We're very grateful: moral emotions, role models, and trust predict vaccine uptake intent in India
India has been at centrestage of the global fight against the COVID-19 pandemic, with more than 44 million cases and more than half a million deaths (as of Feb 2023). There is also growing concern over the emergence of newer mutations and variants of the virus. The pandemic in India triggered a humanitarian crisis among its vulnerable groups such as the poor, migrant workers, and marginalized sections. Having suffered through a third wave of outbreak owing to the Omicron variant in January 2022, the Government of India and state governments have stepped up vaccination efforts since the second wave, which was in March–June 2021. By February 2023, more than 2.2 billion vaccine doses were administered in India, with recent government data indicating that more than 70% of the eligible population had received at least one dose. However, the fraction of fully vaccinated people (67% as of February 2023) is far behind that of other countries that face a similar burden of COVID-19 cases (Ritchie et al., Reference Ritchie, Mathieu, Rodés-Guirao, Appel, Giattino, Ortiz-Ospina, Hasell, Macdonald, Beltekian and Roser2020).
In order to prevent catastrophic effects of subsequent waves related to variants of concern, health experts have argued for the need to extensively scale up vaccination coverage, particularly among densely packed urban populations (Mandal et al., Reference Mandal, Bhatnagar, Arinaminpathy, Agarwal, Chowdhury, Murhekar, Gangakhedkar and Sarkar2020; Pandey et al., Reference Pandey, Sah, Moghadas, Mandal, Banerjee, Hotez and Galvani2021). Prior to May 2021, vaccine availability was a significant challenge for achieving this ambitious goal, but since then several new vaccines have received approval in India and have been made available to the adult population. However, attitudes and perceptions related to vaccines, as well as their acceptability, have remained uncertain since India's first phase of vaccinations began with frontline workers and doctors in January 2021.
COVID-19 vaccine hesitancy in India
As international scientific efforts progress in developing and delivering effective vaccines to provide immunity against COVID-19, it becomes important to examine the various factors associated with willingness and/or intention to take a COVID-19 vaccine when available. In countries like India, where cultural heterogeneity is along various dimensions, it becomes important to understand underlying attitudes related to the COVID-19 vaccine in order to better frame messaging and communication interventions to encourage vaccine uptake (see also Tagat et al., Reference Tagat, Kapoor, Arora, Chakravarty, Mukherjee and Roy2022; Ticku et al., Reference Ticku, Puthillam and Kapoor2021). However, there has been relatively little work done on exploring behavioural factors associated with vaccine hesitancy among adults and the COVID-19 vaccine in India.Footnote 1 Large-scale national surveys (e.g. Bansal et al., Reference Bansal, Raj, Shukla and Sunder2021; Umakanthan et al., Reference Umakanthan, Patil, Subramaniam and Sharma2021) have found that wealthier individuals (higher income, residents of urban housing communities, those able to maintain social distancing, among others) were in general more favourable towards taking the COVID-19 vaccine in India. Common concerns around the vaccine were similar to the findings from Danabal et al. (Reference Danabal, Magesh, Saravanan and Gopichandran2021), mostly related to adverse side effects. In a specialized sample of medical students in India, vaccine hesitancy was much lower at 10.6% (February–March 2021); however, concerns related to vaccine efficacy, mistrust in government agencies, and lack of awareness regarding eligibility for the vaccine contributed to hesitancy (Jain et al., Reference Jain, Saurabh, Kumar, Verma, Goel, Gupta, Bhardwaj and Raghav2021). Tagat et al. (Reference Tagat, Kapoor, Arora, Chakravarty, Mukherjee and Roy2022) also noted how beliefs in vaccine effectiveness impact vaccine uptake behaviours.
Against this background of existing scholarship on COVID-19 vaccine hesitancy and attitudes, knowledge, and perceptions towards vaccines, we examine the role of three previously unexplored behavioural factors in predicting vaccine uptake intent in India. Note that we are unable to examine vaccine uptake and recognize that there could be an intent-action gap in such self-report measures of willingness to take the vaccine that our analysis may not fully account for. Specifically, we wish to address research questions related to the impact of each of the below factors on vaccine uptake intent in India: preventive health behaviours (PHBs) (RQ1a); interpersonal trust and role models (RQ1b) and positive and negative moral emotions (RQ1c). Furthermore, we also explore the association between COVID-19 infection/vaccination status and past PHBs (RQ2). We use data from an extensive online survey conducted between May and June 2021 in India with 953 participants. Notably, the data we rely on are self-reported and therefore subject to various caveats in interpretation (Boruchowicz et al., Reference Boruchowicz, Lopez Boo, Roseth and Tejerina2021). However, given that randomized experiments were increasingly challenging to implement during the pandemic, using self-report data can provide useful inputs to develop targeted communication and health campaigns for the unvaccinated or partially vaccinated in India that are specific to behavioural factors such as moral emotions, role models, and trust. Below, we outline the motivation and rationale for investigating the role of these three behavioural factors, identifying both, a research gap as well as a potential gap in health communication policy.
