Multidisciplinary team working is the agreed approach for mental health services to address complex needs in severe mental illness. In Ireland this has been delivered in accordance with the model outlined in The Psychiatric Services - Planning for the Future 1 but there has been limited study of the real world practice of multidisciplinary teams, including the relative roles of different team members in providing for the varying needs of service attenders. In contrast to the UK, where the National Services Framework 2 has provided a model for interdisciplinary working, services in Ireland have largely evolved according to the styles and practices of individual teams. Moreover, activities have been greatly determined by resource allocation with many teams operating for substantial periods without the full complement of multidisciplinary inputs. Reference Browne, Magar and Sheppard3 A recent discussion document failed to identify a single published study of multidisciplinary team working from Ireland, thus highlighting the lack of real-world evidence regarding the functioning of community mental health teams (CMHTs) to inform development of mental health services. 4
Since 2002 the St Anne's general adult psychiatry team in Limerick has operated with a full multidisciplinary complement that has allowed for the introduction of a number of evidence-based practices around management of anxiety symptoms and suboptimal prescribing. Reference Meagher and Moran5-Reference Moran, Raju, Saunders and Meagher7 In addition, this service provides a working example of how CMHT practices evolve without specific guidelines around roles and responsibilities for individual team members. The aim of this cross-sectional study was to investigate the role of individual multidisciplinary team members in overall service provision. We also examined the relationship between diagnosis, symptom profile and service utilisation to specifically explore whether individuals with more severe illness receive multidisciplinary care.
Method
The St Anne's service provides for a mixed urban and rural population of approximately 50 000 in the south-east city and county of Limerick. The team complement at December 2006 included two consultant psychiatrists, one specialist registrar, three senior house officers, eight community mental health nurses, one psychologist, one occupational therapist, and shared input from a social worker and addiction counsellor (0.5 whole time equivalent each).
Between September 2006 and January 2007 we assessed the complete service case-load including patient demographics, ICD-10 diagnoses 8 (made by a single consultant psychiatrist), service contacts, frequency of attendances, duration of service contact and treatment experiences (including multidisciplinary team member contacts and pharmacological treatment exposure). Severe mental illness was defined as a diagnosis of any major mood (bipolar affective disorder or recurrent depressive disorder with psychotic features) or enduring psychotic disorder (schizophrenia, schizoaffective disorder, persistent delusional disorder). Shared care was defined as attendance with two or more multidisciplinary team members but given the gatekeeper role of medical staff all service attenders are regularly reviewed at out-patient clinics such that shared care inevitably involves attending the doctor and one or more other multidisciplinary team members. In addition, all service attenders were assessed with the Health of the Nation Outcomes Scale (HoNOS) by a single trained clinician (D.M.) to avoid issues with interrater reliability. Reference Wing, Beevor, Curtis, Park, Hadden and Burns9,Reference Bebbington, Brugha, Hill, Marsden and Window10
Statistics
Statistical analyses were conducted using SPSS version 14.0 for Windows. Age, duration of attendance, total and single item HoNOS scores are expressed in means (s.d.). Mann-Whitney U-tests were used to compare the severity of HoNOS scores (including subscale scores) for attenders with multidisciplinary team members v. those not attending that multidisciplinary team member, those receiving shared care v. doctor only, and for those with severe mental illness v. those without. Fisher's exact test was used to compare the frequency of severe mental illness in those receiving shared care v. doctor only attenders and also the frequency of attendance with the occupational therapist for people with bipolar v. unipolar disorders. Frequency of attendance of those with severe mental illness v. non-severe mental illness was compared with independent t-tests. Correlation coefficients were used to assess the relationship between HoNOS ratings and the frequency of attendance. A Bonferroni correction (significance levels at P<0.01) was applied where multiple testing was conducted.
Results
Overall, 504 patients were attending the service. Of these 53% were female. Mean age was 44.3 years (s.d. = 14.1), mean duration of service attendance was 6.1 years (s.d. = 7.4) and 39% (n = 200) had severe mental illness. A total of 461 people (91%) were receiving psychotropic medications and 316 (62%) were receiving shared care.
Table 1 compares general clinical characteristics for the population according to multidisciplinary contacts. Although 45% (n = 141) of people receiving shared care had severe mental illness, this comprised 70% of the severe mental illness population. Those individuals receiving shared care had relatively greater current morbidity (v. doctor only) measured by total HoNOS scores (8.6 (s.d. = 5.9) v. 6.3 (s.d. = 5.5); P<0.001). Also, those people attending the addiction counsellor (P<0.001), social worker (P<0.001), and occupational therapist (P<0.05) had higher total HoNOS scores than the general population attending the service.
