cycle was defined as an intermenstrual interval of 21–35 d and a menstrual period with 3–7 d(Reference Doi, Al-Zaid and Towers30). Based on the definition of regular menstruation and normal menstrual bleeding(Reference Doi, Al-Zaid and Towers30,Reference Marnach and Laughlin-Tommaso31) , menstrual status was further categorised as follows: AAM (≤11, 12, 13, 14, ≥15 years old), menstrual blood loss (heavy, normal and light), menstrual period (<3, 3–7, >7 d) and menstrual cycle (<21, 21–35, >35 d).
According to the cut-off values of anaemia recommended by the most recent WHO criteria, anaemia in non-pregnant women at sea level who were aged 15 years and above was defined as Hb < 120 g/L, among which mild, moderate and severe anaemia were defined as 110 g/L ≤ Hb < 120 g/L, 80 g/L ≤ Hb < 110 g/L and Hb < 80 g/L, respectively, which was consistent with current Chinese anaemia thresholds(1,Reference Cappellini and Motta32,33) . Additionally, based on WHO criteria, measured Hb concentrations were adjusted by altitude level and smoking status because residential elevation above sea level and smoking are known to increase Hb concentrations(1). If we used uniform measured Hb concentrations, the prevalence of anaemia in persons residing at high altitudes or smoking might be underestimated(1,34) (Online Supplementary Tables S1 and S2).
Statistical analysis
The mean and standard deviation of Hb concentration were used to estimate Hb concentration levels. Count and percentage were introduced to describe the prevalence of anaemia and the distribution of demographic characteristics, health status, lifestyles and menstruation status. The χ 2 test was used for categorical variables. Univariate and multivariate logistic regressions were adopted with OR and the 95 % CI to analyse factors correlated with anaemia/severe anaemia. The Hosmer–Lemeshow goodness-of-fit test was used to assess model fit. The NFPCP medical service information system was applied for data collection and storage. Microsoft SQL server 2012 (Microsoft Corporation) was used for data cleaning and management. Statistical analyses were performed with SAS software (version 9.3; SAS Institute, Inc.) and R software (version 4.0.3). Two-sided P-values <0·05 were considered statistically significant.
Ethical approval
The present study was reviewed and approved by the Institutional Research Review Board at the National Health Commission and the National Health Council’s Ethics Review Committee. Informed consent was obtained from every subject before they participated in the study.
Results
A total of 5 679 782 pre-pregnant women aged 20–49 years from thirty-one provinces in China were enrolled in the present study (Fig. S1). The mean age of women participating in the study was 29·23 (6·07) years. Participants were mostly 20–34 years old (81·47 %), Han ethnicity (88·67 %), senior high school education or below (78·79 %), farmers (67·84 %) and Rh-positive blood type (99·61 %). The overall mean and standard deviation of Hb concentration in all subjects was 129·01 g/L (14·34 g/L). Among them, the proportion of women with Hb concentrations of 130 g/L was the highest, comprising 3·54 % (201 247) of women (Fig. 1).

Fig. 1. Distributions of Hb concentration among pre-pregnant women in mainland China. The number of women (total number 5 679 782): Hb < 40 g/L 2880; 40 g/L ≤ Hb < 60 g/L 1387; 60 g/L ≤ Hb < 80 g/L 15 905; 80 g/L ≤ Hb < 100 g/L 133 065; 100 g/L ≤ Hb < 120 g/L 1 028 167; 120 g/L ≤ Hb < 140 g/L 3 358 605; 140 g/L ≤ Hb < 160 g/L 1 064 363; 160 g/L ≤ Hb < 180 g/L 61 891; Hb ≥ 180 g/L 13 519. ![]() , Pre-pregnant women;
, Pre-pregnant women; ![]() , anaemia cut-off for non-pregnant women.
, anaemia cut-off for non-pregnant women.
