Food insecurity (FI) is defined as limited access to adequate healthy food because of insufficient household money or other resources(Reference Coleman-Jensen, Gregory and Singh1). According to a survey in 2018, about 11·1 % of US households were food insecure at some point in the year(Reference Coleman-Jensen, Rabbit and Gregory2). FI is a major public health concern with a variety of adverse medical outcomes such as depression, diabetes and CVD(Reference Leung, Epel and Willett3–Reference Saiz, Aul and Malecki5). Research has shown an association between elevated FI and obesity among women(Reference Townsend, Peerson and Love6–Reference Wilde and Peterman9). Other studies in men were limited and the results were inconsistent(Reference Townsend, Peerson and Love6,Reference Wilde and Peterman9–Reference Larson and Mary11) . Few studies have focused on young adulthood, a critical time period for the transition to self-sufficiency and the development of obesity(Reference Suchindran, North and Popkin12). Research has shown that young adults (18–35 years of age) are more vulnerable to weight gain than all other age groups(Reference McTigue, Garrett and Popkin13,Reference Sheehan, DuBrava and DeChello14) . In addition, the increasing risk of metabolic syndrome and CVD among young adults worsens through the life course(Reference Truesdale, Stevens and Lewis15). Thus, weight gain prevention among young adults would have significant implications for long-term health benefits.
Although there has been much evidence indicating the link between FI and obesity(Reference Townsend, Peerson and Love6–Reference Larson and Mary11), the mechanism through which this occurs remains unclear(Reference Franklin, Jones and Love16,Reference Rogers, Kegler and Berg17) . Several studies indicated that individuals experiencing FI tend to alternate between hunger and consumption of energy-dense unhealthy foods(Reference Widome, Neumark-Sztainer and Hannan18,Reference Tester, Lang and Laraia19) to avoid the higher cost of healthy foods such as lean meat, fruits and vegetables(Reference Drewnowski20). This compensatory dietary pattern could lead to cyclical weight gain(Reference Seligman and Schillinger21,Reference Ambrosini22) , while other studies found that the availability of unhealthy foods was associated with obesity but did not play a mediating role(Reference Kowaleski-Jones, Wen and Fan23). Therefore, the potential mediating role of diet healthfulness (DH) between FI and obesity is worth further investigation.
BMI has been the most commonly used tool to determine obesity(Reference Townsend, Peerson and Love6–Reference Suchindran, North and Popkin12,24) . However, this method fails to distinguish between fat and fat-free mass(Reference Fedewa, Brett and Michael25). In fact, research has found that waist circumference (WC), a way to assess abdominal obesity, is a more accurate method to measure body composition and predict obesity-related health risk(Reference Fedewa, Brett and Michael25,Reference Janssen, Peter and Robert26) . Thus, both BMI and WC were used to measure overall obesity and abdominal obesity, respectively, in the current study.
The objective of the current study was to clarify the relationship between FI and WC, FI and BMI among young adults aged 18–35 years using data from The National Health and Nutrition Examination Survey, 2011–2016. In addition, the study examined whether biological sex modified the main effects, and whether DH played a mediating role in the relationship.
Methods
Study sample
The National Health and Nutrition Examination Survey is a cross-sectional representative survey conducted by the National Center for Health Statistics and the Centers for Disease Control and Prevention(27) that uses a complex, multistage probability design to sample the civilian, non-institutionalised population in the USA. Our study combined data from the 2011–2012, 2013–2014 and 2015–2016 National Health and Nutrition Examination Survey cycles, the most recent survey years for FI data. During these cycles, Hispanics, non-Hispanic Asians, non-Hispanic Blacks, older adults and low-income Whites/others were oversampled by the design. Full details of the study design, recruitment and procedures are available at the Department of Health and Human Services(27). Out of the total sample (n 29 902), 5640 participants were aged 18–35 years; 17·25 % of them (n 973) were excluded due to missing values of FI, BMI, WC, DH or general health, resulting in 4667 participants in the final sample.
Measures
Food insecurity
The 10-item US Food Security Survey Module was used to assess adult FI status(Reference Bickel, Nord and Price28). It asked about the size of meals, skipping meals and not eating for a whole day. Similar to previous studies, an affirmative answer on at least one of these ten items was defined as ‘food insecurity’(Reference Portela-Parra and Leung29,Reference Gundersen and Ziliak30) .
Body mass index
BMI (kg/m2) was calculated as weight in kilograms divided by height in meters squared and then rounded to one decimal place.
