1. Introduction
Fairburn and colleagues have proposed a model suggesting that common mechanisms operate across all eating disorder (ED) diagnostic categories [Reference Fairburn, Cooper and Shafran1, Reference Fairburn, Cooper, Shafran and Fairburn2]. This transdiagnostic conceptualization aims to identify processes that are common across ED, with the ultimate aim of improving their clinical treatment. Due to the life-threatening potential of these disorders, the importance of developing effective treatment is a priority. Fairburn’s transdiagnostic approach, developed from traditional Cognitive Behavior Therapy, proceeds from the notion that all eating disorders have similar characteristics and underlying psychopathology reflected in analogous attitudes and behaviors [Reference Fairburn, Cooper and Shafran1]. In a number of clinical cases the diagnosis migrates from anorexia to bulimia or from bulimia to EDNOS [Reference Fairburn, Cooper, Shafran and Fairburn2]. The majority of eating disorder patients (over 50%) are originally diagnosed with EDNOS, which, before the development of the transdiagnostic model, was not covered in studies assessing the efficacy of eating disorder treatments. As a result, there were no specific recommendations for the management of people diagnosed with EDNOS [Reference Fairburn, Cooper, Shafran and Fairburn2].
Numerous interrelated factors have been implicated in the development of ED, and epidemiological studies have identified risk and protective factors common to these diseases [Reference Micali, De Stavola, Ploubidis, Simonoff, Treasure and Field3, Reference Westerberg-Jacobson, Edlund and Ghaderi4]. A comparison to distinguish overlapping and specific factors between various types of ED can be difficult because of discrepancies across study designs and samples, as well as diagnostic procedures and measures. Some of these shortcomings could be tackled by assessing specific features of different ED-related conditions within the same study. Although over the years research efforts have led to some evidence for the validity of a transdiagnostic cognitive-behavioral model of ED, only a few studies have examined this model in children and adolescent patients [Reference Decaluwé and Braet5–Reference Bailey, Parker, Colautti, Hart, Liu and Hetrick10].
EDs are increasing in prevalence with remarkable rapidity, affecting an ever larger part of the population. The age of onset of the disease is lower, with a worsening of the prognosis and the need for differential treatments; The male/female ratio has changed and the number of males is growing [Reference Robergeau, Jill and Silber11, Reference Treasure, Claudino and Zucker12].
Although “binge-eating” behaviors and compensatory behaviors (e.g., purging, fasting, excessive exercise) have a low prevalence in young patients [Reference Gowers, Crisp, Joughin and Bhat13, Reference Fisher, Schneider and Burns14], a “continuum” between BN and AN exists, with a frequent transition from one disorder to another [Reference Eddy, Dorer, Franko, Tahilani, Thompson-Brenner and Herzog15]. Some authors [Reference Lask16–Reference Peebles, Wilson and Lock18] agree in reporting an increased incidence among children exhibiting an ED of other psychiatric conditions such as depression, anxiety or obsessive-compulsive disorder in children with an ED [Reference Spindler and Milos19–Reference Hildebrandt, Bacow, Markella and Loeb21].
Despite the presence of neuropsychological disturbances in people with ED being known (e.g., ruminations and obsessions about weight, shape and eating), and personality traits such as perfectionism and impulsivity [Reference Bento, Pereira, Maia, Marques, Soares and Bos22, Reference Slof-Op't Landt, Claes and van Furth23], they are neglected/not included in the diagnostic criteria (e.g., fear of weight gain and a sense of lacking control) [Reference Wildes, Marcus, Crosby, Ringham, Dapelo and Gaskill24]. Most EDs emerge during adolescence, a period of brain reorganization [Reference Konrad, Firk and Uhlhaas25]; malnutrition, during this crucial period, can negatively affect illness trajectories. The biological findings in ED can be best understood as the result of disturbed eating behaviors, but other factors could be causally linked as risk and maintaining factors. All dominant models of the ED implicate personality variables in the emergence of weight concerns and the development of specific symptoms such as binge-eating and purging [Reference Treasure, Claudino and Zucker12].
In Fairburn’s transdiagnostic model, eating disorders are understood as cognitive problems [Reference Fairburn, Cooper, Doll, O'Connor, Bohn and Hawker26]. According to this approach, the underlying cause of all eating disorders is the same set of dysfunctional self-worth beliefs: the “core psychopathology” that involves the overestimation of body weight, appearance, and their control [Reference Fairburn, Cooper and Shafran1]. In eating disorder patients the sense of self-esteem is primarily determined by their weight, figure, and the ability to control them. Consequently, they engage in behaviors that reinforce core psychopathology [Reference Fairburn, Cooper, Doll, O'Connor, Bohn and Hawker26]. Moreover Fairburn identified other mechanisms that maintain core psychopathology, such as shape- and weight-checking (weighing oneself on a daily basis, comparing oneself with others) and/or shape- and weight avoidance (avoiding mirrors, swimming pools, and trying on clothes; never weighing oneself), interpreting each sensation or discomfort as “a sense of being fat, ” marginalization of activity in other life domains (social withdrawal), as well as preoccupation with thoughts about food, weight, and appearance. In addition, some patients display maintenance mechanisms typical of general psychopathology. These are clinical perfectionism, low self-esteem, and interpersonal difficulties [Reference Fairburn, Cooper and Shafran1]. These mechanisms do not necessarily occur in every patient and they do not always coincide in time with core psychopathology. These mechanisms do not automatically lead to eating disorders. The fundamental condition is that the individual has a set of dysfunctional convictions regarding the significance of weight and shape, and the priority of having them under control. The transdiagnostic therapy protocol was developed based on 30 years of experience, observation, and revision of the traditional cognitive behavioral approach by trial and error. CBT-E (Cognitive Behavior Therapy-Enhanced) was designed as individualized intervention involving modules selected and ordered according to a specific problem conceptualization developed together with the patient [Reference Fairburn, Cooper, Doll, O'Connor, Bohn and Hawker26]. The main goal of Cognitive Behavior Therapy in the transdiagnostic model is to improve patients’ quality of life by achieving a resolution of symptoms. Thus, the primary objective can be achieved by modifying the convictions about the importance of weight and shape, and having them under control. Beliefs can be modified directly, by replacing an earlier way of thinking with a new, more adaptive one or indirectly, by disrupting the mechanisms that maintain maladaptive thinking. Maintenance mechanisms are disrupted through the achievement of specific objectives, such as normalization of eating habits, decreased dietary restraint, elimination of the number of binge-eating episodes and compensatory behavior, giving up on weight and shape checking/avoidance, learning to deal with emotions in other ways than by eating, and becoming more active in other areas of life. In sum, the cognitive-behavioral transdiagnostic model proposes that a system of dysfunctional self-evaluation is fundamental to the maintenance of ED. Self-worth is defined in terms of control over eating, weight or shape that maintains the effort of dietary restraint. Inflexible dietary rules are difficult to maintain, and “binge-eating” behavior occurs when cognitive control over eating is squandered. Several mechanisms are responsible for ED maintenance: 1) Low self-esteem is proposed to motivate individuals to pursue achievement in the valued domain of weight and shape control to increase feelings of self-worth; 2) Clinical perfectionism, i.e., evaluation of the self in terms of achievement in the valued domain of eating, weight and shape, thereby increasing efforts of dietary restraint; 3) Interpersonal problems may lead to increased efforts of dietary restraint in an effort to achieve the perceived socially valued ideal; 4) Mood intolerance may encourage binge-eating and purging as a way to cope with the experience of intense states of distress and severe mood instability. The aforementioned model of ED suggests that whereas maintaining mechanisms may differ at the individual level, they do not differ at the diagnostic level [Reference Fairburn, Cooper, Shafran and Fairburn2, Reference Fairburn, Cooper, Doll, O'Connor, Bohn and Hawker26].
