The COVID-19 pandemic has had a profound impact on the mental health of healthcare workers globally. The nature of the pandemic, including the high transmissibility of the virus, lack of effective treatments, unprecedented workload and shortages in personal protective equipment (PPE), resulted in significant challenges for healthcare staff,Reference Lake, Narva, Holland, Smith, Cramer and Fitzpatrick Rosenbaum1,Reference Dobson, Malpas, Burrell, Gurvich, Chen and Kulkarni2 with ongoing consequences for mental health.Reference Umbetkulova, Kanderzhanova, Foster, Stolyarova and Cobb-Zygadlo3,Reference Cenat, Farahi, Dalexis, Darius, Bekarkhanechi and Posson4 In addition, healthcare workers have had to navigate complex ethical dilemmas, such as deciding who should receive treatment when resources are limited, which have resulted in moral distress.Reference Riedel, Kreh, Kulcar, Lieber and Juen5–Reference Norman, Feingold, Kaye-Kauderer, Kaplan, Hurtado and Kachadourian7 Social isolation, stigma and dealing with extensive absenteeism within the workforce have all created further burdens and mental health risk during varied stages of the pandemic.Reference Iacobucci8 A now extensive evidence base highlights the high mental health need and range of factors associated with psychological distress among hospital staff responding to COVID-19.Reference Chutiyami, Cheong, Salihu, Bello, Ndwiga and Maharaj9,Reference Dragioti, Tsartsalis, Mentis, Mantzoukas and Gouva10 Recent evidence suggests that nuanced factors may be associated with changes in mental health over time.Reference Umbetkulova, Kanderzhanova, Foster, Stolyarova and Cobb-Zygadlo3
Longitudinal research to date has provided valuable insights into the psychological impacts of the pandemic.Reference Cenat, Farahi, Dalexis, Darius, Bekarkhanechi and Posson4,Reference Robinson, Sutin, Daly and Jones11 A recent systematic review of longitudinal research across disasters and health emergencies indicated that pandemics are associated with significantly higher levels of post-traumatic stress symptoms (PTSS) compared with most other disaster types, and higher levels of anxiety that reduced after the first year to levels consistent with other disasters.Reference Newnham, Mergelsberg, Chen, Kim, Gibbs and Dzidic12 Longitudinal studies of healthcare workers’ mental health symptoms have revealed worsening psychological symptoms over time,Reference López Steinmetz, Herrera, Fong and Godoy13–Reference Th'ng, Rao, Ge, Neo, De Molina and Lim15 although a small number have demonstrated improvements in the latter stages of the pandemic.Reference Umbetkulova, Kanderzhanova, Foster, Stolyarova and Cobb-Zygadlo3 Importantly, workload stress has increased over the pandemic period across global settings,Reference Th'ng, Rao, Ge, Neo, De Molina and Lim15 increasing psychological stress among staff,Reference Park, Closser, Cooney, Atkins, Thrul and McDonald16 with significant implications for retention and staff leave patterns.Reference Hendrickson, Slevin, Hoerster, Chang, Sano and McCall17,Reference McGuinness, Zhong, Eades, Di Donato, Collie and Kelsall18 To date, studies have focused on areas heavily affected by the pandemic, and few studies have explored the mental health impacts for healthcare workers operating in settings with widespread public health protections.Reference Newnham, Mergelsberg, Tearne, McEvoy, Stanley and Celenza19
Western Australian context
Western Australia's early response to the COVID-19 pandemic was proactive and effective in preventing the spread of the virus.Reference House, Rawlins, Dyer, Boan and Musk20 The state government implemented a range of measures in the initial stages, including international and state border closures, quarantine requirements, rapid lockdowns and an extensive vaccination campaign. As a result, 99% of the 2.7 million population had received two COVID-19 vaccinations and 65% had received three vaccinations before the first major community outbreak in March 2022,Reference Macali21,22 and thus healthcare staff had been largely protected from infection risk and surges in healthcare need. However, witnessing the pandemic's effects on the physical and mental health of healthcare staff overseas created significant anticipatory stress.Reference Digby, Winton-Brown, Finlayson, Dobson and Bucknall23 An assessment of PTSS, depression and anxiety status among Western Australian healthcare staff in the lead up to the borders reopening (and the first major community wave) demonstrated moderate levels of mental health concerns, despite the low number of COVID-19 cases.Reference Newnham, Mergelsberg, Tearne, McEvoy, Stanley and Celenza19 Reported mental health concerns were lower than those recorded in other states of AustraliaReference Dobson, Malpas, Burrell, Gurvich, Chen and Kulkarni2,Reference Smallwood, Karimi, Bismark, Putland, Johnson and Dharmage24,Reference Holton, Wynter, Trueman, Bruce, Sweeney and Crowe25 and global reports,Reference Saragih, Tonapa, Saragih, Advani, Batubara and Suarilah26,Reference Marvaldi, Mallet, Dubertret, Moro and Guessoum27 indicating some support for the mental health effects of strong protections early in the pandemic.Reference Newnham, Mergelsberg, Tearne, McEvoy, Stanley and Celenza19
Study aims
Western Australia's engagement in emergency preparedness for the 2 years preceding the COVID-19 outbreak presents a unique setting to explore the longitudinal impacts of pandemic response on the healthcare system. Accordingly, we aimed to determine the risk and protective factors associated with changes in mental health status among Western Australian healthcare workers responding to the pandemic. We assessed symptoms of PTSS, depression and anxiety both before and after the first major community wave of COVID-19, and measured a range of risk and protective factors at each time point. Building on the findings at baseline,Reference Newnham, Mergelsberg, Tearne, McEvoy, Stanley and Celenza19 it was hypothesised that (a) PTSS, depression and anxiety symptoms would increase across the sample after the first COVID-19 wave in Western Australia; (b) female gender, nursing professions, sleep difficulties and workplace stressors would be associated with increases in PTSS, depression and anxiety symptoms over time; and (c) higher levels of social support, workplace support and older age would play a protective role for PTSS, depression and anxiety symptoms over time.
