Preterm birth is defined as delivery before 37 weeks of gestation. It is a leading cause of perinatal mortality and morbidity and is associated with a higher risk of metabolic, neurological and CVD in adulthood(Reference Luu, Rehman Mian and Nuyt1,Reference Bavineni, Wassenaar and Agnihotri2,Reference Prior and Modi3) . Preterm birth is the second largest cause of child deaths under 5 years, with an estimated incidence of 11·1 % worldwide and 7·1 % in China in the year 2020(Reference Blencowe, Cousens and Oestergaard4). Several literature reviews have identified a series of risk factors for preterm birth, including older maternal age, a history of preterm birth, maternal chronic infection, short cervix, short interpregnancy interval, multiple pregnancy, smoking, working more than 40 h/week, heavy lifting during pregnancy and maternal malnutrition(Reference Berger, Rath and Abele5,Reference Newburn-Cook and Onyskiw6,Reference Sanchez, Kupp and Sheridan7,Reference Torchin and Ancel8,Reference Stewart and Graham9,Reference Bloomfield10,Reference Triunfo and Lanzone11) . In fact, maternal nutritional imbalance may be a key factor in preterm birth(Reference Triunfo and Lanzone11). Recent studies have found that, during pregnancy, increased intake of fish and shellfish and the elongated n-3 PUFA contained therein may promote longer gestation and prevent preterm birth(Reference Olsen and Secher12).
Fish and shellfish are important sources of essential nutrients, including protein, Se, iodine, vitamin D and long-chain PUFA. Fish and shellfish contain a large amount of n-3 PUFA, which is classified as an essential fatty acid and is essential for the development of membranes and new tissues. Moreover, n-3 PUFA only comes from the maternal diet(Reference Olsen and Secher12,Reference Hosomi, Yoshida and Fukunaga13,Reference Allen and Harris14) . Several prospective cohort studies have consistently shown the protective roles of fish and shellfish consumption in preventing preterm birth, with women who had higher fish and shellfish consumption showing decreased risk of preterm birth(Reference Olsen and Secher12,Reference Olsen, Osterdal and Salvig15,Reference Haugen, Meltzer and Brantsaeter16,Reference Leventakou, Roumeliotaki and Martinez17,Reference Brantsaeter, Englund-Ogge and Haugen18,Reference Klebanoff, Harper and Lai19) . The dietary guidelines for pregnant women by the Chinese Society of Nutrition recommend that seafood should be consumed 350–525 g/week during the second and third trimester of pregnancy(20). However, the extent to which fish and shellfish consumption plays a role in shaping pregnancy outcomes is unclear, as evidence regarding maternal consumption and birth outcomes is inconclusive. Some clinical trials and studies found that fish and shellfish consumption was not associated with preterm birth(Reference Guldner, Monfort and Rouget21,Reference Oken, Kleinman and Olsen22,Reference Heppe, Steegers and Timmermans23,Reference Benjamin, Mitchell and Canfield24,Reference Nykjaer, Higgs and Greenwood25) , while others suggested that fish and shellfish consumption reduced the risk of preterm birth(Reference Mohanty, Siscovick and Williams26).
Most of these studies were conducted in coastal countries such as Denmark(Reference Olsen and Secher12,Reference Olsen, Osterdal and Salvig15) , Norway(Reference Haugen, Meltzer and Brantsaeter16,Reference Brantsaeter, Englund-Ogge and Haugen18) , France(Reference Guldner, Monfort and Rouget21) and other European countries(Reference Leventakou, Roumeliotaki and Martinez17) or coastal states such as Massachusetts in the USA(Reference Oken, Kleinman and Olsen22), where people consumed a large amount of fish. On the contrary, Lanzhou is an inland city where people consumed relatively less fish(Reference Needham and Funge-Smith27). Results from Western coastal areas may not be generalised to the Chinese inland urban population as a whole. In light of the inconsistent results on the association between fish and shellfish consumption and preterm birth, as well as different fish and maternal habits in fish consumption, it is both important and urgent to assess fish and shellfish consumption during pregnancy and its impact on preterm birth in a Chinese population.
The aim of this study was to determine how the consumption of fish and shellfish during pregnancy affected the risk of preterm birth. We hypothesised that higher intake of fish and shellfish was associated with lower risk of preterm birth. We also classified preterm birth into moderately preterm and very preterm in addition to spontaneous and medically indicated preterm birth and explored their associations with fish and shellfish intake.
