Managing episodes of acute mental illness without admission to hospital has been advocated since the 1960s (Reference Wasylenki, Gehrs and GoeringWasylenki et al, 1997). In England, government policy for mental healthcare proposed the setting up of 335 crisis resolution teams nationally for this purpose (Department of Health, 1999, 2000). The studies cited to attest to their likely efficacy (Reference Joy, Adams and RiceJoy et al, 1998) describe work from the 1970s and 1980s. At the time it was argued that this evidence base was dated, taking old fashioned asylum care as its reference point, rather than services based around community mental health teams which, by then, were the norm (Reference Pelosi and JacksonPelosi & Jackson, 2000).
Johnson and colleagues (Reference Johnson, Nolan and Hoult2005a ,Reference Johnson, Nolan and Pilling b ), working in North London, have reported a before-and-after and a randomised controlled trial of a crisis resolution team. Both indicated a substantial reduction in admissions. However, both described a service which had recruited one of the foremost clinical leaders in the field. It is thus reasonable for us to ask whether similar gains could be achieved widely.
Between 2001 and 2004 there was a rapid expansion in the number of crisis resolution teams in England (Glover & Barnes, Reference Glover and Barnes2002, Reference Glover and Barnes2004, Reference Glover and Barnes2005). We set out to explore the extent to which these were successful in reducing admissions, comparing admission trends in areas grouped on the basis of their implementation history.
The same government policy also mandated the setting up of a national network of assertive outreach teams providing intensive community-based support for frequently relapsing and difficult-to-engage patients. These were implemented more quickly than crisis resolution teams. We studied these in parallel.
METHOD
Data sources
Outcome data came from English National Health Service (NHS) routine admissions statistics. Records of general psychiatric admissions for adults under 65 years of age were collated to give numbers and occupied-bed-days for health administrative areas (primary care trusts) for the 6 administrative years 1998/9 to 2003/4. Psychiatric sub-specialties including forensic, psychotherapy and learning disabilities were excluded. Admissions crossing the end of the administrative year (31 March/1 April) were also omitted, as these can sometimes be double counted.
Details of crisis resolution teams and assertive outreach teams were taken from the annual mental health service mapping set up to monitor policy implementation (Glover & Barnes, Reference Glover and Barnes2002, Reference Glover and Barnes2004, Reference Glover and Barnes2005). These were among the most carefully scrutinised items in this source, as they were used for rating local performance and to report progress towards high-profile government targets. Data from 2001, 2002 and 2003 were used to identify the date of first appearance of each team, the primary care trust areas it served and its model fidelity characteristics for each year. From these, primary care trusts were grouped on the basis of the year in which they first acquired any crisis resolution or assertive outreach team (broad definitions), any crisis resolution team on call 24 hours a day, 7 days a week (‘24/7’), or assertive outreach team with evening and weekend working (narrow definitions). Other model fidelity characteristics for which data were available were based on softer (adherence to specified working styles) or more contentious (24/7 on call for assertive outreach) criteria.
We used mixed analysis of variance to test the association between team provision and the repeated measure of annual admissions to hospital. Covariates were the size of the population and the Department of Health's Allocation of Resources to English Areas (AREA) mental health needs index (Reference Sutton, Gravelle and MorrisSutton et al, 2000). Separate exercises were undertaken for all working age adults and for younger (age 18–34 years) and older (35–64 years) men and women. Two sets of models were constructed, one using designations based on broad team definitions, the other on restrictive definitions. We estimated the scale of impact of team implementation on hospital admissions and bed use by calculating the differences (attributable reduction) seen in mean values for the change from the first to the last 2-year period for which we had data. Here, primary care trusts with teams established by 2001, and those with no teams by 2003, were compared using unpaired t-tests.
Data were analysed using the Statistical Package for the Social Sciences version 12.01 for Windows.
