Body fat proportion (%BF) is a major issue in health. Recent studies estimate that 23·2 % of the world's adult population is pre-obese and 9·8 % is obese(Reference Kelly, Yang and Chen1). In Europe, this figure is even higher. According to the WHO(2), over 50 % of the European adult population is pre-obese or obese. The use of skinfold thickness measurement to evaluate regional and body distribution of subcutaneous adipose tissue and to predict body fat has become one of the most widely used anthropometric techniques in nutritional status and body composition assessment(Reference Jackson, Ellis and McFarlin3). It is based on the two-compartment model which divides the body into fat mass and fat-free mass(Reference Lee, Nieman and Lee4). Other, more sophisticated methods for estimating body fat, namely dual-energy X-ray absorptiometry (DXA), are not convenient for large-scale field studies or for routine practice(Reference Heymsfield, Lohman, Wong and Heymsfield5), as the equipment is expensive and not portable.
The skinfold thickness technique is a highly informative, non-invasive, portable and inexpensive bedside and field method to determine body fat. However, the different types of skinfold calliper available present some limitations that make them unattractive and perhaps less used in daily practice. Some models, recognised in the specialised literature, have a rotating needle over an analogue scale which makes measurement difficult during the established measuring time interval of 2–4 s(Reference Lee, Nieman and Lee4) after pressuring the tissue, according to the designed modus operandi. The technical procedure can be compromised by the reading of the needle position as well as the subjectivity associated with the mental counting of the pre-defined time interval. In addition, because measurement values need to be manually annotated in those available models, the evaluation procedure is frequently interrupted, therefore it becomes more time consuming or requires a second technician to annotate the data. In any case, both solutions have intrinsic error sources.
To predict body density and %BF, regression equations are required after the skinfold thickness measurement. In fact, the large number of equations available requires the selection of the most appropriate, based on its validity within the population under study(Reference Bemben, Massey and Bemben6). These calculations are an additional task, which make the assessment of body fat even more difficult and time consuming.
Therefore, the development of a new, more accurate instrumentation for %BF determination using skinfold thickness measurement, which also has data-recording capacity, is currently required. The purpose of the present study was to evaluate the accuracy and the functionality of a new digital skinfold system, the Liposoft 2008+Adipsmeter V0 (LA), for measuring skinfold thickness and determining body fat proportion.
Methods
Subjects and design
The LA system comprises of a modified Harpenden (H) calliper with digital skinfold thickness-reading capacity (Adipsmeter V1.0) incorporating wireless transmission for a software application (Liposoft 2008) and predictive equations for the body density and the %BF calculation(Reference Restivo, Amaral and Mendes7).
An automatic measurement of skinfold thickness was achieved using a traditional H calliper (the most recommended calliper to be used)(Reference Fidanza8, Reference Marfell-Jones, Olds and Stewart9) and integrating digital sensorisation and wireless communication capabilities with a LabVIEW software application. This application follows the recommended skinfold measurement protocol(Reference Lee, Nieman and Lee4, Reference Fidanza8, Reference Jelliffe, Jelliffe, Zerfas and Jelliffe10, Reference Norton and Olds11).
To obtain these new features, slight mechanical changes were introduced. The old dial mechanical indicator was replaced by a simple, inexpensive and linear miniaturised encoder easily interfaced with a computer, for a contactless skinfold thickness measurement. The wireless communication is based on ZigBee technology. The wireless receiver used for communication with any personal computer is of universal serial bus type. The system is inexpensive, has 9 h of autonomy and can be easily recharged.
The information acquired is digitally recorded in a system-integrated database and could be used later for following up individual progress. The common anthropometrist reading errors due to measurement with a moving needle in front of an analogue scale within a mental time interval counting are eliminated. So, the automatic measurement system is not so demanding and requires less of a technician's skills and time.
Right after performing the skinfold thickness measurement, the technician can choose the appropriate body density and %BF predictive equation and promptly determine the %BF. The system offers an intuitive route through the procedure using an established sequence(Reference Fidanza8–Reference Jelliffe, Jelliffe, Zerfas and Jelliffe10). The LA application data recording process permits visual graphic inspection during measurement and so it helps to control the measurement quality, namely the differences between measurements. In fact, any skinfold thickness measurement considered unreliable by the technician can be erased and a new measurement can be performed. The LA integration of a database system allows the recording and continuous updating of data for each individual. Finally, if desired, it is possible to print a test report and to export the test data.