Methods
Population and study design
The retrospective study was conducted during 2010–2012 in the Gansu Provincial Maternity and Child Care Hospital, the largest maternity and childcare hospital in Lanzhou, China(Reference Qiu, He and Cui28). The target population was pregnant women who came to the hospital for delivery, aged 18 years or older, with no history of mental illness and with gestational ages ≥ 20 completed weeks. Among the 14 535 pregnant women who came to the hospital for delivery, 176 were excluded because of being younger than 18 years, or with mental illness, or with gestational weeks of <20, leading to 14 359 eligible women approached for study participation. Among those 14 359 women approached, 3712 refused to participate and 105 did not complete in-person interviews, leading to a total of 10 542 pregnant women (73·4 %) who completed the questionnaire. After exclusion of multiple births and still births, 10 179 women having singleton live birth were included in the study (Fig. 1).
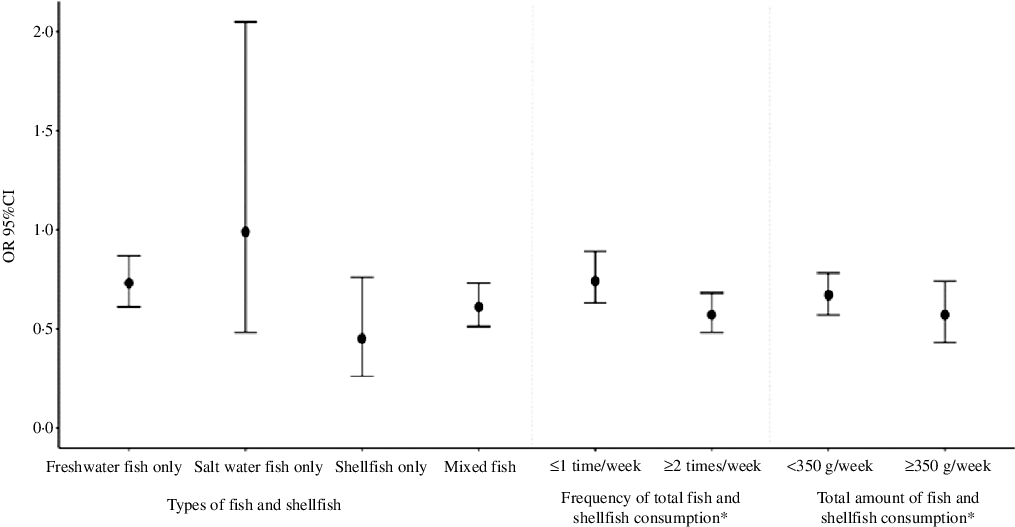
Fig. 1. Associations between fish and shellfish consumption and risk of preterm birth.
All study procedures were approved by the human investigation committees at the Gansu Provincial Maternity and Child Care Hospital. Eligible women were informed of study procedure upon their arrival at the hospital for delivery. After obtaining written consent, trained study interviewers conducted in-person interviews at the hospital using a standardised and structured questionnaire. All questionnaires were interviewer-administered. The majority of women (84 %) were interviewed within 1 to 3 d after delivery. Eligible women were interviewed using a standardised and structured questionnaire to collect information on demographic, environmental and lifestyle factors. On the other hand, information on birth outcomes and maternal complications was extracted from medical records.
Dietary assessment
An FFQ was administered at enrollment to inquire about participants’ dietary habits since the start of pregnancy and the prevalence of various food consumption including fish and shellfish. Fish and shellfish consumption was assessed by three items, ‘salt-water fish (hairtail, etc.)’, ‘fresh-water fish (carp, etc.)’ and ‘shellfish (shrimp, crabs, mussels, etc.)’. Intake of any amount of fish and shellfish is defined as fish and shellfish consumption. For each fish and shellfish item, participants were asked about both the frequency and the amount (g) of each item. The frequency item asked whether participants eat fish and shellfish consumption on a daily basis, weekly basis or monthly basis and further asked how many times they eat based on their choice of daily, weekly or monthly consumption (‘never’, ‘how many times per day’, ‘how many times per week’ and ‘how many times per month’). The frequency was further categorised into three frequency groups: never, ≤ 1 time/week and ≥ 2 times/week. A total fish and shellfish amount was calculated by multiplying the frequency and amount of each item. Based on the recommendations of Chinese Nutrition Society(20), the total fish and shellfish amount was further classified into three categories: never, < 350 g/week and ≥ 350 g/week. Details of fish and shellfish consumption assessment items on the FFQ were shown in Supplementary File S1.
Preterm birth
Preterm birth was defined as delivery before 37 completed weeks of gestation. Preterm birth was further categorised into late preterm (34–< 37 weeks), moderately preterm (32–< 34 weeks), very preterm (28–< 32 weeks) and extremely preterm (< 28 weeks) based on the gestational age at delivery, which was calculated from the first day of the last menstrual period(29). To improve statistical efficiency, we combined late preterm and moderately preterm into moderate preterm group and very preterm and extremely preterm into very preterm group. In addition, preterm birth was categorised based on clinical presentations: spontaneous preterm birth and medically indicated preterm birth. Spontaneous preterm birth refers to spontaneous onset of labour or labour following preterm premature rupture of membranes. Medically indicated preterm birth refers to delivery induced for medical reasons, such as pre-eclampsia, intrauterine growth restriction or fetal distress(Reference Ananth and Vintzileos30,31) .