The overall prevalence of anaemia among pre-pregnant women in our study was 21·64 % (95 % CI 21·60 –21·67 %) in mainland China (mild anaemia: 14·10 %, moderate anaemia: 7·17 % and severe anaemia: 0·37 %). As shown in Fig. 2 and Supplementary Table S3, the prevalence of overall anaemia and severe anaemia was the highest in Tibet (overall: 65·09 %; severe anaemia: 4·72 %) and the lowest in Beijing (overall: 7·47 %; severe anaemia: 0·11 %) among thirty-one provinces. In addition, we calculated and summarised the prevalence of anaemia at different severity levels among pre-pregnant women in these thirty-one provinces of China. Mild anaemia accounted for the highest proportion of overall anaemia, except in Tibet, in which the proportion of moderate anaemia was the highest (61·02 %).

Fig. 2. Prevalence of anaemia among pre-pregnant women in mainland China. (a) Prevalence of overall anaemia. ![]() , 7·47–15·00;
, 7·47–15·00; ![]() , 15·10–17·00;
, 15·10–17·00; ![]() , 17·10–21·00;
, 17·10–21·00; ![]() , 21·10–23·00;
, 21·10–23·00; ![]() , 23·10–30·00;
, 23·10–30·00; ![]() , 30·10–65·10. (b) Prevalence of severe anaemia.
, 30·10–65·10. (b) Prevalence of severe anaemia. ![]() , 0·11–0·21;
, 0·11–0·21; ![]() , 0·22–0·30;
, 0·22–0·30; ![]() , 0·31–0·40;
, 0·31–0·40; ![]() , 0·41–0·80;
, 0·41–0·80; ![]() , 0·81–2·00;
, 0·81–2·00; ![]() , 2·01–4·72. The dark colour reflects high prevalence and the light colour indicts low prevalence. The names of the provinces are marked at their provincial capitals. The number of women in the provinces included in our study (total number 5 679 782) are as follows: Beijing 20 514; Tianjin 28 226; Hebei 385 872; Shanxi 9306; Inner Mongolia 72 163; Liaoning 64 027; Jilin 60 835; Heilongjiang 57 435; Shanghai 6439; Jiangsu 47 436; Zhejiang 211 629; Anhui 365 711; Fujian 188 288; Jiangxi 213 918; Shandong 636 233; Henan 606 398; Hubei 310 340; Hunan 471 939; Guangdong 457 884; Guangxi 217 544; Hainan 38 658; Chongqing 75 037; Sichuan 321 822; Guizhou 185 604; Yunnan 225 808; Tibet 9096; Shaanxi 35 862; Gansu 145 586; Qinghai 37 568; Ningxia 42 812; and Xinjiang 129 792.
, 2·01–4·72. The dark colour reflects high prevalence and the light colour indicts low prevalence. The names of the provinces are marked at their provincial capitals. The number of women in the provinces included in our study (total number 5 679 782) are as follows: Beijing 20 514; Tianjin 28 226; Hebei 385 872; Shanxi 9306; Inner Mongolia 72 163; Liaoning 64 027; Jilin 60 835; Heilongjiang 57 435; Shanghai 6439; Jiangsu 47 436; Zhejiang 211 629; Anhui 365 711; Fujian 188 288; Jiangxi 213 918; Shandong 636 233; Henan 606 398; Hubei 310 340; Hunan 471 939; Guangdong 457 884; Guangxi 217 544; Hainan 38 658; Chongqing 75 037; Sichuan 321 822; Guizhou 185 604; Yunnan 225 808; Tibet 9096; Shaanxi 35 862; Gansu 145 586; Qinghai 37 568; Ningxia 42 812; and Xinjiang 129 792.
Results of the Hosmer–Lemeshow test showed that model fitting was acceptable in our study (P > 0·05). Table 1 presents the variation in anaemia prevalence among women with different characteristics. Although women with different anaemia statuses and without anaemia had significantly different distributions of demographic characteristics, health status/lifestyles and menstruation status in our study (P < 0·01), some of these differences were very small due to the large sample size. Among the age groups, the overall anaemia prevalence was higher in the 20–24-year-old group (22·15 %). For mild anaemia, the prevalence decreased with age. However, the prevalence of severe anaemia increased monotonically with age. In terms of region, the overall anaemia prevalence was lowest in the northeast (17·89 %), and severe anaemia prevalence was lowest in the east (0·30 %). The prevalence of overall anaemia was significantly lower in the groups of women who were of Han ethnic origin, without a history of pregnancy, with an educational level of master’s degree or above, with the occupation of teachers or civil servants, B blood type, Rh-positive blood type, obesity, meat and egg eaters, alcohol consumption and without a history of anaemia (P < 0·01) (Table 1). Women with AAM ≤ 11 years old, light menstrual blood loss, menstrual period within 3 d and menstrual cycle over 35 d presented a lower prevalence of overall anaemia (P < 0·01). The correlated factors in severe anaemia were basically the same (Table 1).
