Introduction
The implementation of evidence-based guidelines in primary health care is expected to bring about improved health outcomes, and early detection and reduction of the burden of disease. However, the precise nature of getting evidence into practice is so resistant to explanation that it has been described as occurring in a ‘black box’ (Sullivan et al., Reference Sullivan, Blevins and Kauth2008; Factor-Litvak and Sher, Reference Factor-Litvak and Sher2009). Consequently, and in spite of rigorously developed evidence-based guidelines being available and widely disseminated for a vast range of health problems, there is still a gap between evidence and practice (Miller and Kearney, Reference Miller and Kearney2004; Kitson, Reference Kitson2009). Because no ‘magic bullets’ for guideline implementation have been discovered (Shojania and Grimshaw, Reference Shojania and Grimshaw2004; Brouwers et al., Reference Brouwers, Hanna, Abdel-Motagally and Yee2009; Kitson, Reference Kitson2009), the uptake of evidence into practice remains poorly understood.
Approaches to the implementation of evidence have evolved over time from a primary focus on the nature of evidence itself (‘science push’) to the implementation behaviours of individual clinicians (‘demand pull’), and then a combination of ‘push-pull’. ‘Science push’ is a unidirectional process in which the benefit of using research evidence pushed out for clinicians to receive passively is expected to be self-evident (McWilliam et al., Reference McWilliam, Kothari, Ward-Griffin, Forbes and Leipert2009; Randell et al., Reference Randell, Mitchell, Thompson, McCaughan and Dowding2009). Passive distribution methods are still being used, perhaps for want of effective alternatives (Graham et al., Reference Graham, Logan, Harrison, Straus, Tetroe, Casswell and Robinsons2006). The consequences of the ‘science push’ approach to implementation has resulted in a lack of attention to implementation as a process and has contributed to the persisting gap between evidence and practice (Rycroft-Malone, Reference Rycroft-Malone2006).
‘Science push’ has been combined with ‘demand pull’ in which sophisticated efforts were made to educate clinicians to pull in evidence that has been presented to them in increasingly palatable forms (Dopson et al., Reference Dopson, Fitzgerald, Ferlie, Gabbay and Locock2002; Kuronen et al., Reference Kuronen, Jallinoja, Airola and Patja2010). In 235 studies comparing 309 interventions, some improvements in care were associated with reminders (14.1%), some with educational materials (8.1%), audit and feedback (7%) and a mere 6% showed improvement using multifaceted educational outreach (Grimshaw et al., Reference Grimshaw, Thomas, MacLennan, Fraser, Ramsay, Vale, Whitty, Eccles, Matowe, Shirran, Wensing, Dijkstra and Donaldson2004). However, with no definitive behavioural strategies found to improve the uptake of evidence, other approaches are required to inform the implementation of guidelines into practice.
Push and/or pull approaches to the implementation of evidence have failed to consistently influence practice decisions because they fail to accommodate the messy world of health-care practice. The facilitation of evidence into practice requires methods that acknowledge the chaos and unpredictability of health-care settings and multiple layers of interaction and change cycles (Rycroft-Malone, Reference Rycroft-Malone2008). Barriers to the adoption of evidence into practice have been attributed to a lack readiness of health professionals to change their practice, rather than a lack of willingness to change (McCormack et al., Reference McCormack, Manley and Walsh2008). Readiness to change practice is impaired by a lack of awareness, familiarity, agreement, self efficacy, motivation and expectations of success (Grol and Wensing, Reference Grol and Wensing2004; Brouwers et al., Reference Brouwers, Hanna, Abdel-Motagally and Yee2009).