Waist circumference
WC (cm) was taken to the nearest 1 mm, measured at the level of iliac crest in the Mobile Examination Center(27). For males, WC larger than 102 cm was defined as abdominal obesity, and for females, WC larger than 88 cm was defined as abdominal obesity(Reference Klein, Allison and Heymsfield31).
Diet healthfulness
The potential mediating variable was the self-appraised healthfulness level of one’s own diet. Participants were asked ‘In general, how healthy was your overall diet over the past 12 months?’ The ratings were made on a five-point scale from excellent to poor (1: excellent, 2: very good, 3: good, 4: fair, 5: poor).
Biological sex
Biological sex was self-reported by participants as male or female.
Covariates
Other variables including age, race (Mexican American, other Hispanic, non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, other), country of birth (US v. other countries), self-reported general health (1: excellent, 2: very good, 3: good, 4: fair, 5: poor) and family poverty-to-income ratio (<=1·3 v. >1·3) were included in the analyses as potential confounders. The cutoff of 1·30 for family poverty-to-income ratio was chosen because it is the eligible cutoff for federal nutrition support programmes such as the Supplemental Nutrition Assistance Program and the National School Lunch Program(Reference Kaur, Lamb and Ogden32).
Statistical analysis
Univariate analyses were performed to describe every variable of interest for the entire sample and for each biological sex. Continuous variables, including age, BMI and WC, were described with weighted means and sd. Categorical variables, including race, country of birth, FI, DH, general health and income-to-poverty ratio, were described with unweighted frequencies and weighted percentages.
Bivariate analyses of the covariates with FI, BMI and WC were done separately. Chi-square tests were conducted to test the relationships between FI and categorical covariates (i.e., race, biological sex, country of birth, general health and income-to-poverty ratio). Simple linear regression tests were conducted to test the relationships between BMI and all the covariates, and also WC and all the covariates. The association between FI and age, BMI and WC was examined by simple linear regression tests as well.
Two multiple linear regression models controlling for potential confounders were used to assess the association between FI and BMI, and also FI and WC in the overall sample. Diagnostic tests were conducted for the normality assumption, outlier detection and multicollinearity. Interaction terms of biological sex and FI were then created and added to the models to test if biological sex was an effect modifier. Stratified analyses within each biological sex were also conducted.
We further adjusted for education and marital status to assess the main effects of FI on BMI and WC for the entire sample and for each biological sex as sensitivity analyses. We also examined the dose–response relationships between FI and BMI, and FI and WC using tests for trend depending on the number of affirmative answers in the Food Security Survey Module (full security: 0, marginal food security: 1–2, low food security: 3–5, very low food security: 6–10) for males and females. Tests for trend were conducted using simple linear regression models stratified by biological sex.
Structural equation modelling was used to explore if the effects of FI on BMI and FI on WC were mediated by DH. Structural equation modelling is an approach to examine both the direct (c’) and indirect effects (a * b) of FI on BMI and FI on WC. Figure 1 provided the basic theoretical forms of the structural equation models tested. All of the models were adjusted for age, race, country of birth, general health and family income-to-poverty ratio. For all analyses, survey sampling weights were applied to take into account the complex sampling strategy of the National Health and Nutrition Examination Survey and increase the representativeness of the sample. We used a P value < 0·05 to assess significance. All analyses were performed using SAS 9·4 (SAS Institute).