Preliminary data inspection and cleaning
Both data sources were inspected in detail for quality before analysis. Of 303 primary care trusts, team provision data were ambiguous for 19, and 2 underwent a boundary change preventing trend analysis. Hospital admission data showed substantial omission of patients’ genders in 10 primary care trusts, and worrying discontinuities in admission numbers (a rise or fall by more than 50% or 33% respectively, in any single year) in 130 primary care trusts. In 69 of these, discontinuity problems related to a single year, and three independent observers, masked to the identity or team status of the areas, agreed that the remaining observations indicated an unambiguous trend from which the missing point could be calculated. On this basis, 74 primary care trusts were omitted from analysis, leaving 229, 69 of which had one smoothed point in their admission data. This represents 76% of the total, between them covering 22.6 million people aged 18–64 years.
RESULTS
Over the 6 years, admissions in the 229 primary care trusts overall fell by 23% for younger and 0.5% for older people. For all ages combined, the median change was –11%, (interquartile range +6% to –23%). Crisis resolution teams were already in place in 34 (15%) of the primary care trusts by 2001; 14 (6%) and 51 (22%) added teams in 2002 and 2003 respectively, leaving 130 (57%) with no team. Crisis resolution teams that were always on call were in place in 12 (5%) primary care trusts in 2001, with 10 (4%) and 30 (13%) reaching this level of provision over the next 2 years respectively. Assertive outreach teams appeared more rapidly; 144 primary care trusts (63%) had this facility by 2001, with 23 (10%) and 36 (16%) following in 2002 and 2003 respectively, leaving only 26 (11%) uncovered. Assertive outreach teams providing evening and weekend working were seen in 86 (38%) primary care trusts in 2001, with a further 18 (8%) and 38 (17%) achieving this in 2002 and 2003 respectively.
Simple inspection of the change in hospital admission numbers suggested that crisis resolution teams were associated with greater falls; 74% of primary care trusts with a broadly defined crisis resolution team and 83% of those with a narrowly defined team in place by 2001 showed a fall in total admissions, compared with only 60% of those with no team by 2003/4. The impact appeared greater for older patients and for women. By contrast, the effect of assertive outreach teams was erratic with, if anything, smaller proportions of primary care trusts with assertive outreach teams showing a fall.
Figure 1 shows plots of the modelled trends in the average annual hospital admission numbers for primary care trusts, grouped by year of first provision, from the mixed analysis of variance. The two plots on the left are drawn from the model using broad definitions for both team types. Those on the right are based on restrictive definitions and include an additional category for primary care trusts with teams but not reaching the narrow definition level. Both graphs in relation to crisis team provision show the line for primary care trusts with teams in place by 2001 falling much more sharply than that for those with no team. For assertive outreach, primary care trusts with no provision show sharper falls than others although, in this case, in the model using restrictive team definitions the plots are not statistically significantly different even at the P<0.05 level.

Fig. 1 Modelled trends in mean annual hospital admissions for people of both genders and age-groups, for primary care trusts grouped by team provision status. CRT, crisis resolution team; AOT, assertive outreach team.
Models were calculated for all hospital admissions, and for the four age/gender subgroups. For broadly defined crisis resolution teams, only the model for women aged 35–64 years showed a significant effect at the P<0.001 level. For restrictively defined crisis resolution teams, this level was reached by the models for all admissions, and admissions for older men and women. The model for younger women was highly significant (P=0.003), but not that for younger men (P=0.03). Broadly defined assertive outreach team status was significantly associated with less reduction in admission at the P<0.01 level only in the model for older women (P=0.005), narrowly defined status not at all. Models for bed usage generally produced weaker significance levels. At the P<0.01 level, only restrictively defined crisis resolution team status figured significantly (all people, P=0.005; younger women, P=0.005; older men, P<0.001). To check that the process of data smoothing for the 69 primary care trusts with isolated defective data points had not substantially altered the result, all these analyses were re-run omitting these records. Apart from generally weaker significance levels, the pattern was unchanged.
If greater reduction in hospital admissions was a consequence of implementation of crisis resolution teams, it should follow in time. Figure 2 shows plots for modelled admission numbers in primary care trusts classified by the year of first provision of restrictively defined crisis resolution teams for younger and older working age adults separately. In the chart for those aged 35–64 years, the gradient of the plot for primary care trusts introducing teams in 2002 shows a marked change at the appropriate point. This time-related feature was seen in plots for both women and men in this age-group, but not in plots for younger people. The plot for areas introducing teams by 2001 shows a falling trend preceding 2001; as noted above, many of these teams were in place several years before this date.