Method
Participants and procedure
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2013. All procedures involving human participants were approved by the Department of Health North Metropolitan Area Mental Health Services Human Research Ethics Committee (approval number: RGS-4034). Healthcare staff employed at four major tertiary hospitals and a large mental health service in metropolitan Perth and the Peel region were invited to participate. All health staff (including doctors, nurses, midwives, allied health professionals, auxiliary staff, executives and management) were eligible. The study was promoted via online flyers through Department of Health staff communications, hospital-wide forums and team meetings. A website was established, accessed via a QR code on the flyer, which would direct staff to the survey. All participants provided written informed consent online before accessing the survey at each time point. Participants completed the first survey between 30 November 2021 and 7 March 2022. The data were deidentified, and participants created a private unique code to link data at later stages. Respondents were asked to provide their email address to enable follow-up, which was stored separately to the data. The follow-up assessment was conducted between 5 September and 31 October 2022. All participants who had consented and provided an email address were sent an email inviting their participation in the second survey. Completion of the questionnaires took 15–20 min. At each time point, three participants were selected at random and sent a $50 supermarket gift voucher to thank them for their time.
Measures
A suite of validated and original measures was administered at each time point via an online survey.Reference Qualtrics28 Full psychometric details for the study measures have been published previously.Reference Newnham, Mergelsberg, Tearne, McEvoy, Stanley and Celenza19
Demographic characteristics
Demographic data were collected on age, gender, profession, department, work setting, employment status, prior experience working with infectious disease, COVID-19 exposure and training.
Workplace factors
Work-related stressors and supports scales were developed by the study team, based on a review of the relevant literature, consultations with healthcare staff (n = 7), and team expertise. The scales were designed to capture relevant stressors and supports and were revised at follow-up to reflect the current context. Workplace stressor items included concerns regarding infection (COVID-19 and other illness), increases in workload, access to PPE, financial security, team cohesion, management of home and work responsibilities, and stigma. Supports included frequent and timely information, clarity of responsibilities, access to PPE, hospital leadership responsiveness, team and management support. Workplace stressors and supports were measured on a five-point Likert scale, sum scores were calculated, and higher scores indicated higher levels of work-related stress or satisfaction, respectively. Internal consistency was high at baseline for workplace stressors (α = 0.88, ωt = 0.90) and supports (α = 0.91, ωt = 0.92).
Protective factors
Coping strategies were assessed with the four-item Brief Resilient Coping Scale questionnaire,Reference Sinclair and Wallston29 rated on a five-point Likert scale (α = 0.71). Higher scores indicated better coping. Social support was measured with the three-item Oslo Social Support ScaleReference Dalgard, Bj and Tambs30 (α = 0.77). A sum score was calculated (range: 3–14), with higher scores indicating stronger social support. The average interitem correlation was good (Mean r = 0.55), with α = 0.77.
Sleep quality
Sleep difficulties were assessed with the Sleep Condition Indicator.Reference Espie, Kyle, Hames, Gardani, Fleming and Cape31 A sum score was calculated ranging from 0–32, with higher scores indicating greater sleep difficulty. We applied a cut-off score of 16 to report prevalence of probable insomnia disorder, shown to have a sensitivity of 89% and specificity of 82%.Reference Espie, Kyle, Hames, Gardani, Fleming and Cape31 The average interitem correlation was good (Mean r = 0.52), with α = 0.88 at baseline.
PTSS
Trauma exposure was measured via the PCL-5 Trauma Checklist, and PTSS were assessed with the Primary Care PTSD Screen for DSM-5.Reference Prins, Bovin, Smolenski, Marx, Kimerling and Jenkins-Guarnieri32 A sum score was calculated for those who experienced trauma, on five items related to the experience they listed as most distressing (range: 0–5, higher scores indicating higher levels of PTSS). The average interitem correlation suggested that the items were homogeneous, but also containing sufficient unique variance (Mean r = 0.31), with α = 0.69. Prevalence of probable clinical levels of PTSS was reported with a cut-off point of 4 points as recommended.Reference Prins, Bovin, Smolenski, Marx, Kimerling and Jenkins-Guarnieri32,Reference Williamson, Stickley, Armstrong, Jackson and Console33
Depressive symptoms
Depression was assessed with the Patient Health Questionnaire-9,Reference Kroenke, Spitzer and Williams34 scoring each of the nine DSM-5 depression criteria on a four-point Likert scale. The average interitem correlation suggested that the items were homogeneous, but also containing sufficient unique variance (Mean r = 0.46) with α = 0.88. Sum scores were calculated (range: 0–27), with higher scores indicating higher levels of depression. Scores of 5, 10, 15 and 20 were taken as the cut-off points for mild, moderate, moderately severe and severe depression, respectively, consistent with prior research in a comparative sample.Reference Smallwood, Karimi, Bismark, Putland, Johnson and Dharmage24
Anxiety symptoms
Anxiety was assessed with the Generalised Anxiety Disorder-7,Reference Spitzer, Kroenke, Williams and Löwe35,Reference Swinson36 using the four-response option. The average interitem correlation suggested that the items were homogeneous, but possibly not containing sufficient unique variance (Mean r = 0.61), with α = 0.92. Sum scores were calculated (range: 0–21), and scores of 5, 10 and 15 were taken as the cut-off points for mild, moderate and severe anxiety, respectively, consistent with prior research.Reference Smallwood, Karimi, Bismark, Putland, Johnson and Dharmage24
Data analysis
Data were exported from Qualtrics (XM Platform for Windows, Qualtrics, Seattle, Washington, USA; www.qualtrics.com) and uploaded in R statistics (version 4.2.2 for Windows, Lucent Technologies Inc., New Jersey, USA; www.r-project.org). Descriptive statistics were reported in tables. Little's missing values analyses were conducted and missing data were imputed with mean values. Three conditional latent growth curve analyses were completed to assess changes in symptoms over time, using the lavaan packageReference Rosseel37 for each outcome (PTSS, anxiety and depression). Nine predictors were included for the intercept (age, gender, profession, COVID-19 exposure, trauma exposure, work stressors, coping, social support and work support, all of which were assessed at baseline), and the interaction effects between work support and COVID-19 exposure and insomnia and COVID-19 exposure. Four variables assessed at follow-up (work stressors, work support, profession change and trauma exposure: total of 13 variables and two interaction effects) were added as predictors of the slopes. Categorical predictors in the analyses were grouped into fewer levels: gender (0 = male, 1 = female), profession (0 = managerial, 1 = admin, 2 = allied health, 3 = doctor, 4 = nurse and midwifery), profession change (0 = not changed, 1 = changed), COVID-19 exposure (0 = no exposure to COVID-19, 1 = exposure to COVID-19) and trauma exposure (0 = no trauma exposure, 1 = exposure to trauma). Age, insomnia, coping, social support, work support and workplace stressors were included as continuous variables. Goodness of fit of the dataReference Kenny38 to the models was assessed with χ 2 (P < 0.050), comparative fit index (CFI; >0.95), Tucker–Lewis index (TLI; >0.95), root mean square error of appoximation (RMSEA; <0.06) and standardised root mean square residual (SRMR; <0.06).