Table 1. The variation of anaemia prevalence among pre-pregnant women
(Numbers, percentages and confidence intervals)
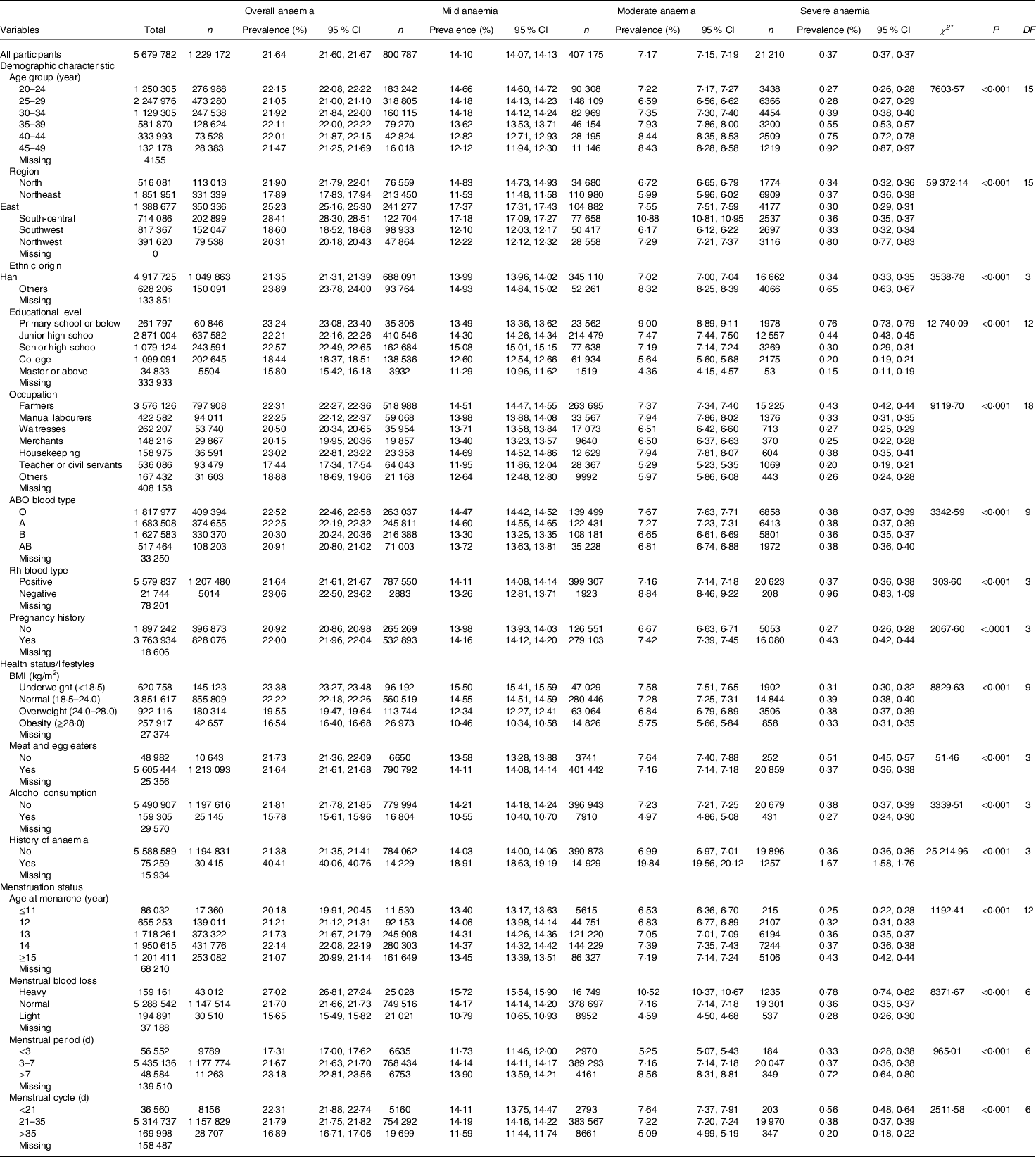
n, number; Rh blood type, Rhesus blood type.