Moral emotions
COVID-19 behavioural research with Indian samples has also investigated the role played by moral emotions (Ticku et al., Reference Ticku, Puthillam and Kapoor2021) – emotions that are associated with broader societal concerns and whether/how individuals will uphold such moral standards (Haidt, Reference Haidt, Davidson, Scherer and Goldsmith2003; Tangney et al., Reference Tangney, Stuewig and Mashek2007). For instance, negative moral emotions (such as contempt towards others or shame towards oneself) for not adhering to PHBs like wearing a mask were associated with measures like social distancing. Sociomoral emotions such as these serve multiple functions, particularly in the context of large coordination problems such as curbing the spread of COVID-19. For instance, López-Pérez et al. (Reference López-Pérez, Hanoch and Gummerum2022) identified how individuals preferred to induce shame in COVID-19 rule violators to teach them a lesson; in other words, coronashaming was inflicted on transgressors of lockdown rules.
Trust
In general, lack of trust in government and public agencies, in the overall medical community and health system, and in information received about the vaccine can contribute to COVID-19 vaccine hesitancy (Danabal et al., Reference Danabal, Magesh, Saravanan and Gopichandran2021; Jain et al., Reference Jain, Saurabh, Kumar, Verma, Goel, Gupta, Bhardwaj and Raghav2021; Kanabar & Bhatt, Reference Kanabar and Bhatt2021; Kanozia & Arya, Reference Kanozia and Arya2021). Therefore, trust-building activities are crucial from a public health point of view. When it comes to childhood vaccination, such as MMR, review studies (e.g. Brown et al., Reference Brown, Kroll, Hudson, Ramsay, Green, Long, Vincent, Fraser and Sevdalis2010) indicated that parents who decline vaccines trust media and other sources of information more than information from hospitals, medical professionals, and the government, and also have lower perceived disease threat. There has also been ongoing work on vaccine hesitancy in more concentrated settings. Danabal et al. (Reference Danabal, Magesh, Saravanan and Gopichandran2021) used community surveys in urban and rural Tamil Nadu and found that vaccine hesitancy was at 40.7%. Importantly, they found that older, more educated individuals were more likely to trust COVID-19 vaccines, whereas younger people, women, and those residing in rural areas were more likely to favour natural immunity and/or mistrust the vaccine.
Role models
One method adopted to build trust in COVID-19 vaccines by government officials in India was to publicly receive immunization and advertise the same widely (Kanabar & Bhatt, Reference Kanabar and Bhatt2021). Such a role model effect can impact preventive behaviours such as increasing vaccination rates. Similarly, research has shown how vaccine uptake among healthcare workers can facilitate appropriate health behaviours among the general public (Biswas et al., Reference Biswas, Mustapha, Khubchandani and Price2021; Parente et al., Reference Parente, Ojo, Gurley, Le Master, Meyer, Wild and Mustafa2021). Additionally, Bansal et al. (Reference Bansal, Raj, Shukla and Sunder2021) found that having friends or family who were also vaccinated was strongly associated with vaccine preference. This indicates that role models need not be only public personalities, but also those in one's immediate social circle. To the best of the authors’ knowledge, an empirical investigation of such a role model effect in the context of COVID-19 vaccine uptake is yet to be undertaken.
PHBs and vaccine attitudes
Prior work suggests that PHBs, such as willingness to take the vaccine, not only vary by socio-cultural context (Al-Sanafi & Sallam, Reference Al-Sanafi and Sallam2021) but also by several behavioural (Tagat et al., Reference Tagat, Kapoor, Arora, Chakravarty, Mukherjee and Roy2022), informational, religious (Kanozia & Arya, Reference Kanozia and Arya2021) and emotional factors (Kapoor & Tagat, Reference Kapoor and Tagat2022). Earlier work on vaccine attitudes in India has focused largely on child vaccination, and a review of adult vaccinations (Dash et al., Reference Dash, Agrawal, Nagvekar, Lele, Di Pasquale, Kolhapure and Parikh2020) finds that low coverage is a concern when it comes to vaccine-preventable diseases. This is particularly the case among medical and paramedical students (i.e. doctors or healthcare workers in training). For example, work by Madhivanan et al. (Reference Madhivanan, Krupp, Yashodha, Marlow, Klausner and Reingold2009) used focus group discussions to show high acceptability of the human papillomavirus (HPV) vaccine among female medical students in the southern city of Mysore. Another study using students as participants found that having a background in biological sciences was associated positively with willingness to take a vaccine (Rashid et al., Reference Rashid, Labani and Das2016).
With specific reference to COVID-19, conspiratorial beliefs and political ideology are associated with COVID-19 risk perception among Indians (Puthillam & Kapoor, Reference Puthillam and Kapoor2021), which can thereby impact adherence to preventive behaviours, such as vaccination.
In addition, there have been various international studies that look at attitudes and perceptions towards COVID-19, focusing on disease threat, PHBs, and at-risk populations (van Bavel et al., Reference van Bavel, Cichocka, Capraro, Sjåstad, Nezlek, Pavlović, Alfano, Gelfand, Azevedo, Birtel, Cislak, Lockwood, Ross, Abts, Agadullina, Aruta, Besharati, Bor and Choma2022; e.g. Roy et al., Reference Roy, Tripathy, Kar, Sharma, Verma and Kaushal2020; Vacondio et al., Reference Vacondio, Priolo, Dickert and Bonini2021). Such studies focus on outcomes such as perceived disease threat and how it might affect future behaviours (particularly preventive behaviours; see, for example, Shook et al., Reference Shook, Sevi, Lee, Oosterhoff and Fitzgerald2020).