Table 1. Clinical characteristics of service attenders according to multidisciplinary team member contact
| n | Age, years Mean (s.d.) | Duration of attendance, years Mean (s.d.) | Severe mental illness % | Total HoNOS score Mean (s.d.) | |
|---|---|---|---|---|---|
| Community mental health nurse | 208 | 46.9 (14.8) | 8.2 (8.5) | 58 | 8.2 (5.9) |
| Psychologist | 95 | 37.7 (12.9) | 2.8 (4.1) | 11 | 7.7 (4.8) |
| Social worker | 56 | 39.9 (3.5) | 4.5 (4.9) | 43 | 11.6 (5.9) |
| Occupational therapist | 40 | 37.5 (12.8) | 4.7 (4.6) | 50 | 9.6 (5.7) |
| Addiction counsellor | 20 | 37.2 (9.0) | 3.1 (3.5) | 10 | 14.4 (5.2) |
| Doctor only | 188 | 45.0 (13.1) | 5.4 (6.8) | 27 | 6.3 (5.5) |
| Shared carea | 316 | 44.0 (14.6) | 6.5 (7.7) | 45 | 8.6 (5.9) |
The mean frequency of attendance was 9.1 (s.d. = 7.9) occasions for the overall case-load (range 1-40) with greater frequency in individuals with severe mental illness v. non-severe mental illness (11.6 (s.d. = 0.6) v. 7.0 (s.d. = 6.7); P<0.001). Frequency of attendance correlated significantly with total HoNOS scores (r =0.21, P<0.001) and with the subscales for social impairment (r =0.25, P<0.001) and symptoms (r =0.18, P<0.01) but not the sub-scales for behaviour or impairment.
Individuals attending the social worker had significantly higher scores for HoNOS sub-scales relating to problem behaviour (P<0.001), symptoms (P<0.001) and problems with social function (P<0.001). Individuals attending the occupational therapist had significantly higher HoNOS sub-scale scores for problems with social function (P<0.001). People attending the addiction counsellor had significantly higher subscale scores for problem behaviour (P<0.001), psychiatric symptoms (P = 0.001) and problems with social function (P =0.002). The only major trend for people attending the psychologist was for higher scores for psychiatric symptoms and this was not significant when a correction for multiple testing was applied (P =0.02) (Fig. 1).
Table 2 shows the primary diagnoses for people attending each of the multidisciplinary team members. Community mental health nurse activities were focused on people with schizophrenia and related conditions, whereas two-thirds of the psychology case-load related to depressive illness. The most common primary diagnosis for those attending the addiction counsellor was recurrent depressive disorder reflecting that this is a common comorbidity in people with substance misuse problems. Shared care (n = 319) involved input from nursing (n = 207); psychology (n= 76); social work (n = 59); occupational therapy (n = 47); and the addiction counsellor (n = 20).
Table 2. Primary diagnoses (%) of individuals attending multidisciplinary team members
| Schizophrenia-like disorders | Major mood disordera | Recurrent depressive disorder without psychosis | Anxiety disorder | Substance misuse | Organic mental disorder/intellectual disability | Other | |
|---|---|---|---|---|---|---|---|
| Total case-load | 31 | 8 | 45 | 10 | 2 | 2 | 2 |
| Community mental | 49 | 9 | 28 | 10 | 2 | 2 | 0 |
| health nurse | |||||||
| Psychologist | 8 | 2 | 67 | 13 | 1 | 2 | 7 |
| Social worker | 39 | 4 | 50 | 5 | 0 | 0 | 2 |
| Occupational therapist | 33 | 17 | 32 | 13 | 2 | 3 | 0 |
| Addiction counsellor | 11 | 0 | 56 | 0 | 33 | 0 | 0 |
| Doctor only | 20 | 8 | 52 | 11 | 2 | 4 | 3 |
| Shared care | 37 | 8 | 41 | 9 | 3 | 1 | 1 |
Compared with those attending the doctor only, those receiving shared care were more likely to have severe mental illness (73% v. 27%; P<0.001), higher HoNOS subscale scores for psychiatric symptoms (P<0.001), problems with social function (P<0.001), and higher total HoNOS scores (8.6 (s.d. = 5.9) v. 6.4 (s.d. = 5.5); P<0.001) (Fig. 2).
