Background
“If you look at the times somebody’s beliefs have been changed, it’s often because of a story that hits them in the heart." – Melanie Green, The Story Collider
At its core, STEM research is based on the values of objectivity and a quest for the truth. But how can objectivity and truth hold up in a world clouded by feelings, misunderstanding, skepticism, misinformation, rumor, and forms of “fake news?” At the same time, scientists are increasingly feeling vulnerable, attacked, and disconnected from lay communities even as they are tasked with defending and explaining complicated information. It is now more important than ever for scientists to find ways to connect and engage a public audience. This article is invested in how the concept and structure of story connect hearts and minds and can be an effective and mediating method in how scientists deploy information to the public.
Story is “always already” a part of scientific research. It may be that the bigger question now is how to highlight those stories when it feels like there is a war against science and so much is at stake. Does it benefit science to show its humanity – and therefore its human flaws – by using story to communicate research to the public? If so, how can the story structure be harnessed to address facts and discoveries with clarity, nuance, and truth? (There is some debate about the semantic difference between the concepts of “narrative” and “story.” However, since there is no consensus on the best term, in this article, we use the two synonymously to mirror current multifaceted conversations in the field [Reference Halverson1–Reference Steiner4]).
Epistemologies of science – or “how we know what we know” – is actively engaged by historians and philosophers of medicine and science, medical humanists, and practitioners of Narrative Medicine, and is intuitive to many scientists. Researchers in Clinical and Translational Science are especially nimble with how they come to understand certain information as fact, as it is their task to move discovery from bench to bedside, then from bedside to practice. It is research about the most fundamental mechanisms of what makes us human, from our biology to our behavior. The fact is, scientific information rests on the tension between the hypothesis that a team of researchers may seek to confirm, their methods of enacting their study, the raw reality of the facts themselves, and the statistical efforts made to find clarity in the numbers. For example, the biology of neuroscience does not change whether or not we believe it to be true, but the how and why of translational science is subject to human intervention that impacts the questions we ask and the results we see. This intervention happens in terms of how the science gets translated to other researchers and to the public, as well as how it engages with the discoveries made by other researchers. In other words, it is dynamic and subject to real-time knowledge, experience, and unconscious bias. This is also compounded by the fact that science, by nature, builds upon science – or, put more plainly, research that confirms or advances the same story.
Although the idea of story may be perceived as an unstable force in scientific truth, embracing the narrative aspects of science can fortify its importance by giving it a way to become legible to audiences of all levels of expertise. Furthermore, it is an effective tool to use in educating the next generation of CTS investigators to be more effective educators and communicators of translational science by clarifying a path for connecting with audiences. Connecting story to new concepts has also helped medical and graduate students contextualize information and expedite their understanding. Personal stories about why scientists do what they do can be compelling and invoke passion and connection. Adding narrative to research, which might appear as an abstraction to those outside of the discipline, can have significant impact not only in public understanding, but to the sense of purpose and connections felt by the scientists themselves. Our team has trained thousands of researchers around the world in the use of stories in communicating science to all audiences [Reference Kaplan-Liss, Lantz-Gefroh and Bass5]. Participants in workshops report being transformed, in part by this innovative process of learning as well as by a profound realization surrounding the personal connections to the stories they had lived and shared.
It may be clear to you by now, reader, that we stand by story. Keeping the human story as the driving force in our communication engages our students, shapes our research, and improves our ability to translate our work to the populations the work is intended to impact. In this study, we will introduce a novel pedagogy to help craft a story and a repeatable process that enables the researcher to relate to the people involved. Akin to understanding your research subjects, this process paves the way to recognize the “characters” in your own research story. We describe the architecture of a story, provide an innovative tool to compose a story for researchers who want to incorporate it into their own work, and suggest instructional resources for additional support.
Story in Science Communication
Many university-based science communication programs have emerged since the 1990s, all with the mission to tackle the advancement and support of science through the process of clear communication. Story became a vital part of this process. Why? Story sticks. Research shows that our brains can contextualize new information when it is placed in the context of story more effectively than in any other format [Reference Boris6]. We learn through all our senses and stories captivate us through the description of visual imagery, the voice of the storyteller, and the emotional connections that, in addition to engaging readers and listeners, may even provide a release of oxytocin when we are moved [Reference Zak7].