Evidence-based guidelines that address major health problems have high priority for implementation. Therefore, the implementation of a guideline for reducing cardiovascular risk was chosen as the focus of this study for the likelihood that practitioners would be familiar with it and be actively using it. Cardiovascular disease is the biggest killer worldwide (World Health Organization, 2008b) and is associated globally with marked health inequity linked to ethnicity and socio-economic status (Thurston et al., Reference Thurston, Kubzansky, Kawachi and Berkman2005; Kim et al., Reference Kim, Kawachi, VAnderhoorn and Ezzati2008; Beauchamp et al., Reference Beauchamp, Peeters, Wolfe, Turrell, Harriss, Giles, English, McNeil, Magliano, Harrap, Liew, Hunt and Tonkin2010). New Zealand's indigenous Māori people, and indigenous peoples elsewhere (Baum, Reference Baum2007; Marmot, Reference Marmot2007), suffer worse health overall than non-Māori and are disproportionately affected by cardiovascular disease, the main cause of the increasing difference in life expectancy between Māori and non-Māori (Tobias et al., Reference Tobias, Sexton, Mann and Sharpe2006). Because of the imperative and urgency to improve cardiovascular health, implementation of the Assessment and Management of Cardiovascular Risk (AMCVR) guideline (New Zealand Guidelines Group, 2003) is of high priority. Implementation of that guideline was chosen for this study because of its high profile. This study aimed to explore the realities of everyday nursing practice associated with the implementation of a guideline.
Method
Design
A qualitative research approach was used in this study in order to access rich descriptions of what are complex primary health-care nursing practices. Focus groups were held with primary health-care nurses, doctors and managers associated with the implementation of the AMCVR guideline. Interviews were held with district health board primary health-care funder/planners. A general inductive approach was used to guide systematic condensing and summarising of textual data, and then linking of the summary of findings to the research objective. This method provides for interpretations that can be traced back to the words of the participants (Thomas, Reference Thomas2006).
Setting
The setting of this study is a region of New Zealand with one small city, several towns and remote rural areas. Each of these locations has characteristics that impact differently on primary health-care delivery, and therefore participants were chosen from a variety of practice settings to gain maximum variation of perspectives. The population found in the study area was believed to be at higher risk of cardiovascular disease for two reasons: a higher median age (38.9 versus 35.9) and higher proportion of Māori (31.7% versus 14.6%) than the general New Zealand population (Statistics New Zealand, 2006).
Participants
There were 33 participants, including 20 primary health-care nurses, four GPs, five primary health-care managers and three funder/planners. Primary health-care nurses were eligible for inclusion if their work was associated with the implementation of the AMCVR guideline. Doctors, managers and funder/planners were included for their perspectives of nurses’ work as they implement the guideline. All participants were working in a region of high health need with significant health inequity for Māori, particularly cardiovascular health, so that their work with the guideline was expected to have a high profile. Potential participants who were nominated by their colleagues indicated their willingness to be included and were selected to gain maximum variation of perspectives of those working with the guideline.
Data collection
Ethics approval was gained from the relevant regional New Zealand Ministry of Health Ethics Committee, the University of Technology, Sydney, Human Research Ethics Committee. Ethical standards were maintained throughout the study. Seven focus groups of three to five participants (five groups of nurses, one of doctors and one of managers), and three individual interviews with funder/planners were held to discuss the topics identified in Table 1 below. The timing and venues for data collection were at the discretion of participants; all data collection took place in meeting rooms convenient to their work places and schedules. One researcher (AM) conducted all focus groups of an average of 65 minutes for nurses’ groups, and 30 minutes for the GPs’ and managers’ groups, and three individual interviews with funder/planners of 30 minutes each. The groups and interviews were recorded and transcribed verbatim.
Table 1 Interview topics
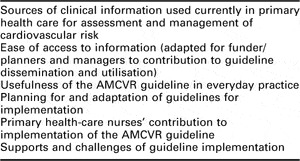
AMCVR = Assessment and Management of Cardiovascular Risk.
Data analysis
A general inductive approach to data analysis was used to access and distil the informational content of the transcribed recordings of focus groups and interviews. The purposes of such an approach are to condense raw text into a summarised format, to establish clear and transparent links between the research aim and the findings and to produce a valid, overall representation of participants’ perceptions (Thomas, Reference Thomas2006).