Standardized measures of personality traits generally confirm clinical descriptions of individuals with anorexia nervosa restrictive subtype (AN-R) as constricted, conforming, and obsessional individuals. Another picture suggesting affective instability and impulsivity has emerged from the assessment of subjects with BN. However, considerable heterogeneity exists within ED subtypes, and a number of special problems complicate the interpretation of data in this population. These include young age at onset, the influence of state variables such as depression and starvation sequelae, denial and distortion in self-report, and the instability of subtype diagnoses.
The present explorative research aimed to assess in a large multicenter transdiagnostic sample of patients with ED whether the cognitive behavioral transdiagnostic model would fit in young patients. The aim of the study was to determine the extent to which relationships within this model are equivalent between different ED diagnoses, testing the correlations between all the additional maintaining factors and core eating disorder maintaining mechanisms in AN, BN and EDNOS. Specifically, the descriptions of the behavioral and psychological traits are finalized to analyze a possible preliminary model of “spectrum” of ED in childhood and adolescence using the subtypes of the DSM-IV-TR diagnosis.
2. Methods
2.1. Study design and subjects
This research was based on a cross-sectional study of 419 children and adolescent patients (mean age 14.7 ± 2.14 years; age range 7–18 years; males 13.8%) at first admission or readmissions in six Italian Neuropsychiatry Units in 2013 with diagnosis of eating disorders (ED) according to the DSM–IV–TR criteria [27] adapted to childhood [Reference Bravender, Bryant-Waugh, Herzog, Katzman, Kriepe and Lask28]: anorexia nervosa (AN), bulimia nervosa (BN) and eating disorders not otherwise specified (EDNOS). Inclusion criteria were diagnosis of ED according to the, age between 7 and 18 years, and availability for participating in several psychological evaluation sessions. Exclusion criteria were a history of any type of personality or psychotic disorder, diagnosis of intellectual disability, medical pathology not correlated with the ED, significant general medical instability (e.g., severe hypotension or bradycardia, dehydration, electrolyte imbalance), presence or history of any communicative, learning or pervasive developmental disorders, a history of traumatic brain injury or any other neurological illness and substance or alcohol abuse or dependence during the preceding year. The recruitment period was 18 months. The considered subtypes of the DSM-IV-TR diagnosis were: anorexia nervosa restrictive subtype (AN-R), anorexia nervosa binge-purging (AN-BP), bulimia binge-purging (BN-BP), bulimia non purging (BN-NP), binge eating disorders (BED) and eating disorder not otherwise specified (EDNOS).
2.2. Clinical units
The clinical sites were selected on a geographic basis to account for different regional contexts not only in terms of the size of the ED epidemics, but also in terms of the socio-demographic, socioeconomic, and organizational ED care differences that can exist across regions. Moreover, the level of integration of services provided (outpatient, day hospital, residential care units, and hospitalization services), and excellent results regarding organizational requirements and performance were also considered. The clinical Italian centers participating in the study were: Eating Disorders Service for Children and Adolescents, San Paolo Hospital, Milan; Eating Disorders Service, Villa Miralago, Varese; Eating Disorders Services, ASL n. 1 ‘Palazzo Francisci’, Todi, Perugia; Eating Disorders Service, IRCSS Stella Maris Foundation; Regional Eating Disorders Service for Children and Adolescents, Policlinico S. Orsola Malpighi, Bologna; Eating Disorders Service ‘Fondazione Stella Maris Mediterraneo, “G. Gioia”, Chiaromonte, Potenza.
2.3. Ethical issues
The study was carried out according to the standards for good ethical practice of the Health Units involved, and was approved by the local ethical committee board of each clinical site. Written informed consent from a parent or guardian of each patient was obtained.
2.4. Measures
The constructs of the model were measured using standardized instruments. The dimensions that allowed assessment of key factors of ED diagnosis and core eating disorder mechanisms (dietary restraint and binge-eating) among children and adolescents were extrapolated from the questionnaires.