Beginning in 2009, the Alan Alda Center for Communicating Science at Stony Brook University became a leader in spearheading the paradigm shift in the dissemination of research to all audiences with workshops in communicating science for universities, medical facilities, and national labs around the country. Story was at the core of the Alda Method©, which was based on journalism and improvization. In the beginning, the first half of an opening conference plenary was devoted to convincing participants that communication even mattered. Later, grantors, like the National Science Foundation, helped propel the movement when they included communication to the public, or “broader impacts” into the grant process, and suddenly the opening of the Alda Center plenary in subsequent events was no longer needed. Researchers were beginning to understand its value.
The idea caught fire and science communication programs that included improvization and storytelling started springing up in universities, medical schools, businesses, and museums. Programs like The Story Collider and iBio used stories to help people connect with complicated concepts and initiatives. Graduate students grabbed the reins and championed programs around the world telling the stories of their research in 3-min thesis competitions and NASA’s Famelab. In 2015, the SciComm symposium launched, bringing together faculty, students, and researchers in a half-day session that, based on enthusiasm, expanded the next year, and the hashtag SciComm was born. Certificates and degrees in science communication became standard fare. And because of its relevance to clinical research, journals like JAMA, Lancet, and the American Medical Association have published on the important use of story in both research and reflective, creative-non-fiction capacities. Dr Rita Charon, founder and director of the influential program in Narrative Medicine at Columbia University, states in a recent Lancet perspective column that in fact, the narrative is what researchers and humanists have in common, “Instead of bifurcating arts from sciences, we can recognize that rigorous epistemological standards reside alongside disciplined esthetic methods in the day-to-day work of all investigators, all of whom use narrative actions to transmit the known and the seen to others [Reference Charon8].”
The standards regarding dissemination of research have shifted, allowing story and human connection into the rule book. Communication training for physicians and scientists is a growing field, and at the graduate level, offers students at an early stage of their careers the tools to explain the humanity behind their research, and how that humanity can bolster the importance of that research.
The Compassionate Practice®: Connecting with People
Our contribution to this paradigm shift, The Compassionate Practice®, is an interdisciplinary curriculum developed by the authors of this paper at the Texas Christian University (TCU) School of Medicine. The method provides a quick, repeatable process that can be used to understand and appreciate the people involved in the stories of science: researchers, research subjects, community members, funders, the media, patients, and the public. This process is based on the methods of a seminal theater scholar, Konstantin Stanislavski, which emphasizes exploration of character, given circumstances, and objectives to cultivate empathy for the characters in the play. In The Compassionate Practice®, we correlate the examination of a written theatrical character to the examination of real people to encourage deeper understanding that informs connection and behaviors one chooses to take. Let’s illustrate the process with a fictional story of Chelsea, a research coordinator, trying to enroll participants in a research study:
In the waiting room of a primary care clinic, Chelsea approaches a patient named Richard carrying a clipboard and several flyers about a new clinical trial. She sits down next to him and begins to tell him about an “awesome opportunity to improve hypertension treatment!” During the conversation Richard does not make eye contact, consistently looks toward the office door. Chelsea eventually takes notice of Richard’s discomfort and says, “Sir – it is really important that this clinical trial have people like you in it.” This statement triggers a negative emotional response, and Richard rejects her outright, “Are you serious? Did you really just say people like me? Get out of here and leave me alone.”
From a distance, it’s simple to see some of the assumptions made by Chelsea that led to this outcome. Perhaps we can even recall similar encounters in our own work and lives. Intent does not always lead to positive outcome and taking a moment to step back and consider the stories of others can provide us with curiosity and perspective-taking that builds relationship and connection.
Stories begin with characters like Richard and Chelsea. Character can be understood as the roles we occupy based on our context. As individuals, we play several roles throughout a given day. Chelsea may be a mother for an hour in the morning before becoming a coordinator when she steps into the clinic. While we are always both “characters,” one role will emerge more predominantly depending on our given circumstances at that moment. Given circumstances refer to what the play tells us about what is going on socially, economically, physically, and emotionally for the characters in this play. This can be translated to the real world as the process of examining our own social, economic, physical, and emotional context. The circumstances we are in inform our choices and ultimately the stories we tell ourselves and each other. Objectives are the goals driving us to action. When objectives are left unexplored, the missed opportunity to understand a person’s motivation leads to miscommunication and residual conflict. Let’s take a quick look at Table 1 to see how these concepts played out in the encounter between Richard and Chelsea.
