Recent international research demonstrates that between 40 and 47% of attendees at a Sexual Assault Referral Centre are known to mental health services. Reference Brooker and Durmaz1–Reference Brown, Du Mont, Macdonald and Bainbridge3 The role of sexual violence and abuse has been also well documented in the aetiology of mental health disorders where there is an additive effect. Reference Jonas, Bebbington, McManus, Meltzer, Jenkins and Kuipers4 For example, those subjected to extreme sexual violence are more likely to be: alcohol dependent, drug dependent, admitted to a psychiatric unit and to have attempted suicide. 5
Implementation of policy
In 2008, in recognition of the impact of sexual violence and abuse on mental health, it became policy, that all those on the care programme approach (CPA) should be assessed by ‘trained’ mental health clinicians for their experience of sexual violence/abuse. In 2008/9 a national training programme was piloted in eight mental health trusts. In the context of routine enquiry, and some 8 years on, it is pertinent to ask to what extent the CPA is being adhered to today in this regard. A national survey of mental health trusts, using freedom of information requests, was undertaken in 2015 in order to examine this. Providers were asked about clinical practice in relation to sexual violence/abuse and the CPA and a response rate of 79% was obtained. All trusts stated that they recorded whether routine enquiry took place but only 14% of trusts audited this activity (n = 5). One such reported audit examined ten admissions over a period of 1 week. The average proportion of staff reported to have been trained to undertake routine enquiry was 66% (range 35–100%) with all trusts stating that such training was mandatory.
Data on routine enquiry was requested from the Health and Social Care Information Centre (HSCIC). This was the first ever request they had received on this topic. These data revealed that, in total, there were 335 727 people on the CPA in England but whether routine enquiry had taken place was recorded for just 17% of this group (56 914). Provider trusts can choose to submit data on this topic unlike other CPA items, which are mandatory to record. In 2014/15, over half of providers (57%) chose not to submit data on the indicator (Fig. 1). For the 30 providers that did submit information the data field was only 41% complete. Only 11 trusts out of 53 returned full data on the abuse indicator.
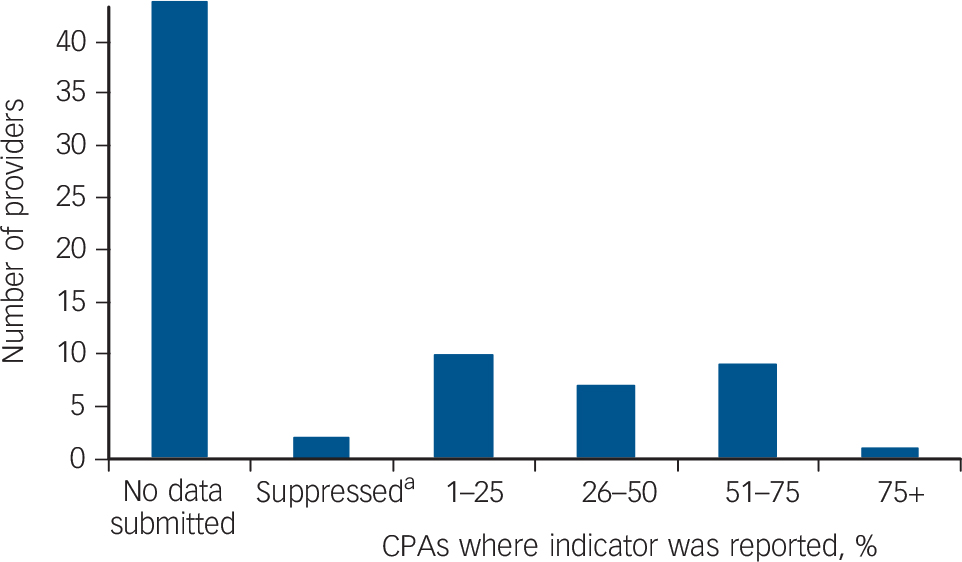
Fig. 1 The number of National Health Service mental health trusts that returned care programme approach (CPA) data to the Health and Social Care Information Centre (HSCIC) on the abuse indicator (2014/15).
a. The value for these providers was suppressed and all other numbers were rounded to the nearest five.
It seems clear from the data presented that all impetus has been lost on the initiative that commenced in 2008 to establish routine enquiry as part and parcel of the CPA assessment. In the course of this project, the Department of Health was approached and asked whether routine enquiry in the CPA was still national policy. The Department of Health referred us to NHS England who in turn referred us back to the Department of Health. Both agencies could not answer our question. In this policy vacuum it is perhaps not surprising that providers' efforts are waning.
In the course of working on this project, a mental health service in Tees, Wear and Esk Valley was identified that has been making formal efforts to become ‘trauma-informed’. The trauma-informed mental health service has been developed over the past 10 years and includes: the design of a specific pathway; staff training (including formulation, use of assessment measures and core skills); design of written guidelines and information sheets for service users, clinical staff and managers alike; and promotion and ownership by the Trust Board itself. Soft outcome measures revealed that the model, which specifically explored sexual violence/abuse, reduced staff sickness and decreased the use of ‘as needed’ medication and control and restraint. Reference Brooker, Brown, Tocque and Kennedy6 The use of outcome measures such as the Trauma Screening Questionnaire Reference Brewin, Rose, Andrews, Green, Tata and McEvedy7 revealed that 80% of those admitted had experienced trauma that was largely unresolved.
Way forward
Is it important that this area of practice is enhanced, and if so, how should improvements be made? First, the Department of Health and NHS England should agree under whose bailiwick this sits. Second, it should be a mandatory requirement that returns are made to the HSCIC on this area of the CPA as for other CPA indicators. Third, commissioners should be addressing shortfalls in staff training, which in some trusts are as low as 35%. Finally, what role, if any should the Care Quality Commission (CQC) be playing? The CQC inspects in relation to four main key areas of enquiry: safety, effectiveness, caring and well-led. Under ‘safety’, the following indicator is outlined: are there reliable systems in place to keep people safe and safeguarded from abuse? Unless routine enquiry takes place how can patient safety be accurately assessed?




eLetters
No eLetters have been published for this article.