Results
Descriptive statistics, missingness and bivariate correlations
A total of 563 individuals accessed the baseline survey, 533 provided consent to participate and 431 provided data. The follow-up survey was accessed on average 7.84 (s.d. = 1.11) months after the baseline survey, by a total of 241 people, with 218 starting the survey questions (50.6% response rate). Detailed baseline data have been reported previously.Reference Newnham, Mergelsberg, Tearne, McEvoy, Stanley and Celenza19 Of the 218 who completed the follow-up survey, 11.5% of data were missing. There were 11 cases with >80%, and 21 cases with >50% of missing data. Little's missing completely at random test on n = 218 was significant (P < 0.001), indicating the data were not completely missing at random; people dropped out of the survey over time, but no other patterns were observed when comparing the demographic, predictor and outcome values in those with missing and no missing data, using the naniar package.Reference Tierney and Cook39
Of the 218 people who completed the follow-up survey, we were able to match baseline data for 183 participants; n = 35 had follow-up data but no matched baseline data, and n = 249 had baseline data but no follow-up data. There were no differences at baseline between those who completed the follow-up and those who did not, except for employment (P = 0.002), with fewer people in casual employment contracts completing the follow-up survey (0.5% at follow-up v. 5.2% at baseline). We ran the models with and without imputed values, to check whether imputation of missing values biased our results, and we found no difference in patterns of results. This provided support that imputation of missing values did not change or skew our analyses.
The following results only include the matched participants (n = 183). The mean age of the sample at baseline was 42.8 (s.d. = 11.6), comprising predominantly women (84% women, 15% men and 0.5% other gender). At baseline, most participants worked with in-patients (n = 54, 30%), out-patients (n = 38, 21%) or both (n = 48, 26%). Fewer worked in the emergency department (n = 25, 14%), the office (n = 21, 11%), or in the community (n = 6, 3.3%) or other setting (n = 6, 3.3%). There was no difference between baseline and follow-up in the number of areas people worked in, and participants worked mostly in one area (time point 0 (T0): 77% v. time point 1 (T1): 80%; P = 0.500). The sample comprised mostly nurses (n = 77, 42%) and allied health professionals (n = 55, 30%), followed by administrative (n = 20, 11%) and managerial staff (n = 15, 8.2%). Doctors (n = 8, 4.4%), midwives (n = 6, 3.3%) and executives (n = 1, 0.5%) are less represented in the sample. Between the baseline and follow-up survey, nurses (n = 29, 43%) and allied health professionals (n = 20, 30%) chose to change their professional role most often. Those in managerial (n = 6, 9.1%), administrative positions (n = 5, 7.6%), practicing as midwifes (n = 4, 6.1%), executives (n = 1, 1.5%) or doctors (n = 1, 1.5%) changed their professions least often (see Table 1 for a detailed comparison between employment status and work settings at baseline and follow-up).
Table 1 Changes in employment and work settings for healthcare workers in Western Australia (N = 183)
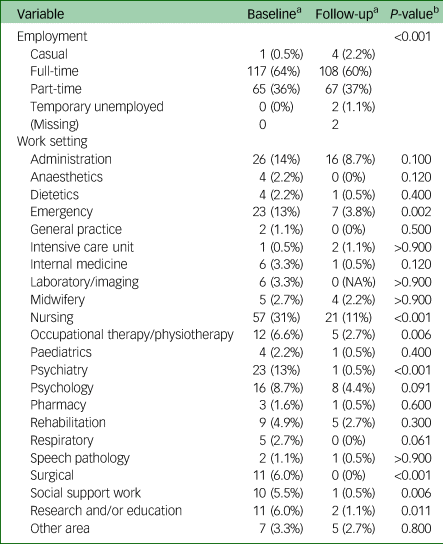
a. n (%).
b. Fisher's exact test; Pearson's χ 2-test.
Most survey respondents did not have prior experience with a pandemic outbreak (n = 144, 79%). In the baseline survey, exposure to COVID-19 was assessed with three items, two of which were repeated at follow-up. On these two items, there were significant increases in exposure to COVID-19 from baseline to follow-up (all P < 0.001). At follow-up, more participants had provided direct care to COVID-19 patients (52% v. 14% at baseline) and more worked in a COVID-19 clinic or swabbed patients (27% v. 9.8% at baseline). The proportion of people reporting that they had been exposed to COVID-19 in the workplace was similar (T0: 49% v. T1: 55%; P = 0.200).
There was a similar rate of reported exposure to traumatic experiences across the study period (T0: 84% v. T1: 88%; P = 0.400) and the number of traumas experienced (T0: mean 3.2, s.d. = 2.1 v. T1: mean 3.4, s.d. = 2.0; P = 0.200). Table 2 shows the detailed trauma types assessed at baseline and follow-up; experiencing infectious disease and a life-threatening illness were the only two that significantly increased in frequency over time. The sum of trauma exposures did not change over time (T0: mean 3.2, s.d. = 2.1 v. T1: mean 3.4, s.d. = 2.0; P = 0.200).
Table 2 Trauma exposure among healthcare workers in Western Australia (N = 183)
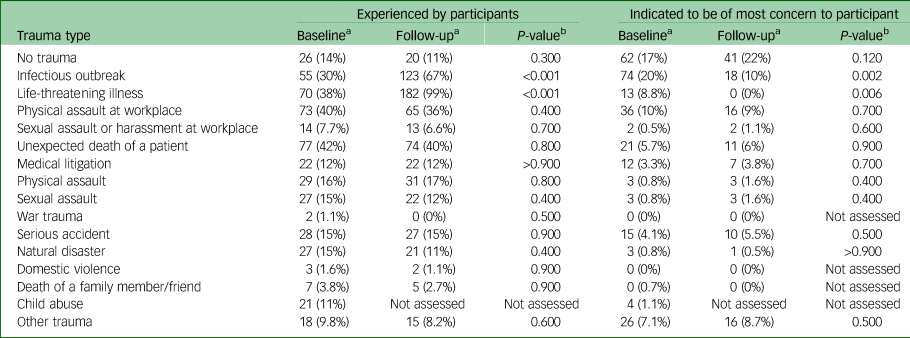
One item was not in the follow-up survey as this related to a trauma experienced in childhood specifically and would not have changed over time. Types of ‘Other trauma’ reported at baseline and follow-up included staff violence, verbal abuse and bullying, limited adherence to proper mask wearing and physical distancing by staff including line managers and doctors, co-worker suicide, prolonged duress when senior co-workers have regular meltdowns, self-harm and suicide attempts, murder and family mental health issues.
a. n (%).
b. Fisher's exact test; Pearson's χ 2-test.