2.5. Standardized instruments
The standardized instruments that were used are the following:
a) Eating Disorder Inventory-3 (EDI-3) [Reference Garner29, Reference Clausen, Rosenvinge, Friborg and Rokkedal30].
b) Eating Disorder Examination, 12th edition (EDE 12.0D) [Reference Cooper and Fairburn31–Reference Berg, Peterson, Frazier and Crow34].
c) Youth Self-Report and Child Behavior Checklist (Self-Report and Parent-Report) [Reference Achenbach and Ruffle35, Reference Adambegan, Wagner, Nader, Fernandez-Aranda, Treasure and Karwautz36].
d) Child Adolescent Perfectionism Scale (CAPS) [Reference Hewitt and Flett37].
e) Body Uneasiness Test (BUT) [Reference De Panfilis, Rabbaglio, Rossi, Zita and Maggini38, Reference Cuzzolaro, Vetrone, Marano and Garfinkel39].
2.6. Indicator variables of the cognitive behavioral transdiagnostic model
2.6.1. Key factors
- Low self-esteem was measured using the “low self-esteem” EDI-3 scale. The EDI-3 low self-esteem scale assesses negative self-evaluation, cognitions of worthlessness, hopelessness and personal failure.
- Perfectionism was assessed using two scales: one from the EDI-3 perfectionism subscale and the other from the CAPS Self-Oriented Perfectionism scale.
- Interpersonal difficulties were measured using the EDI-3 “Interpersonal Problems” subscale, which assesses difficulty communicating feelings and developing intimate relationships with others, and social apprehension.
- Mood intolerance was assessed with the following: (i) EDI-3 “Affective problems” scale, which measures emotional dysregulation and interoceptive deficits (ii) and YSR “Anxious-depressed” subscale, which measures rapid changes in mood and poor emotional control. The anxious-depressed subscale used in this study was selected because it contained items measuring aspects of both anxiety and depression in childhood and adolescence.
- Overevaluation of weight and shape was assessed using three scales, one from the EDI-3, called “Body dissatisfaction”, the second from the BUT, “Body image concern”, and the third from EDE 12.0D “Shape concern”.
2.6.2. Core eating disorder mechanisms
- Dietary restraint was assessed using the EDE 12.0D “Restraint” scale
- Binge-eating was assessed using the EDI-3 “Bulimia” scale
Moreover, since many patients present both restriction behaviors and binge-eating, in order to better characterize the diagnostic groups, we created an index calculated via the relationship between the EDE subscale scores of “Bulimia” and that of “Restraint” (B/R Index = Bulimia + 1/Restraint + 1) in order to assess in the single subjects the prevalence of restraint or “binge-eating” behaviors.
2.7. Data recording
Patients and their parents completed all the psychological tests during the first few days of the clinical assessment. Physicians and psychologists collected data. The web-based research database was available for clinicians who accessed it online. The database was structured as an Electronic Health Record system (EHR) and it is intended to record clinical, psychosocial and behavioral information about the patient.
2.8. Statistical analysis
Collected data were related to demographic and physical characteristics and to the evaluation of specific behavioral and psychological traits. Data cleaning and checking preceded statistical analysis. All categorical data were described as number of subjects and percentage while continuous variables were presented as mean ± standard deviation, median, minimum and maximum values. In the case of categorical variables, the Pearson Chi-square test and the Fisher's exact test were used. In the case of continuous variables (test scores), the Kruskal Wallis nonparametric analysis of variance was used to evaluate significant differences between diagnoses. Multiple Comparisons between diagnoses were performed by the non-parametric Mann-Whitney U test for continuous variables and Fisher’s exact test for categorical variables. P-values adjusted for multiplicity were obtained by the Bonferroni method. Correlations among continuous variables were investigated by the nonparametric Spearman's rank correlation coefficient (Spearman's rho). All tests were two-tailed and a P < 0.05 was considered statistically significant.
Table 1 Demographic and maintaining factor characteristics by type of Eating Disorder.
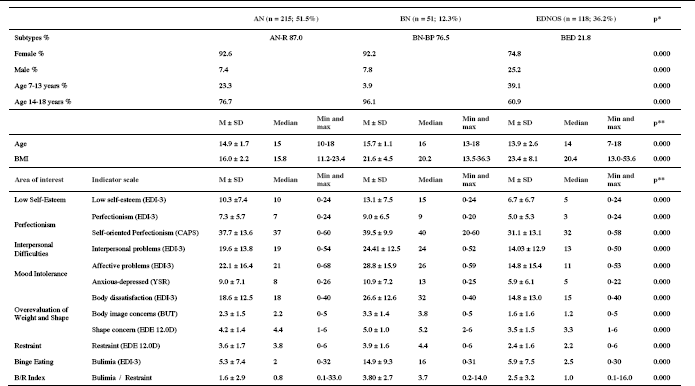
Table 2 Correlation between additional and core maintaining factors by type of Eating Disorder: Spearman’s Rho correlation coefficient.
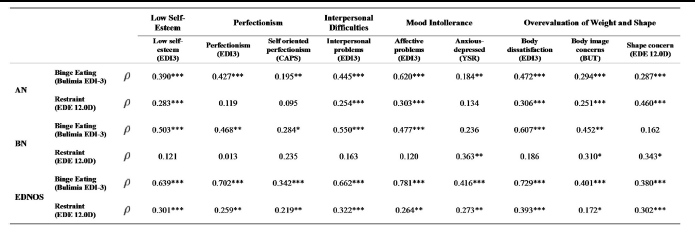

Fig. 1 Principal Component Analysis with diagnosis of Eating Disorders (AN, BN, EDNOS): projection of variables on the subspace of the first two principal components. The horizontal line is the Principal Component 1 while the vertical line is the Principal Component 2.
Table 3 Demographic and clinical characteristics by subtype of eating disorder.