* χ2 test was used to examine the difference of demographic characteristics among different Hb concentrations groups (non-anaemia group v. mild anaemia group v. moderate anaemia group v. severe anaemia group).
Compared with those aged 20–24 years, women in the older age groups were more likely to suffer from anaemia by multivariable logistic regression, especially in women aged 40–44 years (adjusted OR (aOR) = 1·11, 95 % CI 1·09, 1·12) (Table 2). Meanwhile, women aged 45–49 years had a higher odds of having moderate-to-severe anaemia than other age groups. Residing in different regions was correlated with the status of being anaemic as well. Women of other ethnic origins showed an increased odds of suffering from anaemia (aOR = 1·11, 95 % CI 1·10, 1·12). Women with an education of master’s degree or above (aOR = 0·76, 95 % CI 0·73, 0·78) or with an occupation of teacher or civil servant were less likely to have anaemia than those who with a primary school education or who were farmers, respectively. In terms of ABO blood type, people with B blood type seemed to be consistently less likely to suffer from anaemia of different severity categories than those with O blood type. The results of the Rh blood type group revealed that women with Rh-negative blood type were 1·10-fold more likely to have anaemia. These correlations were consistent according to anaemia severity levels. Women with a history of pregnancy presented a higher odds of anaemia than women without a pregnancy history (aOR = 1·07, 95 % CI 1·06, 1·08) (Table 2).
Table 2. Factors correlated with anaemia among pre-pregnant women in mainland China
(Odd ratios values and their 95 % confidence intervals)
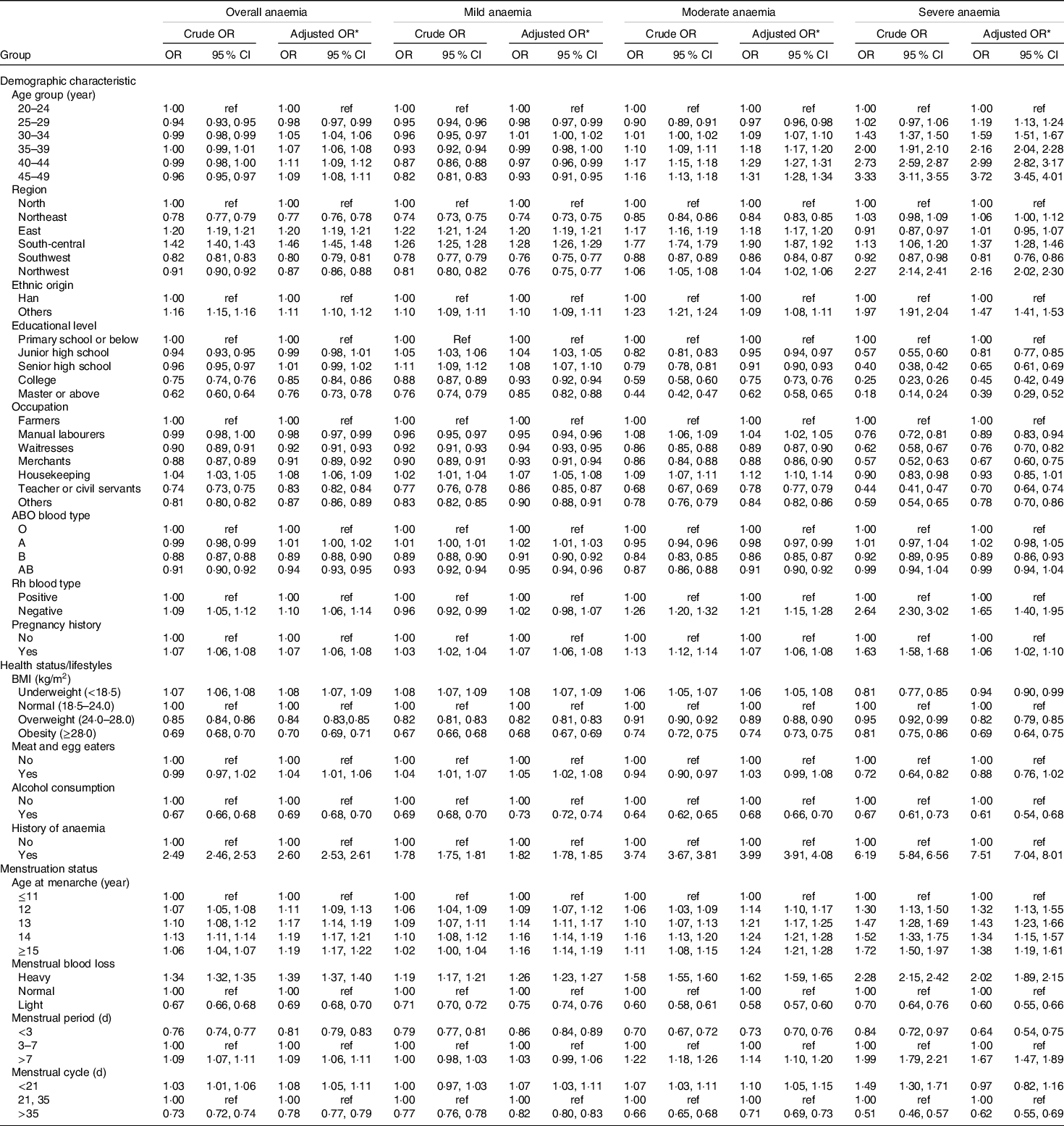
ref, reference; Rh blood type, Rhesus blood type.
The OR for mild, moderate and severe anaemia categories were compared with non-anaemia category.