Levels of work stress and work support experienced by healthcare professionals in Western Australia changed over time. Work stress decreased slightly (T0: mean 46.3, s.d. = 12.9 v. T1: mean 39.9, s.d. = 12.2, P < 0.001; d = 0.51) and work support decreased substantially (T0: mean 34.1, s.d. = 9.7 v. T1: mean 5.3, s.d. = 7.2; P < 0.001, d = 3.37) during the first wave of the pandemic. Overall, rates of PTSS, depression and anxiety symptoms remained stable over time (see Table 3).
Table 3 Mental health statistics for healthcare workers in Western Australia at baseline and follow-up (N = 183)
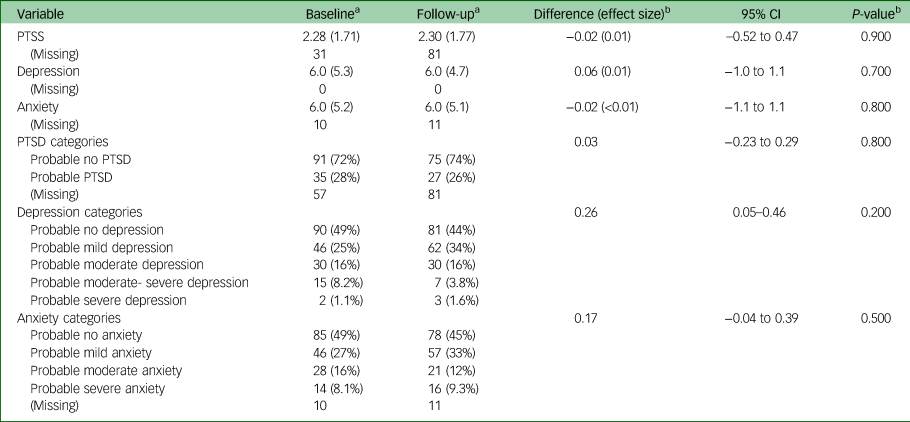
PTSS, post-traumatic stress symptoms; PTSD, post-traumatic stress disorder.
a. n (%).
b. Standardised mean difference (Cohen's d); Welch two-sample t-test.
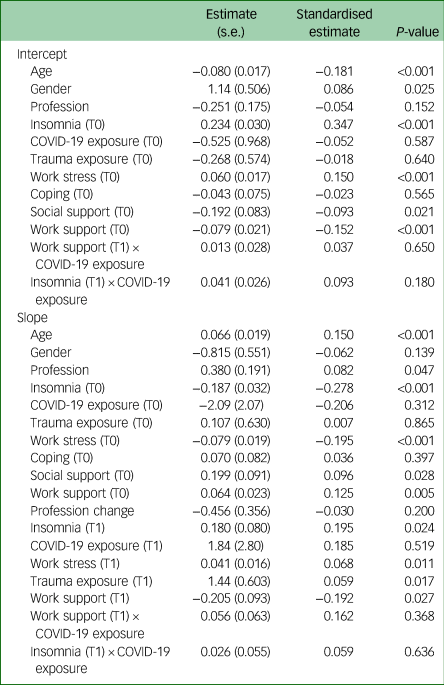
Latent growth model for PTSS and associated risk and protective factors
The hypothesised model had an excellent fit: χ2(5) = 2.15, P = 0.827, CFI = 1.0, TLI = 1.08, RMSEA < 0.001 and SRMR = 0.003. Both the intercept (2.96, s.e. = 1.08; P = 0.006) and slope (2.81, s.e. = 1.29; P = 0.029) were significant, indicating that PTSS was different from zero at baseline and increased significantly over time. The intercept and slope significantly covaried (−1.18, s.e. = 0.91; P < 0.001), which indicates that those with higher PTSS at baseline had a smaller decline in PTSS over time. As shown in Table 4, trauma exposure, work stress and insomnia significantly predicted PTSS severity at baseline, and insomnia (assessed at T0), trauma exposure (assessed at T0), work stress (assessed at T0 and T1), work support (assessed at T1) and the interaction between work support and COVID-19 exposure (assessed at T1) significantly covaried with the change of PTSS over time.
Table 4 Regressions covarying with the intercept and slope of post-traumatic stress symptoms
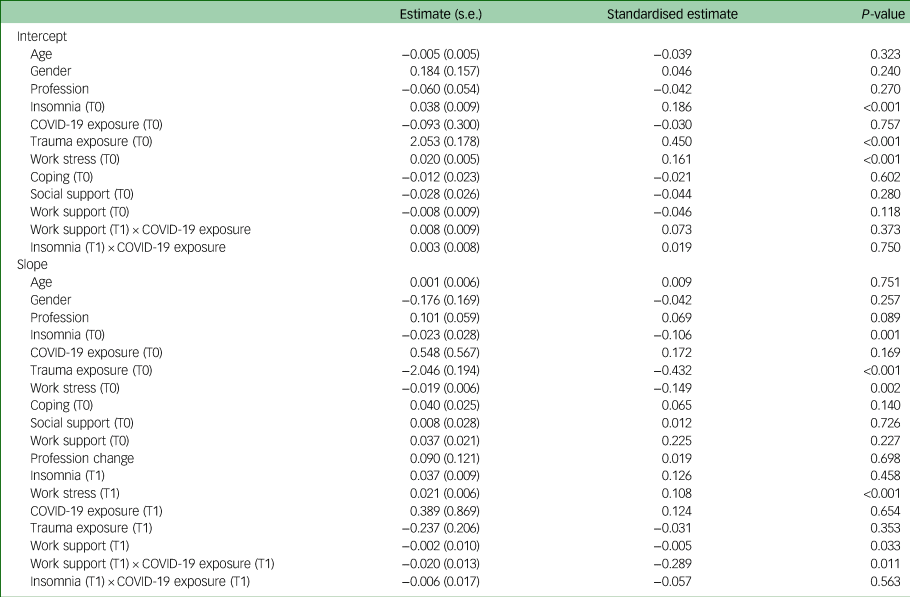
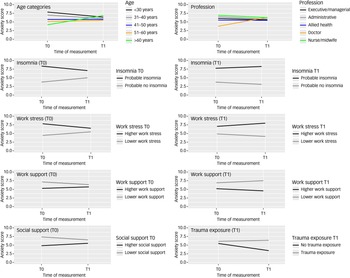
The directions of the significant effects are displayed in Fig. 1. Other predictors and interactions did not significantly affect the slope. Those with higher levels of baseline insomnia, work stress and trauma exposure had significantly higher PTSS baseline scores. Those with lower levels of these factors at baseline converged with those with higher levels over time. Further, those reporting higher work stress and lower work support measured at follow-up, had slightly higher PTSS at follow-up compared with those with lower work stress and higher work support. Those reporting lower work support at follow-up had experienced a larger increase in PTSS between baseline and follow-up than those reporting higher work support at follow-up. Insomnia measured at follow-up was associated with PTSS at baseline and at follow-up.

