Introduction
Community engagement is a priority for Clinical and Translational Science Award (CTSA) programs to increase the speed of translating research to practice and to ultimately improve community health and reduce health disparities [Reference Patten, Albertie and Chamie1,Reference Martinez, Russell, Rubin, Leslie and Brugge2]. Effective engagement requires a shared understanding of neighborhood health care quality and outcomes. Creating this shared understanding can be challenging without timely and accurate local health data, or ways to provide the data that are directly applicable to improving community health.
While health data are frequently only publicly available at the county level or higher, there is evidence such data may obscure significant heterogeneity that exists at more granular geographic areas, such as ZIP code [Reference Bi, He and Konty3]. Without this level of specificity [Reference Braveman, Dekker, Egerter, Sadegh-Nobari and Pollack4], it is difficult to identify patterns of inequity, merge data with local knowledge, and create the shared understanding necessary to begin building enduring partnerships grounded in trust. Trust in motivations and shared goals are essential and underlie “buy in” on both sides of the partnership [Reference Passmore, Fryer and Butler5]. Trusted partnerships lead to effective planning, implementation, and evaluation of interventions that promote community health and well-being.
The University of Wisconsin Institute for Clinical and Translational Research (UW ICTR) has an opportunity to overcome the challenge of providing local health data through data collected by the Wisconsin Collaborative for Healthcare Quality (WCHQ). WCHQ is a voluntary collaborative of over 20 health systems in Wisconsin that submit primary care data from their patient electronic health records every 6 months. The data include 25+ outcome and care measures that span the primary care continuum (see Supplementary Fig. 1). WCHQ data covers 65% of the primary care providers in the state and 3.5 million patients.
UW ICTR partnered with WCHQ and formed the Neighborhood Health Partnerships Program (NHP) to develop health reports at the ZIP code level for researchers and other partners working to improve community health and health equity.
With an eye toward supporting a shared understanding of community health outcomes and care, the NHP team engaged both researchers and a broad range of individuals involved in community health improvement organizations that are critical to ensuring that research efforts are both relevant and impactful in communities [Reference Selker and Wilkins6]. This includes the health care delivery system, public health agencies, and non-governmental community organizations.
The NHP team took a human-centered design approach to engagement, using co-design methods to ensure the way data are presented and shared will maximize the stakeholders’ ability to access it, understand it in context, and translate it to action. Co-design methods have been shown to effectively engage stakeholders to build products and research that have strong and enduring impacts on health [Reference Greenhalgh, Jackson, Shaw and Janamian7–Reference Vechakul, Shrimali and Sandhu9].
While human-centered design principles are being applied to various geographies, settings, and health issues, a recent scoping review revealed that there is limited information in the literature to describe human-centered methods like co-design or their impacts in public health research. Very few initiatives have clearly described or documented methods or results [Reference Bazzano, Martin, Hicks, Faughnan and Murphy10]. This article describes the co-design methods that were used to design NHP reports and data-to-action tools. The article also provides some early indicators on the adoption of the resulting reports and data-to-action tools, and the degree to which they are meeting diverse stakeholder needs. The methodology described has the potential to support CTSAs in increasing the community adoption and usability of CTSA program products and tools, and increasing community engagement in research activities.
Methods
The NHP journey, depicted in Fig. 1, began in 2018 with a vision of using geo-coded WCHQ data to support community-based public health efforts. This section summarizes the steps that led to co-design activities, including 1) assessing interest and needs, 2) prototyping the reports, data-to-action tools, and dissemination processes, and then 3) outlines our co-design activities in detail.