Other variables
Maternal height and pre-pregnancy weight were used to compute maternal BMI (kg/m2) before pregnancy, which was categorised as underweight (BMI < 18·5 kg/m2), normal weight (18·5 kg/m2 ≤ BMI < 24 kg/m2) and overweight and obesity (BMI ≥ 24 kg/m2) using the standard of Working Group on Obesity in China(Reference Zhou32). Women with underweight, overweight and obesity were all grouped into abnormal BMI group. The list of covariates for the multivariate models included maternal age (<25, 25–29, 30–34 and ≥ 35 years), education level (< 9, 10–15 and ≥ 16 years), monthly income (RMB < 2000, 2000–4000 and > 4000 yuan), parity (nulliparous or parous), gestational diabetes (yes or no), gestational hypertension (yes or no), adequate physical activities during pregnancy (physical activities no <30 min at ≥ 3 times/week), passive smoking during pregnancy (yes or no), multi-vitamin and protein supplement intake during pregnancy (yes or no, collected from the FFQ) and total energy intake (continuous variable).
Statistical analysis
Statistical significance was assessed with the χ 2 tests for all categorical variables. Unconditional logistic regression models were used to estimate OR and 95 % CI for the associations of fish and shellfish consumption with preterm birth and its clinical subtypes. Specifically, we used the category of ‘Never (no fish and shellfish consumption)’ as the reference for all analyses. In addition, we adjusted for joint confounding by including the variables (see covariate list) as explanatory variables simultaneously in the models. P for trend was obtained by incorporating the categorical variables as linear terms in the models. All P values were two-sided and defined to be significant at P < 0·05. All statistical analyses were performed with IBM SPSS Statistics for Macintosh (Version 25.0, IBM Corp.).
Results
Descriptive statistics
Consumption of any fish and shellfish was reported by 82·9 % (n 8441) of women, while 17·1 % (n 1738) of women reported no fish and shellfish intake in our study. The median energy intake calculated by the FFQ was 1613·94 kcal, with the 25th and 75th percentile being 1347 kcal and 1906 kcal, respectively. The overall proportion of preterm birth in the study population was 10·01 % (n 1019), comprising 81·8 % (n 833) of moderate preterm births and 18·2 % (n 186) of very preterm births. Of all preterm deliveries, 33·2 % (n 338) were medically indicated preterm births and 66·8% (n 681) were spontaneous preterm births.