Table 1. Gaining perspective through character, circumstances, and objectives

Chelsea’s Objective has driven her to appeal to Richard’s identity as a Black man underrepresented in clinical trials. However, because of Richard’s Given Circumstances, along with the history of racism in clinical research, this statement triggers a negative emotional response, and he rejects her outright, “Are you serious? Did you really just say people like me? Get out of here and leave me alone.”
These two-character stories have collided, and we have arrived at an impasse because of competing goals or objectives and the challenges of intent versus impact. While Chelsea’s intent is a good one, her lack of insight into the context of Richard’s perspective, and possible lack of recognition of what is informing her own actions have led to the wrong impact. If Chelsea had taken steps to learn more about Richard’s story, she would have been better equipped to connect. Imagine the difference if Chelsea had instead used questions like: “What are your feelings about clinical research?” or “What would you like to know or understand about this research study that might make you feel a little more comfortable?” While these questions might not have convinced Richard to join the trial, inquiry is a compassionate way of understanding another person’s story and would have provided Chelsea with important information on Richard’s given circumstances and objectives to share the story of this clinical trial.
Start with Them
All good communication begins with a clear consideration of the audience. Who are they? Why do they care? The impact of your story will only be met if you consider the people involved. It makes sense that in a conference forum or in a journal such as the Journal of Clinical and Translational Science, that a researcher may be able to speak in their own discipline-specialized language. But it behooves us to learn to be “multi-lingual,” so that we can explain our research to people with varying levels of expertise. Doing this involves an actively empathetic approach in order to understand how your work might be perceived and internalized by those who would benefit from it. A simple process to help you understand your audience, as introduced through the “Character” analysis in Table 1, provides a first step to successful storytelling.
After you have defined the people involved, it helps to think of the story structure. If you are preparing for a talk, presentation, or paper for the public and want to prepare, we have developed a tool called What’s the story? which can be found in supplementary material. We developed this form to teach the use of story to medical students and faculty as part of the The Center for Compassionate Communication curriculum at UC San Diego’s T. Denny Sanford Institute for Empathy and Compassion.
We offer a simplified version of the story form in Table 2 in order to continue to illustrate the process. Imagine Chelsea began with inquiry to learn more about Richard’s story, and then used elements of this structure to relay information about the clinical trial.
Table 2. Simplified story form
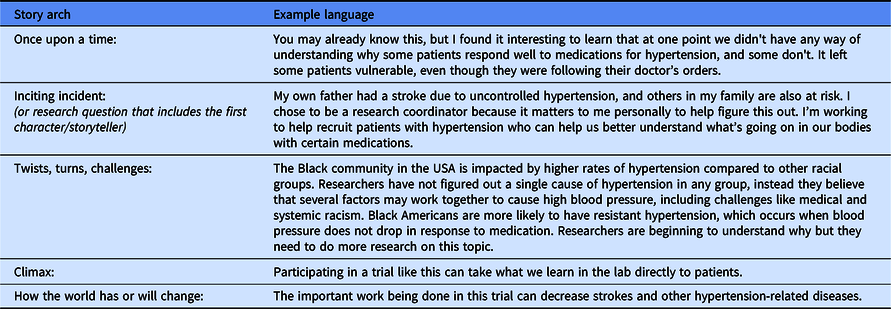
Beginning with common ground is always a good first step to build curiosity in the listener and connection between the audience and the storyteller. We can always find common ground, even when it does not seem obvious. In the sample above, Chelsea focuses the story on their common ground of hypertension to help connect with Richard. In the real world, the sample would likely be fluid and conversational, but this table can give the reader an idea of how this story might play out in written form or as the beginning of a group presentation.
The beginning of a story sets the stage for what was true before the advent of the research question, engages the emotions of the listener, and builds connection with the storyteller. It’s an important foundation, because the arc of storytelling takes you from what was true, through an inciting incident (your research question), into the characters involved who encounter twists, turns, and surprises that carry the audience into a climax of discovery – and out the other end when the world is different because of that journey. Scientist, playwright, and educator Holly Kerby, from Story Form Science, often asks her students to consider the beginning and the ending first, so they can recognize the scope of change.
