New daily persistent headache (NDPH) is a persistent headache (greater than 3 months) that is clearly remembered with pain becoming continuous and unremitting within 24 hours according to the International Classification of Headache Disorders 3rd edition. 1 It may be migraine or tension-type-like or have elements of both. Prognosis is unpredictable and two outcomes may be seen: a self-limiting subtype that resolves within several months without therapy or a refractory subtype that is resistant to treatment. 1 The refractory subtype is challenging, and there is no established treatment for refractory NDPH since this entity remains poorly understood.
Two patients presented to the headache clinic with NDPH and were treated with peripheral nerve blocks (NB).
Case 1: A 41-year-old right-hand-dominant female dentist presented with a 6-month history of continuous occipitotemporal pressure and stabbing headaches associated with photophobia and phonophobia. The onset of her headaches developed on a specific day after a suspected upper respiratory tract viral infection. She recovered fully from the infection in 2 weeks. Acetaminophen and ibuprofen provided no relief for the headaches. Her medical history was significant for menstrual-related migraine occurring once a month.
Case 2: A 19-year-old right-hand-dominant female student presented with a 4-month history of continuous occipitotemporal pressure headaches without photophobia, phonophobia, nausea, or vomiting. The onset of her headaches developed upon waking one morning and it became unremitting. She denied any recent trauma, infection, surgery, travel history, or sick contact. Over the counter analgesics provided no relief. Her medical history was significant for anxiety with no prior history of headaches.
Their headaches were not associated with positional change or worsening with Valsalva maneuvers. Both patients denied other neurological, systemic, or rheumatological symptoms. They were reluctant to take oral medications in fear of systemic side effects. Their neurological examinations were unremarkable with the exception of tenderness on palpation in the nerve distribution supplied by the greater and lesser occipital and auriculotemporal nerves bilaterally with superimposed cutaneous allodynia. Magnetic resonance imaging of their heads with gadolinium was remarkable. They were diagnosed with NDPH based on their clinical presentation.
NB without steroids were suggested based on the examination finding and their preference of a therapy with minimal systemic side effect. Bupivacaine 0.5% (5 mg/ml) was injected to the greater (3 ml each side, 6 ml in total), lesser (2 ml each side, 4 ml in total), occipital nerves, auriculotemporal nerves (1 ml each side, 2 ml in total), bilaterally once a week for 4 weeks, and then once a month for 3 months (Figure 1). Pain freedom was achieved within 15 minutes of injections. Response was sustained weekly during their first 4 sets of weekly injections and only a mild re-emergence of pain 3 to 4 days before the next set of injections when transitioned to monthly injections. Subsequent injections provided a similar response for the next 3 months. Both patients had in-person assessments with their follow-up injections (weekly for 4 weeks followed by monthly for the next 3 months).
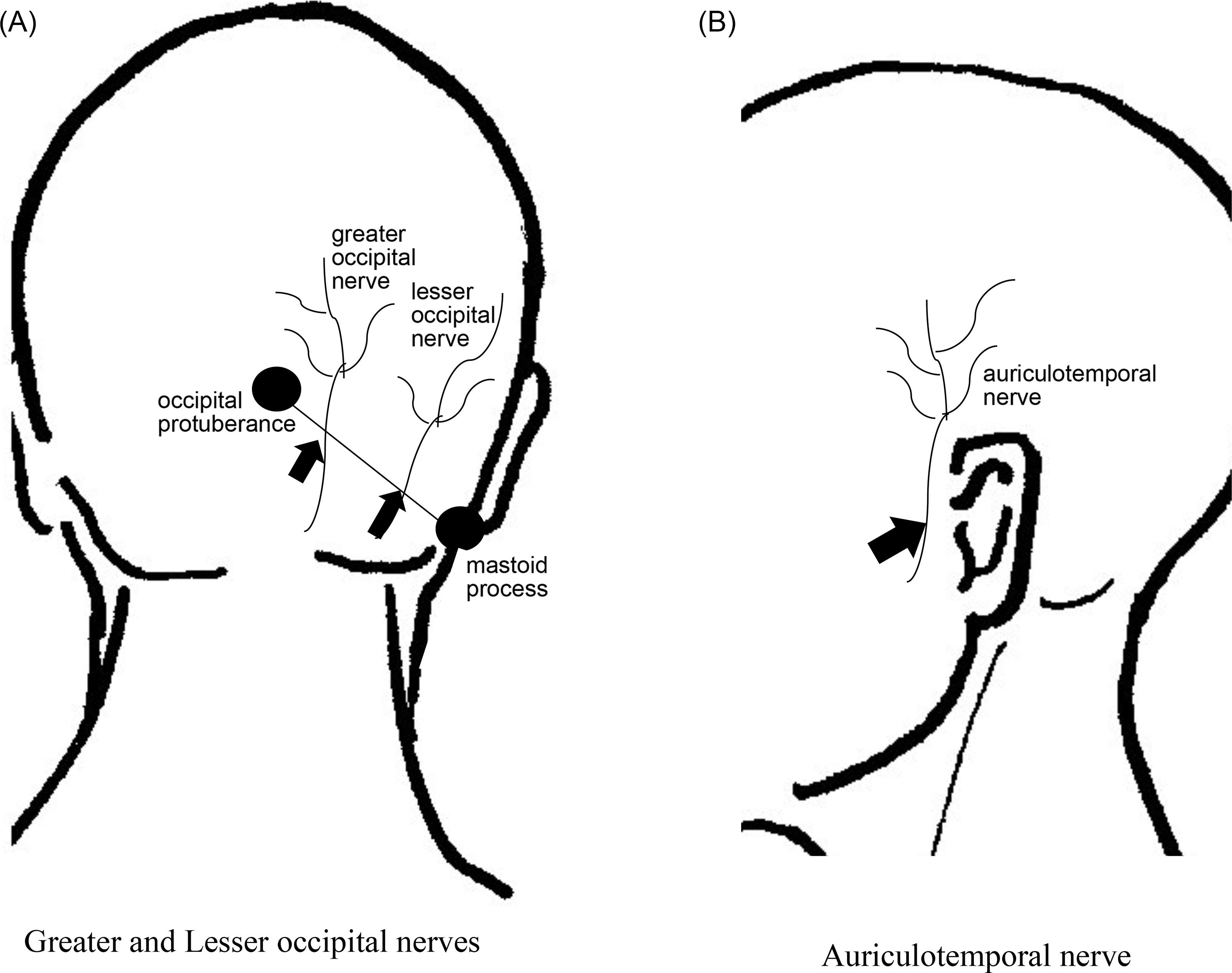
Figure 1: Landmark and Injection sites (arrows)
1. Greater occipital nerve: 2/3 from mastoid process to occipital protuberance
2. Lesser occipital nerve: 1/3 from mastoid process to occipital protuberance
3. Auriculotemporal nerve: 1.5 cm anterior to the ear at the level of the tragus
Although the exact pathophysiology of NDPH remains unclear, previous studies have shown that NDPH can be associated with recent history of infections (case 1), surgery, trauma, stressful event, or it could be completely spontaneous (case 2). Reference Rozen2 Rozen and Swidan proposed that NDPH might be related to the release of proinflammatory cytokines resulting in central nervous system inflammation. Reference Rozen and Swidan3 It may also be related to a hypersensitized state that was set off from an inciting event. The response to NB in patients with NDPH has been previously reported; however, no guidance has been provided from previous literature on who is appropriate and suitable to receive NB as a treatment for NDPH.