There is, however, extensive work on applications of various health behaviour models to understanding attitudes and perceptions towards vaccines in general. In a systematic review, Herzog et al. (Reference Herzog, Álvarez-Pasquin, Díaz, Del Barrio, Estrada and Gil2013) found that higher awareness among healthcare workers was associated with greater willingness to get vaccinated, whereas more concerns around side effects were associated with a lower willingness to take a vaccine.
Method
Participants
DataFootnote 2 were collected via multiple site-entry methods (Reips, Reference Reips2002) using an online survey (see Supplementary Appendix A for questionnaire). Participants could choose to take the survey in either Hindi or English; they were then given information about the nature of the survey, what they would be expected to do, risks, benefits and the confidential and voluntary nature of participation. After providing informed consent, they could begin the survey. A total of N = 1004 participated in the study between 28 May and 22 September 2021. A majority of the participants (N = 953) participated in the months of May and June 2021 and we restrict our sample to data collected during this period as there were large time gaps between participants and vaccination policy changes following June 2021. This includes the Union Government taking over COVID-19 vaccination drives across India, which was previously managed by individual State governments (Rao, Reference Rao2021). Vaccination was also made free of cost starting June 2021 (Menon, Reference Menon2021), which could have also influenced vaccination intentions. Of these, data for 770 participants were available on current vaccination status (the chief outcome variable), which forms the sample used for analysis. The study was approved by the Institutional Review Board at Monk Prayogshala (#058-021).
Measures
COVID-19-related information
Participants responded to a series of questions related to COVID-19-related preventive behaviours and outcomes. This included whether participants were ever infected by COVID-19, whether they were ever tested, and if they had received at least one dose of any COVID-19 vaccine. On an 11-point scale (0 = Does not apply at all to 10 = Applies very much), participants provided information on engagement in PHBs in the past month, including staying at home, avoiding social gatherings, maintaining physical distance with those outside of family, mask-wearing when outdoors, washing hands regularly, and wearing masks around strangers (Fetzer et al., Reference Fetzer, Witte, Hensel, Jachimowicz, Haushofer, Ivchenko, Caria, Reutskaja, Roth, Fiorin, Gómez, Kraft-Todd, Götz and Yoeli2020). Participants also responded to a similar scale (0 = not at all to 10 = completely) on preventive behaviours but in the context of having been vaccinated (for example, if you get vaccinated, how likely are you to … stay at home).
COVID-19 vaccine
Participants were also asked to rate on an 11-point scale how likely they were to take any COVID-19 vaccine (0 = not at all to 10 = extremely). This is our key (self-reported) measure of vaccine uptake intent, as we are unable to verify actual vaccination status among survey participants. Then, they provided information on how concerned they were about the serious side effects of vaccines as well as the ingredients in the vaccine, on an 11-point scale (0 = not at all concerned to 10 = extremely concerned).
Moral emotions
These questions are based on the Moral Foundations Theory (Graham et al., Reference Graham, Haidt, Koleva, Motyl, Iyer, Wojcik and Ditto2013) and the EAST framework for designing effective behaviour change strategies by the Behavioural Insights Team, UK (Lunn et al., Reference Lunn, Belton, Lavin, McGowan, Timmons and Robertson2020). Participants responded to a series of questions related to positive and negative moral emotions associated with taking the COVID-19 vaccine. On a scale of 0 = not at all to 10 = extremely, participants rated the extent to which they felt the following emotions regarding the COVID-19 vaccine. The negative moral emotions were contempt, anger, disgust, shame, embarrassment, and guilt. A sample item was ‘Contempt towards others who don't get vaccinated’. Positive moral emotions included gratitude, awe, compassion, and pride. A sample item was ‘Compassion towards others who get vaccinated’. Moral emotions were included based on preliminary findings indicating that they are reliable predictors of PHBs in the Indian context (see also Ticku et al., Reference Ticku, Puthillam and Kapoor2021). Separate composite measures were constructed using the positive and negative moral emotions statements, as a total of the individual items. Both measures displayed high internal consistency and reliability (αpositive = 0.91; αnegative = 0.93).
Trust
This comprised items along an 11-point scale (0 = don't trust at all to 10 = completely trust), asking how much participants trusted the following sources: family members, neighbours, people they knew personally, people they interact with on social media, scientists, the medical community (doctors, healthcare workers, nurses), hospitals, and politicians.
Role models
Participants also responded to the following yes/no question: ‘If/When X gets vaccinated, only then will I choose to get the vaccine (select all that apply)’, on a series of stakeholders (X) classified either as horizontal or hierarchical. Horizontal or immediate role models were those that were in the personal social network of the respondents (immediate family members, neighbours, friends of a similar age, relatives, or co-workers), whereas hierarchical role models were classified as those that were assigned some duties or roles by society and were perceived to wield power over decisions (family doctors, healthcare workers they know and trust, boss/work supervisor, the Prime Minister, or the Health Minister). The total number of role models required to convince participants to get vaccinated was computed, and two variables were derived, representing the ratio of horizontal and hierarchical role models to total role models, respectively.