-
1. Assess Interest and Needs
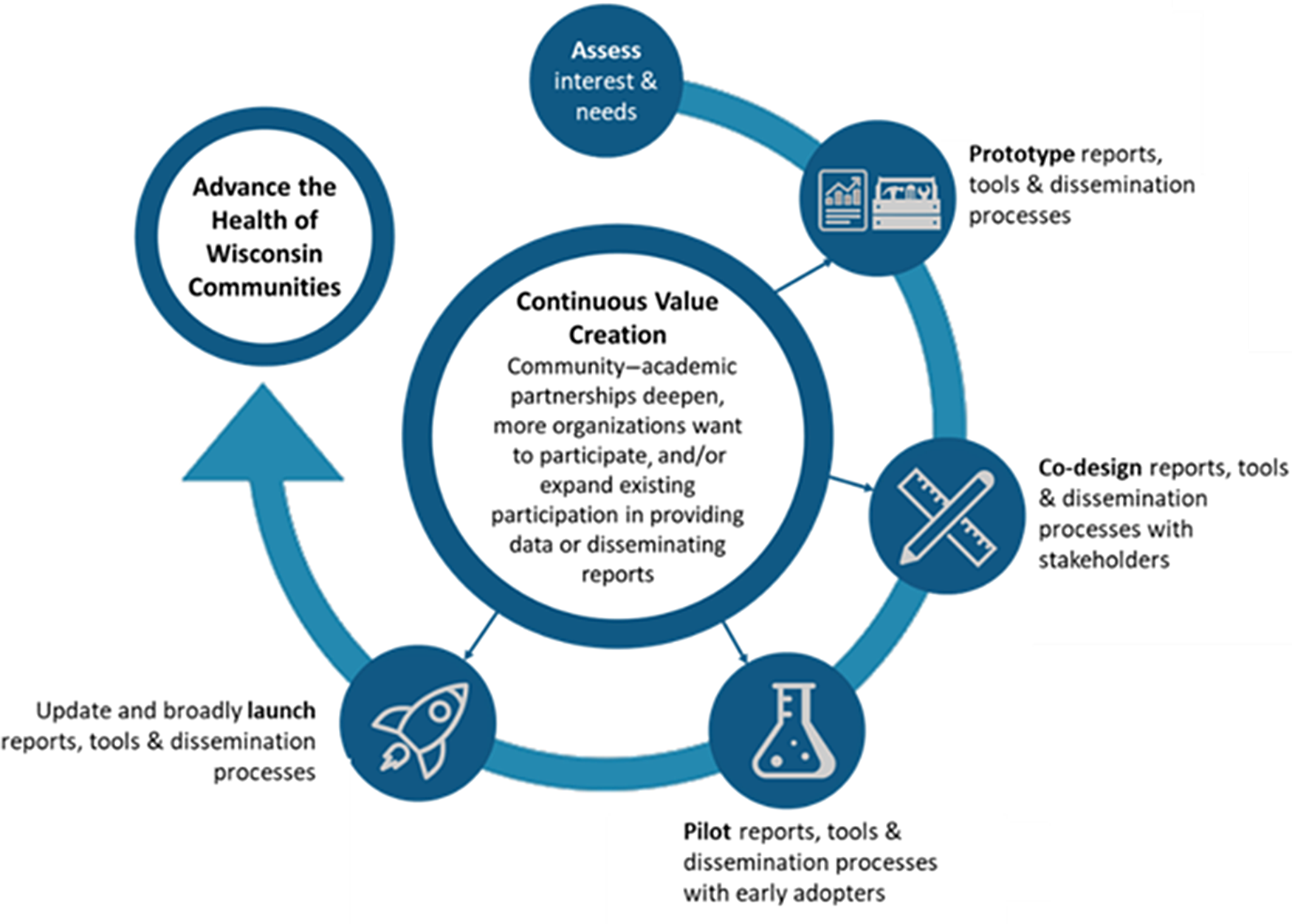
Fig. 1. Neighborhood Health Partnerships Program Plan to Advance the Health of Wisconsin Communities.
The NHP team sought early input from diverse audiences to assess interest in geo-coded local data sources and solicit feedback on needs that could be addressed by it. In 2018, an early concept was presented to 200+ individuals from 60+ organizations across Wisconsin, including health systems, community clinics, hospitals, local businesses, community organizations, payers, pharmacies, and the Wisconsin Department of Health Services. These audiences expressed enthusiasm for the concept and provided feedback that the reports, in addition to highlighting the extent of disease control, should focus on the prevalence of disease, track outcomes longitudinally over time, identify disparities, and translate findings to how they affect health.
Additionally, the team conducted a survey of researchers working with community organizations, representatives of community coalitions, and local public health departments in Wisconsin (n = 371). This survey was designed to gauge interest in data at the ZIP code level and a potential list of health outcome and care measures. Among the 76 respondents, 96% expressed interest, with the most interest reported for measures of risk factors (e.g., tobacco use, obesity, and high blood pressure), chronic conditions (e.g., heart disease, diabetes, and stroke), and mental health (e.g., depression). When asked what best described their need for this resource, 79% selected the statement: “I need it because nothing else can provide me with up-to-date data on the health of local communities.” Respondents indicated a direct focus in 53 of Wisconsin’s 72 counties – 34 in rural counties, 24 in urban counties, and 11 statewide.