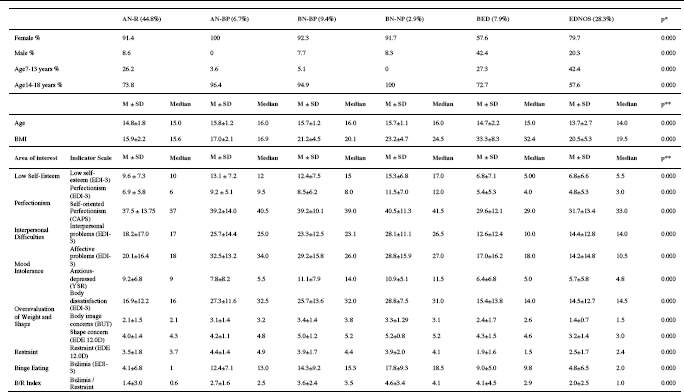
Note: AN, anorexia nervosa; BN-NP, bulimia nervosa non-purging type; EDNOS, eating disorder not otherwise specified; AN-R, Anorexia Nervosa Restrictive Type; BN-P, Bulimia Nervosa Purging Subtype; BED, Binge Eating Disorder; BMI, Body Mass Index; EDI-3, Eating Disorder Inventory 3; CAPS, Child and Adolescent Perfectionism Scale; YSR, Youth Self Report; BUT, Body Uneasiness Test; EDE 12.0D, Eating Disorder Examination Questionnaire; M, Mean; SD, standard deviation; p*, Pearson chi square, p **, Kruskal Wallis nonparametric test p.
Table 4 Principal component analysis for AN-R, AN-BP, BN-P, BN, BED, EDNOS: factor loadings for the first two rotated principal components.
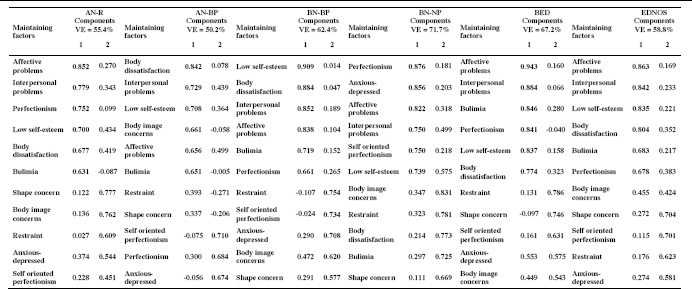
Note: principal component analysis based on correlation matrix; rotation method: Varimax with Kaiser normalization; VE = Variance Explained by the first two components; AN-R, anorexia nervosa restricting type; AN-BP, anorexia nervosa binge-purging type; BN-P, bulimia nervosa purging type; BN-NP, bulimia nervosa non-purging type; BED, binge eating disorder; EDNOS, eating disorder not otherwise specifie
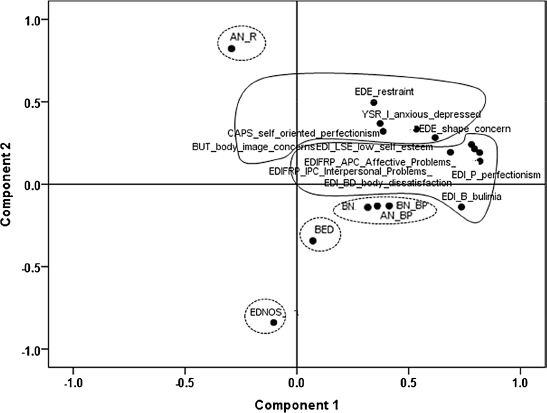
Fig. 2 Principal Component Analysis with diagnosis of Eating Disorders (AN-R, AN-BP, BN-BP, BN, BED, EDNOS): projection of variables on the subspace of the first two principal components. The horizontal line is the Principal Component 1 while the vertical line is the Principal Component 2.
A Principal Component Analysis (PCA), based on the correlation matrix and with rotated components by the Varimax method with Kaiser Normalization, was performed. PCA is a descriptive exploratory technique designed to analyze the pattern of relationships among all the variables included in the analysis. PCA aims to produce a small set of independent principal components from a larger set of related original variables. It is a technique used to bring out strong patterns in a dataset. It's often used to make data easy to explore and visualize. The results of a PCA are usually discussed in terms of component scores, sometimes called factor scores (the transformed variable values corresponding to a particular data point), and factor loadings (the weight of each standardized original variable on each principal component). Factor loadings represent the correlation between the original variables and the components, and are the key to understanding the underlying nature of a particular factor. PCA can supply the user with a lower-dimensional picture by using only few principal components, usually the first two components, so that the dimensionality of the transformed data is reduced. Variables are represented in terms of the distances between them in a low-dimensional space. The display of the variables in the final coordinate system, for example in the scatter plot of the first two components, provides an indication of the nature of the relationships between them. The interpretation in PCA is often based upon proximities between points in a low-dimensional map (i.e., two dimensions). The proximity between variables means that these tend to correlate together in the observations. All statistical analyses were performed by the SPSS statistical package, version 21.
3. Results
The final sample comprised 419 children and adolescents with ED. Of the sample, 73% were between 14 and 18 years old. The percentage of males aged between 7 and 13 years was 34%, while 26% of this younger age class were females. The contribution of each center to the study sample is the following: Eating Disorders Service for Children and Adolescents, San Paolo Hospital, Milan: 14, 6%; Eating Disorders Service, Villa Miralago, Varese: 5.5%; Eating Disorders Services, ASL n. 1 ‘Palazzo Francisci’, Todi: 22.4%; Eating Disorders Service, IRCSS Stella Maris Foundation, Pisa: 14.6%; Regional Eating Disorders Service for Children and Adolescents, Policlinico S. Orsola Malpighi, Bologna: 36.3%; Eating Disorders Service ‘Fondazione Stella Maris Mediterraneo, “G. Gioia”, Chiaromonte, Potenza: 6.7%.
3.1. Description of the results based on the three main diagnoses AN, BN and EDNOS
Table 1 shows that all the demographic, physical and indicator variables displayed significant differences by diagnosis.
Multiple comparisons showed no gender difference only between AN and BN and no BMI difference only between BN and EDNOS. Concerning the areas of interest variables, perfectionism (EDI-3), self-oriented perfectionism (CAPS), anxious-depressed (YSR) and restraint (EDE 12.0D) presented no significant difference in their mean values between AN and BN groups. Mean levels of “Bulimia” (EDI-3) were not different between AN and EDNOS. All the other comparisons resulted significant.