Data analysis involved five steps of induction informed by Thomas (Reference Thomas2006) and Pope et al. (Reference Pope, Ziebland and Mays2000). Initially, the transcriptions were read through several times to get an overall sense of what was said. The second step began with systematic annotation of the transcripts identifying the text associated with topics mentioned and naming them provisionally for their informational content. Indexing followed, with the construction of a table for each transcript including assigning code names to segments of text and then aggregating codes into categories according to similarity of content. Constant comparison of codes to verbatim data and with each other ensured the best fit for aggregating codes firstly into 29 categories that were reduced to 27 categories on further review. Categories were then aggregated for similarity of content into four provisional themes. Criteria were developed for the informational content of each theme and the goodness of fit was reviewed by tracking back from categories to codes to the verbatim data. Allocation of codes to categories and categories to themes was reviewed once more (AM) for fit against the criteria for each theme and reviewed by another author for appropriate fit (JC). Through further review and discussion of the nature of the four themes, the three authors agreed on a further level of abstraction as an overarching concept that encompassed each of the four themes. Participants were not asked to check whether the results coincided with their personal views because the overall synthesis and abstraction involved in data interpretation and analysis produced findings in which individual participants may not recognise themselves specifically or their particular narrative (Morse et al., Reference Morse, Barrett, Mayan, Olson and Spiers2002).
Results
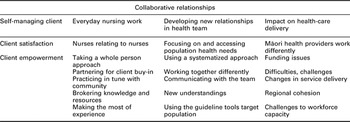
Data analysis generated four themes: self-managing patient, everyday nursing practice, developing new relationships in the health team and impact on health-care delivery. Each theme represents a facet of nurses’ work with the cardiovascular guideline, and collectively they reveal the realities of everyday nursing practice associated with the implementation of the guideline. The concept of collaborative relationships drew together the essence of each theme and is presented as the overarching theoretical construct (Table 2).
Table 2 Overarching theoretical construct with associated themes and categories
Self-managing patient
Nurses were adamant that implementing the guideline requires health care that empowers patient self-management. The ‘self’ in self-management could involve a range of family/whanau (Māori for family, usually wider than nuclear family) and/or self/other partnerships. Two characteristics of patient self-management were revealed: empowerment and satisfaction. Nurse focus groups stressed the importance of ‘letting the patient determine priorities’ to ‘set goals’ and ‘take control of their own health’. Conversation about patient self-management included acknowledgement of the complexity of the journey, both for patients and health professionals, and that readiness for change was an important factor in empowerment:
‘You can't just fix it. You've got to allow people to decide what they want … One of my kaumatua [Māori elder] says to me, “Why do you want to keep fixing me?’
(Practice Nurse)
Empowerment was valued highly by all participants as foundational to self-management:
‘For the patient to become self-managing, that's the goal. It's knowing how to get there. A journey in itself…’
(Practice Nurse)
Even though a patient's choices may not be optimally cardio-protective, nurse participants voiced their respect for a patient's right to decide the timing and pace of change: ‘You can't just fix it. You've got to allow people to decide what they want …’ (Practice Nurse). Patient satisfaction was apparent from nurses’ observations that patients appreciate intensive one-on-one education and planning associated with implementing the guideline.
‘The feedback from the patients is just amazing and that something they mention a lot is that they really value their wellness plan because they own it. They're setting their own achievable small goals … Instead of just going to their GP to get their three monthly prescriptions for meds’
(Practice Nurse)
This theme underscored nurses’ patient-centred approach to implementing the AMCVR guideline and their awareness of the importance of building relationships to optimise patients’ self-care.
Everyday nursing practice
Everyday nursing practice represented how nurses worked towards the integration of guideline recommendations into usual health care overall so that it was embedded in normal practice. Nurses spoke about the need to use knowledge gained from experience and to tap into a wide variety of community-based resources to help patients make lifestyle changes. Cardiovascular risk assessment was seen by nurses as just one aspect of overall health assessment.