Discussion
This is the first study (to our knowledge) to report the use of the HoNOS across a complete Irish service population. We found shared care to be the norm with the majority of service attenders receiving multidisciplinary treatment. Moreover, greater intensity of multidisciplinary team exposure was evident for those with greater morbidity measured on HoNOS and those with severe mental illness suggesting that multidisciplinary activities are directed towards those with greatest need.
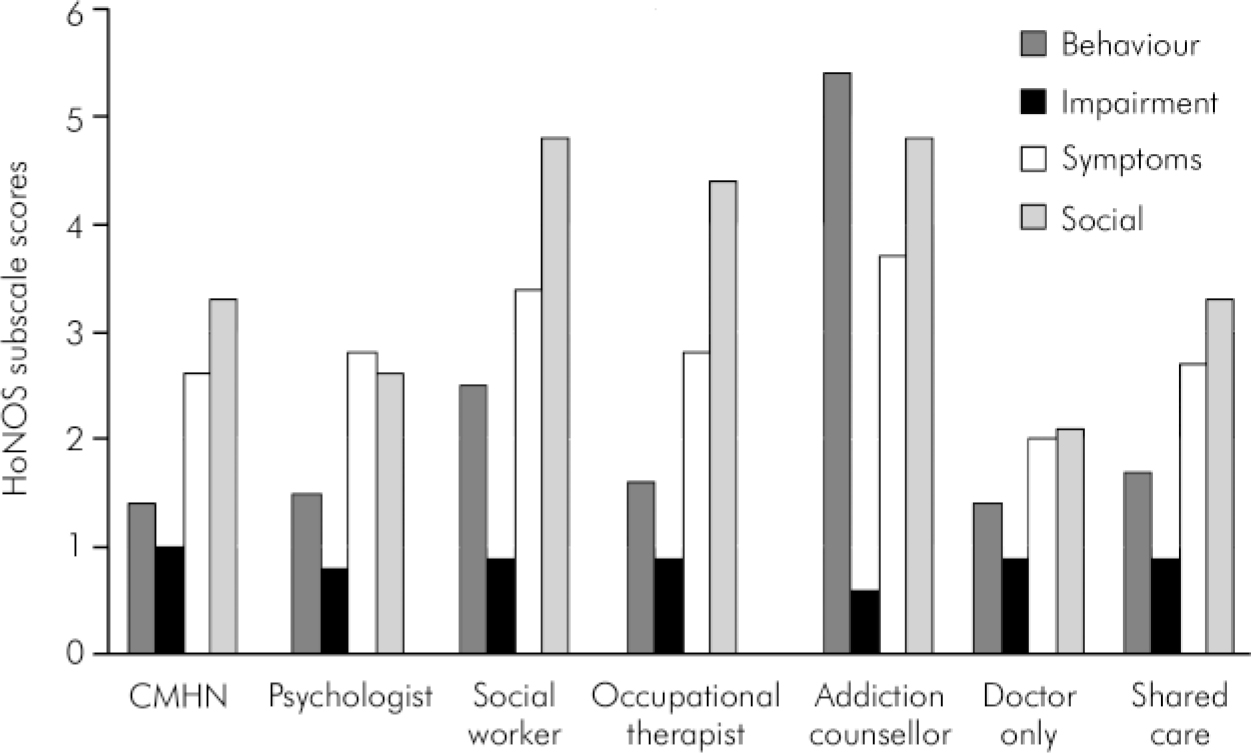
Fig. 1. Health of the Nation Outcome subscale scores for attenders with various mutlidisciplinary team members. CMHN, community mental health nurse; HoNOS, Health of the Nation Outcome Scale.