Fig. 1 Risk and protective factors associated with change in post-traumatic stress symptoms (PTSS) over time, in Western Australian healthcare professionals.
The significant interaction between work support and COVID-19 exposure indicates that there were differences in PTSS at baseline, but not at follow-up (i.e. everyone had high PTSS at follow-up). Not being exposed to COVID-19 at baseline and having high work support were associated with lower levels of baseline PTSS, whereas those who reported lower work support reported higher PTSS at baseline, similar to those who were exposed to COVID-19. The group that had not been exposed to COVID-19 at baseline and who reported high work support, experienced the largest increase in PTSS between baseline and follow-up.
Latent growth model for anxiety and associated risk and protective factors
The hypothesised model had an excellent fit: χ2(5) = 7.32, P = 0.198, CFI = 0.997, TLI = 0.981, RMSEA = 0.025 and SRMR = 0.009. The intercept (7.12, s.e. = 2.42; P = 0.003) was significant, but not the slope (−2.73, s.e. = 4.29; P = 0.525), indicating that anxiety symptoms were different from zero at baseline, but did not change significantly over time. The intercept and slope significantly covaried (−13.42, s.e. = 0.99; P < 0.001), indicating that those with higher anxiety symptoms at baseline had a smaller reduction in anxiety symptoms over time and those with lower anxiety symptoms at baseline had a larger increase. As shown in Table 5, age, gender, insomnia, work stressors, social support and work support significantly predicted anxiety severity at baseline, and age, profession, insomnia (assessed at T0 and T1), work stressors (assessed at T0 and T1), work support (assessed at T0 and T1), social support (assessed at T0) and trauma exposure (assessed at T1) significantly covaried with the change of anxiety over time.
Table 5 Regressions covarying with the intercept and slope of anxiety symptoms
The directions of the significant effects are displayed in Fig. 2. Other predictors and interactions did not significantly affect the slope. Younger age groups (≤40 years) showed a slight decrease in anxiety over time, and the middle age groups (41–60 years) showed no change (all stayed within mild anxiety levels). The older age category (>60 years) showed an increase in anxiety (from, on average, reporting no anxiety at baseline to mild anxiety at follow-up). Doctors showed significantly lower anxiety levels at baseline compared with other professions, but their anxiety levels converged with other professions at follow-up. Those with higher (versus lower) levels of insomnia, work stress and trauma exposure showed higher levels of anxiety at baseline and follow-up. Those with higher levels of social and work support showed lower levels of anxiety at baseline and follow-up.
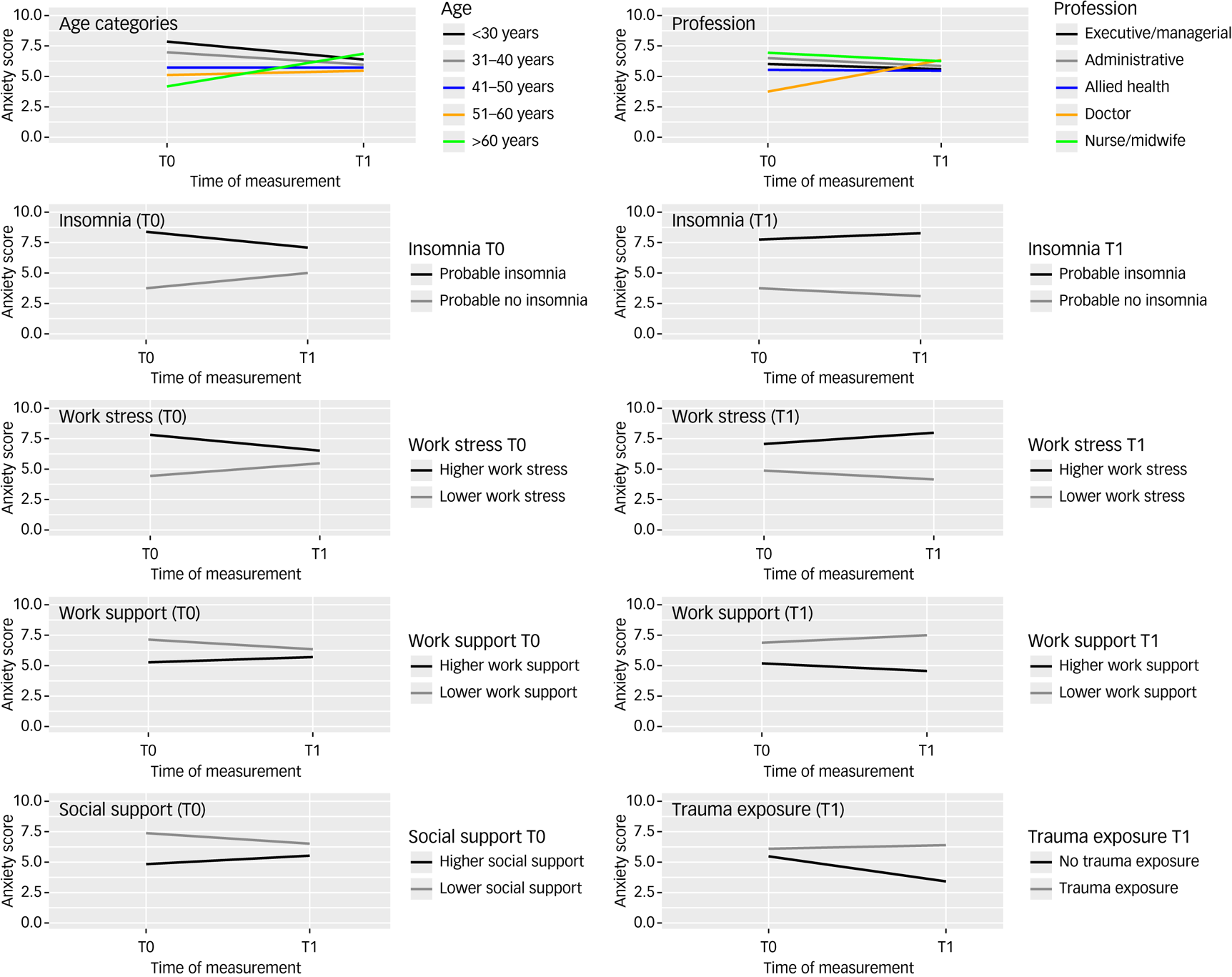
Fig. 2 Risk and protective factors associated with change in anxiety over time, in Western Australian healthcare professionals.
