Adolescence is a critical stage for the growth and development of healthy eating behaviours between childhood and adulthood. The WHO defines an adolescent as any person aged between 10 and 19 years(1). The first transitions in eating patterns and behaviours from childhood to adolescence depend on the food environments and experiences that parents provide to their children, and these reinforce the food choices that adolescents make. Adequate nutrient intake has been positively associated with academic performance(Reference Neumark-Sztainer, Story and Resnick2) and reduced the risk of obesity and developing chronic diseases in adulthood(Reference Schneider, Dumith and Orlandi3). Healthy dietary patterns established during adolescence are more likely to extend into adulthood. Therefore, it is imperative for adolescents to have nutrition knowledge and cultivate healthy dietary behaviours for growth and health.
Story et al. (Reference Neumark-Sztainer, Story and Perry4,Reference Story, Neumark-Sztainer and French5) , reported that the following factors influence adolescent eating behaviours: (1) individual (e.g. food cravings, preferences and body image); (2) social and environmental (e.g. family and peers); (3) physical, environmental or community setting (e.g. school, convenience store and food availability) and (4) societal factors (e.g. mass media, marketing and advertising). Parents’ education level, household income and family composition are the main external factors that affect nutritional status among adolescents(Reference Scaglioni, De Cosmi and Ciappolino6). Adolescents from low-income families have fewer educational and financial resources than do those from high-income families(Reference Duncan and Murnane7) and may therefore develop unhealthy dietary patterns (i.e. energy-dense food and low vegetable and fruit intake) due to a lack of access to healthy food, an overabundance of energy-dense food and a lack of economic resources with which to purchase adequate food(Reference Rydén and Hagfors8,Reference French, Tangney and Crane9) . However, a healthy diet can be obtained at low cost with eating habit changes through improved nutrition knowledge(Reference Kaufman-Shriqui, Fraser and Friger10).
Eighty percentage of students attend after-school tutoring in Taiwan(11), making the after-school programme an integral part of adolescents’ daily lives. Thus, dinner time during after-school programmes may provide a chance to promote healthy eating habits. Few studies have examined students from economically disadvantaged families and assessed whether a short-term after-school nutrition education (ASNE) programme can improve their dietary quality and nutrition knowledge. This pilot ASNE programme can serve as an illustrative method for improving knowledge and changing eating behaviours among disadvantaged groups. Therefore, it is critical to develop a tailor-made after-school nutrition intervention programme for adolescents, particularly those from low-income families. This study investigated whether short-term ASNE programmes can improve nutrition knowledge and healthy eating behaviour among 10- to 15-year-old adolescents from economically disadvantaged families.
Methods
Participants and recruitment
This study used a one-group pretest–posttest design. Participants were 5th–9th graders (10 to 15 years) who participated in free after-school programmes provided by the nonprofit organisation Boyo Social Welfare Foundation. Participants in the 5th and 6th grades were studying in elementary school, whereas those in the 7th–9th grades were studying in junior high school. Admission to the programme was limited to households with an average monthly distributable income of US$180–$212 per person after deducting all expenses (basic living expenses, rent, mortgage and medical expenses for critical illness in the family) from the total household income.
All participants received nutrition education while attending the after-school programme. We recruited 161 adolescents from three after-school programme locations in central and southern Taiwan (Taichung City, Nantou County and Chiayi County). We excluded eight students who did not participate in the posttest. Of the remaining 153 participants (seventy-eight elementary school students and seventy-five junior high school students), ten were excluded due to unreasonable energy intake (< 800 or > 4000 calories for boys; < 500 or > 3500 calories for girls). A total of 143 participants were analysed.
After-school nutrition education programme
The ASNE programme aimed to enable adolescents to make good food choices. It taught students (1) to recognise the six major food groups which are used in the Dietary Guideline of Taiwan (whole grains, dairy, soya/fish/egg/meat, vegetables, fruits, oil/nuts) to ensure they selected a varied and healthy diet; (2) to know how healthy body weight is associated with a healthy diet and (3) to read, interpret and use nutrition labels for making healthy food choices. This tailored educational programme was delivered by a trained dietitian and involved interactive games and informational handouts. The syllabus is presented in Supplementary Table 1. The tailor-made ASNE programme spanned 3 months (March–May 2019) with one session per month. Each 1-h session was divided into a 20- to 30-min lecture and 30- to 40-min interaction (Q&A or reward-based quizzes). The nutrition intervention courses were taken by the same teacher and using the same materials, and 80 % of the same staff collected dietary and anthropometric information. All the staff members were trained using standard procedures before the interview.