The early input that was received, along with lessons learned from other work, led the team to a set of program goals and an approach to achieving them. The primary goals are to:
-
Provide local, timely, and actionable health data and data-to-action tools to support and inform strategies that advance health and health equity in Wisconsin communities.
-
Continuously expand the value and reach of the program by motivating improved data through enhanced participation from health systems and widespread adoption of reports and data-to-action tools.
-
2. Prototype for co-design
With interest confirmed and goals set, the NHP team prototyped an infrastructure to deliver timely and actionable data. Prototyping has been shown to be a critical first step in piloting and ultimately scaling successful projects with communities. [Reference Brown and Wyatt11] Prototypes developed included reports, data-to-action action tools, and the dissemination infrastructure (a “Navigator” program). The team created prototypes in advance of co-design sessions with the intention of simulating the products and processes of the program that could then be tested, iterated, and refined with potential end users. This approach ensured that the prototype was technically feasible given the constraints of available data and reporting tools and condensed the time asked of participants. Potential end users face incredible demands, particularly during COVID-19, so securing enough time to fully co-design a first prototype would have been unreasonable.
Report Prototypes
The team worked with the UW Health Innovation Program (HIP) to build a data and reporting infrastructure with WCHQ data as the primary data source. The infrastructure was supplemented with 2014–2018 American Community Survey (ACS) and 2011–2017 Wisconsin Behavioral Risk Factor Survey (BRFS) data.
The first NHP report prototypes were built in Qlik, a tool that would allow the team to quickly produce reports for any ZIP code (with sufficient data) on any of the 25+ publicly reported measures from WCHQ.
Action Tool Prototypes
In addition to the reports, the team prototyped a set of data-to-action tools that would support report users in understanding the data and using it to prioritize needs, build partnerships, plan, implement, and evaluate. The team started by scanning the growing landscape of currently available data-to-action tools and resources and by interviewing individuals and organizations that commonly support the use of data for action. This scan and later interviews enabled the identification of best practices and pitfalls to avoid, leading to prototypes of three action tools: 1) Making Sense of the Data and Moving from Data to Action, 2) Aligning Community Priorities and Data, and 3) Ideas for Taking Action (see Supplementary Table 1).
Dissemination Infrastructure Prototype
The reports and data-to-action action tools can only be useful if they are disseminated to the individuals, organizations, and communities that can benefit from them with the appropriate context and support. The dissemination infrastructure prototype was centered on the role of “Navigator” and driven by three goals to ensure:
-
1) Data are delivered with full context of the social determinants that can impact health by place;
-
2) Report users are fully supported in their efforts to interpret and use the data;
-
3) Infrastructure can reach a wide range of users, including those looking to establish academic or community partnerships.
The team recruited a set of “early adopter” Navigators who are well versed in the many factors that contribute to health in a neighborhood and will ensure that data are delivered with the appropriate context. Early adopter Navigators have established partnerships with individuals and organizations that are likely to use and benefit from the use of NHP reports and data-to-action tools. These Navigators also have experience establishing and maintaining community–academic partnerships and connecting their partners with evidence-based strategies for action.
The early adopter Navigators (see Supplementary Fig. 2) were identified through UW ICTR’s community engagement core, the Community Academic Partnerships core (ICTR-CAP). ICTR-CAP is a federation of 40+ programs at UW-Madison and Marshfield Clinic that centralize and organize access to research and training resources for investigators and communities [Reference Quanbeck, Mahoney, Kies, Judge and Smith12].
-
3. Conduct Co-Design
To ensure that NHP reports, data-to-action tools, and processes would be useful to a diverse set of end users, the team developed a co-design strategy based on the principles of human-centered design. Human-centered design is defined as “understanding people in context and from their own perspectives, testing various solutions on a small scale, and continuously iterating through this process” [Reference Sandhu13]. Co-design seeks to “understand the problem through the eyes of the user. It does not require big numbers, unlike a statistically significant survey, but it does require spending quality time with a small number of participants, mapping their journeys, identifying obstacles and developing mitigating strategies” [Reference Evans and Terrey14].
A multidisciplinary team was assembled to develop the co-design strategy, combining expertise in co-design methods, community engagement, and the data sources and reporting tools.
Co-design goals were to:
-
1) Improve the accessibility, usability, and overall experience that stakeholders have with NHP program assets;
-
2) Build enthusiasm for NHP program and assets;
-
3) Recognize and address power imbalances between academic researchers and community members and build mutual trust.