Those reporting no probable insomnia, lower work stress and lower work support at follow-up demonstrated a slight reduction in anxiety symptoms between baseline and follow-up, whereas those with probable insomnia, higher work stress and lower work support at follow-up experienced a slight increase in anxiety over time. Those reporting trauma exposure at follow-up had stable anxiety over time, whereas those with no trauma exposure had a reduction in anxiety over time.
Latent growth model for depression and associated risk and protective factors
The hypothesised model had an excellent fit: χ2(5) = 6.46, P = 0.264, CFI = 0.997, TLI = 0.976, RMSEA = 0.025 and SRMR = 0.006. The intercept (6.19, s.e. = 2.60; P = 0.017) was significant, but not the slope (−2.65, s.e. = 4.15; P = 0.523), indicating that depression symptoms were different from zero at baseline, but did not significantly change over time. The intercept and slope significantly covaried (−14.75, s.e. = 1.07; P < 0.001), indicating that those with higher depression symptoms at baseline had a smaller reduction in depression symptoms over time, or, in other words, those with lower depression symptoms at baseline had a faster increase in depression symptoms over time. As shown in Table 6, insomnia, work stressors, social support and work support significantly predicted the level of depression symptoms at baseline and insomnia (assessed at T0 and T1), work stress (assessed at T0 and T1), work support (assessed at T0), social support (assessed at T0) and profession change (assessed at T1) significantly covaried with the change of depression symptoms over time.
Table 6 Regressions covarying with the intercept and slope of depression symptoms
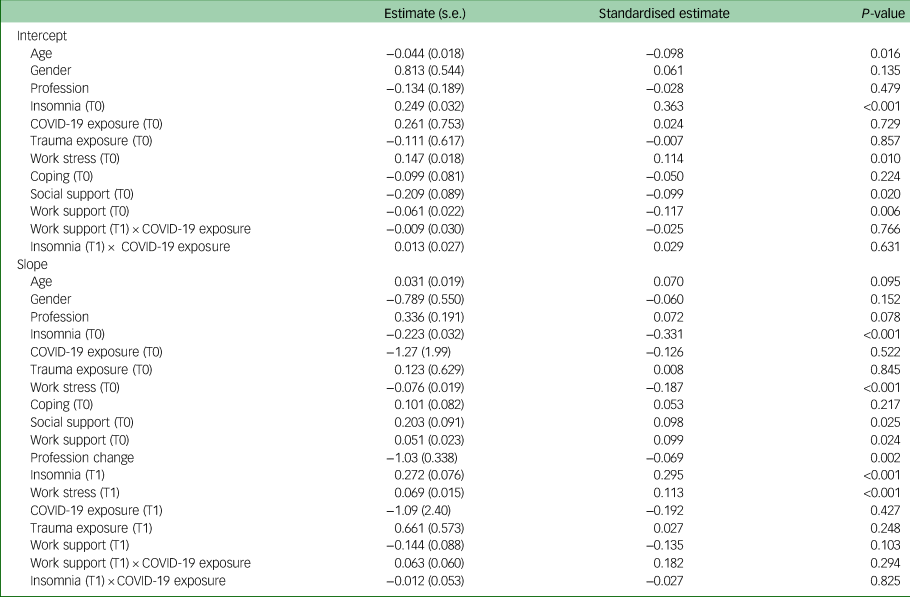
The directions of the significant effects are displayed in Fig. 3. Other predictors and interactions did not significantly affect the slope. Those with higher (versus lower) levels of insomnia and work stressors at baseline showed higher levels of depression at baseline, and those with higher and lower baseline insomnia converged together at follow-up. Participants with higher (versus lower) levels of insomnia and work stress at follow-up showed higher levels of depression at baseline, which stayed higher at follow-up. Those with higher levels of social and work support at baseline showed lower levels of depression at baseline, but this difference reduced at follow-up. Finally, depression levels decreased for those who changed their profession and increased for those who did not change their profession; however, the differences at baseline and follow-up were minimal.