Instruments, measures and procedures
Participants’ demographic information and nutrition knowledge, attitudes and practices were collected using self-administered questionnaires. Interviewers used a semi-quantitative FFQ (SFFQ) to collect dietary information. This information was collected before and after the interventions to assess the differences in the participants’ food intake and healthy eating behaviours.
Nutrition knowledge, attitudes and practices
The questionnaire comprised fourteen questions to assess the adolescents’ dietary and nutrition knowledge, attitudes and practices and was divided into three sections: (1) The ‘Nutrition Knowledge’ section comprised six questions with 1 point for a correct answer and 0 for an incorrect answer. The maximum score was 6 points. (2) The ‘Nutrition Attitudes’ section comprised four questions; participants selected ‘agree’, ‘ambivalent’ or ‘do not agree”’ to indicate their agreement with a statement, and the options were scored from 1 to 3, respectively. For Question 7, ‘False’ was worth 1 point and ‘True’ received no points. The maximum score was 10 points. (3) The ‘Nutrition Practice’ section comprised four questions; participants selected the most appropriate answer on a three-point scale. ‘Frequently’ was worth 3 points, ‘sometimes’ was worth 2 points and ‘rarely or never’ was worth 1 point. Question 13 was scored in reverse, and the maximum score was 12 points. The details of the questionnaire can be found in Supplementary Table 2.
Dietary intake
The SFFQ had thirty-six questions on schoolchildren’s daily dietary intake, with specific questions concerning consuming three meals (breakfast, lunch and dinner), eating out, drinking sugary drinks, eating fried foods and consuming dietary supplements in the past month. The validation and reliability of the SFFQ have been demonstrated among adult women(Reference Chou, Chu and Wu12) and college students. The intraclass coefficients of repeated measurements for nutrient intake were 0·51–0·90. The SFFQ was validated with biochemical data, and the Spearman correlation coefficient was 0·31 and 0·34 for vitamin B6 and folate intake, respectively (data not shown).
Healthy eating behaviour was assessed using the Dietary Guideline of Taiwan, specifically the following nine components(Reference Lee, Huang and Chang13): wholegrain intake (servings/d), vegetable intake (servings/d), fruit intake (servings/d), dairy intake (servings/d), meat ratio, frequency of snack intake (such as salty or sweet biscuits, d/week), sugary drink intake (servings/d), fried food intake when eating out (servings/d) and frequency of eating breakfast (times/week). The meat ratio was calculated by dividing lean proteins (e.g. poultry, fish and tofu) by higher fat meats (e.g. beef, pork and lamb)(Reference Hurley, Oberlander and Merry14).
Anthropometric measurements
The participants’ body weight (kg), body fat (%), height (cm), waist circumference (cm) and handgrip (lb) were measured before and after the intervention using TANITA BC202 body composition scales, Inbody Inkids portable sonic altimeters, tape measures and the Baseline Smedley spring-type hand dynamometer. Handgrip strength was measured two times in the dominant hand. The hand dynamometer has been validated previously(Reference Güçlüöver, Kutlu and Ciğerci15,Reference Guerra and Amaral16) . The participants’ BMI was compared against the Health Promotion Administration’s recommended BMI for children and adolescents to determine if participants were underweight, had normal weight, were overweight or were obese(17). The definition of overweight and obese was a BMI greater than the 85th and 95th percentiles for gender and age, respectively, of the Taiwanese population. All measurements were completed one-on-one in March (pretest) and May (posttest), and the data were recorded by the researcher to maintain privacy.
Data analysis
Continuous variables were represented by mean ± sd, and categorical variables were represented by the numbers (percentages). All data analyses were conducted using SAS 9.4 statistical software. We used the χ 2 or Fisher’s exact test to compare the baseline characteristics in categorical variables between elementary and junior high school students. We used generalised estimating equation models to evaluate the intervention effects on nutrition knowledge, attitudes and practices; dietary quality; and anthropometrics for adolescents. Generalised estimating equations were used to analyse repeated measurements while accounting for the potential confounders. Gamma distribution with a log-link function was used for the highly skewed dependent variables. The coefficients were exponentiated to obtain a ratio and percentage increase or decrease in measurement outcomes. All models were adjusted for age, gender and region. P-value of < 0·05 was considered to be a statistically significant.