The NHP team worked with early adopter Navigators and funding organizations to recruit participants from a broad range of organizations, including academic, community, government, health systems, and clinics. The team conducted 11 sessions with 53 individuals, from 30 organizations. The sessions were conducted in three waves, each 2–3 months apart. This allowed the team to incorporate the feedback received and then test again with a new audience. Figure 2 summarizes the sessions and participants.

Fig. 2. Neighborhood Health Partnerships Program co-design sessions and attendees.
The sessions were originally envisioned as half-day, in-person sessions, but were reimagined as shorter, 90-minute virtual sessions due to the COVID-19 pandemic.
A journey mapping activity was at the center of the sessions, facilitated using a predefined set of personas – a diabetes researcher, a program manager for a community organization, a director of community health at a health system, and a Navigator. While there are many approaches to co-design, the team decided that journey mapping was the best opportunity to get a holistic view of what a user may experience during their interaction with NHP. In the short 90 minutes, journey mapping illuminated moments of potential confusion, frustration, and delight [Reference Gibbons15].
Personas used in journey mapping were developed through empathy mapping activities with the project team and knowledge gained through stakeholder interviews (see example in Supplementary Fig. 3). Personas were intended to focus discussions through a shared understanding of persona needs, anticipated behaviors, and goals. They also invited co-design participants to step out of their own perspective, often making them more willing to provide critical feedback [Reference Neate, Bourazeri, Roper, Stumpf and Wilson16].
During journey mapping, participants were asked to assume the role of the persona and reflect on their experiences as they interacted and used the various reports and data-to-action tools during the three phases – making a request for a report, reviewing a report, and acting on the report. During each step, participants were asked to share what the persona liked about the prototype, what they wished was different, and what they had questions about. Figure 3 is an example of the outputs of one of the sessions. In most cases, various solutions/ideas were captured during the journey mapping discussion, but at the conclusion of the activity, a few minutes of additional solution brainstorming were provided.

Fig. 3. Neighborhood Health Partnerships Virtual Whiteboard output example.
Each of the participants brought their perspectives, capabilities, and connections, making the discussion and focus of each one of the sessions entirely unique. Facilitators were asked to be flexible in their approach and given permission to pivot from the prescribed process/agenda based on the needs and interests of the group. This maximized engagement, fresh thinking, and ultimately, novel ideas.
Results
Although each session took on its own unique personality, major themes did emerge when the discussions were analyzed as qualitative data. The team downloaded all of the feedback collected on the virtual whiteboard tool from each session into Excel. The feedback was then categorized by broad area (e.g., general, reports, action tools, etc.), and then specific element (e.g., trend line, building partnerships, etc.). The feedback in each resulting category was then reviewed and potential solutions were proposed if they did not already occur organically during the sessions. These potential solutions were then bucketed into major “themes” to be further refined.
Themes included 1) focus on framing the data to build trust, so that users are more confident that sources are reflective of their community, 2) supplement the main data source with additional demographic and social determinants data to provide more context on community health, 3) provide benchmarks in a way that provides context on what is possible rather than ranking communities against one another, 4) further define the role of the Navigator and clarify parameters around how reports can be used and shared, and 5) make data-to-action tools more visual and simplify language. A full list of recommended improvements is available in Supplementary Table 2.
Improvements were then mapped based on their expected impact/effort required (see Supplementary Fig. 4). As a result:
-
low-impact/high-effort solutions were eliminated;
-
high-impact/low-effort solutions were built into plans to complete prior to pilot;
-
low-impact/low-effort or high-impact/high-effort solutions were discussed further and, in most cases, were tabled until after pilot launch
Once all co-design sessions were complete, a communication went out to all participants to recap what was learned, what changes would be made, and when the pilot would begin.
Overall, co-design goals were met. The process enabled input from a broad stakeholder group to evolve reports, data-to-action tools, and dissemination infrastructures to better meet diverse needs, while also building enthusiasm and trust with participants. Session evaluation results show that participants were confident that with the suggested changes, the final co-designed NHP reports and data-to-action tools would be immediately useful in promoting community–academic partnerships and in planning, implementing, and evaluating research and other initiatives in communities.
In the co-design evaluation survey of early adopter Navigator participants, 96% (n = 16) of participants felt “moderately” to “very” confident that they would be able to use these reports and data-to-action tools and/or help one of their partners use them. Following co-design sessions with members of community-based organizations, 87% (n = 16) said they were “moderately” to “extremely” likely to request a report for at least one measure. These early indicators were later reinforced during training as 93% (n = 14) of the trained Navigators reported that they see value in the reports and data-to-action tools.