Maternal socio-demographic characteristics differed in fish and shellfish consumption. As shown in Table 1, women who never consumed fish and shellfish during pregnancy were more likely to be younger than 25 years (n 419), with education years ≤ 9 (n 702) and household income of < 2000 yuan (n 651) compared with women who ever consumed fish and shellfish. Table 1 also shows the distributions of selected characteristics in women with preterm and full-term deliveries. Maternal age younger than 25 years or older than 35 years, lower education, lower income, multipara, passive smoking, gestational diabetes and hypertension during pregnancy were associated with increased risk of preterm birth.
Table 1. Description of study population by fish and shellfish consumption and by preterm birth
(Numbers and percentages)
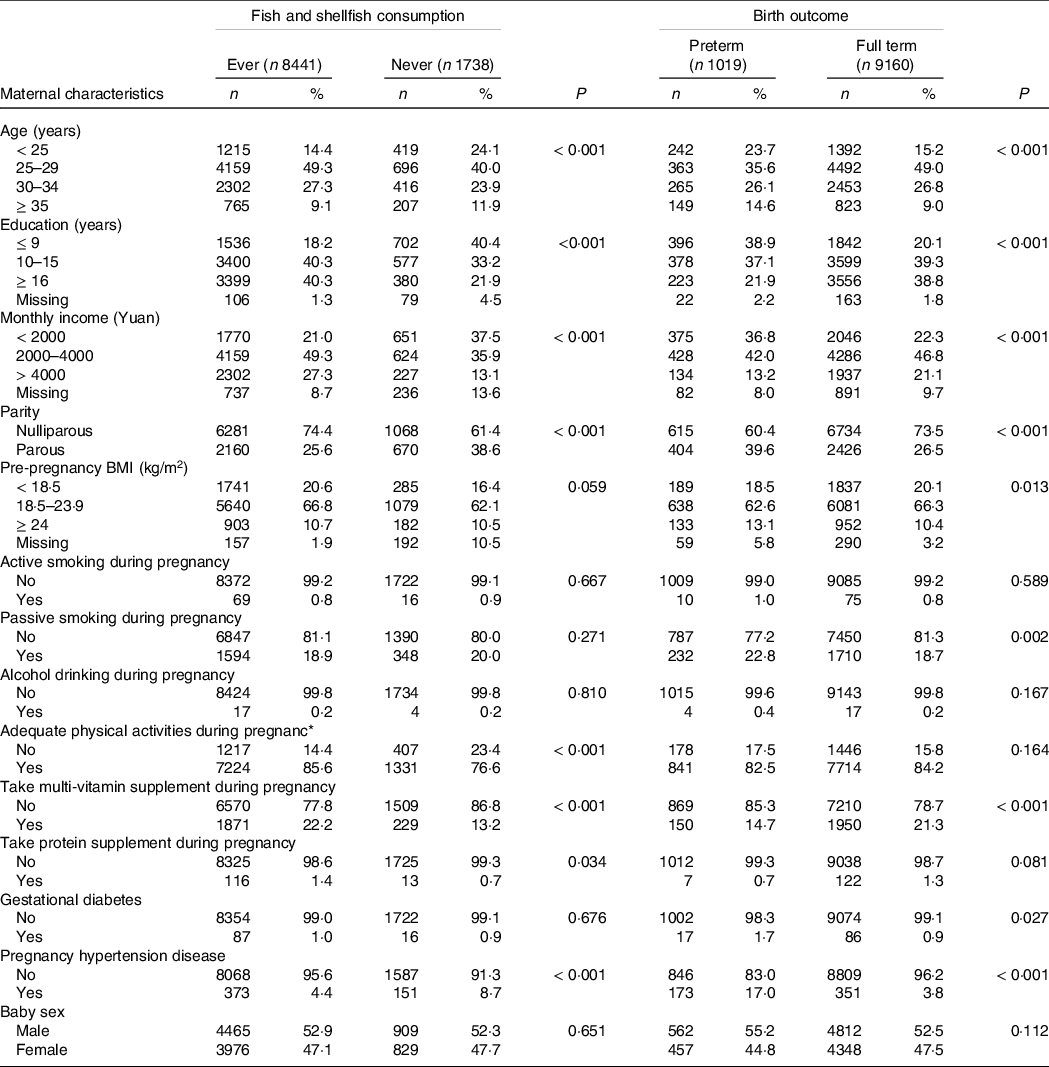
* Adequate physical activities refer to physical activities no < 30 min at ≥ 3 times/week.
Fish and shellfish consumption (total and by type)
Fish and shellfish consumption was associated with decreased risk of preterm birth (OR = 0·65, 95 % CI 0·56, 0·77, Table 2 & Fig. 1). When we examined fish and shellfish consumption by types, significant associations were remained for freshwater fish intake (OR = 0·73, 95 % CI 0·61, 0·87), shellfish intake (OR = 0·45, 95 % CI 0·26, 0·76), as well as any two or three kinds of fish intake (OR = 0·61, 95 % CI 0·51, 0·73), but not for saltwater fish. After stratification by subtypes, similar associations were found for subtypes of preterm birth, when fish and shellfish types were examined (shown in Table 3).
Table 2. Associations between fish and shellfish consumption and risk of preterm birth
(Numbers and percentages; odd ratio and 95 % confidence intervals)
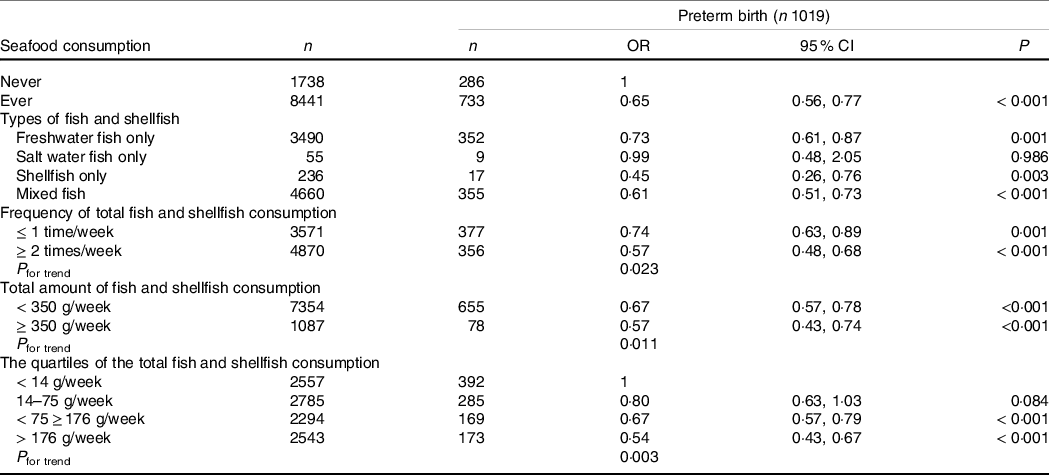
Adjusted for maternal age, educational level, monthly family income, parity, hypertensive disorder during pregnancy, gestational diabetes, pre-pregnancy BMI, smoking (active and passive smoking) during pregnancy, physical activities during pregnancy, multi-vitamin and protein supplement intake during pregnancy and total energy intake.