Results
Sociodemographics
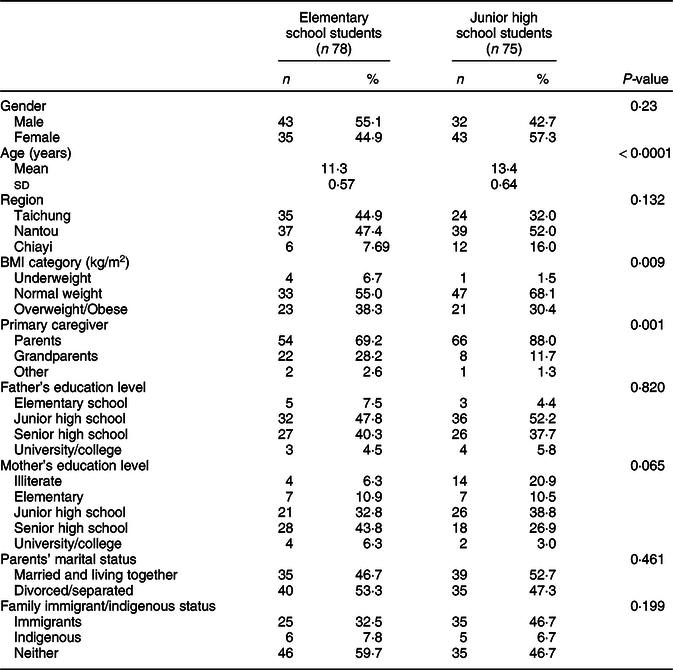
The participants’ demographic variables are presented in Table 1. The percentages of boys among the elementary and junior high school students were 55·1 % and 42·7 %, respectively. Moreover, 38 % and 30·4 % of elementary and junior high school students were either overweight or obese, respectively (P = 0·009). The primary caregivers were grandparents for 28 % and 11·7 % of elementary and junior high school students, respectively (P = 0·001). Twenty-one percentage of the participants had mothers who were illiterate, with 46·7 % of the mothers of junior high school participants being from immigrant families. Respectively, parents of 53·3 % and 47·3 % of elementary and junior high school students were divorced.
Table 1 Demographic and household characteristics of the study participants (n 153)
Anthropometric measurements
Table 2 presents the pretest and posttest anthropometric measurements. Among the elementary and junior school students, height increased by 1·01 % (P < 0·001) and 0·40 % (P < 0·001), handgrip increased by 11·6 % (P < 0·001) and 11·4 % (P < 0·001) and body fat percentage decreased by 14·8 % (P = 0·32) and 4·88 % (P < 0·001), respectively.
Table 2 Differences in anthropometric measurements between pre- and post-intervention among elementary and junior high school students (n 153)
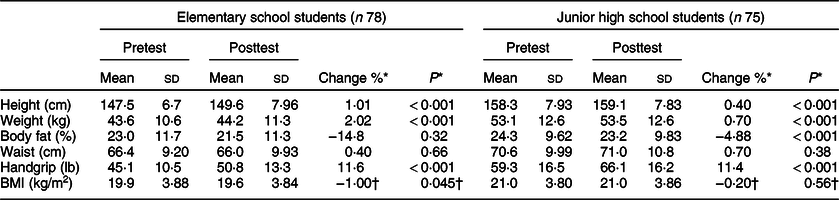
* Values were adjusted for age, gender, BMI and region using generalised estimating equations.
† Values were adjusted for age, gender and region using generalised estimating equations.
Nutrition knowledge, attitudes and practices
Elementary and junior high school students scored significantly higher on the posttest ‘Nutrition Knowledge’ survey than on the pretest survey (+5·70 %/6·18 %, P = 0·02). For ‘Nutrition Attitudes’ and ‘Nutrition Practices’, junior high school students had higher posttest scores, but the differences were not significantly different. Elementary students had lower posttest scores in ‘Nutrition Practices’ (–5·82 %, P = 0·03; Table 3).
Table 3 Differences in nutrition knowledge, attitudes and practices between pre- and posttest scores among elementary and junior school students (n 153)
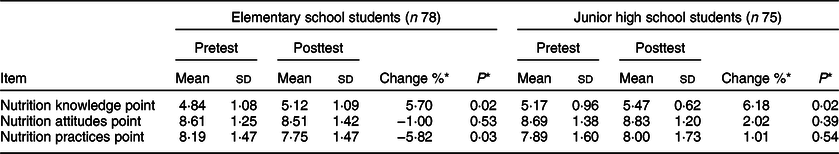
* Values were adjusted for age, gender and region using generalised estimating equations.
Dietary intake
Table 4 presents the pretest–posttest food intake and eating behaviours. Elementary and junior school students’ posttest fruit intake decreased by 22·9 % (P = 0·02) and 18·9 % (P = 0·03) servings, respectively, compared with their pretest intake, while breakfast frequency decreased by 4·88 % per week (P = 0·06) in junior school students. However, posttest intake related to snacking and fried foods when eating out was significantly lower, with snacking occasions decreasing from an average of 3·49 d to 2·74 d each week (–21·3 %, P = 0·008) and fried foods when eating out decreasing from an average of 0·41 to 0·29 servings/d (–28·8 %, P = 0·01).