Socio-demographic characteristics (Controls)
At the end of the survey, respondents provided details on a range of individual and household characteristics. These include their sex, age, educational qualification, occupation, religion, caste, and annual household income. All summary statistics are presented in Table 1, alongside a t-test for differences between the vaccinated (at least one dose) and unvaccinated sample. For the remainder of this manuscript, we refer to these groups as the vaccinated and unvaccinated samples.
Table 1. Summary statistics and t-test for differences by vaccination status
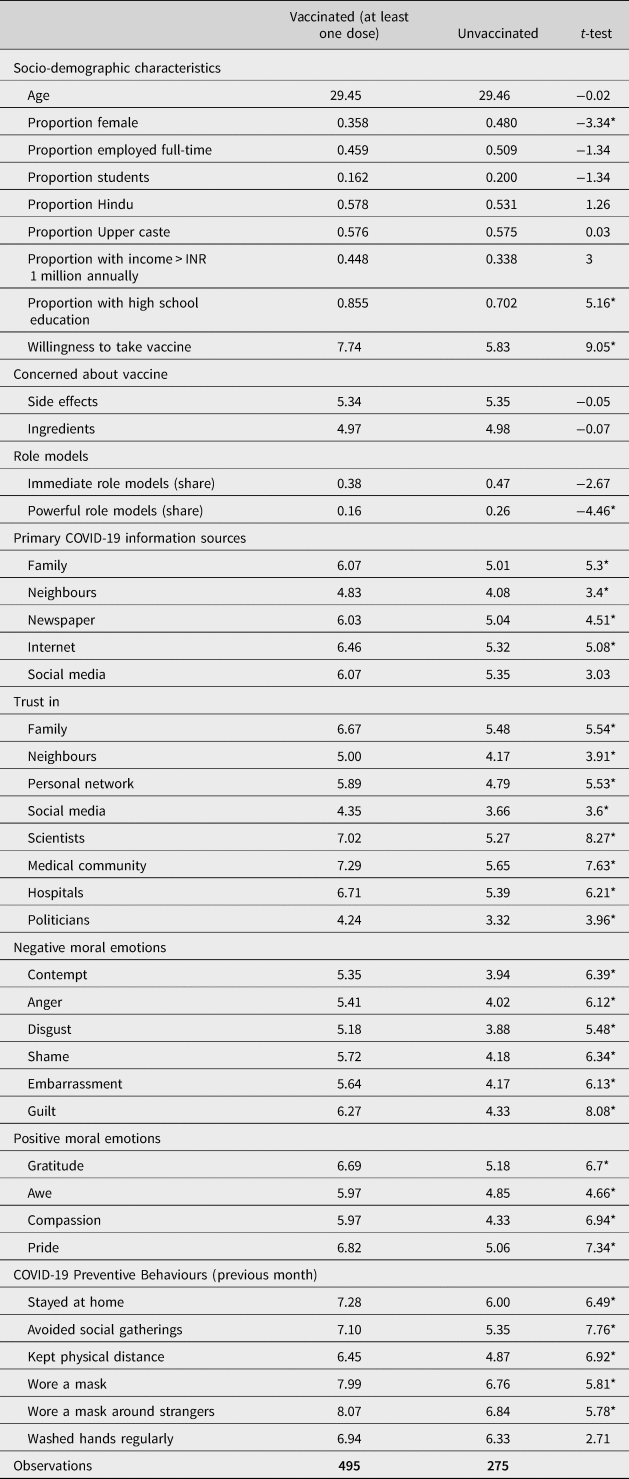
Note: *p < 0.001
Analysis
Three separate regressions were developed to empirically investigate the role of factors in RQs 1a, 1b and 1c, where the dependent variable was willingness to take the vaccine,Footnote 3 and the independent variables (IVs) in Model 1 were preventive behaviours; IVs in Model 2 were role models as well as trust in various stakeholders, and IVs in Model 3 were positive and negative moral emotions. These are presented in Equations (1)–(3).
where Vaccinei is a variable that takes a value of 0 to 10, with 0 indicating a complete unwillingness to get vaccinated and 10 indicating a complete willingness to get vaccinated. COVIDi is a vector of COVID-related variables specific to the ith individual, such as their infection and testing status, as well as the number of confirmed cases and vaccinated individuals in their city. Behsi is a vector of COVID-appropriate behaviours related to maintaining physical distance, wearing a mask, staying at home, avoiding social gatherings and handwashing. X i is a vector of individual-specific characteristics such as age, sex, occupation, educational qualification, income group, caste and religion. Trustik is a scale variable taking values 0 to 10, with 0 being do not trust at all to 10 being trust completely for the kth institution (family, neighbours, personal contacts, social media, scientists, medical community, hospitals and politicians). RoleModelsi are shares of immediate and powerful role models to total role models needed to take the vaccine. Finally, MoralEmoik captures measures of k moral emotions (contempt, anger, disgust, shame, embarrassment, guilt, gratitude, awe, compassion, and pride). Error terms are denoted by ηi, ${\rm \epsilon }_{ik}$![]() and δik. We first treat the dependent variable as a censored outcome variable (with the lower limit at 0 and the upper limit at 10) and run Equations (1)–(3) using a Tobit regression framework.
and δik. We first treat the dependent variable as a censored outcome variable (with the lower limit at 0 and the upper limit at 10) and run Equations (1)–(3) using a Tobit regression framework.