Table 3. Associations between fish and shellfish consumption and preterm birth by length of gestation and cause
(Numbers and percentages; odd ratio and 95 % confidence intervals)
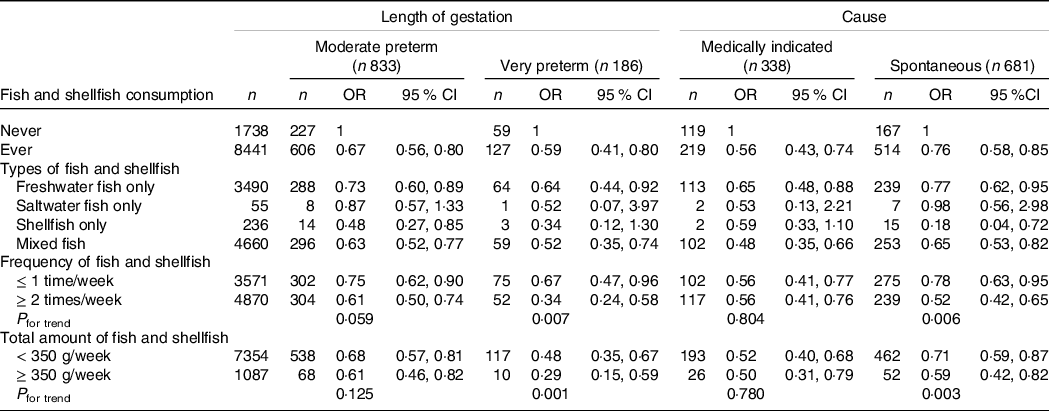
Adjusted for maternal age, educational level, monthly family income, parity, hypertensive disorder during pregnancy, gestational diabetes, pre-pregnancy BMI, smoking (active and passive smoking) during pregnancy, physical activities during pregnancy, multi-vitamin and protein supplement intake during pregnancy and total energy intake.
Frequency of fish and shellfish consumption
For fish and shellfish consumption frequency, we observed a decrease in the risk of preterm birth with increasing frequency of fish and shellfish intake. Increasing frequency of fish and shellfish consumption, compared with no fish and shellfish consumption, was associated with decreasing odds of preterm birth: for ≤ 1 time/week, OR = 0·74 (95 % CI 0·63, 0·89); for ≥ 2 times a week, OR = 0·57 (95 % CI 0·48, 0·68). The P for trend was 0·023 (Table 2 & Fig. 1). Similar trend patterns were also observed for very preterm birth (P for trend = 0·007, Table 3) and spontaneous preterm birth (P for trend = 0·006, Table 3).
Weekly amount of total fish and shellfish consumption
We also examined the weekly amount of total fish and shellfish consumption, as shown in Table 2 and Fig. 1. Only 1087 out of 10 179 (10·7 %) women consumed a total amount of fish and shellfish above the recommended 350 g/week by the Chinese Nutrition Society, which is a very low rate. Increasing weekly total amount of fish and shellfish consumption, compared with no fish and shellfish consumption, was also associated with decreasing odds of preterm birth: for < 350 g/week, OR = 0·67 (95 % CI 0·57, 0·78); for ≥ 350 g/week, OR = 0·57 (95 % CI 0·43, 0·74). The P for trend was 0·011. Significant trend effect was also seen between weekly total amount of fish and shellfish consumption and very preterm birth (P for trend = 0·001) and spontaneous preterm birth (P for trend = 0·003).
Considering only a small portion of pregnant women consumed over 350 g/week of fish and shellfish, we further categorised fish and shellfish consumption based on quartiles and did a similar analysis. As shown in Table 2, compared with the <14 g/week fish and shellfish consumption, only the 75–176 g/week (OR: 0·67, 95 % CI 0·57, 0·79) and the ≥ 176 g/week (OR: 0·54, 95 % CI 0·43, 0·67) consumption groups were associated with decreasing odds of preterm birth, while the 14–75 g/week consumption group showed no significant difference.
Fish and shellfish consumption and preterm birth by maternal age and BMI
We further analysed whether maternal age, pre-pregnancy BMI underweight and pre-pregnancy BMI overweight were effective modifiers of fish and shellfish consumption using interaction analysis through logistic regression (Table 4). Interaction was observed between total fish and shellfish consumption with maternal age (P for interaction = 0·041) and pre-pregnancy BMI underweight (P for interaction = 0·012), but not with pre-pregnancy BMI overweight (P for interaction = 0·173). Significant decreased risk of preterm birth was associated with fish and shellfish consumption among women who were aged 30 years or older (OR = 0·71, 95 % CI 0·55, 0·91) and those who had pre-pregnancy BMI underweight (OR = 0·61, 95 % CI 0·49, 0·76).