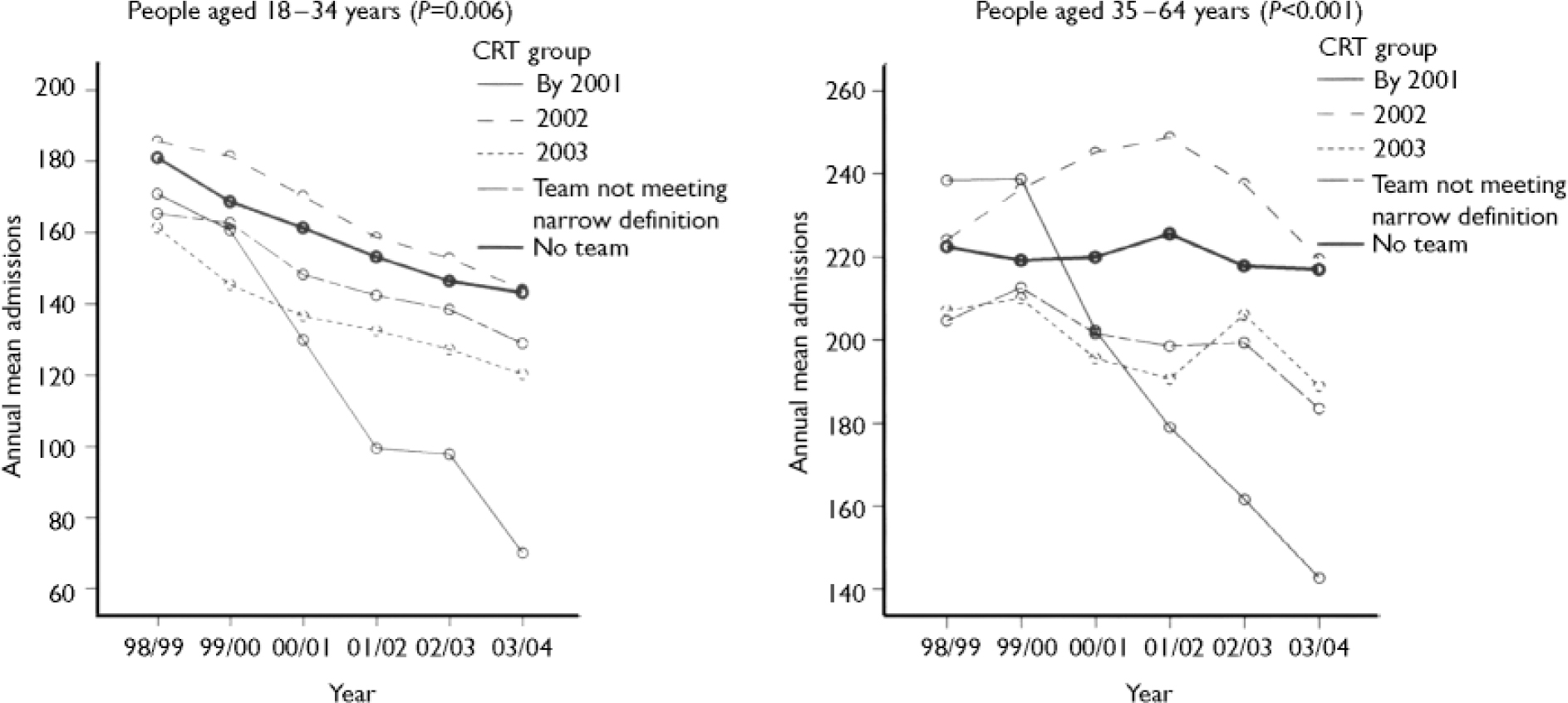
Fig. 2 Modelled trends in mean annual admissions for younger and older people, for primary care trusts grouped by 24/7 crisis team provision. CRT, crisis resolution team.