Nurses were aware that the level of deprivation that a person experienced was closely associated with their level of cardiovascular risk. The whole person view required an understanding of overall life circumstances, support needs and pace of change. One nurse group spoke about offering comprehensive care:
‘I don't care about cv risk [whispering] I care about the relationship I have with them [patients]. Because for us we're a community development team. We look at all of the family … so if there's any older people in the house, “Do you need anything? We have a home-based nursing service. Do you need some home-care for your elderly?” ’
Goal setting had to be realistic, and for some patients multi-generational poverty had created a sense of hopelessness:
‘There are a lot of social factors you know. People who are unemployed. They never really get a good job. They never have that steady income. There are a lot of things that are out of their control’
(Practice Nurse)
Cardiovascular health as a life-long goal required ongoing support for patients. Participants agreed that sustained support following risk assessment requires enduring relationships. Nurse participants appreciated the importance of being available and accessible to their patients:
Nurse 1 – ‘And they come here because they know that we care about them’.
Nurse 2 – ‘We'll listen to them’.
Nurse 3 – ‘We'll take the time’.
However, they were also concerned that mass screening would create heavy demands not only on health-care services, but would also expose the need for coordination of community-based help for people:
‘… you have to have services to refer people to. No point in identifying a risk if you can't do anything about it. And it has been about making sure that everyone has access to the range of services … I mean it's not just a matter of saying “You've got a risk here. Take a pill”; “You've got transport? Na”- those sort of things …’
(Manager)
In spite of their concerns about implementing the guideline:
‘… nurses have just jumped at this whole new approach…. It's as if the nurses are doing what they became a nurse for … They've actually become, like “ I'm home” ’
(Practice Nurse)
Nurse focus groups spoke about how they valued their relationships with each other, but were concerned about a lack of communication about how to implement the guideline. The guideline recommended what to do but not how to do it and they were not sharing the know-how of their practice.
Developing new relationships in the health team
Implementation of the guideline in a changing health-care environment has resulted in clinicians working together differently. The sheer volume of work involved in cardiovascular screening and follow-up has been one factor that has contributed to a realisation of the largely untapped potential of nurses in general practice. Changes in practice associated with implementing the guideline were more positive for nurses than for doctors. As nurses were taking on a more satisfying role in direct patient care, doctors also needed to change their practice in a number of ways that required new understandings in the health-care team.
As primary health-care nurses adopted a more active role in patient consultations, there was a noticeable change in how doctors and nurses were relating:
‘I think for me it's meant that you work with the GP as a team and I think over the last few years, with a lot of the things that we've been doing it's become a team effort… gives you a feeling of trust and respect’
(Practice Nurse)
Working together differently resulted in better teamwork and made a difference to patients’ knowledge and confidence. One of the nurse groups found that:
‘People with chronic diseases don't come in asking about their pills. With better education they're more at ease about how things are going because they are more in control. So the doctors are rapt because it saves them time. So it's good teamwork’
(Practice Nurse)
In addition, nurse-led clinics were working well for cardiovascular risk assessment and ongoing self-management:
‘We've run a nurse-led clinic for many years so it allows some independence for a lot of the nurses and I'd say a lot of the CVD risk is initiated by the practice nurse’
(Practice Nurse)
Even though GPs were aware of the health promotion needs of their enrolled populations, they were overwhelmed with treating those with illness, especially in areas of high health need where there are:
‘… just over 70% Māori and a fairly high level of deprivation and high morbidity which puts a heavy workload to cover that. And lots of comorbidities. … our doctor-nurse ratio is pretty high and our patient–doctor ratio is pretty high … we're stretched’
(GP)
The GP group indicated they were at a loss as to how to encourage healthy people to come forward for cardiovascular screening. They were more at ease with ‘explaining to them (patients who present for treatment) what they should do’ (GP). Māori health-care providers had more active relationships with the entire population they served (mainly Māori) than general practice providers who tend to see only those patients who came through the door of their clinic with a problem or needing a prescription repeat. As one funder/planner put it:
‘Māori providers themselves know how to access and link [with the Māori population]. [But for others] there are cross-cultural issues getting the right service to the right people at the right time’
(Funder/planner)
Impact on health-care delivery
The last theme concerned the impact on guideline implementation of difficulties in communication, integration and coordination of care across the region and the lack of resources available to services. All the clinician groups conveyed a sense of despair that they did not have the capacity for integrated and coordinated cardiovascular risk profiling, mass cardiovascular screening and the follow-up that was required after assessment.