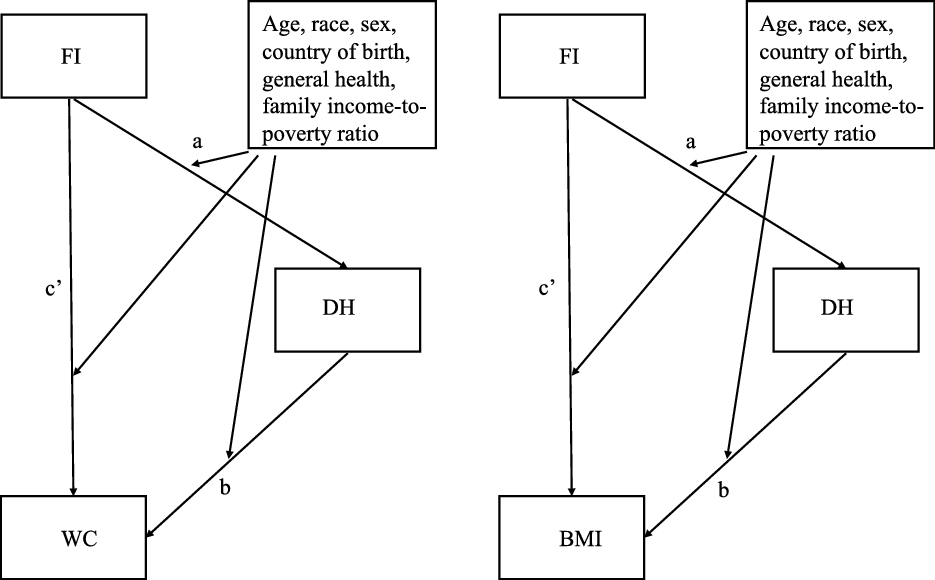
Fig. 1 Mediation effects of DH between FI and BMI, and FI and WC. DH, diet healthfulness; FI, food insecurity; WC, waist circumference
Results
The weighted average age of the entire sample (n 4667) was 26·33 years (sd = 0·14 years). Females comprised 48 % of the sample and males 52 %. The descriptive statistics for the entire sample and for each biological sex are listed in Table 1. The WC of females was lower than that of males (P < 0·001), while the BMI was higher (P = 0·049). The prevalence of abdominal obesity among females was much higher than that among males (P < 0·001). Males had higher income-to-poverty ratio than females (P = 0·002). Females reported better DH than males (P = 0·044). The descriptive statistics for people who were food secure and food insecure are listed in Table 2. People who were food secure comprised 66 % of the sample and food insecure 34 %. We further compared our variables of interest between eligible participants (i.e., participants aged 18–35 years) who were included and those excluded (due to missing values) from the analyses. The results indicated that those who are younger, non-Hispanic White, males, born in the USA and with higher income-to-poverty ratio were more likely to be included (see online supplementary material, Supplemental Table 1).
Table 1 Characteristics of participants aged 18–35 years by biological sex, NHANES, 2011–2016
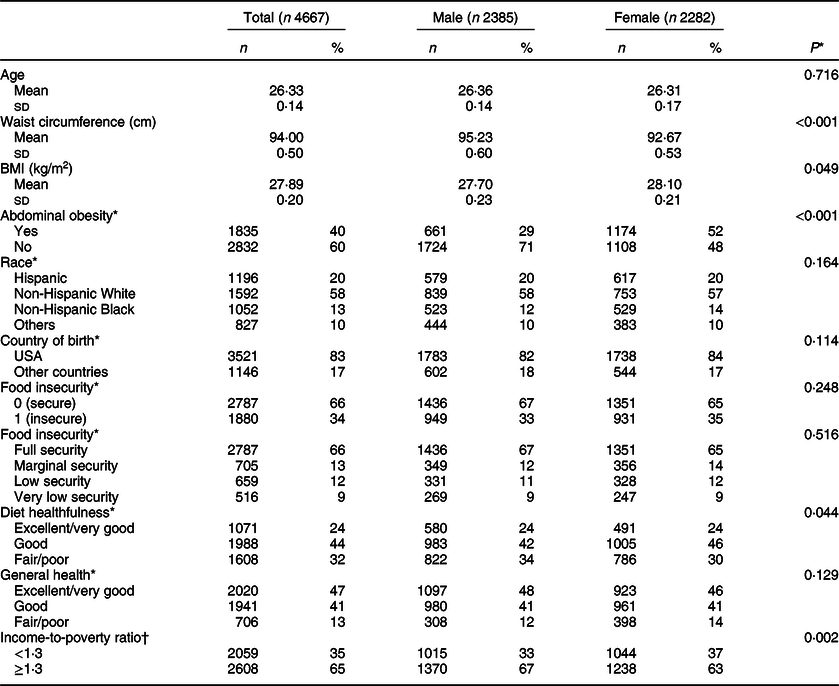
NHANES, National Health and Nutrition Examination Survey.
* P values were generated using chi-square tests or t-tests.
† The weighted % uses the analytic weights to generate population-based estimates of prevalence for the included sample. Numbers may not sum to 100 % due to rounding.