* Multivariable-adjusted OR (95 %CI) were adjusted for age group, region, ethnic origin, educational level, occupation, ABO blood type, Rh blood type, pregnancy history, BMI, meat and egg eaters, alcohol consumption, history of anaemia, age at menarche, menstrual blood loss, menstrual period and menstrual cycle.
Factors of health status/lifestyles and anaemia prevalence were also presented. In BMI categories, women who were underweight showed a significantly higher prevalence of anaemia (23·38 %) with an aOR of 1·08 (95 % CI 1·07, 1·09). Correspondingly, only the severe anaemia category presented an inconsistent association with underweight (aOR = 0·94, 95 % CI 0·90, 0·99). Compared with women with a normal BMI, overweight and obese women had 16 % and 30 % lower odds of experiencing anaemia (aOR = 0·84, 95 % CI 0·83, 0·85; aOR = 0·70, 95 % CI 0·69, 0·71). The habit of eating meat and eggs was found to be associated with mild anaemia (aOR = 1·05, 95 % CI 1·02, 1·08) but was not correlated with moderate or severe anaemia after further adjustment. Moreover, alcohol consumption was associated with a reduced odds of anaemia (aOR = 0·69, 95 % CI 0·68, 0·70). Furthermore, the odds of anaemia was 2·60 times higher (95 % CI 2·53, 2·61) in women who self-reported a history of anaemia; this increased to 7·51 times (95 % CI 7·04, 8·01) in the severe anaemia subgroup (Table 2).
In terms of menstrual status, women with late menarche were more likely to have anaemia than those aged ≤ 11 years at menarche. The same results were also detected for the three anaemia severity levels. Women with heavy menstrual blood loss, longer menstrual period (>7 d) and shorter menstrual cycle (<21 d) had higher odds of experiencing anaemia, while those with light menstrual blood loss, shorter menstrual period (<3 d) and longer menstrual cycle (>35 d) exhibited reduced odds for anaemia (Table 2).