Each model was also run separately for the unvaccinated and full (partially or fully vaccinated and unvaccinated) samples. To address RQ2, additional regressions were run where the extent to which participants engaged in PHBs in the past month was the dependent variable. The key independent variable of interest was whether or not individuals had received at least one dose of any COVID-19 vaccine at the time of the survey. To check for robustness, regressions were also run using ordinary least squares in Stata 16.2, using robust standard errors and smoothed daily vaccinations and cases in India per million on the date the respondent participated in the survey. Results are presented in the form of coefficient plots of key explanatory variables and OLS regression results can be found in Supplementary Appendix Table B.1. The results of the censored regression are reported separately (Table 2).
Table 2. Tobit regression results
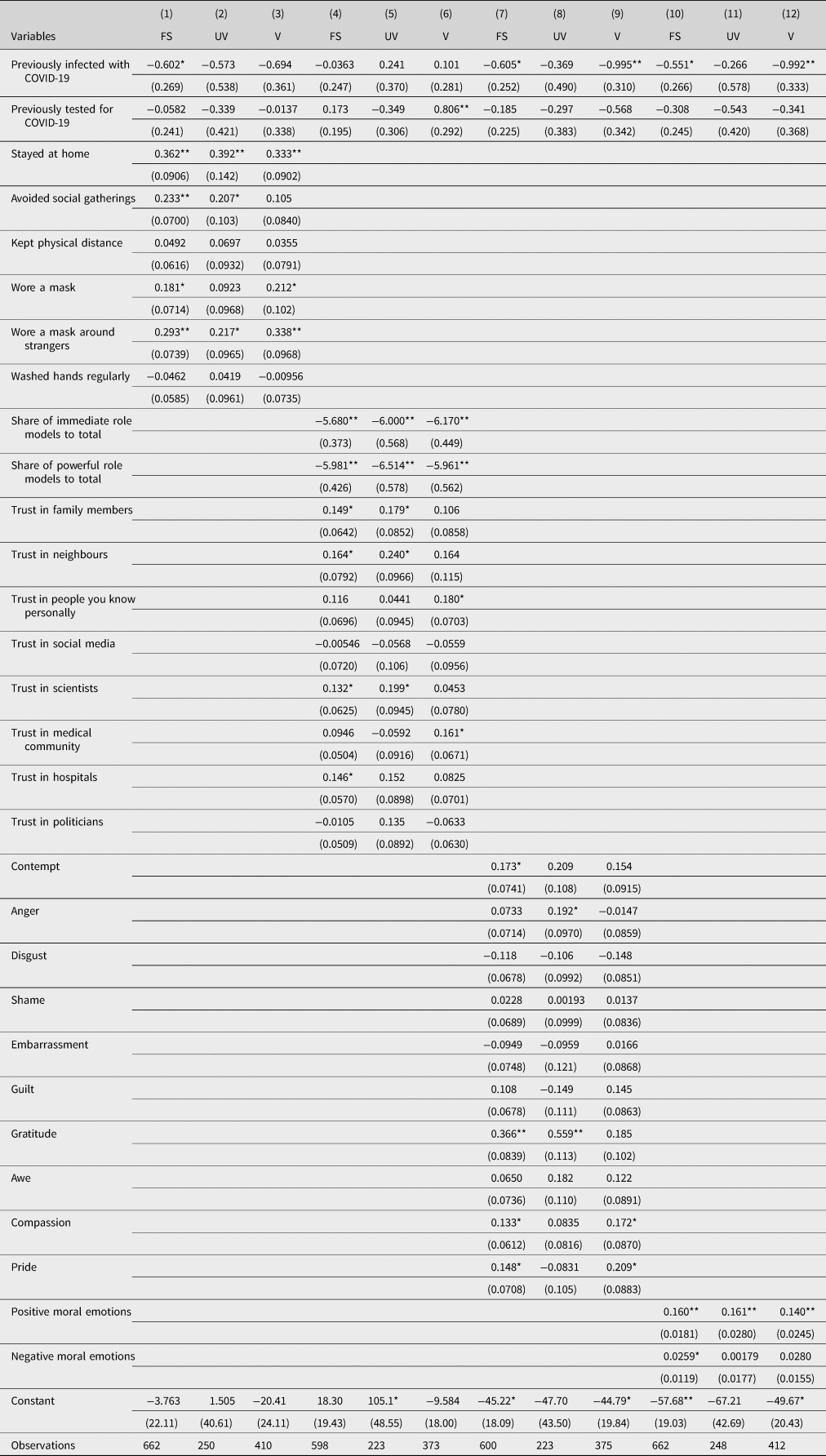
Note: Results reported are coefficients of censored (Tobit) regression (lower limit is 0 and upper limit is 10) of vaccine uptake on explanatory variables in Equations (1)–(3). FS, full sample; UV, unvaccinated sample only; V, vaccinated sample only. Additional controls included were age (in years), occupation, educational qualification, income group, caste group and religion. Additional controls for log of number of confirmed cases and vaccinations on day of survey response also included in all estimations. Robust standard errors in parentheses **p < 0.01, *p < 0.05.