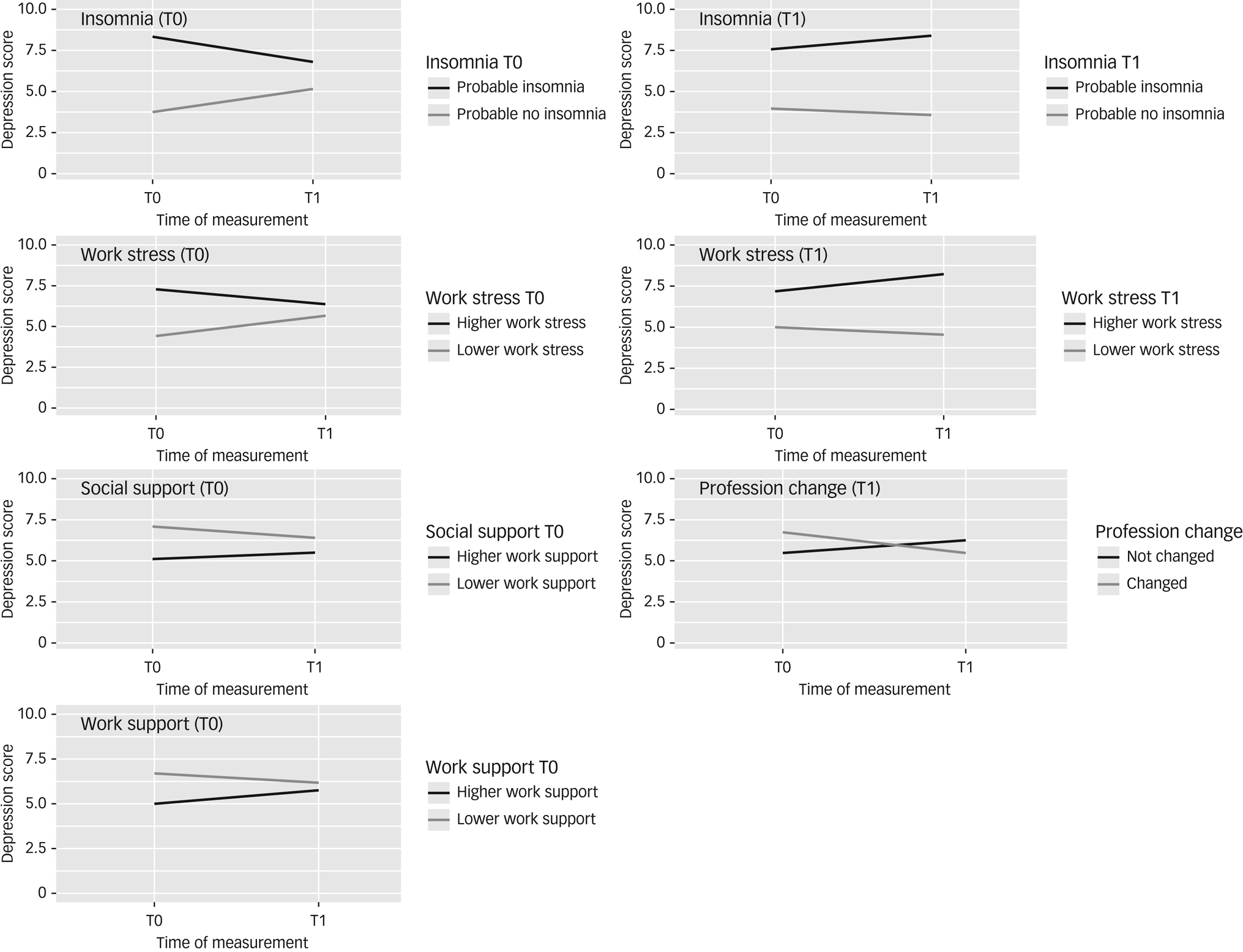
Fig. 3 Risk and protective factors associated with change in depression over time, in Western Australian healthcare professionals.
Discussion
Among healthcare workers responding to Western Australia's first COVID-19 wave, overall rates of PTSS, depression and anxiety remained stable over time; however, latent growth modelling revealed more nuanced patterns of change. Across all three mental health outcomes, a catch-up effect was evident, so that those with lower levels of symptoms at baseline demonstrated a larger increase in symptoms over time, converging with those reporting higher levels of symptoms. Conversely, those with higher levels of symptoms reported a smaller reduction, so that moderate levels of PTSS, depression and anxiety symptoms were evident among healthcare workers over the first wave of the pandemic in Western Australia. At follow-up, 21.4% of healthcare staff in our study reported probable levels of depression, and 24.1% reported probable anxiety; rates substantially higher than comparative Australian community samples (3–12.9% for depression and 10.6–17.5% for anxiety),Reference Stocker, Tran, Hammarberg, Nguyen, Rowe and Fisher40 although consistent with symptom levels reported by an Australian community sample (24.8 and 20%, respectively) during the first COVID-19 lockdown.Reference Hammarberg, Tran, Kirkman and Fisher41 The findings indicate that the onset of the first COVID-19 wave, although small compared with Australian and global data, created work-related stressors that increased mental health burden for healthcare staff that had not been as heavily affected before the wave, at a time when resources and workplace support were significantly reduced.
Longitudinal studies have depicted trajectories of increasing mental health symptomsReference Sasaki, Asaoka, Kuroda, Tsuno, Imamura and Kawakami14,Reference Hoffmann, Schulze, Löffler, Becker, Hufert and Gremmels42 and reduced self-perceived job performanceReference López Steinmetz, Herrera, Fong and Godoy13 among healthcare workers responding to the pandemic. However, more recent longitudinal assessments have shown some improvements in healthcare worker mental health in the latter stages of the pandemic,Reference Fattori, Comotti, Mazzaracca, Consonni, Bordini and Colombo43,Reference Mediavilla, Fernández-Jiménez, Martinez-Morata, Jaramillo, Andreo-Jover and Moran-Sanchez44 consistent with population pandemic data.Reference Newnham, Mergelsberg, Chen, Kim, Gibbs and Dzidic12 The current study extends prior longitudinal findings by assessing trajectories of psychological symptoms in a geographical setting that had two additional years to prepare for the onset of the COVID-19 pandemic. Accordingly, although healthcare staff faced significant anticipatory anxiety and stress and ongoing resource restrictions, the direct impacts of the pandemic were tempered by widespread community and health system preparedness, and low levels of transmission, compared with other Australian and international settings.Reference Newnham, Mergelsberg, Tearne, McEvoy, Stanley and Celenza19,Reference House, Rawlins, Dyer, Boan and Musk20
Study hypotheses (b) and (c) were partially supported, with key risk and protective factors influencing the pattern of psychological symptoms over time. Workplace stressors, including concerns about COVID-19 exposure, increases in workload, changes in role or responsibilities, reduced sense of community with colleagues, long COVID and vaccine access, were associated with all three mental health outcomes at baseline, and exacerbated anxiety and depression symptoms over time. Conversely, workplace support was protective for PTSS, anxiety and depression at baseline and follow-up. Workplace support included timely and clear information provided by hospital leadership and managers, access to PPE and training, leadership responsiveness to feedback, feeling supported and engaged in meaningful work. Both work stressors and supports were reported by participants to have reduced over the first COVID-19 wave (of particular note, a substantial reduction in workplace support despite the increasing COVID-19 case numbers). Workplace factors have demonstrated significant associations with mental health outcomes globally,Reference Willis, Ezer, Lewis, Bismark and Smallwood45,Reference Muller, Hafstad, Himmels, Smedslund, Flottorp and Stensland46 and highlight specific avenues to improve staff well-being at team and systemic levels.Reference Newnham, Mergelsberg, Tearne, McEvoy, Stanley and Celenza19 Healthcare staff have highlighted the importance of strong management, clear and timely sharing of information and workplace policies, and the protective role of team and management support during the pandemic, to reduce risk of burnout and moral injury.Reference Park, Closser, Cooney, Atkins, Thrul and McDonald16,Reference Willis, Ezer, Lewis, Bismark and Smallwood45 Prolonged periods of perceived institutional betrayal during the pandemic have been associated with a threefold increase in burnout, and increased desire to leave the workplace.Reference Park, Closser, Cooney, Atkins, Thrul and McDonald16
Contrary to our hypotheses, gender and specific healthcare profession were not associated with mental health outcomes over time in our study, although a change of professional role was associated with a small reduction in depression. Assessments conducted later in the COVID-19 pandemic have suggested that gender and profession have played less of a role in psychological health than originally indicated,Reference Fattori, Comotti, Mazzaracca, Consonni, Bordini and Colombo43 and workplace factors may be more important. Prior trauma exposure was associated with heightened PTSS at both baseline and follow-up in our study, and trauma exposure occurring during the study period was associated with increases in anxiety. Healthcare staff are exposed to a broad range of trauma types within and external to their professional roles. For example, workplace violence was reported by 40% of our sample at baseline and 36% reported exposure to workplace violence during the first wave. Attention to the safety of healthcare workers is critical to ensuring wellbeing, job satisfaction and optimal performance;Reference Park, Closser, Cooney, Atkins, Thrul and McDonald16 and systems of support in healthcare settings must be trauma-informed.Reference Chirico, Afolabi, Ilesanmi, Ferrari, Szarpak and Magnavita47