The accuracy of skinfold thickness measurements, carried out by the LA, was compared with those obtained with a non-modified H calliper, from two samples of adults and older adults in a university-based cross-sectional study. A comparison was also conducted between estimated and DXA-%BF.
The adult sample had forty-five individuals, recruited on a voluntary basis within some faculties from the University of Porto. The older adult sample comprised fifty-six individuals engaged in an exercise programme at the Physical Activity, Health and Leisure Research Centre of the Sports Faculty – University of Porto. The study was conducted according to the guidelines laid down in the Declaration of Helsinki(12). All the participants were informed of the study purposes as well as the different procedures. Verbal informed consent from all the subjects was witnessed and formally recorded.
Data collection
Skinfolds were measured with the LA and with an H calliper with similar resolutions, in a random order. Measurements were taken along the right side of the body and for three consecutive times with each calliper, according to the International Standards for Anthropometric Assessment recommendations(Reference Marfell-Jones, Olds and Stewart9), using triceps, subscapular, biceps, iliac crest and front thigh sites. Height (m) was measured with the individuals barefooted, using a stadiometer (Seca 708; Seca Limited, Birmingham, UK), with a resolution of 0·001 m(Reference Lee, Nieman and Lee4). Body mass (kg) was measured by a scale (Seca) (resolution of 0·1 kg) with the individuals barefooted and wearing light clothes(Reference Lee, Nieman and Lee4). All the measurements were obtained at the same visit.
Reference %BF was evaluated in a three-compartment model with DXA equipment (Hologic QDR-4500). Body composition was estimated by QDR Software for Windows XP, version 12.4 (Hologic, Inc., Bedford, MA, USA). All scans were performed by the same technician using standard procedures as described in the Hologic Users Manual. Complete body DXA scans were made with a scan time of approximately 8 min. The %BF determined by the system represents (fat mass (g)/total mass (g) × 100) (DXA-%BF). Both the callipers and the DXA were previously calibrated.
Data analysis
For the adult sample, %BF derived from skinfold measurement with the LA system and the H calliper was calculated using the Peterson et al. (Reference Peterson, Czerwinski and Siervogel13) equation (Peterson-%BF), developed and validated with a four-compartment model.
The %BF of the older adult sample was predicted with the body density Visser et al. (Reference Visser, van den Heuvel and Deurenberg14) regression equation and transformed into %BF with the Brozek formula(Reference Brozek, Grande and Anderson15) (Visser-%BF), which were both developed and validated against a two-compartment model. The mean values of DXA-%BF were compared with Coin et al. (Reference Coin, Sergi and Minicuci16) reference values, according to sex and age.
Means and standard deviations were calculated for the quantitative and continua variables. The normal distribution of the variables was tested using the Kolmogorov–Smirnov test. Association between the skinfold measurements from the LA system and H callipers was evaluated by Pearson's correlation coefficients (r). Association between the Visser-%BF and Peterson-%BF (either using the LA system or H callipers) with DXA-%BF was evaluated by Pearson's or Spearman's correlation coefficients (r) considering the normality of data distribution.
The mean and sd of the differences in skinfold thickness measurement between the LA system and those obtained with H callipers were calculated as LA minus H. The same calculations were conducted for the %BF obtained by the LA system and H equipment and by the appropriated equations. Mean difference and the sd of the differences between the DXA-%BF and %BF estimated from both skinfold measurement equipments were also calculated. The differences were compared using the paired-samples t test or Wilcoxon test, according to the data distribution.
A Bland & Altman plot(Reference Bland and Altman17) for difference against mean for all skinfold thickness measurements from the LA system and H callipers was used to compare the accuracy and level of agreement for the skinfolds thickness measured by both methods. A second Bland and Altman plot for the comparison of the accuracy and level of agreement of the LA and H system for the %BF estimates was also prepared.
Total error between Peterson-%BF and Visser-%BF towards DXA-%BF was also calculated(Reference Heymsfield, Lohman, Wong and Heymsfield5):
where Y 1 is the predicted value, Y 2 is the actual value and n is the number of paired observations.
