A 6-year-old male suffered a ground-level fall and head injury. He developed seizures shortly after arriving in the emergency department and needed intubation for airway protection. Multiple intubation attempts were required before successful passage of the endotracheal tube. He was extubated the following day and developed persistent post-extubation stridor. Laryngoscopy several days later demonstrated subglottic stenosis (SGS) (Figure 1). He underwent successful endotracheal balloon dilation (Figure 2) and was discharged with resolution of stridor.
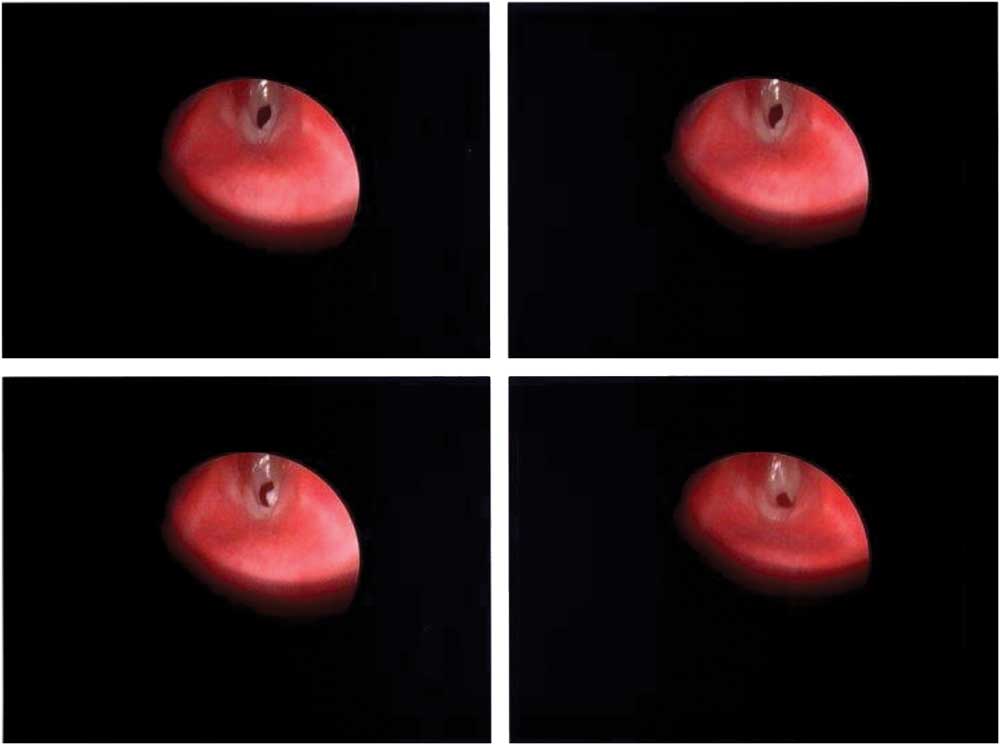
Figure 1 Endoscopic view of subglottis demonstrating subglottic stenosis.
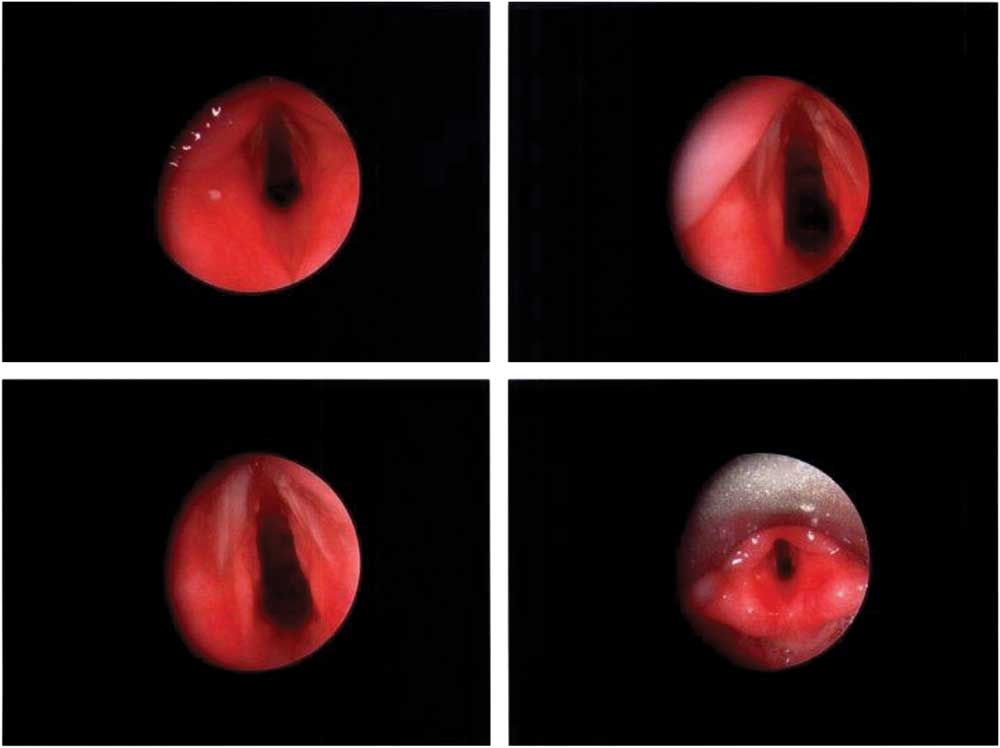
Figure 2 Post-procedural endoscopic view of subglottic space.
SGS is an obstructive airway lesion at the level of the cricoid cartilage and can present as a life-threatening airway emergency. Acquired SGS is differentiated from congenital by a history of trauma or instrumentation, and more severe symptoms. Iatrogenic injury from endotracheal intubation accounts for 90% of acquired SGS cases in pediatric patients, with an incidence ranging from 1% to 12% after intubation.Reference Flint 1 - Reference Manica, Schweiger and Maróstica 3 Symptoms of SGS may present after a latent period and can include biphasic stridor, increased work of breathing, abnormal phonation, dysphasia, recurrent croup, or prolonged upper respiratory infections.Reference Flint 1
Management options include endoscopic or open surgical approaches, with success dependent on acuity and degree of stenosis.Reference Avelino, Maunsell and Jubé Wastowski 4 , Reference Maresh, Preciado and O’Connell 5 In the event of a failed airway due to SGS, the optimal mode of transtracheal oxygenation in patients under 8 years old remains controversial, with needle tracheotomy or surgical tracheotomy below the cricoid ring as the preferred methods due to the underdeveloped cricothyroid space.Reference Law, Broemling and Cooper 6
Competing interests: None declared.
Keywords: subglottic stenosis, pediatric, intubation