In Table 2, the correlations between core maintaining mechanisms (binge-eating and restraint) and the additional maintaining factors by type of Eating Disorder are reported.
Results of the PCA for the entire ED sample have shown that the first principal component was characterized by “Bulimia” and the second one by “Restraint”. In all ED and in each diagnostic subgroup, the first principal component was strongly and positively correlated with six of the original variables: “Bulimia”, perfectionism, body dissatisfaction, low self-esteem, interpersonal problems and affective problems. The second principal component was strongly and positively correlated with “Restraint”, shape concern, body image concern, self-oriented perfectionism, anxious-depressed mood. This suggests that the variables that define each principal component are strongly and positively correlated and vary together.
Fig. 1 shows the relationships between the examined variables in the subspace of the first two components for the entire ED: Two aggregations of variables were clearly distinguished: (1) “Bulimia”, perfectionism, body dissatisfaction, low self-esteem, interpersonal problems and affective problems; (2) “Restraint”, shape concern, body image concern, self-oriented perfectionism, anxious-depressed mood dimensions. Within each aggregation, variables with the highest correlations are represented. The scatter plot of the first two components included and highlighted the position of the three diagnoses with respect to all the maintaining factors variables. The AN group was particularly linked to restraint, and the BN group was particularly related to “Bulimia”. The EDNOS group appeared to be opposed to the AN group.
3.2. Description of the results based on the six diagnosis subtypes AN-R, AN-BP, BN-BP, BN-NP, BED and EDNOS
Multiple comparisons revealed gender differences between AN-R and BED, between AN-BP and BED and between BN-BP and BED (p < 0.05). In fact, the BED category contains the highest percentage of males of all groups (42.4%) and in AN-R, AN-BP and BN-BP the higher percentages of females (100% for AN-BP, 92.3% for BN-BP and 91.4% for AN-R). No differences in BMI were observed between AN-R and AN-BP (p = 0.150), between BN-BP and BN-NP, between BN-BP and EDNOS and between BN-NP and EDNOS (p > 0.05). Concerning age, multiple comparisons showed the following statistically significant differences (p < 0.05): AN-R vs. EDNOS, AN-BP vs. EDNOS and BN-BP vs. EDNOS.
Concerning variables related to the considered maintaining factors, there were no significant differences between AN-BP vs. BN-BP, between AN-BP vs. BN-NP or between BN-BP and BN-NP. BED and EDNOS presented significant different values only for shape concern and body image concerns (p < 0.05). Significant differences for a large number of indicator variables were observed for BN-BP vs. EDNOS, for AN-BP vs. EDNOS, for BN-NP vs. EDNOS and for AN-R vs. EDNOS. The indicator variables with less inter-diagnosis differences through multiple comparisons were anxious-depressed (YSR), perfectionism (EDI-3) and self-oriented perfectionism (CAPS); on the contrary, the variables with the higher number of inter-diagnosis differences were body dissatisfaction (EDI-3), restraint (EDE 12.0D) and low self-esteem.
To better characterize the six ED subtypes, an index calculated as rate between the “Bulimia” and the “Restraint” scores (B/R Index = Bulimia + 1/Restraint + 1) was used. A significant difference among the diagnostic groups was observed for this index (p < 0.001). Multiple comparisons showed significant differences between diagnostic subtypes (p < 0.05) with the exception of AN-BP vs. BN-BP; AN-BP vs. BN-NP; AN-BP vs. BED; BN-BP vs. BN-NP; BN-BP vs. BED; BNNP vs. BED, BED vs. EDNOS. This analysis evidenced a gradient in the index values, with a minimum in AN-R (1.4 ± 3.0) and a maximum in BNNP (4.6 ± 3.4) and BED (4.1 ± 4.5) (Table 3).
Differences in the correlations between indicator variables and the two core maintaining factors were observed among the six diagnoses. Correlation analysis results suggested that in AN-R the restraint indicator variable is related to shape concern (ρ = 0.461, p < 0.01), affective problems (ρ = 0.289, p < 0.01), body dissatisfaction (ρ = 0.286, p < 0.01), low self-esteem (ρ = 0.278, p < 0.01), interpersonal problems (ρ = 0.265, p < 0.01), body image concern (ρ = 0.223, p < 0.01), and anxious-depressed (ρ = 0.198, p < 0.01). In AN-BP, the binge-eating indicator variable is associated with body image concerns (ρ = 0.545, p < 0.01), body dissatisfaction (ρ = 0.457, p < 0.01), and affective problems (ρ = 0.444, < 0.05). In individuals with BN-BP, the binge-eating indicator variable is linked to body dissatisfaction (ρ = 0.606, p < 0.01), interpersonal problems (ρ = 0.558, p < 0.01), affective problems (ρ = 0.509, p < 0.01), low self-esteem (ρ = 0.482, p < 0.01), and perfectionism (ρ = 0.468, p < 0.01). In the same group of patients restraint is only correlated with the anxious-depressed indicator variable (ρ = 0.336, p < 0.05). In patients with BN-NP, binge-eating is related to body image concern (ρ = 0.768, p < 0.01), body dissatisfaction (ρ = 0.722, p < 0.01), low self-esteem (ρ = 0.632, p < 0.05), and interpersonal problems (ρ = 0.592, p < 0.05). In BED, binge-eating is strongly correlated with affective problems (ρ = 0.931, p < 0.01), body dissatisfaction (ρ = 0.852, p < 0.01), interpersonal difficulties (ρ = 0.819, p < 0.01), perfectionism (ρ = 0.785, p < 0.01), and low self-esteem (ρ = 0.759, p < 0.01). In EDNOS, binge-eating is particularly correlated with affective problems (ρ = 0.727, p < 0.01) and restraint is mainly related to body dissatisfaction (ρ = 0.408, p < 0.01), shape concern (ρ = 0.374, p < 0.01), and interpersonal problems (ρ = 0.370, p < 0.01).