A common concern and frustration for all participant groups was the lack of funding to implement the guideline. The GP group was particularly despondent about the lack of financial assistance:
Doctor 1 – ‘That's what the problem is. You know the guideline is being pushed to save money at the other end. It makes sense doesn't it, economically?’
Doctor 2 – ‘But we really need to be resourced at this end. I'm amazed. … No resourcing at this end! You must be mad. It's just a crazy situation! It's not going to work! It's all gonna fall flat!’
A practice nurse group was equally at loss as to how they were going to implement the guideline within existing resources:
Nurse 2 – ‘There's no point screening if you can't follow up with what's required …’
Nurse 3 – ‘… there was nothing actually about what you gonna do when you've found them! Who's gonna pay for all this extra work that is going to be done?’
A lack of coordination and data sharing among practices interfered with community-based mass screening of the target population. Screening was a waste of time if the clinical data and risk score were not accessible to those who would follow-up with the patient. At least when screening was held at a GP clinic, the patients coming through the door were likely to be enrolled at that practice. As one nurse participant explained:
‘… going into work places, they may not be our patients … If you identify a risk, how are you gonna manage non-registered patients?’
All focus groups were concerned about the capacity of the primary health-care workforce to implement all of the guideline recommendations and were at a loss to know how to cope especially with screening and early detection. Nurses, doctors and managers spoke about the challenges of clinical staff shortages and the need for upskilling health professionals. The GP group acknowledged that although most of the work involved in implementing the guideline could be carried out by practice nurses (eg, risk assessment, patient education and follow-up), there were not enough of them to do that.
The four themes depict motivated, person-centric, health professional teams who agree with the intentions of the guideline, but are struggling to find ways to implement the recommendations for prevention and screening, given their existing workload. The notion of collaborative relationships was central to each of the themes and formed an overarching connection among them. In the first theme, a mutually trusting relationship between clinicians and patients in supporting self-management was central to all other relationships involved in implementing the guideline. The second theme, everyday nursing practice, focussed on the need to build professional know-how through sharing insights gained from weaving the guideline recommendations into usual care. The third theme, developing new relationships in the health team, revealed that interdisciplinary collaboration enhanced patient–clinician collaboration and engendered better doctor–nurse teamwork. The fourth theme captured the frustration of clinicians struggling to gain the resources required for the communication, integration and coordination of care to support guideline implementation.
Discussion
Even though the AMCVR guideline provided high-quality evidence for what to do, it failed to satisfy health-care professionals’ need to know how to implement the recommendations. In spite of their clear willingness to work with the guideline, a lack of knowing how to do this successfully has caused confusion and frustration and led to fragmentation of services. The importance of collaborative relationships between all players involved in implementation of the guideline in this study has been well represented in the literature (D'Amour et al., Reference D'Amour, Ferrada-Videla, San Martin Rodriguez and Beaulieu2005; Reeves et al., Reference Reeves, Zwarenstein, Goldman, Barr, Freeth, Hammick and Koppel2009; Shultz and Kitson, Reference Shultz and Kitson2010; Gaboury et al., Reference Gaboury, M. Lapierre, Boon and Moher2011; Jackson and Bluteau, Reference Jackson and Bluteau2011; Schmidt, Reference Schmidt2011). This study has underscored not only the importance of collaborative relationships between health professionals, but also the crucial role of relationships with patients, their families and agencies outside a general practice in the implementation of this guideline.