Sleep difficulties were associated in our study with higher levels of PTSS, depression and anxiety at baseline, and with increases in all three mental health difficulties over time. Meta-analyses of studies conducted during the COVID-19 pandemic indicate that two in five healthcare workers reported sleep difficulties.Reference Pappa, Sakkas and Sakka48 Constant changes in protocols and policies, irregular work hours, increased absences within work teams, fear of personal exposure to COVID-19 and the emotional burden of patient care have created a perfect storm for sleep disturbances among healthcare staff.Reference Marvaldi, Mallet, Dubertret, Moro and Guessoum27,Reference Pappa, Sakkas and Sakka48 The relationship between sleep difficulties and mental health issues appears to be bidirectional, and the current study indicates that sleep issues at baseline and follow-up were associated with increases in PTSS, depression and anxiety over time. These findings are consistent with evidence of the harmful effects of sleep disturbance among healthcare workers globally, which suggests a strong relationship between sleep disturbance and psychological distress,Reference Pappa, Sakkas and Sakka48 reduced concentration and cognitive function,Reference Medic, Wille and Hemels49 and increased risk of COVID-19 infection.Reference Kim, Hegde, LaFiura, Raghavan, Luong and Cheng50 Thus, sleep is a key risk to address in supporting healthcare professionals’ mental health in health emergencies.Reference Newnham, Mergelsberg, Tearne, McEvoy, Stanley and Celenza19,Reference Pappa, Sakkas and Sakka48
Limitations
Several limitations should be considered. First, despite efforts to recruit a large and diverse sample, the final number of matched cases was small. The length of the survey, and substantial burden on healthcare workers at the time of the study may have contributed to the limited participation rate. However, the sample size was comparable with other published longitudinal studies of healthcare staff during the pandemic.Reference Umbetkulova, Kanderzhanova, Foster, Stolyarova and Cobb-Zygadlo3 Second, although the study presents an assessment of healthcare workers’ mental health before and after the first COVID-19 wave, it should not be considered a pre- and post-pandemic design. Staff were acutely aware of the impending pandemic and the baseline symptom levels likely reflect anticipatory stress and high workloads in the lead up to the first outbreak.Reference Digby, Winton-Brown, Finlayson, Dobson and Bucknall23 Third, self-report measures do not reflect rates of psychopathology. Rather, the findings present an indication of the level of symptoms present in the sample. Further research is needed to determine specific areas for targeted intervention to support healthcare workers responding to prolonged emergency stressors, such as pandemics.
Implications
Western Australia successfully navigated the early years of the COVID-19 pandemic with minimal community transmission, enabling preparation of the healthcare system and widespread vaccination before a major outbreak.Reference Newnham, Mergelsberg, Tearne, McEvoy, Stanley and Celenza19,Reference House, Rawlins, Dyer, Boan and Musk20 However, despite the extended period of emergency preparedness, healthcare workers experienced significant psychological concerns. The current findings suggest that the first wave of the pandemic created a ‘catch-up’ in psychological difficulties among healthcare staff, so that those reporting low levels of PTSS, depression or anxiety before the first COVID-19 wave were likely to catch-up to those experiencing higher levels of psychological difficulties over time. Workforce recovery will require innovative, whole-of-sector, long-term approaches to support the well-being of staff. Strategies to improve workplace mental health require SMART work design principles (stimulating, mastery, agency, relational, tolerable demands), including additional training for management to ensure positive and inclusive workplace culture, clear communication and ongoing consultation of staff during periods of workplace change, relational approaches to building connectedness among teams, and clarity of role descriptions.Reference Park, Closser, Cooney, Atkins, Thrul and McDonald16,Reference Parker and Knight51 Further, ensuring the protection of staff from workplace violenceReference Somani, Muntaner, Hillan, Velonis and Smith52 and infection risk,Reference Kim, Hegde, LaFiura, Raghavan, Luong and Cheng50 and recruitment of additional staff to ensure effective workload management,Reference Digby, Winton-Brown, Finlayson, Dobson and Bucknall23 continue to be crucial needs. Coordinated efforts to support staff mental health will ensure sustainability of the health system during and beyond health emergencies.
Data availability
The data that support the findings of this study are available from the corresponding author, E.A.N., upon reasonable request.
Acknowledgements
We are grateful to the healthcare staff that participated in the study, for providing their time and insights.
Author contributions
The study was designed by E.A.N., E.L.P.M., J.T. and P.M.M., with input from all authors on survey design. E.A.N., E.L.P.M., S.S., J.T., H.K., T.S., A.C., G.D. and S.H. led data collection, and E.L.P.M. conducted data analyses. E.A.N. and E.L.P.M. wrote the first draft of the manuscript, and P.M.M. provided first revisions. E.A.N., E.L.P.M., S.S., S.H., J.T., A.C., T.S., N.M., G.D., H.K. and P.M.M. provided feedback and revisions on the manuscript, and approved the final version.
Funding
We acknowledge funding from the Western Australian Government Department of Jobs, Tourism, Science and Innovation (to S.H.) and the Western Australian Department of Health (to E.A.N. and P.M.M.). The first author (E.A.N.) was supported by a Curtin Research Fellowship. The funding bodies played no role in the design of the project, collection of data, analysis, interpretation of results or decision to publish.
Declaration of interest
None.












eLetters
No eLetters have been published for this article.