Table 4 Differences in food intake and eating behaviours between pre- and posttest among elementary and junior high school students (n 143)
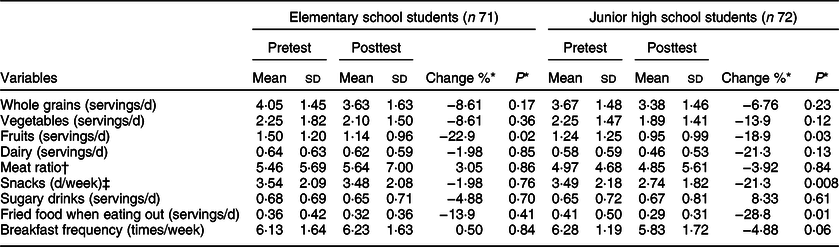
* Values were adjusted for age, gender and region using generalised estimating equations.
† The meat ratio was calculated by dividing lean proteins (e.g. poultry, fish and tofu) by higher fat meats (e.g. beef, pork and lamb).
‡ Snacks included salty or sweet biscuits.
Discussion
Our study demonstrated that after-school nutrition intervention is an effective approach for improving nutrition knowledge and reducing the intake of snacks and fried foods among adolescents, especially junior high school students. Furthermore, body fat decreased and handgrip increased in both elementary and junior high school students. Obesity is associated with socio-economic status(Reference van Ansem, Schrijvers and Rodenburg18); in neighbourhoods with low socio-economic development, overweight or obese children outnumber underweight children(Reference Evers and Hooper19,Reference Lioret, McNaughton and Cameron20) . Many studies have demonstrated a positive correlation of highly processed foods and sugary drinks with body fat percentage(Reference Schneider, Dumith and Orlandi3,Reference Costa, Del-Ponte and Assuncao21) . Therefore, reducing the intake of these foods could possibly help lower body fat in adolescents. A 9-month diet and lifestyle education programme was effective in reducing central adiposity through improvement in the nutrition knowledge and a decline in the intake of unhealthy diets in preteenagers (11–12 years)(Reference Wadolowska, Hamulka and Kowalkowska22). Body fat percentage in boys typically peaks at age 11 years and either decreases or remains steady during adolescence, whereas it continues to increase in girls throughout adolescence. Both boys and girls exhibited decreased body fat and increased handgrip after adjustments for age, BMI and region (see online supplementary material, Supplementary Table 3). Therefore, lower posttest body fat percentages in girls may reflect post interventional changes in their dietary practices, such as reduced consumption of fried food and snacks(Reference Laurson, Eisenmann and Welk23). A short period of nutrition education intervention may arouse students’ awareness of food choices, but further study is needed. In addition, we are unable to rule out the influences of normal physiological changes and physical activity.
Our findings indicated that nutrition knowledge improved following this short-term ASNE programme, whereas attitude and practices did not. A US study on short-term nutrition intervention for 4th grade students indicated that after four nutrition education sessions, the intervention group’s scores regarding attitude, self-efficacy, preference and knowledge of vegetables were significantly increased (P < 0·001)(Reference Wall, Least and Gromis24). An upward trend was noted in junior high school students’ nutrition attitudes and nutrition practices posttest survey scores but not in elementary school students, possibly owing to the students’ attentiveness during the programme sessions. Furthermore, no discernible change in attitudes and practices was observed despite an increase in knowledge.
Lower fruit intake was noted in both groups. A systematic review indicated that fruit consumption increased with multicomponent interventions and at least some parental involvement, but a limited effect was observed with a nutrition education programme only(Reference Van Cauwenberghe, Maes and Spittaels25). The decrease in fruit intake observed in our study may be due to the following reasons. First, fruits are usually prepared by primary caregivers in Taiwanese families, but our ASNE programme did not include participants’ primary caregivers. Second, fruits are costly, and consumption is affected by seasonal variation. We cross-validated with the question about the frequency of fruit intake in the past week of pre- and post-intervention, and the frequency of fruit intake was not significantly different. This may indicate that these participants have the same eating behaviour, but the lower intake might be due to personal preferences affected by seasonal variation. Third, the SFFQ had three questions regarding fruit intake, and the students may have overestimated their fruit intake in their responses in the first test. Moreover, the frequency of breakfast consumption was significantly low among junior high school students. Participants ate breakfast out approximately 4 d/week. Major reasons for skipping breakfast were lack of hunger, time and money (data not shown). For adolescents, eating nutritious food mostly depends on food availability, affordability and accessibility in the family.