Discussion
The importance of anaemia among non-pregnant women as a major public health problem worldwide is widely recognised. According to the WHO, the classification of public health significance for anaemia in populations based on prevalence was defined as follows: severe (≥40 %), moderate (20·0–39·9 %), mild (5·0–19·9 %) and normal (≤4·9 %)(1). We found that the prevalence of anaemia among pre-pregnant women in mainland China was 21·64 %, which was considered a moderate health problem. Previous studies have suggested that half of anaemia cases worldwide are attributed to Fe deficiency, and anaemia prevalence was an important health indicator(1,4) . Based on global population-representative data, Stevens proposed that the prevalence of anaemia and severe anaemia among non-pregnant women was 21 and 0·5 % in East and Southeast Asia, 33 and 1·0 % in Central Asia, and 47 and 2·4 % in South Asia, respectively(Reference Stevens, Finucane and De-Regil15). The prevalence of anaemia obtained in our study was similar to that in East and Southeast Asia, but the prevalence of severe anaemia was lower than that in East and Southeast Asia.
In our study, we found that Tibet exhibited the highest prevalence of both anaemia and severe anaemia among thirty-one provinces in mainland China. A previous study suggested that the prevalence of anaemia in pregnant women living in Tibet was 50·6 %, higher than in other provinces(35). Nevertheless, the prevalence of anaemia among pre-pregnant women in Tibet has not been reported before. Tibet is located at an average altitude of 4000–5000 metres, in a plateau environment with a cold and dry climate, low pressure and oxygen-poor status. The Tibetan people are accustomed to drinking Tibetan butter tea in daily life, but drinking too much Tibetan butter tea may cause polyphenols to form an insoluble complex with Fe, reducing the absorption rate of Fe(36). The highest prevalence of anaemia in Tibet might be closely related to plateau weather conditions, the local economy, dietary habits and health education levels.
Previous studies have found that age is associated with the prevalence of anaemia(Reference Kamruzzaman, Rabbani and Saw37–Reference Vindhya, Nath and Murthy39). In the present study, the prevalence of anaemia was lowest in the 25–29 age group (21·05 %) and highest in the 20–24 age group (22·15 %), similar to a previous study(Reference Qiuyue, Shikun and Jue40). Younger women are prone to Fe deficiency anaemia due to menstrual blood loss, and unhealthy dietary patterns, such as dieting, might make this population more susceptible to malnutrition and anaemia. It is worth noting that the peak for women’s fertility occurs in the early 20s(Reference Meczekalski, Czyzyk and Kunicki41), so the overall anaemia prevalence is higher among young women in this age group who are trying to conceive, which can have a great impact on the health of their future generations. Our study found that the prevalence of mild anaemia was highest in the 20–24 age group, while the prevalence of moderate/severe anaemia was highest in the 45–49 age group. These findings were partially consistent with the study of Rasha(Reference Arabyat, Arabyat and Al-Taani42). Compared with previous studies, we also found that other demographic characteristics, such as ethnic origin, educational level and occupation, were associated with the prevalence of anaemia(Reference Kibret, Chojenta and D’Arcy26,Reference Kamruzzaman, Rabbani and Saw37,Reference Le38) . Anaemia is considered a marker of socio-economic disadvantage, with the poorest and least educated at the greatest risk for anaemia and its sequelae(Reference Balarajan, Ramakrishnan and Ozaltin43). We revealed that women with higher educational levels and non-farmer occupations were less likely to develop anaemia. Although there were statistically significant differences in most of the demographic characteristics in our study due to the large sample size, these differences were actually very small.