A PCA was performed in order to explore the relationship between the core and additional maintaining factors in ED. The rotated principal components matrix of the first two components is presented in Table 4. This table shows the rotated principal components matrix for each of the six ED diagnoses as well as the total variation accounted for the first two principal components. For nearly all diagnoses, with the exception of BN-NP and AN-BP, the first principal component was related to “Bulimia” and the second to “Restraint”, showing the independence of the two variables. On the contrary, in BN-NP “Restraint” and “Bulimia” were positively correlated in the second component, while in AN-BP restraint was not clearly associated with any of the two principal components. For AN-R, BN-BP, BED and EDNOS, the first principal component was usually correlated with “Bulimia”, perfectionism, body dissatisfaction, low self-esteem, interpersonal problems and affective problems scores; while the second principal component was usually correlated with “Restraint”, shape concern, body image concern, self-oriented perfectionism, and anxious-depressed dimensions. However, anxious-depressed and body image concerns did not show a specific relationship with one of the two components in BED, because of their relationship with both components. A similar condition was observed for body image concerns in EDNOS. Results seemed to indicate an incomplete adherence to the transdiagnostic model. In fact, the relationships between the several analyzed aspects were not the same in every subgroup; however, such differences were observed in particular in the two subgroups with the lower sample size (AN-BP = 28 patients and BN-NP = 12 patients).
To complete the analysis we produced a PCA including the diagnosis variable (AN-R, AN-BP, BN-BP, BN-NP, BED and EDNOS). The scatter plot of the first two components is shown in Fig. 2, which includes and highlights the position of the six diagnoses with respect to all the maintaining factor indicator variables. AN-R group, particularly related to “Restraint”, shape concerns and anxious-depressed aspects, was not linked to AN-BP, BN-BP and BN-NP groups, which seemed to constitute an unique cluster, particularly related to “Bulimia”, affective and interpersonal problems and perfectionism. The EDNOS group appear to be opposed to the AN-R group, whereas the BED group seemed to be independent from the others.
4. Discussion
4.1. Summary of the main findings
In this study, a mixture of transdiagnostic and disorder-specific processes was implicated in the maintenance of ED in 419 Italian children and adolescents; specifically, the behavioral variables (restraint and binge-eating) acted as poles of attraction of the other variables, configuring a general design closed to the transdiagnostic model. However, the ED diagnoses continue to have a role in discriminating the correlations between variables in different patient groups. In our sample, all the inter-correlations between the variables considered were positive and highly significant. In particular, the correlation analysis suggested that low self-esteem, perfectionism, interpersonal difficulties, mood intolerance and overevaluation of weight and shape processes were all strongly related to the core maintaining factor “Bulimia” and “Restraint”. Moreover, over-evaluation of weight and shape, mood intolerance and interpersonal problems resulted important areas of concern in the correlations with the central mechanisms of disorders, also in the stratified analyses by diagnosis. At the same time, some differences between the variable relations in each diagnostic group were observed.
For each diagnosis, the first principal component was strongly and positively correlated with “Bulimia”, perfectionism, body dissatisfaction, low self-esteem, interpersonal problems and affective problem scores; meanwhile, the second principal component was strongly and positively correlated with “Restraint”, shape concern, body image concern, self-oriented perfectionism and anxious-depressed dimensions. The PCA including the diagnosis variable was produced and highlighted the position of the three diagnoses with respect to all the maintaining factor variables. The AN group was particularly linked to restraint and the BN group was particularly related to “Bulimia”. The EDNOS group appeared to be opposed to the AN group.
Concerning variables related to the considered maintaining factors, there were no significant differences between AN-BP and BN-BP, AN-BP and BN-NP or BN-BP and BN-NP, indicating these three subtypes as a very homogeneous subgroup.
A significant difference between the diagnostic groups was observed for the index calculated as rate between the “Bulimia” and the “Restraint” scores and this analysis evidenced a gradient in the index values, with a minimum in AN-R and a maximum in BN-NP and BED (4.1 ± 4.5). In this context it would be possible to argue in favor of a specific sequence in these behavioral characteristics that could be considered in agreement with Brooks and colleagues [Reference Brooks, Rask-Andersen, Benedict and Schiöth40] that outlined an impulse-control “spectrum” model of ED is suggested, providing evidence to support a single neural model across a continuum of restricted vs. impulsive behavior.
Differences in the correlations between indicator variables and the two core maintaining factors were observed among the six diagnoses. In this case, it is possible to observe the presence of a kind of gradient for which the relationships between preeminent behavioral factors for diagnosis and additional maintenance factors are overall very strong in BN-NP and weaker in AN-R.
PCA indicated for all diagnoses (with the exception of BN-NP and AN-BP) that the first principal component was related to “Bulimia” and the second to “Restraint”, showing the independence of the two variables. On the contrary, in BN-NP “Restraint” and “Bulimia” were positively correlated in the second component, while in the AN-BP group, “Restraint” was not clearly associated with any of the two principal components. PCA including the diagnosis variable highlights the position of the six diagnoses with respect to all the maintaining factor indicator variables.
Tailoring interventions to clinically relevant subtypes could be a strategy for improving treatment response. The current study contributes to and extends existing research documenting the validity of personality subtypes in individuals with ED. Using PCA, we identified the following four subtype clusters:
1) AN-R
2) AN-BP, BN-BP, BN-NP
3) BED
4) EDNOS
The cluster constituted by AN-BP, BN-NP and BN-BP, characterized by emotion dysregulation and low self-esteem, is the one with the strongest correlations with all the variables considered. This could be due to the fact that this model was originally developed through the analysis of patients diagnosed with bulimia nervosa and further extended to the entire group of ED patients [Reference Fairburn, Cooper and Shafran1, Reference Lundgren, Danoff-Burg and Anderson41].
4.2. How the findings are related to previous research
A failure to recognize clinically relevant subtypes in ED may hinder treatment research if the interventions studied target a heterogeneous population. An approach to identifying clinically relevant subtypes is to focus on comorbid psychopathology. For example, there is increasing interest in the utility of subtyping individuals with ED based on patterns of within-group heterogeneity in personality psychopathology [Reference Wildes, Marcus, Crosby, Ringham, Dapelo and Gaskill24].
