Introduction
As of early February 2021, about 106 million cases of coronavirus disease (COVID-19) have occurred worldwide, with approximately 27 million cases reported in the United States. 1,2 While this disease was first encountered in Wuhan, China, it has rapidly spread throughout the world, causing a global pandemic. As the number of cases exponentially increases, so does the need for preparedness. Hospital systems have recognized the need to increase inpatient and critical care bed capacity. In order to meet this demand, many states have developed alternative care hospitals (ACHs), more commonly referred to as field hospitals.
Health care systems in the state of Rhode Island were asked to partner with the state and other agencies in creating 3 ACH, with the largest having a 600-bed capacity. This ACH is located in the exhibit hall of a convention center. Over a few short weeks, a building that once housed sporting events and concerts was transformed into a hospital. The design of the ACH includes 6 wards consisting of 3 to 6, 24-bed pods each, a 12-bed transition pod for decompensating patients requiring a higher level of care at the hospital system’s academic facility, and a resuscitation room for patients requiring intubation or more aggressive resuscitation measures.
Many factors are considered when building an ACH; however, patient care, provider, and staff safety remain the highest priorities. In order to perform systems testing, an in situ simulation session was developed. The primary goal of this session was to identify areas in need of improvement and suggest changes prior to the facility opening its doors to patients. This might include equipment, flow, protocols, communication pathways, and training priorities. Simulation is a well-established tool to accomplish these objectives. Reference Issenberg, Mcgaghie and Petrusa3 Previously, simulation has successfully been used for process and safety evaluation Reference Wexler and Flamm4 ; however, the development of an ACH for COVID-19 poses unique challenges. The most notable challenge in responding to a pandemic is the limited preparation time available in anticipation of rapidly opening for patient care. Other challenges include working with multidisciplinary providers in an unfamiliar work environment, the necessity of infection prevention practices, limited resources, and the development of ACH-specific protocols. The methodology described provides site administrators and medical directors the opportunity to uncover potential shortcomings and prevent patient safety issues prior to their occurrence.
Methods
Four scenarios were developed by an emergency medicine faculty member with experience in simulation and medical education using input from nursing and physician leadership. Scenarios were designed to represent both common clinical situations, as well as low frequency, high acuity events that may arise in the ACH. The scenarios included acute hypoxic respiratory failure, cardiac arrest, fall in bathroom, and staff member syncope. Emergency medicine trained physicians, critical care and medical-surgical trained registered nurses (RNs), and an ambulatory medical assistant (functioning as an inpatient certified nursing assistant [CNA]) were used as the clinical care team in these scenarios. The learning objectives for each scenario can be found in Table 1.
Table 1. Learning objectives
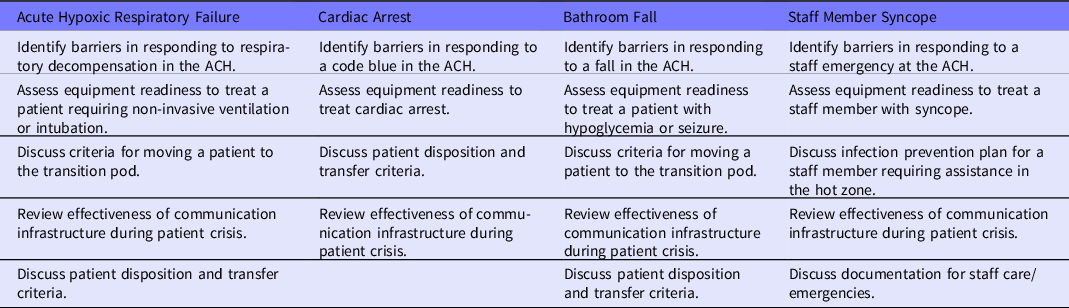
Note: ACH = alternative care hospital.
Prior to the simulation, participants were assigned the following roles: pod physician, pod nurse, pod CNA, transition pod/resuscitation room physician, and transition pod nurse. These roles were chosen to be consistent with staffing patterns at the ACH. A multidisciplinary group of 15 observers, including physicians, nurses, infection prevention specialists, and pharmacists, acted as observers and were provided debriefing forms (see Appendix A) to complete during and after the simulation. Participants did not have access to the scenarios or debriefing forms prior to the start of the session.
The debriefing forms were developed to compile suggestions and comments in regard to communication, team roles/responsibilities, and logistical concerns, including personal protective equipment (PPE), equipment, protocol modification, and overall readiness. A large group of stakeholders were also present, including various administrators (ACH medical director, health system chief nursing executive, and ACH logistics coordinator), members of the supply chain, emergency medical services (EMS), and the National Guard. The large group was included in the debriefing and discussion; however, they did not complete observer forms.
The participants and observers were oriented to the facility and available equipment prior to the simulation. A high technology simulator was used for the cardiac arrest, hypoxic respiratory failure, and bathroom fall cases, while the staff member syncope case used a standardized patient. A simulation operations specialist was on-site to assist with operations.