The adopted level of statistical significance was P = 0·05. The significance levels quoted are two sided. All the statistical analyses were carried out using the Software Package for Social Sciences for Windows, version 14.0 (SPSS, Inc., Chicago, IL, USA).
Results
Descriptive statistics of the adults and older adult samples are presented in Table 1, showing that these two groups are heterogeneous regarding the studied characteristics. The results show that the majority of skinfolds thickness obtained by the LA system are similar to those obtained with H callipers. The estimation of %BF from DXA, the LA system and H measurement converted in %BF by regression equations is also presented in Table 1. The DXA-%BF value was within the tabled body fat reference values for adult women and older sample, while it was slightly higher for the adult men(Reference Coin, Sergi and Minicuci16).
Table 1 Characteristics of the samples
(Mean values and standard deviations)

LA, Liposoft 2008+Adipsmeter V0; BF, body fat; DXA, dual-energy X-ray absorptiometry.
* %BF obtained from LA system and Harpenden skinfolds measurement and equations: Peterson et al. (Reference Peterson, Czerwinski and Siervogel13) equation for the adult sample and Visser et al. (Reference Visser, van den Heuvel and Deurenberg14) and Brozek et al. (Reference Brozek, Grande and Anderson15) for the older adult sample.
Means and sd for skinfolds and %BF differences between the LA system and H callipers are displayed in Table 2, stratified by sex and age groups. The mean differences for skinfolds thickness are small; all are lower than − 0·86 mm with a sd of < 2·80 mm. The sd of skinfolds thickness differences are slightly higher for skinfolds measured in females than for males, except for the iliac crest skinfold in the adult women group. The sd of these differences are also slightly higher for older women than for the adult women. Concerning the mean %BF differences, the results show that LA values are similar to those obtained with H callipers. The mean differences are small, under − 0·24 %, with a very low sd, below 0·81 % BF (Table 2).
Table 2 Skinfolds and percentage body fat differences between the Liposoft 2008+Adipsmeter V0 (LA) system and Harpenden (H) callipers*
(Mean values and standard deviations)
* Differences were calculated as LA minus H.
Bland & Altman plots(Reference Bland and Altman17) for difference against mean for all skinfold thickness measurements and also for %BF, from the LA system and H callipers (Figs. 1 and 2), show that both skinfolds and calculated %BF obtained with the LA system and H callipers are in high agreement, revealing the accuracy of the LA system.
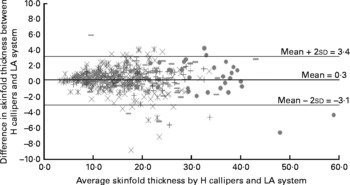
Fig. 1 Bland and Altman plot for difference against mean for skinfold thickness measurements (mm) from the Liposoft 2008+Adipsmeter V0 (LA) and Harpenden (H) callipers.+, Triceps; ![]() , biceps; –, subscapular; × , iliac crest;
, biceps; –, subscapular; × , iliac crest; ![]() , front tight.
, front tight.

Fig. 2 Bland and Altman plot for difference against mean for % body fat estimate from the Liposoft 2008+Adipsmeter V0 (LA) and Harpenden (H) callipers. ![]() , Adults;
, Adults; ![]() , older adults.
, older adults.
For the skinfold thickness measurement with the LA system and H callipers (Fig. 1), the dispersion of values is uniform with a slight rise when skinfolds thickness increases. The mean value for the difference between the two instruments is very low, 0·3 mm, with small limits of agreement between the measurements ( − 3·1 to 3·4 mm). A strong association was found between measurements from the LA system and H callipers; correlation coefficients for each measured skinfold thickness were all above r 0·91 (P < 0·001).
The difference against mean for %BF estimates from the LA system and H measurement and equations (Fig. 2) also shows that %BF estimated by both methods are in high agreement, confirming the accuracy of the LA system. For the adult sample, the dispersion of values is uniform with a slight decrease when skinfolds thickness measurements increase. For the older adult sample, the opposite is observed. The mean value for the difference between the %BF from the two instruments is very low, 0·2 %, with small limits of agreement between measurement ( − 0·8 to 1·2 %). Percentage BF predicted by the LA system and H callipers is strongly correlated in the adult group (r 0·99, P = 0·01) and the same was observed for the older adult group (r 0·98, P = 0·01).