Table 4. Associations between total fish consumption and preterm birth by maternal age (n 10 179) and pre-pregnancy BMI (n 9830)
(Numbers and percentages; odd ratio and 95 % confidence intervals)
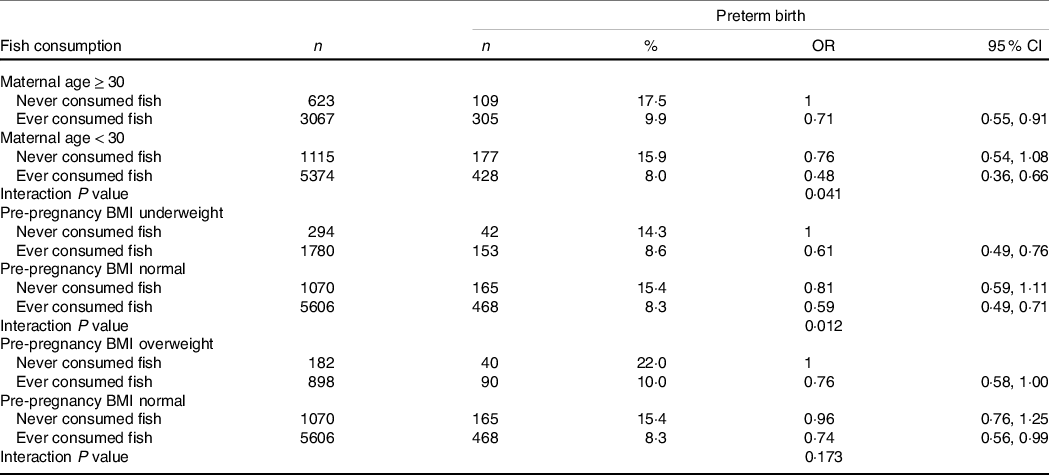
Adjusted for maternal age, educational level, monthly family income, parity, hypertensive disorder during pregnancy, gestational diabetes, pre-pregnancy BMI, smoking (active and passive smoking) during pregnancy, physical activities during pregnancy, multi-vitamin and protein supplement intake during pregnancy and total energy intake.
Discussion
Our main findings in the present study were that there was a significant association between maternal fish and shellfish consumption and lower risk of preterm birth by clinical subtypes. It supports the hypothesis that the incidence of preterm birth could decrease with increasing fish and shellfish intake. Especially, the associations were slightly stronger for very preterm birth and spontaneous preterm birth. These findings have reasonable biological mechanisms. The beneficial effects of fish and shellfish have primarily been attributed to the long-chain n-3 fatty acids. Recent studies confirmed that LCn-3PUFA influenced the formation of prostaglandins in fetal membranes and affected the length of gestation(Reference Salvig and Lamont33). Moreover, several types of fish and shellfish are rich dietary sources of vitamin D(Reference Hypponen and Power34), deficiency of which has been associated with preterm birth(Reference Scholl and Chen35). Fish and shellfish are also a good source of B-complex and several essential amino acids and trace elements (such as Se, Ca, Mg, K and iodine), which are related to possible beneficial birth outcomes(Reference Buppasiri, Lumbiganon and Thinkhamrop36,Reference Morse37) .