Table 2 Characteristics of participants aged 18–35 years by food insecurity, NHANES, 2011–2016
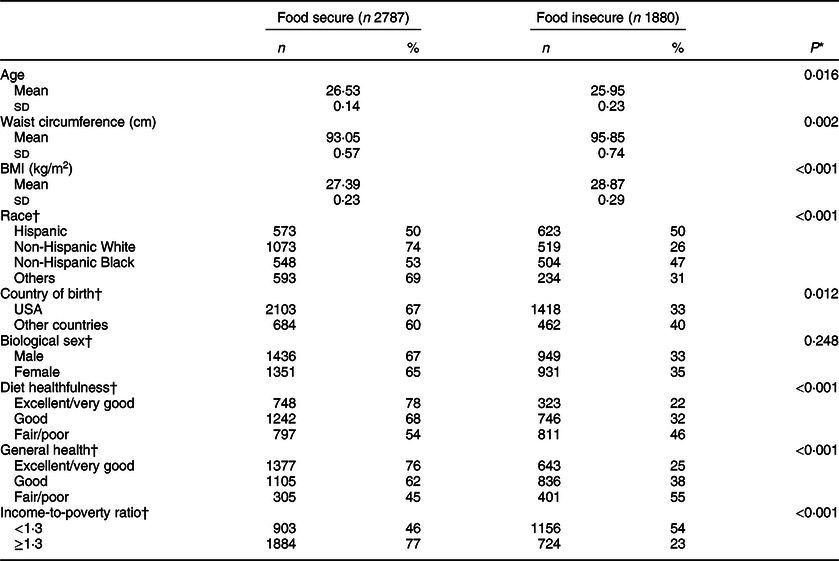
NHANES, National Health and Nutrition Examination Survey.
* P values were generated using chi-square tests or t-tests.
† The weighted % uses the analytic weights to generate population-based estimates of prevalence for the included sample. Numbers may not sum to 100 % due to rounding.
Results of bivariate analyses between FI and covariates are as follows (Table 2): Simple linear regression tests showed that FI was associated with age (P = 0·016), BMI (P < 0·001) and WC (P = 0·002). Specifically, people with FI were younger, had larger WC and higher BMI. Chi-square tests showed that FI was associated with race (P < 0·001). Specifically, 50 % of Hispanic and 47 % of non-Hispanic Black participants were food insecure, while 26 % of non-Hispanic White and 31 % of others were food insecure. People who were born in other countries (40 %) were more likely to be food insecure compared with people who were born in the USA (33 %; P = 0·012). A greater percentage of people with lower income-to-poverty ratio (54 %) were food insecure compared to people with higher income-to-poverty ratio (23 %; P < 0·001). FI was also associated with DH (P < 0·001). Specifically, people who reported worse DH were also more likely to be food insecure: 22 % of excellent/very good, 32 % of good and 46 % of fair/poor DH. People who had worse general health were also more likely to be food insecure (P < 0·001; 25 % of excellent/very good, 38 % of good and 55 % of fair/poor general health).
Results of bivariate analyses between BMI, WC and covariates by simple linear regressions were as follows: Both BMI and WC were associated with age (P < 0·001), country of birth (P < 0·001), race (P < 0·001) and general health (P < 0·001), but not with family income-to-poverty ratio (WC: P = 0·710; BMI: P = 0·551).
The multiple linear regression models between FI and BMI, and FI and WC controlled for age, race, biological sex, country of birth, general health and family income-to-poverty ratio. No outliers were excluded in the analysis, and there was no multicollinearity detected in the model (min (Tolerance) = 0·89, max (VIF) = 1·12). Among the total sample, the data were relatively consistent with an association between FI and BMI (P = 0·052), and FI and WC (P = 0·088) (Table 3). Also, when the interaction terms of FI and biological sex were added into the models, we found interaction effects of FI and sex for both BMI (P = 0·007) and WC (P = 0·031). Specifically, FI was associated with both BMI (P = 0·012) and WC (P = 0·045) among females (Table 3). Females who were food insecure had BMI 1·16 (95 % CI 0·27, 2·05) kg/m2 higher on average than those who were food secure and had WC 2·09 (95 % CI 0·05, 4·14) cm larger. However, the data did not support similar relationships among males, neither the association between FI and BMI (P = 0·568) nor WC (P = 0·462). Additional adjustments for education and marital status did not change the results (see online supplementary material, Supplemental Table 2), but since the values were largely missing for these two variables, we did not include them in the main results. The results of the dose–response relationships between FI and BMI, and FI and WC for each biologicals sex were shown in Table 4. The effect estimates indicated trend effects between FI and BMI, and FI and WC among females, but not among males.