Moreover, research has found differences among these subtypes in patterns of Axis I and II comorbidity, family history of psychopathology, rates of childhood abuse, and psychosocial functioning [Reference Steiger, Richardson, Schmitz, Israel, Bruce and Gauvin42]. Patients with ED could also be meaningfully grouped on the base of perfectionism and impulsivity. The use of dimensional features may enable the identification of fundamental underlying mechanisms, and provide insight into mechanisms that may drive or maintain disordered eating [Reference Slof-Op't Landt, Claes and van Furth23].
In this study several relationships resulted transdiagnostic and similar across diagnoses, including the relationships between low self-esteem and overevaluation of weight and shape, and affective problems and binge-eating as previously reported by Lampard and colleagues [Reference Lampard, Tasca, Balfour and Bissada43]. Overevaluation of weight and shape was associated with dietary restraint across diagnoses but not in BN patients and with different values of the correlation and this is not completely congruent with Lampard’s research [Reference Lampard, Tasca, Balfour and Bissada43].
Low self-esteem is a particularly problematic issue in eating-disordered adult individuals because it often persists after remission of the ED [Reference Daley, Jimerson, Heatherton, Metzger and Wolfe44]. In the present analyses in children and an adolescent population, this issue could be important in maintaining the ED; in particular, it is positively correlated with “Bulimia”, perfectionism, body dissatisfaction, interpersonal problems and affective problems scores. Moreover, it appears that difficulty in regulating emotion is associated with binge-eating (“Bulimia” subscale). Treatment interventions to improve emotion regulation skills related to affective instability may be relevant for all ED diagnoses, primarily when binge-eating is present.
The cognitive-behavioral model proposes that dietary restraint maintains binge-eating. This positive relationship was supported in EDNOS, but not AN or BN. This result in BN is similar to previous studies, which failed to find a positive relationship between dietary restraint and binge-eating in samples of patients seeking treatment for BN or atypical BN [Reference Lampard, Byrne, McLean and Fursland45, Reference Lowe, Thomas, Safer and Butryn46].
Of note, our findings suggest that compared to AN-R patients, individuals with AN-BP, BN-BP and BN-NP are characterized by emotional dysregulation and low self-esteem, and had a stronger correlation with almost all the variables included in the analysis. These findings could converge with previous work, which suggests that a classification scheme based on comorbid specific personality psychopathology may have more clinical utility than current approaches to conceptualizing ED [Reference Westen and Harnden-Fischer47]. A trait-based approach to conceptualizing personality psychopathology is consistent with proposed revisions to the classification of personality disorders in DSM-5 [48]. The BED category and EDNOS category revealed different and specific features in the analyzed areas. Thus, subtyping individuals may be useful across diagnostic categories as a means of identifying clinically relevant subgroups. According to this view, a study examining brain activation associated with response inhibition in adolescents with ED identified differences in neural function between AN-R, AN-BP, and healthy controls [Reference Lock, Garrett, Beenhakker and Reiss49]. Therefore, at least during adolescence, ED subtypes may be distinguishable in terms of neural correlates of inhibitory control.
4.3. How the findings reflect on theory
A consistent picture suggesting affective instability and impulsivity has emerged from the assessment of subjects with bulimia nervosa. Brooks and colleagues outlined a novel evidence-based impulse-control “spectrum” model of ED [Reference Brooks, Rask-Andersen, Benedict and Schiöth40]. A model of ED was proposed that coincides with contemporary suggestions by clinicians and the proposed changes due to be published in the DSM-5. The review summarized evidence supporting a neural model of ED across a continuum of restricted vs. impulsive behavior. They proposed that neuroimaging data of people with ED provide convincing evidence that supports a single impulse-control “spectrum” model of ED. Specifically, a dysregulation of striatal dopaminergic circuits, combined with varying degrees of prefrontal cortex (PFC) related cognitive control contribute to the differential pathologies observed in AN, BN and BED. In addition, genetic data suggests potential polymorphisms for ED in the genes encoding BDNF, COMT and 5HT2A, the interactions between which may contribute to a “spectrum” of disordered eating [Reference El-Hage, Phillips, Radua, Gohier, Zelaya and Collier50–Reference Stice, Spoor, Bohon, Veldhuizen and Small53]. For each diagnosis in our sample, the first two main components consisted of the same indicator variables as in the overall analysis; the first component was strongly and positively correlated with “Bulimia” (impulsive eating behavior), perfectionism, body dissatisfaction, low self-esteem, interpersonal problems and affective problems scores; while the second main component was strongly and positively correlated with “Restraint” (restricted eating behavior), shape concern, body image concern, self-oriented perfectionism, and anxious-depressed affect.
4.4. Limitations of the study
The findings of the current exploratory study need to be considered in the light of several limitations. The first is the low sample size, especially regarding some subtypes; differences in PCA were observed mainly in the two subgroups with the lower sample size (AN-BP = 28 patients and BN-NP = 12 patients). Moreover, this study did not evaluate maintaining factors prospectively, and since the data reported were cross-sectional, conclusions about a possible direction of relationships in the model cannot be formulated. Given the cross-sectional nature of the analyses, it is not possible to actually describe either the ‘core mechanisms' or the ‘additional factors' as maintaining.
Assessing the diagnostic categorization of ED is made difficult by their low diagnostic reliability and also by the frequency of concurrent disorders [Reference Hiller, Dichtl, Hecht, Hundt and von Zerssen54]. In addition, ED diagnoses in this study were determined in accordance with DSM-IV-TR criteria; these criteria were revised in DSM-5. DSM-5 maintained a distinction between AN and BN, but altered the diagnostic criteria so that some patients diagnosed with EDNOS (particularly subthreshold AN and BN) would be currently classified as AN or BN. Information about how changes in the criteria might affect knowledge of complications, course, and treatment response is paramount. For the forthcoming research on this population of children and adolescents it would be interesting to see how the transition to the new diagnostic system changes the prevalence of disease for each diagnosis and how the new groupings fit the transdiagnostic model of maintenance factors [Reference Dalle Grave, Calugi and Marchesini55–Reference Ornstein, Rosen, Mammel, Callahan, Forman and Jay58].