Given the historical development of the St Anne's service (i.e. without an explicit template for multidisciplinary working) this study provides a snapshot of how such services can develop naturalistically. The activities of individual team members varied considerably reflecting their differing roles in providing for the varying and sometimes complex needs of a sector population. The psychologist was more involved with individuals with mood problems, whereas both the occupational therapist and social worker had more varied case-loads that included a high percentage of people with psychosis. Importantly, community mental health nurse activities emphasised the needs of those with severe mental illness thus contrasting with studies in the UK from the early 90s that suggested that without specific guidance, many community mental health nurses gravitate towards those with less severe illness. Reference Gournay11
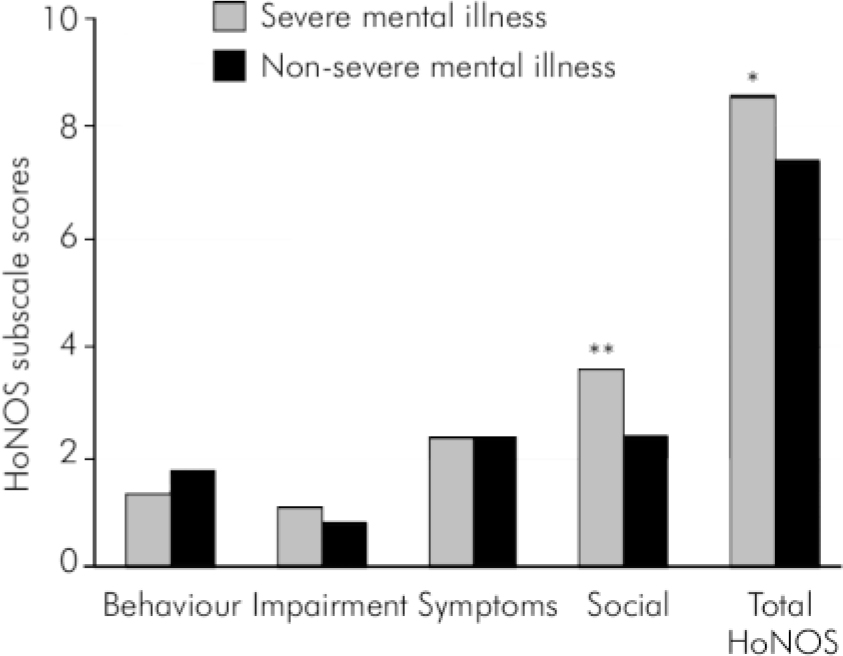
Fig. 2. Comparison of Health of the Nation Outcome subscale scores of individuals with severe mental illness v. those without. HoNOS, Health of the Nation Outcome Scale. *P<0.005; **P<0.001.
The St Anne's case-load differs from that reported in many UK-based studies where typically more than 50% have severe mental illness. Reference Burns12 This reflects the lower threshold in Ireland for accepting ongoing care of those with less severe mental health problems. It is thus particularly important that the needs of more severely ill people are prioritised as they can be displaced by the less severely ill who may advocate more actively for services.
The HoNOS is the most widely used routine outcome measure in British mental health services and is also used in Australasia, Canada and a number of European countries. Reference Pirkis, Burgess, Kirk, Dodson, Coombs and Williamson13 It provides a detailed characterisation of the clinical and social needs of people Reference Salvi, Leese and Slade14 and can predict variance in service utilisation. Reference Broadbent15 It also discriminates between those with differing levels of disability or need, including those receiving standard v. assertive case management. Reference Gallagher and Teesson16 We found that the HoNOS discriminated between individuals with severe mental illness v. those without and also predicted frequency of service contact and breadth of multidisciplinary contact.
People with severe mental illness had higher overall HoNOS scores. Although a cross-sectional design such as applied in this study can assess current or active morbidity, it does not fully capture the severity of illness over time. A principal focus of care for many people with more severe mental illness is to maintain remission and as such this is an important factor in understanding the relatively lower HoNOS scores and longer duration of service attendance for individuals engaged with community mental health nurses. Service need, therefore, cannot be judged merely upon a cross-sectional assessment of active symptomatology, but rather needs to also incorporate measures of severity over time. To a certain extent this is reflected in the diagnostic category where the contrasting natural histories of particular disorders (e.g. severe mental illness v. non-severe mental illness) is recognised. Allocation of service should be sensitive to these various indicators.
In keeping with previous work, higher HoNOS scores were most evident in relation to the social function subscale rather than reflecting greater behavioural or symptomatic difficulties. Reference Browne, Doran and McGauran17 These findings support the current emphasis on socioadaptive functioning in people with severe and enduring mental illnesses as a target for mental health services. 18 Previous work has used the HoNOS to identify individuals suitable for variants of community psychiatry (e.g. assertive case management) and as a measure of changes in clinical functioning, Reference Gallagher and Teesson16,Reference Taylor and Wilkinson19,Reference Hunter, Maclean, Peck, Pullen, Greenfield and McArthur20 although other work suggests that it should be augmented by diagnosis-specific scales. Reference Browne, Magar and Sheppard3,Reference Pirkis, Burgess, Kirk, Dodson, Coombs and Williamson13
In conclusion, this study of activities in a generic Irish CMHT found great variability in clinical activities for different multidisciplinary team members and a close association between illness severity and service utilisation.
Declaration of interest
D.M. is in receipt of an unrestricted educational grant from AstraZeneca Pharmaceuticals.







eLetters
No eLetters have been published for this article.