Person-centric values and beliefs about concordance, empowerment and working together with patients were found to be pivotal in this study to implementing the AMCVR guideline because, ultimately, enacting the recommendations is at the patient's discretion. Concordance refers to partnership in decision-making between health professionals and patients in which patients’ preferences are elicited, valued and respected in the context of co-interpretation and co-conceptualisation (Parker, Reference Parker2005). An essential element of concordant relationships is cultural competence (Betancourt et al., Reference Betancourt, Green, Carrillo and Park2005). Cultural competence is vitally important in health care and has special meaning in New Zealand in light of the imperative to reduce health inequity for Māori (Cram et al., Reference Cram, Smith and Johnstone2003; Hefford et al., Reference Hefford, Crampton and Foley2005). A holistic and relational Māori view of health is an essential element in health and healing, including the importance of wairua (spirit) and whanau (family). From a Māori patient's point of view, health care that has been designed to be culturally appropriate, affordable and accessible gains a high level of patient satisfaction (Maniapoto and Gribben, Reference Maniapoto and Gribben2003). Further research is required to develop knowledge about culturally competent care, which addresses cardiovascular health inequity through implementing the AMCVR guideline.
The role of the patient as principal implementer of evidence in primary health care has been underscored in this study, a factor scarcely recognised in the guideline implementation literature that has so far been more focussed on the behaviours and attitudes of health professionals than on relationships with patients (Grol and Grimshaw, Reference Grol and Grimshaw2003; DiCenso et al., Reference Dicenso, Guyatt and Ciliska2005; Kuronen et al., Reference Kuronen, Jallinoja, Airola and Patja2010), even though reliable predictors of change in professional practice have not been found (Hulscher et al., Reference Hulscher, Wensing, Weijden and Grol2005). In particular, there is a paucity of research about primary health-care practice that leads to health promoting actions of patients (Hrisos et al., Reference Hrisos, Eccles, Francis, Dickinson, Kaner, Beyer and Johnston2009).
Ideally, primary health care for individuals has a population-based approach that addresses inequity at the level of the social determinants of health (Keller et al., Reference Keller, Strohschein, Lia-Hoagberg and Schaffer2004; Neuwelt et al., Reference Neuwelt, Matheson, Arroll, Dowell, Winnard, Crampton, Sheridan and Cumming2009; Edgecombe and Stephens, Reference Edgecombe and Stephens2010). Primary health care is ineffective if it fails to address socio-economic disparities as the most direct means of improving population health (Gervas et al., Reference Gervas, Starfield and Heath2008; World Health Organization, 2008a; Goldberg, Reference Goldberg2009). Participants in this study were aware that treating the biophysical effects of disease characterises a ‘short-term, problem specific, individual-based “downstream” approach’ (Cypress, Reference Cypress2004: 249). Upstream actions are required that strengthen the determinants of health – education, employment, housing, nutrition, income and working conditions (Marmot, Reference Marmot2003; Keller et al., Reference Keller, Strohschein, Lia-Hoagberg and Schaffer2004; Sharpe, Reference Sharpe2006; World Health Organization, 2008a). However, in spite of many guidelines for primary health care, professionals are frustrated and powerless to know how to implement evidence in a way that influences the social determinants of health in vulnerable populations.
A traditional model of clinic-based, illness-focussed primary health care is not conducive to the provision of care that includes health promotion and disease prevention (Workforce Taskforce, 2008; Kuronen et al., Reference Kuronen, Jallinoja, Airola and Patja2010). Even with the best of intentions, such a care environment is bound to cater best for patients attending for treatment rather than delivering on population health outcomes (Daniels et al., Reference Daniels, Kennedy and Kawachi2000; Marmot, Reference Marmot2003; Goldberg, Reference Goldberg2009). The people, processes and structures that impact on care co-create the culture of a clinical environment and are equally implicated in cultural change (Smith, Reference Smith2009; McCormack and McCance, Reference McCormack and McCance2010). Cultural change is difficult to achieve in any clinical setting; however, geographic distances between numerous small general practices in rural settings present challenges to communication and collaboration.