Each scenario concluded with a debriefing session summarizing the case, discussing challenges, and identifying areas for potential improvement. Debriefing forms were completed by the observer group and collected at the end of the session. The larger group was also present for the debriefing. Their comments and suggestions were recorded by a designated member of the simulation team. The comments and suggestions were compiled and organized according to area of focus: logistics, communication, team roles, and responsibilities. The information was then distributed to various areas of leadership for further evaluation and utilization.
Results
The simulation event, including debriefing, concluded after 2.5 hours; 15 participants were present in the observation group and were responsible for real-time evaluations, as well as debriefing at the end of the simulation. These scenarios were instrumental in determining the final facility protocols and identified unforeseen issues that had not been readily identified during meetings or tabletop exercises. The compiled comments and suggestions from the debriefing forms are shown in Table 2.
Table 2. Debriefing comments
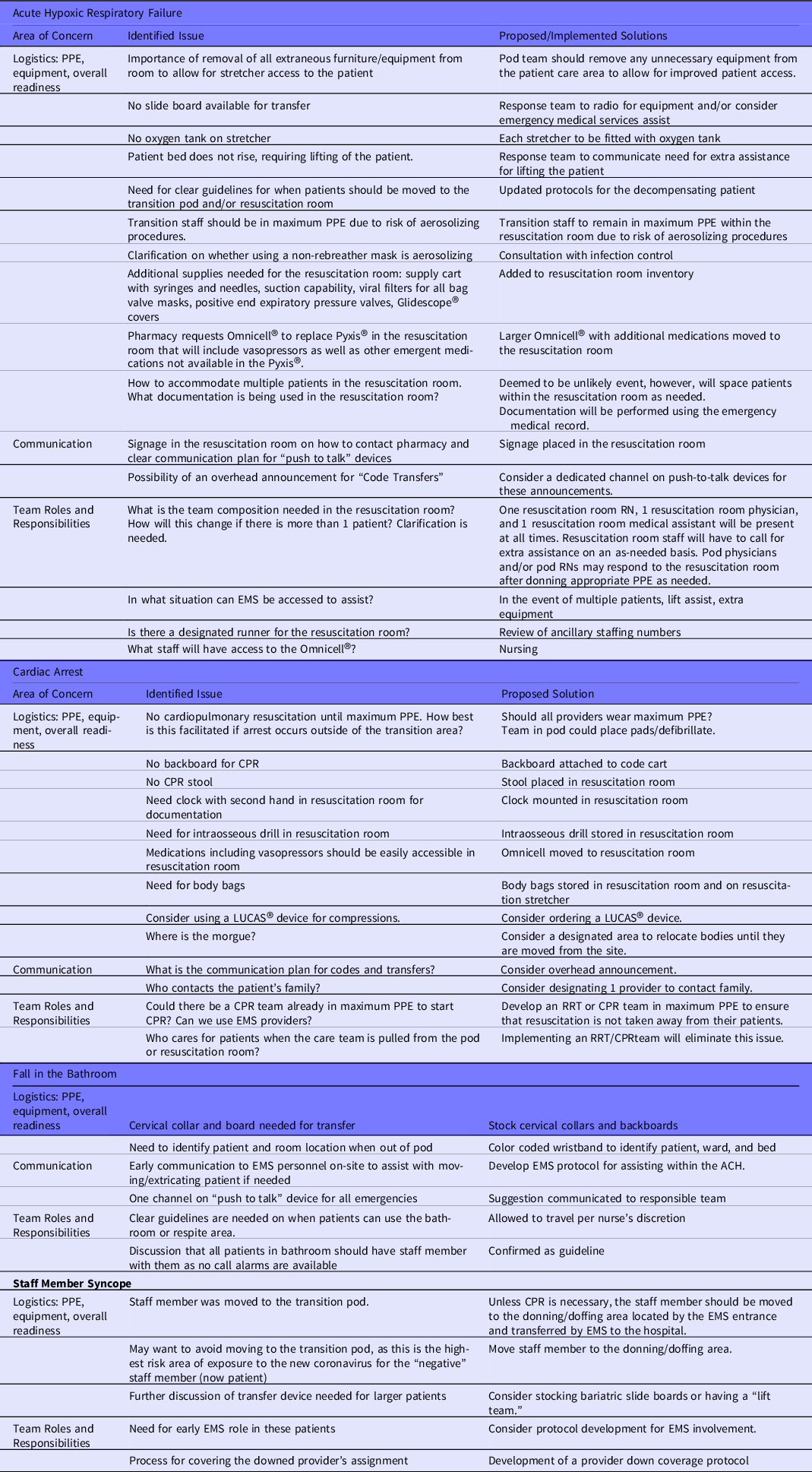
Notes: ACH = alternative care hospital; CPR = cardiopulmonary resuscitation;
EMS = emergency medical services; PPE = personal protective equipment; RRT = rapid response team.