Eating with family can have a positive correlation with vegetable and fruit intake(Reference Draxten, Fulkerson and Friend26,Reference Watts, Loth and Berge27) , and our data indicated that 62·8 % junior high school students had family dinners (data not shown). Parents or caregivers play a vital role in cultivating children’s dietary habits. They can provide a homemade healthy meal to their children that can increase the likelihood of such children meeting dietary recommendations(Reference Draxten, Fulkerson and Friend26,Reference Watts, Loth and Berge27) . Thus, parents and home circumstances may be significant factors affecting the participants’ vegetable intake. Junior high school students’ snacking and fried food intake were also significantly reduced, suggesting that the ASNE programme positively influenced the food preferences of adolescents with high autonomy. However, we cannot rule out the possibility of deliberate underreporting of unhealthy food intake in the posttest. In other nutrition education programmes for schoolchildren, snacking in the intervention group was lower than that in the control group, possibly because students were replacing high-energy foods and sugary drinks with vegetables and fruits or because when given a choice, they opted for healthier snacks(Reference Gallotta, Iazzoni and Emerenziani28–Reference Matvienko30). Dunton et al.’s study on elementary school students’ nutrition education programmes reported that students’ posttest nutrition knowledge and fruit and vegetable intake improved significantly and that their intake of sodas and highly energetic food declined(Reference Dunton, Liao and Grana31). This is probably because nutrition education changes students’ dietary practices by increasing their nutrition-related knowledge.
One retrospective study argued that nutrition education success rates could be increased if the programme applied could continue for 5 months and focused on three goals or fewer(Reference Murimi, Kanyi and Mupfudze32). The current study lasted for 3 months, which was not sufficient to familiarise the students with the importance of diet and health and to result in lasting changes in their dietary practices. The short duration may therefore be a possible factor in the lack of improvements in dietary intake. Furthermore, the parents’ nutrition-related knowledge, attitudes and practices were major factors that affected the children’s diets. However, this study did not offer nutrition education to parents or other primary caregivers. In general, our study demonstrated improvement in the youth self-efficacy of healthy dietary choice on the snack and fried food intake but not for fruit and breakfast intake, which require parental inputs.
This study has several strengths. First, our tailored nutrition programme was focused on both elementary and junior high school in an after-school setting, which allowed us to compare the influence of nutrition education between different age groups, whereas related studies have focused on a single demographic. Second, the nutrition intervention was implemented and integrated into a social welfare after-school tutoring system; this allowed us to provide nutrition-related services such as food aid (bread and powdered milk) to economically disadvantaged students.
Limitations
This study has some limitations. First, the study cohort was limited to students in Taiwan’s central and southern regions and the food environments therein. Therefore, we were unable to compare the results with those for adolescent students in other regions. Second, the diets of schoolchildren are mostly controlled by their primary caregivers to whom the nutrition education programme could not be extended. This may be a contributing factor to the difficulty in changing the dietary practices of schoolchildren. Nevertheless, improvements were noted in nutrition knowledge, and intake of snacks and fried foods was reduced. Third, we did not recruit a control group in this community-based study. Therefore, we are unable to rule out the effect of nature on physical development, seasonal variation in food intake and other changes in school and community environment.
Implications for research and practice
The inclusion of nutrition education into after-school curriculums can help economically disadvantaged schoolchildren and adolescents gain nutrition knowledge and subsequently improve their dietary behaviour. These improvements would benefit their development and could potentially affect future health condition.
Acknowledgements
Acknowledgements: We thank Prof Meei-Shyuan Lee, who develops and provides the semi-quantitative FFQ for collecting dietary information; Boyo Social Welfare Foundation, which is responsible for arranging the participant recruitment. Financial support: This study was supported by China Medical University, Taiwan (Grant No: CMU107-N-27). The sponsor of the study had no involvement in study design, data collection, analysis and interpretation, the writing of the report, and the decision to submit the paper for publication. Conflict of interest: None. Authorship: P.Y.S. and Y.C.H. designed the study, collected, analysed and interpreted the data; Y.T.C.L. and Y.C.H. provided data interpretation; P.Y.S., Y.T.C.L., Z.B.C. and Y.C.H. wrote the paper; Y.C.H. has primary responsibility for the final content. All authors read and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving study participants were approved by the Central Regional Research Ethics Committee of the China Medical University (CRREC-107–086). Written informed consent was obtained from all subjects/patients.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980020004218