Results
With respect to RQ 1a, engaging in PHBs (such as staying at home and wearing a mask around strangers) was broadly associated with greater willingness to take a vaccine, in the full (N = 662), unvaccinated (N = 250), and vaccinated samples (N = 410). Columns 1–3 in Table 2 report the results of the Tobit model. Past COVID-19 infection was significantly associated with a decline in intent to take the vaccine by 0.6 percentage points in the full sample. A unit increase in respondents staying at home (on the 11-point scale) was associated with a 0.36, 0.39, and 0.33 percentage point increase in the willingness to take the vaccine among the full, unvaccinated, and vaccinated samples, respectively. Wearing a mask when interacting with strangers was also positively associated with willingness to take the vaccine, with a unit increase in the scale corresponding to 0.29, 0.22, and 0.34 percentage point increase in willingness to take the vaccine among the full, unvaccinated, and vaccinated samples, respectively. Avoiding social gatherings was also associated with greater vaccine uptake intent in the full and unvaccinated samples. The results from the OLS model are similar and are presented in the coefficient plot in Figure 1 and results are reported in Columns 1–3 in Supplementary Appendix Table B.1. Except for avoiding social gatherings, staying at home and mask-wearing around strangers are statistically significant for both the vaccinated and unvaccinated sample.

Figure 1. Preventive health behaviours and vaccine uptake.
Note: Plot depicts point estimates of coefficients and 95% confidence intervals from three ordinary least squares regressions of vaccine uptake on preventive behaviours, moral emotions, trust and other factors. All regression specifications contain additional covariates on age (in years), sex, occupation, educational qualification, income group, caste grouping, religion, whether previously infected, whether previously tested, natural log of daily vaccinations per million persons and natural log of new cases per million persons on the day of survey response. Corresponding regression results can be found in Supplementary Appendix Table B.1 (Columns 1–3).
Figure 2 contains the results of the OLS regression of vaccine uptake intent on role models and trust (RQ1b), while Columns 4–6 in Table 2 report the results for the Tobit model. In general, reliance on role models (or requiring others to have taken the vaccine in order for respondents to get vaccinated) was negatively associated with willingness to take the vaccine. In the unvaccinated sample, an increase in the fraction of immediate role models to all role models was associated with a 6-point decrease in the willingness to get vaccinated (p < 0.01), whereas the corresponding coefficient for hierarchical role models was slightly larger at 6.51 (p < 0.01). These coefficients are similarly significant in the full and vaccinated samples. It is also possible that the trust and role model variables may be overlapping in their capture of factors associated with willingness to take the vaccine. To be sure, we also conducted pairwise correlation tests and found that the share of immediate role models to total and share of powerful role models to total are not statistically significantly correlated with trust in neighbours and social media. However, they were weakly (r < 0.4) correlated with all other trust variables. Thus, the role models variable may capture only part of what is being captured by the trust variables.

Figure 2. Role models, trust and vaccine uptake.
Note: Plot depicts point estimates of coefficients and 95% confidence intervals from three ordinary least squares regressions of vaccine uptake on preventive behaviours, moral emotions, trust and other factors. All regression specifications contain additional covariates on age (in years), sex, occupation, educational qualification, income group, caste grouping, religion, whether previously infected, whether previously tested, natural log of daily vaccinations per million persons and natural log of new cases per million persons on the day of survey response. Corresponding regression results can be found in Supplementary Appendix Table B.1 (Columns 4–6).
In terms of interpersonal trust, the results find that trust in family members, neighbours, scientists and hospitals in the full sample was associated with a greater willingness to take the vaccine. This appears to be driven by the unvaccinated sample, with the exception of trust in hospitals (which was not statistically significant in the unvaccinated sample). The Tobit estimates indicate trust in the medical community and personal acquaintances are positively associated with vaccine uptake intent in the vaccinated sample (Table 2). There are no statistically significant associations between the trust variables and vaccine uptake intent in the vaccinated sample alone in the OLS estimates.
Finally, Columns 7–9 in Table 2 present the Tobit results and Figure 3 presents the OLS estimates for moral emotions and vaccine uptake intent (RQ1c). Positive moral emotions were strongly associated with increase in willingness to take the vaccine in all samples, in both the OLS and Tobit models. A large part of this is driven by gratitude towards those who have been vaccinated (B full = 0.28, B unvaccinated = 0.48; both p < 0.01). There are smaller positive coefficients for compassion towards others who have been vaccinated (B full = 0.09, B vaccinated = 0.15, p < 0.05) and pride associated with getting vaccinated (B full = 0.11, p < 0.05). Table 2 coefficients suggest that the association of compassion and pride is driven by the vaccinated sample, whereas the result on gratitude is driven by the unvaccinated sample. In terms of the composite variable of positive moral emotions, a unit increase in the score was associated with a 0.12, 0.13 and 0.08 unit increase in the willingness to get vaccinated in the full, unvaccinated and vaccinated samples. In the Tobit model, in terms of moral emotions, contempt towards those who did not take the vaccine is no longer statistically significant in the unvaccinated sample, instead, anger towards those who did not take the vaccine is now positively associated with willingness to take the vaccine (B unvaccinated = 0.192, p < 0.05). The composite variable for negative moral emotions were also significantly associated with greater willingness to take the vaccine (B full = 0.022, B vaccinated = 0.02, p < 0.01), but not in the unvaccinated sample. However, in the full sample (as well as the unvaccinated sample in the OLS results), greater contempt towards those not vaccinated was positively associated with vaccine uptake intent (B full = 0.12, B unvaccinated = 0.193, p < 0.05). No other statistically significant results were obtained for negative moral emotions.