In a retrospective study, Reference Robbins, Grosberg, Napchan, Crystal and Lipton4 Robbin et al. identified 23 NDPH patients who reported a decrease in pain severity with NB. It provided a 60% acute response consistent with at least 1 day of decrease in pain intensity. However, no information reported on how long the NB lasted for. In a retrospective review, Reference Hascalovici and Robbins5 NB were utilized to treat headaches in older adults. The headache disorders included migraine, trigeminal autonomic cephalgias, occipital neuralgia, and NDPH. Patients received on average 4 NB between 1 and 48 months. Treatment response was seen between 50 and 81% for all the subgroups and specifically 2 out of the 3 (67%) NDPH patients had a positive response (reduction in headache days). However, there was limited information reported on the subgroups including patients' history, examination finding, and the number of days in headache reduction. In the pediatric population, Puledda et al. reported that improvement was seen in 13 of 22 (59%) patients with a diagnosis of NDPH who received greater occipital nerve block using 1% lidocaine and 2 patients had sustained response greater than 3 months. Reference Puledda, Goadsby and Prabhakar6 Methylprednisolone was mixed with the lidocaine and no patients received local anesthetics alone.
NB were recommended in the two cases presented because tenderness was elicited on palpation in the nerve distribution supplied by the bilateral greater and lesser occipital and auriculotemporal nerves. The response to NB appeared to be effective and sustained irrespective of their phenotype. Early intervention should be considered because it can be hypothesized that the reduction of afferent transmission from local anesthetics reduces the afferent transmission at the first synapse of the nociceptive pathways which may indirectly decrease the risk of central sensitization and in breaking the pain cycle which leads to chronic pain.
The evaluation of these two cases point to the consideration of NB as a treatment option for refractory NDPH. The presence of wearing-off of NB prior to next treatment is suggestive of ongoing NB benefit; however, the duration of the analgesic effect from NB remains unpredictable. The advantage of NB is its tolerability and side-effect profile. The use of NB can minimize the risk of developing medication overuse headache which is often comorbid in NDPH patients. A clue to predict response to NB may be elicited on examination based on tenderness on palpation in the nerve distribution (for example, occipital, auriculotemporal supraorbital, and supratrochlear nerves); hence, local tenderness as a selection criterion should be considered in future trials. Larger trials should be conducted to evaluate the efficacy of NB in NDPH patients.
Conflicts of Interest
Dr. Tommy Lik Hang Chan has no conflicts of interest (financial or nonfinancial) to disclose relevant or pertain to this study. Dr. Tommy Lik Hang Chan is on the advisory board for AbbVie Inc., Eli Lilly, Novartis, and Aralez Pharmaceuticals Canada. Dr. Tommy Lik Hang Chan has received grant support for education (no personal compensation) from Teva Pharmaceutical industries. Dr. Tommy Lik Hang Chan has received honoraria from Aralez Pharmaceuticals Canada, AbbVie, Lundbeck, and Novartis.
Consent to Participate/Consent for Publication
Informed written consent was obtained from the patients.
Availability of Material
The material analyzed during the current case is available from the author on a reasonable request.
Authors’ Contributions
Dr. Tommy Lik Hang Chan assessed and examined the patients. He wrote the manuscript.