Finally, we explored the extent to which crisis teams were associated with reductions in hospital admissions and bed requirements. Table 1 shows the differences between the changes seen in primary care trusts with teams established by 2001 and those with no teams. Restrictively defined crisis resolution teams were associated with an attributable reduction of a little over 20% in admissions. The reduction for older adults was about one and a half times that for younger working age adults. When all crisis teams were included, significant falls, but of only half the magnitude, were seen for people aged 35–64 years; for younger adults, no significant fall was seen. Attributable falls in bed usage were lower and less statistically significant.
Table 1 Difference in mean fall in hospital admissions and bed days, between primary care trusts with crisis resolution teams introduced by 2001 and those with no teams by 2003, using broad (n=34 and 130) and narrow (n=12 and 130) team definitions

| Data | Difference, % (95% CI) | P |
|---|---|---|
| Broadly defined crisis teams | ||
| Admissions | ||
| All people | -9.9 (-1.7 to -18.1) | 0.02 |
| Women | ||
| 18-34 years | -8.8 (1.9 to -19.5) | 0.103 |
| 35-64 years | -14.6 (-3.0 to -26.2) | 0.014 |
| Men | ||
| 18-34 years | -6.1 (5.7 to -17.9) | 0.305 |
| 35-64 years | -11.5 (-2.2 to -20.8) | 0.016 |
| Bed days | ||
| All people | -3.6 (4.5 to -11.7) | 0.373 |
| Women | ||
| 18-34 years | -8.0 (2.2 to -18.3) | 0.123 |
| 35-64 years | -13.1 (3.3 to -29.4) | 0.117 |
| Men | ||
| 18-34 years | 5.0 (20.1 to -10.1) | 0.51 |
| 35-64 years | -7.2 (5.5 to -20.0) | 0.263 |
| Narrowly defined crisis teams | ||
| Admissions | ||
| All people | -22.7 (-7.1 to -38.4) | 0.008 |
| Women | ||
| 18-34 years | -22.7 (-5.2 to -40.2) | 0.015 |
| 35-64 years | -30.6 (-16.5 to -44.8) | <0.001 |
| Men | ||
| 18-34 years | -16.4 (6.8 to -39.7) | 0.149 |
| 35-64 years | -25.5 (-8.1 to -43.0) | 0.007 |
| Bed days | ||
| All people | -11.6 (5.1 to -28.2) | 0.157 |
| Women | ||
| 18-34 years | -16.5 (6.7 to -39.7) | 0.148 |
| 35-64 years | -23.7 (-2.4 to -45.0) | 0.031 |
| Men | ||
| 18-34 years | 6.4 (42.1 to -29.4) | 0.705 |
| 35-64 years | -21.2 (-3.3 to -39.1) | 0.023 |
DISCUSSION
This paper reports an uncontrolled observational study of trends in psychiatric hospital admission across England and their relationship to the implementation of crisis resolution teams and assertive out-reach teams. Clearly other factors influencing admissions would have been at work at the same time, but with such large changes in the provision of these teams over such a short period it seems reasonable to explore whether any impact is discernible.
There was a widespread fall in hospital admission numbers over the period we studied, in areas with and without new teams. Hence this observation alone in any single area is insufficient to establish the effectiveness of a crisis resolution team. We were able to demonstrate that areas which implemented crisis resolution teams showed greater reductions in admissions for older working age adults than areas which did not, and that where these were always on call, reductions were more marked and were also seen for younger adults. The scale of the reduction in admissions (20% with teams always on call) was much smaller than that reported by early authors (Reference Hoult, Rosen and ReynoldsHoult et al, 1984), but close to the two recent English reports (Reference Harrison, Alam and MarshallHarrison et al, 2001; Reference Johnson, Nolan and HoultJohnson et al, 2005a ). Occupied-bed days also fell in areas with teams always on call, although the difference was smaller (10% overall) and statistically significant only for older working age adults.