Figure 3. Moral emotions and vaccine uptake.
Note: Plot depicts point estimates of coefficients and 95% confidence intervals from three ordinary least squares regressions of vaccine uptake on preventive behaviours, moral emotions, trust and other factors. All regression specifications contain additional covariates on age (in years), sex, occupation, educational qualification, income group, caste grouping, religion, whether previously infected, whether previously tested, natural log of daily vaccinations per million persons and natural log of new cases per million persons on the day of survey response. Corresponding regression results can be found in Supplementary Appendix Table B.1 (Columns 7–9).
In terms of RQ2, the results suggest that not being vaccinated is negatively associated with engaging in PHBs. Figure 4 presents the coefficient plots, separately for each preventive behaviour. Except for regular handwashing, not being vaccinated (relative to those vaccinated with at least one dose) has a negative coefficient on all PHBs. The largest negative coefficient was observed for avoiding social gatherings (B = −1.29, p < 0.01), followed by the coefficient for maintaining physical distance (B = −1.21, p < 0.01). There are similar negative associations between not being vaccinated and staying at home (B = −0.89, p < 0.01), mask-wearing when outdoors (B = −0.79, p < 0.01) and wearing a mask when interacting with strangers (B = −0.8, p < 0.01). In each model, having been previously infected with COVID-19 was also negatively associated with engaging in preventive behaviours recently (B woremask = −0.78; B maskstranger = −0.78, both p < 0.01; B washedhands = −0.71, p < 0.05). In contrast, having been tested for COVID-19 infection was positively associated with engaging in these same preventive behaviours (B woremask = 0.56; B maskstranger = 0.61, both p < 0.01), and to a lesser extent, frequent handwashing (B = 0.51, p < 0.05).

Figure 4. Vaccination status and preventive health behaviours.
Note: Plot depicts point estimates of coefficients and 95% confidence intervals from six ordinary least squares regressions of preventive behaviours on vaccination status. Each regression specification contains additional covariates on age (in years), sex, occupation, educational qualification, income group, caste grouping, religion, whether previously infected, whether previously tested, natural log of daily vaccinations per million persons and natural log of new cases per million persons on the day of survey response.
In supplementary analysis (Supplementary Appendix C), the full sample analysis was run separately for males and females to identify if there were any gender differences.Footnote 4 For RQs 1a, 1b and 1c, the positive association between two preventive behaviours (avoiding social gatherings and mask-wearing) was statistically significant only in the male sample (B avoidsocgathering = 0.211, p < 0.01; B mask = 0.162, p < 0.05), whereas other behaviours were consistent with full sample results reported above. Furthermore, the results on trust were also driven by the male sample, with trust in family members positive and significant for men but not women. Note that there were no major differences in significance in terms of the hierarchical and horizontal role models between men and women.Footnote 5 Interestingly, the positive association between trust in scientists and the medical community in the full sample was stronger among women in our sample, as the coefficients were not statistically significant for men (although the results for trust in hospitals was driven by men). The gender-disaggregated results on moral emotions and their associations with vaccine uptake intent suggest that the positive emotions (compassion and pride), as well as the negative emotion of disgust, were significantly associated with vaccine uptake intent but only for men in the full sample. Indeed, the result on combined moral emotions indicates that the significant association between negative moral emotions and vaccine uptake intent in the full sample is driven by men. For RQ2, there appears to be minor differences in coefficients between men and women, with the exception of previous COVID-19 infection being associated with men less likely to stay at home and women more likely to stay at home. The remainder of the results consistent with the full sample appear to be stronger in the male sample than in the female sample.
Discussion
The purpose of the present study is to examine the determinants of willingness to get vaccinated in India, as well as to examine changes in PHBs as a function of vaccination status. Results indicate that past PHBs like staying at home, mask-wearing around strangers and moral emotions are robustly associated with the willingness to take a COVID-19 vaccine, in both vaccinated (at least one dose) and unvaccinated samples. Results also show that those who were not vaccinated are less likely to adhere to other PHBs, such as wearing a mask; COVID-19 infection status is associated with similar lower adherence to PHBs but having been tested is related to more frequent engagement in behaviours like handwashing.
Getting vaccinated is the epitome of engaging in preventive health behaviour against COVID-19. Thus, individuals who received at least one dose, as well as those who were unvaccinated, are more willing to take a COVID-19 vaccine if they had also stayed at home and worn masks when interacting with strangers in the past month. Past research has similarly found grouping of engagement in PHBs, including willingness to protect oneself and others by taking a COVID-19 vaccine (Latkin et al., Reference Latkin, Dayton, Yi, Colon and Kong2021). Notably, among those who were vaccinated (at least one dose), avoiding social gatherings is not significantly associated with vaccine uptake intent, suggesting some substitution among PHBs but not others (as mask-wearing was significantly associated with vaccine uptake intent). This is similar to earlier work that links vaccination choices with mask-wearing in the Indian context (Tagat et al., Reference Tagat, Kapoor, Arora, Chakravarty, Mukherjee and Roy2022).