In our population, consumption of fish and shellfish ≥ 2 times a week had a protective effect on preterm birth, which is consistent with some earlier findings(Reference Olsen and Secher12). Several observational studies have demonstrated the association of fish and shellfish consumption with lower risk of preterm birth(Reference Olsen and Secher12,Reference Olsen, Osterdal and Salvig15,Reference Haugen, Meltzer and Brantsaeter16,Reference Leventakou, Roumeliotaki and Martinez17,Reference Brantsaeter, Englund-Ogge and Haugen18,Reference Klebanoff, Harper and Lai19) . A meta-analysis from nineteen European birth cohorts found 11 to 13 % reduction in preterm birth among women who consumed fish and shellfish twice or more/week, compared with those who consumed once or less/week (Reference Leventakou, Roumeliotaki and Martinez17). A Norwegian cohort study has categorised fish consumption in a similar manner to our study and reported an adjusted HR of 0·76 for 1–2 servings/week (20–40 g/d), 0·72 for 2–3 servings/week (40–60 g/d) and 0·72 for >/=3 servings/week (>60 g/d), P trend < 0·001(Reference Brantsaeter, Englund-Ogge and Haugen18). Overall, our findings agree with the recommendations of the Chinese Nutrition Society dietary guideline for pregnant women, showing that 350–525 g of seafood should be consumed/week during pregnancy(20). However, it is also noteworthy that too much intake of seafood might also introduce increased levels of toxins and pollutants in pregnancy and thus lead to adverse pregnancy outcomes(Reference Oken and Bellinger38). In a review on fish consumption, methylmercury and child neurodevelopment, Oken et al.(Reference Oken and Bellinger38) found that high consumption of fish was associated with high-dose mercury exposure, which may lead to babies with devastating neurological handicaps, including delayed attainment of developmental milestones, blindness, deafness and cerebral palsy. Our study also found P for trend was significant in spontaneous preterm but not medically indicated preterm, indicating that the most important threshold for fish and shellfish intake may be any intake as compared with no intake at all. This assumption is also supported by our following analysis of preterm risk based on quartiles of fish and shellfish consumption, where we found that the 75–176 g/week and > 176 g/week consumption groups had significantly decreased risk of preterm birth compared with the < 14 g/week consumption group. In a balance of advantages and disadvantages, it is thus suggested that pregnant women intake appropriate amount of fish during pregnancy to maximise its beneficial effects and to minimise its toxic effects. For women who cannot consume the amount of fish and shellfish as recommended by the Chinese Nutrition Society, as shown in our study that nearly 90 % did not consume > 350 g/week of fish and shellfish, consumption of a minimum of 176 g/week of fish and shellfish is recommended to prevent preterm risk.
When we examined fish and shellfish consumption by types, significant associations with preterm birth were observed for freshwater fish intake, shellfish intake, as well as any two or three kinds of fish intake, but not for saltwater fish. The protective role of freshwater fish in preterm birth was encouraging considering the fact that most of the fish and shellfish consumed in the current study originated from freshwater. Freshwater fish constitutes primarily cultured carp, a fish species for which China has a longstanding tradition for culturing with massive production. Carp is a lean fish species with low fat content, and the main feed for carp culture includes bean cake, silkworm pupae, fish meal and other high protein feed. Carp and other freshwater fish are rich in a range of nutrients, including fat, protein, EPA, DHA, Ca, Fe, Zn, iodine, Se, vitamin E, vitamin D3, niacin, etc. However, they may also contain certain contaminants such as DDT, PCB7, Hg, Ar and Cd. The amount of each nutrient and contaminant has been listed in Du et al.’s study(Reference Du, Zhang and Wang39), which generally supported that fish can be regularly consumed to achieve optimal nutritional benefits, without causing significant contaminant-related health risks.
The finding that shellfish intake is protective of preterm birth is interesting considering the reported high levels of heavy metals and other toxins in shellfish harvested in saltwater in some European countries. However, in China, shellfish are mainly manually raised in mariculture. China is a large producing country for shellfish, and shellfish is also one of the most important aquaculture species in China(40). The Chinese government set very strict standards to limit the concentration of heavy metals in shellfish(Reference Liu Huan, Li and Song41). Liu et al. (40) conducted a study to assess the level of heavy metals in various coastal areas of China that include Dalian, Shandong, Zhejiang, Guangdong, East China coast and South China coast and found that heavy metal levels in all these areas were within safe limit. In an inland city like Lanzhou, shellfish are mainly transported from various Marine aquaculture bases in the above-mentioned coastal areas of China and have passed strict testing for heavy metal and toxins and thus do not pose significant health risk to pregnancy.
No significant association was found between maternal saltwater fish and preterm birth, which may be best explained by the relatively small sample size of maternal saltwater fish consumption (n 55). For instance, some previous studies have demonstrated that prediction models based on logistic regression in small data sets might lead to poor predictions that were too extreme and uncertain(Reference Steyerberg42,Reference Altman and Royston43,Reference Vergouwe, Steyerberg and Eijkemans44) . Other possible explanations relate to more contaminants in saltwater fish(Reference Nesheim and Nestle45,Reference Halldorsson, Meltzer and Thorsdottir46) and nutrient loss in the progress of frozen storage period(Reference Sampels47).
Finally, we found significant interactions between fish and shellfish consumption with maternal age and between fish and shellfish consumption with pre-pregnancy BMI underweight in affecting preterm birth. Generally speaking, the positive effects of fish consumption may offset the negative impacts of older maternal age and abnormal pre-pregnancy BMI underweight on preterm birth. Older maternal age and abnormal pre-pregnancy BMI have been identified as risk factors for preterm birth(Reference Ogawa, Urayama and Tanigaki48,Reference Fitzpatrick, Tuffnell and Kurinczuk49,Reference Averett and Fletcher50) , which may be balanced by the beneficial effects of fish and shellfish consumption and thus decrease risk of preterm birth. The finding of significant interactions between fish and shellfish consumption with pre-pregnancy BMI underweight, but not pre-pregnancy BMI overweight was somehow surprising and may be explained by the relatively small sample size in pre-pregnancy BMI overweight group who never consumed any fish. Future large sample-size study may be needed to further explore the association of fish and shellfish consumption with preterm birth among pre-pregnancy BMI overweight population.