One could argue that the methods section of a research article parallels the twists, turns, and surprises that lead the audience to the climax of discovery. One could also argue that in a scientific journal, this area of reporting is the most devoid of emotion as it is meant to indicate how the study could be replicated by others. And yet, it is for this very same reason that a way to clearly communicate and explain these steps is equally crucial; surely, it benefits all of us if others can replicate proof. This is where story and science have the potential to powerfully connect without contradicting each other: by showing how the steps that lead scientists toward a particular discovery are sound and applicable to the people for whom they are conducting this research.
The utility of story can be used in presentations, media interviews, and writing for the lay public in grant applications to disseminate complex science and research findings. Some resources that can provide you more in-depth instruction can be found through online learning modules called The Heart of Communicating Science presented by the American Heart Association and based on The Compassionate Practice® curriculum from TCU. One scientist from these modules, Keisa Mathis PhD, highlighted the vagus nerve as a character in her presentation to a community audience to help them imagine and understand her research on the neuroimmune mechanisms involved in autoimmune-induced hypertension and renal injury. Here is an excerpt of her preparation:
My job as a scientist is to learn and understand how things work. Members of my family suffer from hypertension, and as a person from this community, I’m eager to figure out what’s going on. There are a lot of medications for hypertension– but almost half of people on therapy donʼt have their blood pressure controlled. We need more answers.
Our lab wants to understand a protective mechanism in our bodies controlled by a nerve in our brain called the vagus nerve. We know that exercise, yoga and meditation increase this nerve’s activity in the brain and as a result our heart rate goes down. We feel good when we exercise because of that. But there is also recent evidence that when you increase this nerve’s activity, you can also reduce inflammation. Inflammation in the kidney is one cause of hypertension that wonʼt go away on its own. So, we are interested in finding the switch on this nerve, in order to decrease this inflammation in the kidney – and that would lead to a reduction in blood pressure.
Exercise and yoga can help you feel good – so until my research can catch up to your good habits, I encourage you to continue what you’re doing. If we can figure out new ways to reduce inflammation, this could be a better way of healing our community from diseases like hypertension and taking care of the people we love.
Discussion and Recommendations
We have presented the case for incorporating stories in CTS and provided tools for you to utilize in research and education. Although there remain barriers to widely disseminating the lessons of story, there is also opportunity.
Barriers
Despite the growing interest to utilize story in research, education, and faculty development, there remains a lack of resources and time to support the faculty in the arts and humanities who specialize in the pedagogy surrounding story. We have experienced firsthand the magic of pairing an actor with a physician or researcher to connect the lessons of story with real-world clinical examples that are relatable to the learner. Often, science and medical institutions are unable to support the salaries for arts and humanities faculty, even on a limited basis by way of visiting faculty positions, post-doctoral research for specific projects, and freelance work. In academia, humanists, social scientists, and artists are at somewhat of an impasse regarding their relationship with the sciences. Funding for humanistic programs, which tend to not bring financial gain to universities, has been under assault, and there are frequent – and understandable! – anxieties within humanistic and artistic disciplines about whether or not the only way for them to exist is under the good grace of the sciences. Though incrementally adapting, the promotion and tenure process remains a barrier to inspiring researchers to dedicate some of their time to mastering tools of communication, like the use of story, in their research and publications.
Opportunities to Address Unmet Needs
Despite these challenges, there is progress in efforts to incorporate the humanities in medical and research education. There is now more than a decade of innovative curriculum and experiential learning based on story that can be used to establish best practices. This will allow for scaling up by training trainers and disseminating the curriculum. The Association of American Medical Colleges’ recent white paper on The Fundamental Role of Arts and Humanities in Medical Education sets the stage for addressing many of these barriers calling for interdisciplinary competency and evidence-based teaching and learning of arts and humanities in medicine. They value the research process and promote the use of, “effective integrative pedagogical practices and recognize an expansive view of scholarship in academic promotion and tenure processes.” They are backing up their recommendations with grant support and faculty development opportunities. This provides a model for research disciplines.
A growing number of universities and affiliated centers that have the resources to support humanities programs in medical and research education are witnessing the growing interest and passion their students have for the humanities. From our experience at one of these institutions, lessons surrounding humanism in medicine are even starting to influence which programs prospective students may choose to apply.