This is one of the first studies to examine the impact of role models on vaccine uptake intent. Given that vaccination against COVID-19 is a global public health concern, and that role models have been shown to increase vaccine coverage (Vet et al., Reference Vet, de Wit and Das2011), this was an important variable in the current study. Findings indicate that the more participants relied on role models to have taken the vaccine, the less willing they were to get vaccinated themselves; this is true for both horizontal (e.g. co-workers) and hierarchical (e.g. doctors) role models. It is also true in both vaccinated (at least one dose) and unvaccinated samples. In other words, vaccine-hesitant individuals need more social proof that others have been vaccinated for them to be willing to get vaccinated themselves. This can be juxtaposed with recent work that shows greater vaccine hesitancy among supporters of former American President, Donald Trump, given his anti-vaccine stance (Hornsey et al., Reference Hornsey, Finlayson, Chatwood and Begeny2020). Highlighting the numbers of frontline workers and public health officials along with social norm metrics of local vaccinated populations may be an effective communication strategy to persuade those who are on the fence about getting vaccinated (Santos et al., Reference Santos, Goren, Chabris and Meyer2021). Similarly, OLS results indicate that interpersonal trust in neighbours matters the most for the willingness to get vaccinated among those who had not yet been vaccinated. Results from the Tobit specification suggest that the results on trust in neighbours and family contributing positively to vaccine uptake intent are driven by the unvaccinated sample. On the other hand, trust in hierarchical institutions like hospitals and scientists contribute to a higher willingness to get vaccinated; however, this result holds only in the full sample, indicating that public health messaging from these channels may not enhance uptake intent among any particular group. Both sets of results on role models and trust indicate the necessity of focusing on hyperlocal communities and norms when framing effective health messaging for vaccine uptake in India, which has been suggested elsewhere (Wrigley-Field et al., Reference Wrigley-Field, Kiang, Riley, Barbieri, Chen, Duchowny, Matthay, Van Riper, Jegathesan, Bibbins-Domingo and Leider2021).
Furthermore, moral emotions, both positive and negative, are robust predictors of the willingness to get vaccinated (see also Ticku et al., Reference Ticku, Puthillam and Kapoor2021). Within the broader social context, moral emotions related to vaccine uptake establish a moral norm that is expected to be followed by oneself and imposed on others. In the event that others do not adhere to this norm, moral emotions aid in sanctioning transgressions, thereby establishing the normative behaviour of getting vaccinated. High gratitude (in the unvaccinated sample) and compassion towards others (in the vaccinated sample), but high contempt towards others (in the unvaccinated sample) who did not get vaccinated predict vaccine uptake intent. These findings can be applied in health communication campaigns to establish sociomoral norms, especially highlighting how others may view one who chooses/does not choose to get vaccinated (with gratitude or contempt).
Moreover, PHBs are found to be an interesting behavioural marker that differentiated those who were infected, tested, or unvaccinated. This is in line with Kreps et al. (Reference Kreps, Goldfarb, Brownstein and Kriner2021), who used a sample from the United States and found that vaccinated individuals were more likely to support continued mask-wearing post-vaccination. Those not yet vaccinated are also less likely to engage in several preventive behaviours, thereby providing further evidence for clustering of vaccine uptake intent with engaging or not engaging in behaviours that could protect against COVID-19. Although the analysis does not control for the date of vaccination, being vaccinated at the time of the survey is associated with greater willingness to take part in PHBs such as mask-wearing and social distancing. This is seemingly at odds with any risk-compensating behaviour suggested in the medical literature (e.g. Trogen & Caplan, Reference Trogen and Caplan2021). Being tested is associated with greater tendencies to engage in PHBs, both being markers of increased threat perception translating into behaviour. This is in contrast with findings from Thunström et al. (Reference Thunström, Ashworth, Shogren, Newbold and Finnoff2021), who suggest a negative relationship between maintaining social distancing and testing in the United States. However, it is unclear the specific time period at which this data were collected and may predate widespread testing facilities and vaccination availability. Last, having been infected with COVID-19 was associated with lower likelihood of partaking in preventive behaviours, a marker of lower disease threat perception.
In sum, the current study examines behavioural factors associated with COVID-19 vaccine uptake intent in India, where only 67% of the population is fully vaccinated. In the subsample yet to be vaccinated, engagement in preventive behaviours such as mask-wearing and avoiding social gatherings is positively associated with greater vaccine uptake intent. Requiring more immediate role models to be vaccinated is associated with a lower willingness to take the vaccine, but positive moral emotions such as gratitude towards those who are vaccinated are strongly associated with greater vaccine uptake intent. These results point towards potential health communication strategies for boosting vaccine uptake in the Indian context. For example, governments could use social proof of thanking those who have been fully vaccinated in targeted campaigns aimed at districts or jurisdictions where vaccine uptake remains low. In other contexts, Krpan et al. (Reference Krpan, Makki, Saleh, Brink and Klauznicer2021) point out how responses to providing information could be heterogeneous along lines of prevalence of existing PHBs. Although data on vaccination rates are publicly available, leveraging these to inform well-designed behavioural interventions is key to driving down vaccine hesitancy and achieving universal adult vaccination against COVID-19 in India.
Author contribution
The authors are grateful to Shekar Menon, Priya Nanda, and Siddharta Swarup for inputs during survey design. The authors also thank CORE Net India Network for assistance with survey dissemination. We are grateful to the editor, Adam Oliver, and two anonymous referees for many helpful comments.
Competing interest
The authors declare that there are no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/bpp.2023.12.