The protective effect of fish and shellfish consumption in preventing preterm birth was more obvious in younger age group (OR = 0·48, 95 % CI 0 36, 0·66) than older age group (OR = 0·71, 95 % CI 0 55, 0·91). However, our study also showed women with younger age were less likely to consume fish and shellfish, a pattern consistent with findings in other countries such as USA(Reference Jahns, Raatz and Johnson51), England(Reference Weichselbaum, Coe and Buttriss52) and Norway(Reference Olsen53). These findings imply that younger people were less likely to consume fish despite its larger protective role in preventing preterm birth. One explanation may be that older people attach more importance to nutrition and health than younger people and thus are more likely to consume fish and shellfish for perceived health benefits in addition to its convenience in preparation(Reference Jahns, Raatz and Johnson51). However, future studies are still needed to explore the underlying reasons for less fish and shellfish consumption among younger people and further confirm the associations between fish and shellfish consumption and preterm birth across maternal age and pre-pregnancy BMI. Our findings provide implications for strengthening publicity and education to promote fish and shellfish consumptions among younger pregnant women to prevent preterm birth.
Our study had many strengths. First, the data were collected from a relatively large number of pregnant women and included comprehensive information such as maternal diet, demography, socio-economic factors and pregnant outcomes. Second, we collect detailed information on the consumption of different fish and shellfish types, both in frequency and quantity, which enabled us to run separate analyses. Third, our well-characterised participants cohort had high rates of participation and follow-up, which allowed us to extensively collect information on many potential confounding variables.
Nevertheless, our study also had some limitations. One major limitation is the retrospective study design making it susceptible to selection bias, misclassification and recall bias, which were common in studies that reply on individual recall of former exposure to risk factors. Besides, it is also more difficult to assess temporal relationship in retrospective studies since everything is based on recalls. Future prospective cohort studies are needed to better confirm the impacts of fish and shellfish consumption on preterm birth. Second, the timing of obtaining information through in-person interviews 1–3 d after delivery may introduce potential selection bias. Delivery is such an exhausting process that some women may be too tired to participate in any interviews right after delivery, which may also explain that 3712 chose not to participate and 105 did not complete in-person interviews. Future studies may consider using a longer post-delivery interview time period such as 2 weeks after delivery to increase inclusion rate. Third, fish and shellfish consumption was assessed using a self-designed FFQ and based on self-report. Although the FFQ has been used in various studies of our project, it has not been formally validated and the reliance on self-report may introduce recall bias. Future study may consider validating the FFQ against another standard dietary reference method and improve the quality of dietary reports by combining other more objective measurement methods. Fourth, we did not measure certain biomarkers, such as erythrocytes concentration of n-3 fatty acids or chemical exposures to accurately assess fish and shellfish intake and contaminant intake during pregnancy. Future studies may benefit from adding these biomarkers of environmental nutrients or contaminants. Fifth, the sample sizes were very small for certain types of fish consumption groups such as saltwater fish only and shellfish only groups in the current study, making it difficult to detect statistical significance in their associations with preterm birth. However, these types of fish consumption are not uncommon and also important food sources among pregnant women and thus are of research interest. Future larger sample study is needed to further test the impact of these fish consumption groups on preterm birth. Sixth, we did not control for potential confounding effect brought about by other food sources apart from the fish and shellfish studied in the current study. For instance, pregnant women may also get long-chain n-3 fatty acids from other supplements apart from fish and shellfish. Future study may consider measuring all food sources to confirm the beneficial effect of fish and shellfish more robustly.
In conclusion, our study showed that maternal fish and shellfish consumption was associated with reduced risk of preterm birth. The association was seen for all subcategories of preterm birth and slightly stronger for very preterm birth and spontaneous preterm birth. The amount and the type of fish and shellfish consumption are also important. The findings corroborate the current advice to include fish and shellfish as part of balanced diet during pregnancy. Future studies should consider more potential factors, such as fish and shellfish preparation, nutrient and contaminant and examine whether they are associated with preterm birth.
Acknowledgements
We would like to thank all the participants in this study. This work was funded by Gansu Province of China Health Industry Research Project (GSMSKY-2019-11). L. W. and W. Z.: designed the research; Z. X. F., W. D., S. Z. and C. Z.: analysed the data; W. Z. and L. W.: wrote the paper and all authors: read and approved the final manuscript. The authors have nothing to declare.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114521003858