It was suggested that ABO blood groups convey a special vulnerability to individuals who possess a certain ABO blood type(Reference Seyfizadeh, Seyfizadeh and Yousefi44,Reference Wolpin, Kraft and Xu45) . Seyfizadeh demonstrated that there was no significant difference in Hb concentrations among pregnant women with different blood types(Reference Seyfizadeh, Seyfizadeh and Yousefi44). However, the association has not been investigated among pre-pregnant women. A previous study of Plasmodium vivax infection demonstrated that Hb levels in infected individuals with blood type O were significantly lower than those in individuals with blood type A(Reference Resende, Milagres and Chaves46). Our study revealed that women with blood type B had a lower odds for anaemia than those with blood type O. An individual can be classified as Rh-positive if their erythrocytes express the Rh D antigen; otherwise, an individual is Rh-negative. A previous study suggested that this phenomenon is clinically significant, especially for Rh incompatibility, which could result in consequences along the spectrum of hemolytic disease of the neonate ranging from self-limited hemolytic anaemia to severe hydrops fetalis(Reference Cohen47). To date, no study has revealed the association between Rh blood type and anaemia status. In our study, Rh-negative women had a higher odds for anaemia than Rh-positive women, which might be of particular concern(Reference Morton48). Since reproduction is also implicated in anaemia risk(Reference Miller49), we investigated and demonstrated that women with a pregnancy history were more likely to experience anaemia, in contrast to a previous study of Laura (Reference Goetz and Valeggia50).
Our study showed that underweight women were more likely to suffer from anaemia than those with a normal BMI. The results of a cross-sectional study of 5293 non-pregnant ever-married women in Bangladesh by Kamruzzaman were similar to ours(Reference Kamruzzaman, Rabbani and Saw37). Rasha showed no significant association between anaemia and BMI among women aged 15–49 years(Reference Arabyat, Arabyat and Al-Taani42). By analysing the severity of anaemia, we found that underweight people were more likely to suffer from mild/moderate anaemia than those with normal BMI. Conversely, an inconsistent association between underweight and severe anaemia was detected in our study. A previous study suggested that severe anaemia has multiple causes, and it is important to note that the primary causes of mild and moderate anaemia tend to differ from the principal causes of severe anaemia, although there are limited studies on the aetiology of severe anaemia(Reference Chaparro and Suchdev6).
Our study did not find that eating meat or eggs was a factor in severe anaemia, similar to a previous study(Reference Ma, Zhang and Liu19). Pasricha suggested that consumption of meat at least three times a week was more common in non-anaemic women(Reference Pasricha, Caruana and Phuc51). The lack of detailed quantitative information on meat and egg diets might interfere with these results. There is no doubt that a history of anaemia was a risk factor for anaemia, which presented a similar trend as a previous study(Reference Ma, Zhang and Liu19). In addition, we found that women who drank alcohol were less likely to develop anaemia and severe anaemia, consistent with the subgroup analysis results of another study by Vulser(Reference Vulser, Wiernik and Hoertel52). However, Perumal, who conducted a study to assess risk factors for anaemia in pregnant women in India, reported that alcohol consumption was a significant risk factor(Reference Perumal53). There is no direct study to support this finding in a population of pre-pregnant women. Thus, quantitative information on alcohol consumption is needed in future studies to validate the association.
The menstruation status was striking in anaemia prevalence, as menstruation plays an important role in maintaining a negative Fe balance in women(Reference Blanco-Rojo, Toxqui and Lopez-Parra54). We analysed four aspects of menstruation and found that women with older AAM (>11-year-old), heavy menstrual blood loss, longer menstrual period (>7 d) and shorter menstrual cycle (<21 d) had a higher odds of anaemia. AAM reflects a woman’s health status, and older AAM carries its own health burden(Reference Goon, Toriola and Uever55). Reproductive-age women in these settings are at further risk of anaemia due to Fe loss during menstruation(Reference Abioye, Park and Ripp56). Previous studies have shown that as the menstrual cycle lengthens, ferritin levels and physiological functions of reproductive-age women decrease significantly, making them more prone to experience anaemia(Reference Kocaoz, Cirpan and Degirmencioglu57). The effect of heavy menstrual bleeding on anaemia was similar to our study. Hence, anaemic females with menstruation problems should be treated due to their long menstrual period, short menstruation cycle and abnormal hemorrhage quantity. Notably, small differences can easily be detected with larger sample sizes, so the clinical importance of these ‘significant’ differences should be treated with caution when interpreting the results.