Changes were incorporated into reports and data-to-action tools, and a web-based infrastructure was built to house them at https://nhp.wisc.edu/. Figure 4 offers a view of the evolution of the prototype from first co-design series to the version that is now being piloted.
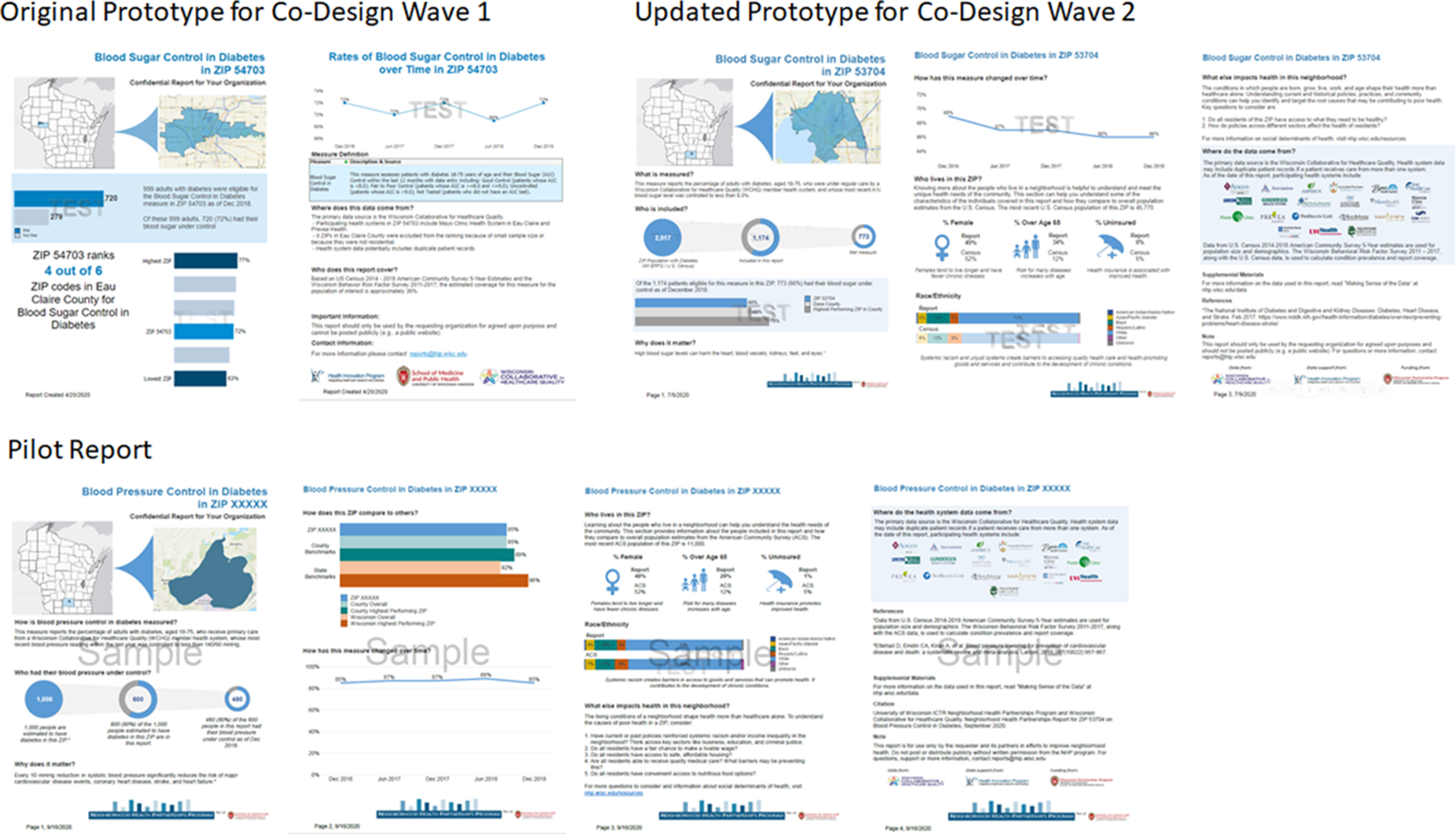
Fig. 4. Neighborhood Health Partnerships report evolution.