Implementation of assertive outreach teams was not associated with any additional reduction in admissions. This was not surprising since the evidence that they reduce admissions in a modern English context is more equivocal (Reference Burns, Creed and FahyBurns et al, 1999; Reference Marshall and LockwoodMarshall & Lockwood, 2000; Reference Killaspy, Bebbington and BlizardKillaspy et al, 2006). The effectiveness observed in the Cochrane review (Reference Marshall and LockwoodMarshall & Lockwood, 2000) arose entirely from two American studies of the 1980s – the only English study included showed no difference. Moreover, assertive outreach teams only care for a small proportion of those who are admitted to hospital, so their impact on total admission rates could only be limited.
The questions raised by the study fall into two broad areas: the reliability and scope of the data and their interpretation.
Our admission data source was deficient in scope in two ways. First, it excluded NHS patients admitted to the independent hospitals sometimes used for overspill provision. Second, the government target number of crisis resolution teams (335) indicated about one for each primary care trust, but the alignment of boundaries was not always exact. Routinely collected data might also be of poorer quality than those collected for research. The period studied was characterised by an unusually large amount of administrative reorganisation which may have had additional adverse effects on the data we used. We have described the data cleaning process we undertook before joining the admission and team data for individual areas. However, these types of weaknesses would be expected to obscure, not produce the type of detailed patterns seen.
Other factors may have had a confounding influence if they were introduced in parallel in the same areas as crisis resolution teams. We attempted to study three such factors. The number of in-patient beds in England was fairly stable in the first half of the period studied, reflecting government sensitivity about possible shortages (Department of Health, 1997). In the second half it fell by about 5%. We attempted a systematic analysis to establish whether primary care trusts with crisis teams were served by hospital trusts which had reduced beds more than others. However, this proved unworkable, since most hospital trusts cover several primary care trusts and the allocation of beds is seldom firmly fixed.
We also explored whether data on crisis accommodation and day hospital provision were sufficiently clear to be brought into the model. In both cases the difficulty was the heterogeneity of these types of service (Reference Briscoe, McCabe and PriebeBriscoe et al, 2004). Whereas some appeared to offer realistic alternatives to admission, others did not; for most our data were unclear. Crisis accommodation showed limited growth (from 160 to 220 beds nationally) and day hospital capacity appeared to reduce.
Interpreting the data
The study showed an association between crisis team implementation and reduction in admissions far beyond what is plausible as a chance finding. However, the range of trends in areas both with and without crisis resolution teams underlined the fact that other influences must have been at work.
One possible explanation of our findings is that rapid implementation of policy on crisis resolution teams might have been serving as a marker of generally efficient, well-run services. Such areas might also be expected to be active in other ways that could reduce admissions without the crisis resolution teams being the mechanism. The best argument against this explanation for the present findings was the difference between the apparent effects of early introduction of the two different sorts of team. Crisis resolution teams were associated with reduced admissions, assertive outreach teams were not.
The disparity between the effect on admissions and bed use was an important finding. Our study could not indicate whether this was because short hospital admissions of less severely ill people were the most preventable, because the people who did still get admitted stayed longer, perhaps because the pressure to discharge them had been reduced or possibly for other reasons. This is an important issue, as the implications for ward and bed management are different.
The reasons underlying the importance of 24 h, 7-day on-call provision cannot be directly determined from the study. The specific relevance of this to effectiveness with younger clients could reflect their greater volatility. However, it could equally be a proxy marker for teams that are better led, designed and resourced.
The additional reductions in hospital admissions were seen most clearly in the teams implemented earliest. One reason for this may simply be that they had longer to show the effect. Unfortunately, this means that the study can still be criticised as demonstrating only the success of crisis resolution teams when implemented by its protagonists, but it cannot be dismissed as anecdotal. The groups of primary care trusts with restrictively defined crisis resolution teams in place by 2002 covered 12% of the population of England, and in the last year for which we have data they recorded 9658 hospital admissions. Our estimate that crisis resolution teams prevented 20% of admissions suggests they averted a further two and a half thousand.
Acknowledgements
We are grateful to Di Barnes and Steven Bradley of the Durham service mapping team for their contributions. The study was funded by the Department of Health.






eLetters
No eLetters have been published for this article.