What Does All This Mean for the Future?
Using story to translate typical research methods may seem daunting at first, especially within fields that tend to prioritize quantitative research. However, as those in the scientific community navigate the multifaceted uses of story, we may find that there are exciting opportunities to strategically utilize interdisciplinary methodologies. Engaging modes of inquiry that often fall outside of the hard sciences expands potentials for innovation and new forms of discovery. “Narrative Inquiry” [Reference Kim9], a form of interview that lifts from qualitative research as well as oral history methods, is a useful concept when designing research studies. Both sets of information-gathering modalities are typical in the humanities and social sciences and offer beautiful opportunities to strategically integrate representatives from disparate-seeming disciplines into a cohesive project.
With that said, there is also a reality that there are untapped opportunities for artists, humanists, and social scientists within medicine and bench sciences, especially if the scientific community is willing to engage the narrative-based, qualitative research methods that nonscientific researchers engage in their own fields. Qualitative research is, after all, largely steeped in the close reading practices inherent to studies in history, theater, literature, journalism, and many others. Consultations or collaborations with representatives from these disciplines are encouraged if institutions want to prioritize interdisciplinary research between the sciences and other disciplines.
Charon, physician and humanist, has developed research surrounding narrative methodologies, particularly in the evolution of clinical trials to evidence-based medicine [Reference Goyal, Charon and Lekas10,Reference Charon and Wyer11]. Such methodologies are actively steeped in deep, intellectually rigorous analyses of story – something that Charon has long practiced and advocated for in clinical practice [Reference Charon12]. These studies are an excellent example of how such research can map onto Clinical and Translational Research. It is also important to note that the Narrative Medicine program, which attracts students from a wide variety of professional backgrounds, has been instrumental in bringing focus and formalized skill to paying close attention to the story. Part of the program’s master’s degree is a required research methods course so that students are equipped to leverage narrative inquiry into their research repertoires once they leave the program, equipping them with practical tools in order to incorporate story. Neuroscientists have also recently defended story as an important way to “lighten the cognitive load of information” [Reference Willems, Nastase and Milivojevic13] and a way to translate findings to the public [Reference Martinez-Conde, Alexander and Blum14]. Additionally, Kotarba et al have delved into research on the identities of scientists through their qualitative research, which emphasizes story in two ways: using story for data, and also requesting that scientists reflect on the culture of their field by reflecting on themselves [Reference Kotarba, Wooten, Freeman and Brasier15].
Kortaba’s study also leads to a useful formation of community-engaged research. The community’s story ideally should be the driver of the research design, enrollment, and dissemination. But often, it does not become a priority, and participants’ and community’s stories do not inform the research protocols, process, and procedures; they only inform the results, not with their experiences, but only with their physiology. Moreover, they often do not hear the results of the research they have contributed to with their bodies. This continues to contribute to division and distrust between the researchers and community participants as illustrated in our example with Chelsea and Richard. By collecting and integrating the community members’ stories into research, there is a healing opportunity to bridge divides while also contributing to interesting, authentic research practices. In order to do this, one must acknowledge all of the players and ask who are the characters in this research narrative? If it is possible to do this for a community of scientists, then surely it is possible to engage these methods for a wide variety of other communities.
The use of story in the dissemination of research has made great strides in the past decade, and there is room for incorporating story in all aspects of clinical translational research including design and enrollment keeping the human subject central to the research process. If scientific and humanistic fields are willing to combine forces for the purpose of highlighting story from the inception of research projects, there is potential that will benefit both fields. By allowing story to be our North Star, we can imagine the new and innovative ways research can be shaped.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/cts.2022.6
Recommended Resources
Center for Compassionate Communication, T. Denny Sanford Institute for Empathy and Compassion, UC San Diego Health
TCU School of Medicine - The Compassionate Practice®
The Heart of Communicating Science, American Heart Association
Story Form Science
Alan Alda Center for Communicating Science
Story Collider
Popular Science’s Favorite Stories of 2020
NIH Clinical Research Stories and You: Personal Stories
AAMC StoryCorp Archive
The Division of Narrative Medicine at Columbia University.
Boston University Center of Excellence in Women’s Health: Community Engagement Training & Resources
Disclosures
The authors do not report any conflicts of interest.
Funding
There are no funders to report for this submission.