Table 3 Weighted multiple linear regression analysis stratified by sex predicting the association between food insecurity and BMI, and food insecurity and waist circumference*
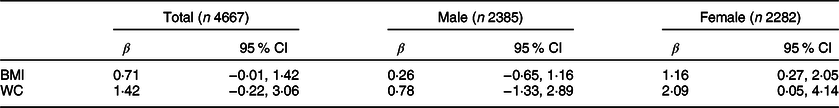
WC, waist circumference.
* All the regression models were adjusted for controlling confounders (age, race, country of birth, general health and income-to-poverty ratio). Biological sex was additionally adjusted for the total model.
Table 4 Dose–response relationship between FI and BMI, and FI and WC for males and females
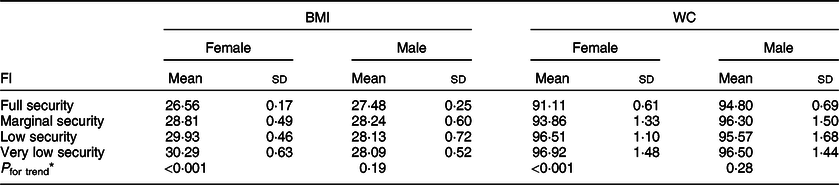
FI, food insecurity; WC, waist circumference.
* Simple linear regression was used to calculate P for trend.
Given the associations between FI and BMI, and FI and WC among females, we further conducted mediation analyses of FI and BMI, and FI and WC among females with two structural equation models. The results (Table 5) indicated that DH was a mediator between FI and BMI (P = 0·003). The total effect of FI on BMI (c = 0·93, 95 % CI 0·30, 1·56) could be decomposed into a direct effect of FI on BMI conditioning on DH (c’ = 0·80, 95 % CI 0·17, 1·42) and an indirect effect through DH (a * b = 0·14, 95 % CI 0·05, 0·23); 14·64 % (95 % CI 1·57 %, 27·70 %) of the total effect between FI and BMI could be explained by DH. DH was also a mediator between FI and WC (P = 0·003). The total effect of FI on WC (c = 1·54, 95 % CI 0·09, 2·99) could be decomposed into the direct effect of FI on WC conditioning on DH (c’ = 1·23, 95 % CI −2·11, 2·67) and the indirect effect through DH (a * b = 0·31, 95 % CI 0·10, 0·51); 20·01 % (95 % CI −1·89 %, 41·91 %) of the total effect between FI and WC could be explained by DH. Females who were food insecure had poorer DH on average and thus had higher BMI and larger WC. Confounding covariates, including age, race, country of birth, general health and family income-to-poverty ratio, were adjusted in the model.
Table 5 Total, direct and mediation effects for BMI and WC among females*
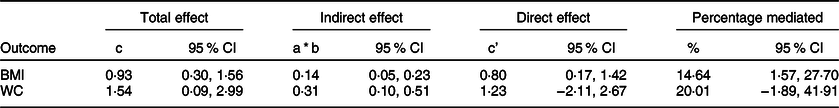
WC, waist circumference.
* All the structural equation models were adjusted for controlling confounders (age, race, country of birth, general health and income-to-poverty ratio).
Discussion
The current study used BMI and WC as measurements of overall obesity and abdominal obesity, respectively, to characterise the relationship between FI and obesity of young adults aged 18–35 years in a large, nationally representative sample. Specifically, we examined whether biological sex moderated the relationship and whether DH mediated the relationship.
Our study found positive relationships between FI and BMI, and FI and WC among young adults when controlling for age, race, country of birth, general health and family income-to-poverty ratio. The results are comparable to previous studies(Reference Wu, Lin and Hsieh33,Reference Souza and Marín-León34) , but the P-values are not particularly low. This is likely due to limited power and differences in study age group, sample size, study design, FI measurement or selection of potentially confounding variables. In addition, our findings indicated that biological sex played a moderating role between FI and BMI, and FI and WC among this population. Specifically, there was a positive association between FI and both BMI and WC among females, which was consistent with previous research(Reference Townsend, Peerson and Love6-Reference Wilde and Peterman9,Reference Gooding, Walls and Richmond35) . There was no association of such among males. We also found positive dose–response relationships between FI and BMI, and FI and WC among females. In other words, for females, the greater the severity of FI, the higher their BMI and the larger their WC on average. These dose–response relationships were not detected among males.