The present study has several strengths. First, we not only assessed the prevalence of anaemia among pre-pregnant women but also took anaemia severity levels into account, resulting in updated data on Hb concentration levels and anaemia prevalence in this important population in mainland China. The definition of anaemia in the present study was based on the latest WHO criteria for anaemia thresholds, enabling our results to be reasonable and comparable. Second, to our knowledge, this is the latest study in this field involving the largest sample size from thirty-one provinces in mainland China. Adequate sample size permits accurate estimates for different age groups or other demographic characteristic subgroups, providing more comprehensive and representative results for this population. The large population-based sampling framework, standardised data collection methods and strict laboratory quality control ensured the reliability of the data. Third, we revealed a correlation between blood types and anaemia status for the first time. Elements of menstruation were also specifically analysed. In addition, health status, lifestyle and other factors were also taken into account to conduct a broader analysis of the prevalence of anaemia.
However, there are some limitations to our study. First, there was potential bias in our study, as part of the information was self-reported by participants. Second, due to the lack of additional information on nutritional testing and dietary habits, we could not accurately identify women with low nutritional reserves or quantify alcohol consumption, which limited the interpretation of the association between anaemia and these factors. Since data on certain important factors, such as other reproductive events (reproductive age and obstetric history) and the use of supplements containing ferrous sulphate, folic acid and vitamin A(7), were not available, we were unable to assess the association between anaemia and these factors in the present study. Therefore, we cannot comment on the counterintuitive findings on the relationship between these health statuses and anaemia. Third, although Fe deficiency is considered the most common cause of anaemia globally(4,58) , there was no information on additional parameters, such as Fe intake, forms of anaemia, causes of anaemia and acute/chronic inflammation, in our dataset(1,4,7) . Consequently, speculation on Fe deficiency anaemia or other types of anaemia should be interpreted with caution.
In summary, the prevalence of anaemia among pre-pregnant women was 21·64 % in mainland China, which is lower than the global prevalence. Reducing pre-pregnancy anaemia in women is an important component of maternal and child health. Interventions, such as health education and health promotion, should be considered to maximise effectiveness and avoid potential harm to this population. Therefore, the above information, along with the safety profile and economic outcomes, could be conducive for policy-makers and health administrators in implementing new strategies and strengthening existing services.
Acknowledgements
The authors would like to express their sincere gratitude to the health workers and participants in the NFPCP for their considerable efforts and collaboration.
This research has received funding from the National Key Research and Development Program of China (Grant No. 2016YFC1000307), National Natural Science Foundation of China (Grant No. 81872634), National Human Genetic Resources Sharing Service Platform (Grant No. 2005DKA21300), National Population and Reproductive Health Science Data Center (Grant No. 2005DKA32408), and Project of National Research Institute for Family Planning (Grant No. 2018NRIFPJ03), People’s Republic of China. The founding sponsors had no role in the design, analysis or writing of this article.
Supervision: Xu Ma and Bei Wang; Funding acquisition: Xu Ma and Bei Wang; Conceptualisation: Jun Zhao and Xiaoyue Zhu; Formal analysis: Xiaoyue Zhu and Jun Zhao; Methodology: Jun Zhao, Xiaoyue Zhu and Xiang Hong; Writing – original draft: Xiaoyue Zhu and Jun Zhao; Writing – review and editing: Jun Zhao, Xiaoyue Zhu, Qiaoyun Dai, Xiang Hong, Xueying Yang, Kaiping Huang, Yue Zhang and Yan Xuan; Validation: Qiaoyun Dai and Xiang Hong; Visualisation: Xiaoyue Zhu, Kaiping Huang and Yue Zhang; Data curation: Hongguang Zhang; Investigation: Yuanyuan Wang, Zuoqi Peng and Ya Zhang; Project administration: Qiaomei Wang, Haiping Shen, Yiping Zhang and Donghai Yan. All authors certified that they have participated in the conceptual design of this work, the analysis of the data and the writing of the manuscript to take public responsibility for it. All authors reviewed the final version of the manuscript and approve it for publication.
The authors declare that they have no competing of interests.
The views expressed in the report are the authors’ and do not necessarily reflect the official policy or position of the National Health Commission of the People’s Republic of China.
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Research Review Board at the National Health Commission and the National Health Council’s Ethics Review Committee. Informed consent was obtained from every subject before they participated in the study.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S0007114521001148