In addition to adjustments to the reports, one of the most powerful learnings from the co-design process was that Navigators needed a tool to more easily identify ZIP codes and/or measures to request reports for. Based on this, the team developed a set of web-based interactive heat maps using Tableau that would allow Navigators to see available ZIPs and to measure performance at a glance (see example in Supplementary Fig. 5).
The NHP pilot launched in October 2020 and will run for 6 months. Based on the evaluation of results, the program will be modified before a broader implementation in summer of 2021. In the pilot period, the program will be evaluated on the value NHP Navigators find from using the reports/tools, the extent they are able to use them in their existing work, and whether or not they can be effectively used to build partnerships and/or uncover opportunities to improve health and health equity. The team is hopeful that including the Navigators and their partners in the co-design process and addressing many of the themes that emerged will greatly improve the chances of success on these metrics.
Discussion and Conclusions
While earliest applications of human-centered design approaches were in the fields of medical engineering, health information management, and web design, research-focused applications are growing and showing some positive results [Reference Searl, Borgi and Chemali17,Reference Lwembe, Green, Chigwende, Ojwang and Dennis18]. Co-design methods have been particularly powerful in finding critical pain points early, leading to better products and experiences, while also building trust with community members and other stakeholders [Reference Evans and Terrey14].
While promising, successfully executing co-design can be challenging. Co-design strategies must acknowledge and mitigate barriers to success including facilitators without proper skills, reluctance to engage, limited capacity of organizations to participate, power issues, and the management of expectations [Reference Hatzidimitriadou, Mantovani and Keating19]. There are also unique considerations and limitations to conducting co-design virtually.
This article shares one path to effectively executing co-design to build assets and a dissemination model for a CTSA-sponsored program aimed at enabling community engagement and health improvement through local health data and data-to-action tools. Based on this experience, the team offers these best practices to:
-
1. Engage with potential program stakeholders as early as possible to confirm interest and better understand the needs that your program will aim to meet.
-
2. Build prototypes based on what you learn from early engagement and needs assessments to give co-design participants something tangible to respond to.
-
3. Use your CTSA community engagement core to recruit co-design participants from existing partnerships with researchers and community organizations.
-
4. Engage a multidisciplinary team to build the co-design strategy. As a collective, the co-design team should bring experience in co-design, community engagement, and technical knowledge related to the product being designed.
-
5. Build a co-design strategy that creates an environment of power balance and trust where all participants can meaningfully participate.
-
a. Limit the use of formal titles
-
b. Allow participants to contribute in multiple ways (e.g., verbally, written, partners, groups)
-
c. Use small groups of 4–6 to create less intimidating and more engaging sessions
-
d. Use personas to guide activities and discussions.
-
-
6. Offer financial incentives to participate and acknowledge the contributions from organizations that have limited capacity.
-
7. For virtual sessions, employ the use of a virtual whiteboard tool (e.g., MURAL) to rapidly capture and build on ideas, simulating an in-person environment with visual aids.
-
8. During sessions, be flexible based on the interests of the group. Facilitators should be willing and able to adapt their planned process/agenda to whatever will result in the most participation, engagement, and new thinking.
-
9. Once co-design sessions are complete, share plans with participants so that they know they were heard and to maintain enthusiasm for the new tool/product.
Our approach and recommended best practices could be used to encourage the use of human-centered design principles to co-design CTSA products and tools that meet the diverse needs of stakeholders and the communities they serve. The team looks forward to continuing to assess the outcomes of the NHP program and co-design efforts in hopes of better understanding the potential and impact of co-design approaches in public health research.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/cts.2021.11.
Acknowledgments
The authors would like to acknowledge other members of the NHP team that worked on this project including Katie Ronk, Taylor Konkle, and Kristina Stephenson.
We also acknowledge the stakeholders who have shared their time, views, and experiences in the NHP co-design efforts described. A full list of participants is available on the NHP website at https://nhp.wisc.edu/program-collaborators/.
Work reported in this article was funded through a Wisconsin Partnership Program grant (Principal Investigator: Maureen A. Smith). The project was supported by contributions from the UW Collaborative Center for Health Equity, the UW Population Health Institute, and the UW Health Innovation Program.
The UW Health Innovation Program contributions were supported through the UW School of Medicine and Public Health Wisconsin Partnership Program, and the Community-Academic Partnerships core of the University of Wisconsin Institute for Clinical and Translational Research (UW ICTR) through the National Center for Advancing Translational Sciences (NCATS), grant UL1TR002373. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Disclosures
The authors have no conflicts of interest to disclose.