These results suggest that young male and female adults act differently in the face of FI(Reference Hernandez, Reesor and Murillo10). Females were more likely to feed themselves unhealthy food in response to FI. Yet males were less likely to do so. It also suggests that alleviating the severity of FI for females, even if not being able to fully eliminate FI, could provide benefits for maintaining healthy weight. The sex difference regarding FI and obesity could be caused by the fact that females were in general more responsible for food selection and preparation for the family(Reference McIntosh and Zey36), and they are thus more aware of food scarcity in the household and react accordingly. It could also be caused by the stress induced by FI(Reference Martin, Maddocks and Chen37), and females are more likely to increase food intake when under stress compared with males(Reference Epel, Lapidus and McEwen38,Reference Al-Asadi39) , especially high fat and sweet foods(Reference Habhab, Sheldon and Loeb40). Yet it is noteworthy that the vast majority (71 %) of young male adults in this population were below the cutoff of WC recommended by American Heart Association for elevated cardiometabolic risk(Reference Klein, Allison and Heymsfield31). On the other hand, a majority (52 %) of females in this population had met the cutoff and were at high risk of obesity-related health conditions(Reference Janssen, Peter and Robert26,Reference Beydoun and Wang41) . The average BMI among females (28·10 kg/m2) was also higher than that of males (27·70 kg/m2) in this population.
In the current study, DH was a mediator between FI and WC among females. In other words, the effects of FI on BMI, and FI on WC among females were mediated by DH. Specifically, females with FI had poorer self-reported DH, and females with poorer self-reported DH had higher levels of BMI and WC. This finding was in line with previous studies testing the mediating role of dietary behaviour between FI and obesity among youth(Reference Wu, Lin and Hsieh33,Reference Smith and Richards42) . This suggests that improving diets would be beneficial for people with FI to maintain healthy weight.
The implications of these findings are twofold. First, community-based DH education should be implemented to promote self-awareness of adopting healthy eating habits such as eating breakfast regularly, avoiding snack consumption and sugary drinks among people with FI, especially females. Second, healthcare providers should try to identify people who are at risk or are currently experiencing FI and provide them with appropriate social services resources such as applying for federal nutrition assistance programmes to get nutritious and sufficient food and thus maintain healthy weight.
There were several limitations in the current study. The current study was cross-sectional study, and therefore causal relationships between FI and BMI, and FI and WC could not be demonstrated. The cross-sectional study did not account for the duration of FI, which is also important for the development of obesity(Reference Wells, Evans and Beavis43). In addition, the cross-sectional approach could result in substantial bias in the mediation analysis(Reference Maxwell, Cole and Mitchell44). The mediator identified in the current study may not be a mediator in longitudinal studies(Reference Maxwell, Cole and Mitchell44). Thus, longitudinal studies examining the long-term effect of FI on BMI and WC and the potential mediating effect of DH are needed in the future. Additionally, some potential confounders, such as education status, marital status and number of children, were largely missing in the dataset and, thus, were not controlled for in the analyses – yet, sensitivity analyses controlling for education and marital status showed the same results. Behavioural variables regarding participants’ physical activities and smoking and drinking behaviours were not controlled for in our analyses and should be included in future studies as well. Furthermore, since young adults with missing values for variables of interest were excluded from the analysis, participants included and excluded from the analyses had different socio-demographic characteristics. The selection effect made our results more applicable for people who were younger, White, born in the USA and had higher income. Finally, we used self-reported measures of FI, and participants were asked to recall their food situation for the previous 12 months. One potential problem could be inaccurate recollection, which may lead to misclassification of FI(Reference Coughlin45). In addition, DH was measured by a self-reported single question. It was more of a proxy measure and did not fully capture eating behaviours or actual energy intake. More objective measures should be applied in future studies.
Conclusion
In conclusion, the current study showed the moderating role of biological sex between FI and BMI, and FI and WC among US young adults. Females with FI were more likely to have higher BMI and larger WC compared with those without FI, while these same relationships were absent for males. The current study also showed that DH was a mediator between FI and BMI, and FI and WC among females. Females with FI had poorer DH and thus had higher BMI and larger WC. These findings should inform more accessible diet health education programmes and nutrition assistance programmes for vulnerable populations.
Acknowledgements
Acknowledgements: None. Financial support: There are no financial supports provided. Conflict of interest: There are no conflicts of interest. Authorship: Y.L. contributed to the research questions, data analysis and manuscript writing and editing. S.R. contributed to the manuscript revision and editing. All authors read and approved the final manuscript. Ethics of human subject participation: The survey was reviewed and approved by the National Center for Health Statistics Ethics Review Board.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980020004577