Solutions to difficult clinical practice challenges require active processes of facilitated support (Bandura, Reference Bandura2000; Bandura, Reference Bandura2006; Manley, Reference Manley2008; McCormack et al., Reference McCormack, Manley and Walsh2008; Walsh et al., Reference Walsh, Moss, Lawless, McKelvie and Duncan2008). Health professionals’ awareness of the interactions between their work activities and the social context of their practice positions them well to envision change (Manley et al., Reference Manley, Titchen and Hardy2009; Nairn, Reference Nairn2009). Clinicians in this study recognised the benefits of working more collegially and extending their everyday relationships to include other health and social services professionals. The positive association that has been found between team-level job satisfaction and quality of care (Mohr et al., Reference Mohr, Young, Meterko, Stolzmann and White2011; Roblin et al., Reference Roblin, Howard, Junling and Becker2011), as well as the role of interagency collaboration in problem solving (Daley, Reference Daley2009) underlines the importance of collaborative relationships within a team and across organisations.
How things are done and what counts as important reflects the inherent values and beliefs that shape a clinical context (Walsh et al., Reference Walsh, Moss and Fitzgerald2006; McCormack and McCance, Reference McCormack and McCance2010), and the work involved in co-creating new ways of working results in improved collegial relationships (Manley, Reference Manley2004). Active collaboration across several general practices at some distance apart may be achieved through the development of communities of practice in which clinicians use video conferencing, web-based social networking and file sharing to support case-review for the purpose of making sense of their experiences, share concerns, reflect on approaches to care and develop new care strategies (Soubhi et al., Reference Soubhi, Bayliss, Fortin, Hudon, Van den Akker, Thivierge, Posel and Fleiszer2010). Further research is required to explore the process and outcome/s of social participation, collective sense-making and bridging the gap between knowing and doing in communities of practice (Soubhi et al., Reference Soubhi, Bayliss, Fortin, Hudon, Van den Akker, Thivierge, Posel and Fleiszer2010).
Not all barriers to the successful implementation of a guideline can be addressed by clinicians in their workplace. Some problems require infrastructural, multi-sectorial, governance, policy and funding interventions (Workforce Taskforce, 2008). For example, health inequity in indigenous peoples is a worldwide issue that must be addressed at all levels in health-care systems (Bacal et al., Reference Bacal, Jansen and Smith2006). This study has emphasised the problems of capacity and capability of the primary health-care workforce to address health inequity for their Māori patients. Others have called for workforce development specifically focussed at recruiting, retaining and strengthening a culturally appropriate health and disability workforce (Ramsden, Reference Ramsden1997; Durie, Reference Durie2003; Ratima et al., Reference Ratima, Brown, Garrett, Wikaire, Ngawati, Aspin and Potaka2007). Furthermore, the structural and socio-economic causes of health inequity must be addressed at the highest level of governance, funding and policy (Marmot, Reference Marmot2010).
The findings have revealed the realities of the implementation of the AMCVR guideline in primary health care. Nurses were committed to improving their practice in spite of environmental constraints on their work. However, there was a pervading sense of despair and frustration about implementing the AMCVR guideline because of a lack of knowing how to do that. The purpose of this study was to provide detailed understanding of guideline implementation for these participants rather than to produce generalisable findings. However, as suggested by Ritchie and Lewis (Reference Ritchie and Lewis2003), when there is homogeneity of the clinical work of several participants, a degree of theoretical transferability is possible.
Conclusions and implications
The findings of this study have provided insight into the essential nature of collaborative relationships in knowing not only what is recommended in a guideline, but also how to weave the recommendations into everyday practice. Health professionals in this study showed that they value the guideline, have a person-centred orientation to care and are willing to implement the guideline, but that skilled facilitation is required for the discovery of new ways of working that are appropriate to the context of their everyday work. The most obvious implication for clinicians is the absolute need for support, processes and resources to develop evidence that informs how to implement guideline recommendations, in addition to recommendations for health-care interventions. Health-care funders and policymakers need to find long-term solutions to the problems of the current funding and service model of primary health care, which addresses the failure to adequately compensate and incentivise health-care providers for the implementation of clinical practice guidelines, especially for preventative health-care interventions. A further implication of this study is that further investment is required in development of clinical leadership at all levels of primary health-care governance and provision.
Acknowledgement
The Ministry of Health, New Zealand, provided funding support for data collection for this study.