GlideScope®, Verathon®, Bothell, WA, USA
Pyxis®, Becton and Dickinson Company, Franklin Lakes, NJ, USA
Omnicell®, Omnicell, Mountview, CA, USA
LUCAS®, Stryker Medical, Lund Sweden, USA
As a result, some changes were implemented almost immediately, including the addition of an Omnicell® with additional capacity into the resuscitation room, allowing a pharmacy to stock a wider scope of emergency medications. Nursing supervisors were granted access to the Omnicell to assist in resuscitations. A doffing station was added at the ambulance egress to the facility to assist in the care of uninfected staff who may need transport to the hospital. A list of necessary resources and equipment was generated for which the administration immediately began to address. Revisions to current protocols began, including cardiopulmonary resuscitation (CPR) management, criteria for transfer to the transition pod, and the development of a CPR/rapid response team (RRT).
Discussion
The purpose of this simulation was to focus on protocol development and systems testing for an ACH. While well-developed and tested protocols are frequently created and modified within a hospital system, they are not directly applicable to the ACH setting due to its dynamic and atypical environment. A multi-disciplinary in situ simulation offers a collaborative and constructive mechanism to gain insight into potential conflicts and safety issues, and to identify and implement changes prior to the opening of the ACH.
Several elements of the in situ simulation process were identified as being critical to the success of this program. In addition to having an experienced and interprofessional team, success was attributed to establishing psychological safety, a team with clear roles, and a debriefing plan.
Psychological Safety
Participants and their roles were established prior to the start of the session during the pre-briefing. Importantly, we specified that the purpose of the session was not to evaluate the clinical capabilities of the providers and staff, but to investigate and assess systems and processes. Removing the aspect of clinical evaluation alleviated some of the pressure from the individuals participating in the simulation and established psychological safety. It should also be noted that this was again acknowledged during the debriefings. In order to make the scenarios as realistic as possible, the participants were assigned their currently employed role; for example, a physician was assigned as the pod physician. The observer group was interdisciplinary and composed of physicians, nurses, pharmacy, and infection prevention personnel, each offering their unique perspective.
Team With Clear Roles
Completing a simulation assessment is best accomplished with a dedicated and experienced simulation team. Our simulation team included 3 experienced simulation faculty. One faculty member served as the voice of the patient and provided case information, 1 led the debriefing, and 1 was dedicated to observation and note-taking. Three simulation operation specialists were present to operate the high technology simulator, reset the physical space, and perform audiovisual documentation. As this is a collaborative team effort, the roles may vary, based on the scope of the project, resources, and personnel available.
Debriefing Process
A well-facilitated debriefing is instrumental in encouraging discussion, knowledge sharing, and identifying areas in need of improvement. For this session, with many participants and observers, it was particularly important to briefly and factually recount the series of events in the simulation. One participant was asked to briefly summarize the case at the beginning of the debriefing. If any phone calls were initiated, the participants were asked to summarize the nature of the communication. These 2 steps allowed for all observers and participants to establish a shared mental model of the simulation case. Next, the simulation participants were given the opportunity to comment on things that went well or posed specific challenges. Finally, the discussion was opened to all present to share observations and suggest solutions to problems identified. It should be noted that there is no single correct way to facilitate a debriefing, as many debriefing frameworks work well for interdisciplinary simulations. Reference Eppich and Cheng5
One of the common themes in each of the scenarios involved transporting a patient to a higher level of care within the facility. Many of these are reported in the debriefing comments for the hypoxic respiratory failure scenario. This was the first simulation case and required an extended debriefing. This is helpful to recognize in regard to time management of the session. Facilitators should recognize that the later scenarios will debrief more rapidly, as it is unnecessary to reiterate points previously discussed in a prior debriefing.
Limitations
It should be recognized that without the cooperation and recognized value from the administration and leadership, this project would not be possible. Full support was provided by the health system chief nursing executive, ACH medical director, ACHF nursing director, and the ACH logistics team.
Every ACH fills a specific niche, experiences unique challenges, and has different resources. While there are certainly common themes identified in this study among various ACH, many of our findings are likely unique to our facility. Therefore, the recommendations in the results section are not prescriptive, but rather demonstrate the granularity of outcomes from this process.
The physicians participating in the simulation were all emergency medicine trained. Emergency medicine physicians are a valuable resource when discussing needs of an ACH and will mostly be staffing the transition pod rather than the wards. Wards will likely be staffed by physicians from other specialties with less experience in critical care, or underutilized providers due to the pandemic. In this ACH design, this includes physicians who typically work in an outpatient or surgical setting and are not usually involved with inpatient medicine. If other specialties were included in the future simulation assessments, additional recommendations might be uncovered. The unique background and difference in training and daily practice of these physicians offer a different perspective. Another challenge was dealing with COVID-19-related restrictions on gathering size and social distancing requirements, limiting the number of people able to participate in the simulation.
Conclusion
The unpredictable nature of this pandemic has increased demands on the health care system. While the development and implementation of the ACH will help alleviate the burden, these have created a new set of obstacles. In situ simulation can be an effective tool for systems testing and evaluating for preparedness during the development of an ACH. We conclude that this study was successful in identifying and resolving possible safety issues prior to the facility opening.
Conflict(s) of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this paper.