Considering the DXA-%BF as the criterion, the new digital system instrumentation LA leads to a similar approximation in the %BF evaluation for adults and older adults, in relation to the traditional H skinfold calliper (Table 3). The total error between DXA-%BF and Peterson-%BF was equal to 3·1 % for skinfold measurement carried out with the LA system and equal to 3·4 % using the H calliper for the adult sample. For the older group, the total error between DXA-%BF and LA Visser-%BF was equal to 5·2 % and between DXA-%BF and H Visser-%BF was equal to 5·4 % (Table 3).
Table 3 Body fat (%) differences and total error between Liposoft 2008+Adipsmeter V0 (LA) system, Harpenden (H) callipers and dual-energy X-ray absorptiometry (DXA)
(Mean values and standard deviations)
%BF, %body fat.
Mean values were significantly different: *P < 0·05, **P < 0·001.
† Calculated by using paired-samples t test for adult data and Wilcoxon test for older adult data (two sided).
A strong correlation coefficient was found between DXA-%BF, LA Peterson-%BF (r 0·95, P = 0·01) and H Peterson-%BF (r 0·94, P = 0·01). Despite this high association, results showed significant differences between the mean value from DXA-%BF and from Peterson-%BF for both sexes (P < 0·05) (Table 3). Strong associations were also found between DXA-%BF and Visser-%BF from the LA system (r 0·90, P = 0·01) and H callipers (r 0·90, P = 0·01). The mean DXA-%BF was significantly lower than that calculated using the LA system (P < 0·001) and H skinfold thickness measurement (P < 0·001) (Table 3).
Discussion
The main goal of the present study was to evaluate the accuracy of the LA system for measuring skinfold thickness and estimating body fat on adults and older adults. The small magnitude of differences, the low sd of these differences and the narrow limits of agreement from Bland and Altman plots show that that the new LA digital system is in agreement with the H skinfold calliper for serial measurements of different skinfolds and for %BF calculations in the same individual. These results support the LA digital system accuracy.
To our knowledge, only few studies until now have assessed the performance and accuracy of using different skinfold calliper models on skinfolds thickness and %BF estimation. The differences in samples and techniques used between studies further limit direct comparisons. Burget & Anderson(Reference Burgert and Anderson18) compared triceps skinfold measurement between the McGaw and Lange callipers in ninety-one adults and fourteen obese adult patients and found a median difference between the callipers of 8 %. In the present study, we observed a lower median difference (2·0 %) between the LA system and H callipers for the triceps skinfold measurement of the adult sample, which can be regarded as positive. Lohman et al. (Reference Lohman, Pollock and Slaughter19) studied the effect of various skinfold callipers (Harpenden, Holtain, Lange and Adipometer), the examiner technique and skinfold prediction equations in female university athletes. The results suggested that for any given prediction equation, the range in mean %BF due to calliper–investigator combinations was 7 %.
Given that body composition changes are clearly related to the ageing process, several mechanisms could influence the precision of non-invasive methods, as in skinfold thickness measurement. To the best of our knowledge, no previous studies have assessed the performance and accuracy of the skinfold calliper among older adults, reinforcing the scope of the present results.
The new LA digital system instrumentation led to similar %BF evaluation for adults and older adults, relatively to the traditional H skinfold calliper. With regard to the results for both samples, a strong association was found between the DXA-%BF and %BF estimation by skinfold and conversion equations, showing that these two methods are in very close agreement. Although the Peterson-%BF for the adult sample and the Visser-%BF for the older adult sample produced slightly higher body fat estimation compared with DXA-%BF, these differences could be attributable to the regression equations used.