4.5. Main conclusions
By providing one of the first tests of the transdiagnostic nature of relationships between additional maintaining factors and core ED maintaining mechanisms in children and adolescents, this study identified several associations between ED mechanisms that are common across all ED diagnoses. However, the results of this study also point toward disorder-specific maintenance processes. Results suggest that the relationship between maintaining mechanisms and eating disorder symptoms may differ. If this is the case, a distinction should be maintained between ED diagnostic groups, particularly AN and BN.
Finally, at the same time, low self-esteem, overevaluation of weight and shape, mood intolerance and perfectionism were associated with core ED symptoms in all ED diagnostic groups, indicating that these may be effective targets for ED prevention and intervention programs.
In sum, it is important to note that transdiagnostic approaches and disorder-focused approaches need not be mutually exclusive [Reference Mansell, Harvey, Watkins and Shafran59] and that a “spectrum” model based on an impulse-control paradigm of ED [Reference Brooks, Rask-Andersen, Benedict and Schiöth40] can be informative. With different intensity grades in the maintenance of any given ED, the current study suggests that all processes identified in the cognitive-behavioral model of ED may be operating across ED diagnoses.
The starvation of AN can lead to binge-eating followed by purging as a compensatory behavior, and EDNOS is largely a hybrid, comprised mostly of patients who do not quite meet the diagnostic criteria for AN or BN. The danger of grouping all ED patients together would also be that the morbidity and mortality will be homogenized, resulting in a reduction in the apparent significance of AN. This could lead to a decrease in treatment for ED, especially for those patients with AN. At the same time, if a completely transdiagnostic theory of ED was accepted, it would be impossible to draw historical comparisons, compare treatment efficacy to historical controls, or estimate sample size for clinical trials [Reference Rounsaville, Alarcon, Andrews, Jackson, Kendell, Kendler, Kupfer, First and Regier60]. Maintaining AN and BN as separate diagnoses could allow us to compare epidemiology and treatment interventions over time: conversely, a change in categorization would render it impossible. Moreover, it might be useful to consider whether other dichotomies, such as mild and severe or acute and chronic, might be a more practical way to classify EDs [Reference Maguire, Le Grange, Surgenor, Marks, Lacey and Touyz61]. Comparing males with females, different ages of onset or precipitating factors, or experimentally different groups, may help reveal the causal pathways of ED in further research.
In conclusion, this study supports both shared and specific cognitive, behavioral, and social characteristics across various types of ED, suggesting the importance of considering both the transdiagnostic approach and the unique features of each ED subtypes in the evolutive age. Future research is needed to identify the mechanisms responsible for differential treatment response among personality subtypes in ED. Therefore, in the light of these findings it would be important to learn how to take action on specific cognitive variables, on meta-cognitive and meta-emotional processes, and primarily to implement techniques to affect the specific maintenance factors of the symptoms. Research could help increase the number of ED patients who benefit from a good diagnostic classification and a tailored treatment in order to decrease the personal and societal costs of such debilitating conditions.
Ethical statements
In the present manuscript all studies have been approved by the appropriate ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Fundings
This research was supported by the Italian Ministry of Health, National Centre for Disease Prevention and Control, CCM, Prevention and Communication Department (Italy).
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
The Working Group of the National Research Project on Eating Disorders: “Predictive factors and psychopathological dimensions related to childhood and adolescent eating disorders”
Dr. Teresa Di Fiandra: Scientific representative, Ministry of Health, Prevention and Communication Department, Italy
Dr. Laura Dalla Ragione: Scientific manager and Regional Eating Disorders Services manager, Umbria, Italy
Dr. Lucia Giombini: Project Manager
Dr. Olivia Curzio, Dr. Michele De Nes, Dr Loredana Fortunato, Dr. Emanuela Colasante, Dr. Sabrina Molinaro: Web based research database, data quality controls before statistical analysis, Institute of Clinical Physiology (IFC), National Research Council of Italy (CNR), Pisa, Italy
The eating disorders services involved offer multidisciplinary treatment for children and adolescents in outpatient, day-hospital and inpatient settings
Dr. Alessandro Albizzati, Dr. Fortunata Cantini, Dr. Francesca Emanuelli – Eating Disorders Service for Children and Adolescents, San Paolo Hospital, Milan, Italy
Dr. Annabella Pozzoli, Dr. Federico Fortunato – Eating Disorders Service, Villa Miralago, Varese, Italy
Dr. Laura Dalla Ragione, Dr. Giovanni Antonelli, Dr. Lucia Giombini – Eating Disorders Services, ASL n. 1 ‘Palazzo Francisci’, Todi, Italy
Dr. Sandra Maestro, Dr. Filippo Muratori, Dr. Silvia Scardigli, Dr. Sara Calderoni, Dr. Elena Brunori, Dr. Francesca Ditaranto, Dr. Diana Bottai – Eating Disorders Service, Fondazione Stella Maris (IRCSS), Pisa, Italy
Dr. Emilio Franzoni, Dr. Luisa Iero – Regional Eating Disorders Service for Children and Adolescents, Policlinico S. Orsola Malpighi, Bologna, Italy
Dr. Rosa Trabace, Dr. Antonella Muscolino – Eating Disorders Service ‘Fondazione Stella Maris Mediterraneo, “G. Gioia”, Chiaromonte, Italy
Acknowledgments
The authors thank Professor Bryan Lask for his generous advice and encouragement. We thank the Istituto Di Ricovero e Cura a Carattere Scientifico Stella Maris and the Institute of Clinical Physiology of the Italian National Research Council for supporting the project. Assistance provided by Doctor Dario Menicagli, University of Pisa, was greatly appreciated. Our gratitude is also extended to Professor David Cohen, Department of Child and Adolescent Psychiatry at La Salpêtrière hospital in Paris, for his reading the manuscript and providing us with significant and constructive suggestions. Alison Frank edited the English version before submission.









Comments
No Comments have been published for this article.