Despite the fact that methodological differences compromise direct comparisons, previous studies comparing %BF from skinfold-based equations to DXA-%BF in healthy adult Caucasians(Reference Jackson, Ellis and McFarlin3, Reference Stewart and Hannan20–Reference Sardinha, Lohman and Teixeira22) also report high correlations between these techniques(Reference Johansson, Forslund and Sjödin21). They depict significant differences between them as well, either overestimated(Reference Stewart and Hannan20, Reference Johansson, Forslund and Sjödin21) or underestimated(Reference Jackson, Ellis and McFarlin3). Stewart & Hannan(Reference Stewart and Hannan20) applied skinfold equations to a sample of twenty-four athletes and noted a total error of 2·9 %, slightly lower than the total error in the present study. Johansson et al. (Reference Johansson, Forslund and Sjödin21) found a strong correlation between %BF determined by DXA and skinfold thickness (r 0·81) in adult men (25–59 years old), but lower than those found in the present study. They also verified that DXA yielded a significantly lower mean fat content compared with skinfold thickness measurement, which is comparable to the present findings. However, Jackson et al. (Reference Jackson, Ellis and McFarlin3) cross-validated the Jackson/Pollock equations on a sample of 1129 young men and women, using DXA as the referent criterion for %BF and concluded that prediction equations based on skinfold measurement underestimated %BF by 1·3 % in men and 3·0 % in women. Sardinha et al. (Reference Sardinha, Lohman and Teixeira22), in a study conducted among sixty-two men, 37·6 (sd 2·9) years old, found a slightly weaker association for the skinfold thickness %BF predicted by the Jackson/Pollock equation (r 0·87) and DXA-%BF compared with the present results. They also found a higher se for the %BF estimation (3·7 %) as well as for %BF predicted by the Durnin/Womersley equation (r 0·85), where the se of estimation was 3·9 %.
Considering healthy Caucasian older adults, few studies have assessed the validity of skinfold thickness in predicting %BF, having DXA-%BF(Reference Haapala, Hirvonen and Niskanen23, Reference Ravaglia, Forti and Maioli24) as the reference method. Different population characteristics bring further difficulty to comparisons between studies. Haapala et al. (Reference Haapala, Hirvonen and Niskanen23) compared skinfold thickness measurement with DXA in a sample of ninety-three women (62–72 years old) and found a stronger association between skinfold method and DXA-%BF (r 0·94) than those found in the present study. However, the skinfold thickness measurement resulted in a significant error of − 0·7 (sd 3·0) kg as well. Ravaglia et al. (Reference Ravaglia, Forti and Maioli24) estimated %BF in sixty-seven men (20–95 years old) using skinfolds. Percentage BF, predicted by skinfold measurement and equations, underestimated DXA-%BF in the group aged >80 years, contrary to the present findings, where skinfold measurements and regression equations overestimated DXA-%BF.
The lack of a random sample selection can be recognised as a study limitation. As participants were recruited on a convenience basis, care should be taken in extrapolating the findings for other age groups and for frail individuals, as well as for those less physically active and for obese individuals.
The present study provided evidence that the LA system is an accurate instrumentation and represents an innovation in the evaluation of skinfold thickness and body composition based on anthropometric measurement. One of the innovations of the LA system is the digital information acquisition of the measurement at a predefined time interval of 2–4 s, according to the described methodology(Reference Fidanza8, Reference Jelliffe, Jelliffe, Zerfas and Jelliffe10, Reference Norton and Olds11). In the available analogical skinfold models, this time interval counting, readout of the needle position and its manual registration were subjectively performed by the technician and are now performed digitally and automatically. As the equipment is digitally sensorised, it not only facilitates skinfold thickness reading but also instantaneously records, stores and analyses data, while the wireless transmission of data in a portable way allows an instantaneous %BF evaluation. So, the test is faster and probable sources of measurement bias are avoided. In fact, the LA system solved some of the intrinsic problems of the skinfold thickness technique measurement.
The authors believe that these innovating features will allow a quicker and broader utilisation of skinfolds. This may also have positive implications for non-clinical and for general use.
Acknowledgements
The present research received no specific grant from any funding agency in the public, commercial or non-profit sectors. E. M. was supported by a doctoral grant from FCT-MCTES (SFRH/BD/36319/2007) and R. S. G. was supported by a research grant from FCT-MCTES (POCTI/ISFL/416-10), within IDMEC – Pólo FEUP. T. F. A., M. T. R., M. F. C. and J. M. designed the study. T. F. A., R. S. G. and E. M. performed the data collection. T. F. A. and R. S. G. conducted data analysis. All the authors contributed to the drafting of the paper. The authors have no conflict of interest.







