In line with worldwide population ageing, the average age of acute hospital in-patients is rising, with associated increases in levels of medical morbidity, general frailty, cognitive impairment and dementia. Many acute hospitals are ill-equipped to deal with the challenging and complex needs of such patients. These shortcomings are particularly highlighted by the challenge to care posed by delirium – a common neuropsychiatric condition that occurs across healthcare settings and patient groups. The impact of delirium is particularly apparent in acute general hospitals, where there is a concentration of vulnerable patients such as frail older people with pre-existing cognitive impairment and dementia. Additional morbidity, longer hospital admissions, increased requirement for long-term care, poorer cognitive profile and increased mortality all result directly from delirium (**Reference Witlox, Eurelings and De JongheWitlox 2010). Over the past decade, the emergence of organisations such as the European Delirium Association (www.europeandeliriumassociation.com) and the American Delirium Society (www.americandeliriumsociety.org), which focus primarily on delirium care and research from multidisciplinary perspectives, has produced an expanding literature. Nevertheless, delirium remains neglected as an area for intervention in general hospitals (**Reference Leslie and InouyeLeslie 2011). It continues to be mismanaged in everyday clinical settings and underappreciated in healthcare planning.
In this article we will first review the definition and prevalence of delirium and then focus on its prevention and management in the context of a cognitive-friendly hospital.
Defining delirium
Nosological confusion surrounds the concept of delirium. Historically, acute generalised disturbances of cognition have been referred to by a number of synonyms, each reflecting delirium occurring in particular populations or treatment settings. These range from the clinically intuitive ‘acute confusion’ to the downright bewildering ‘subacute befuddlement’. DSM-III (American Psychiatric Association 1980) provided systematic criteria for diagnosis that have gradually evolved through successive systems to the recently published DSM-5 (American Psychiatric Association 2013). The latter categorises delirium as a neurocognitive disorder based on criteria that reflect the occurrence of generalised disturbance of brain function (evidenced by cognitive and neuropsychiatric symptoms in which inattention and reduced awareness are central) that is relatively recent in onset, fluctuates and occurs in the context of physical morbidity. This concept draws on the relative simplicity that underpinned DSM-IV and has contributed to its popularity among clinicians and researchers (**Reference Morandi, Davis and TaylorMorandi 2013).
Delirium and dementia
Delirium and dementia are the two major neuropsychiatric syndromes affecting elderly people and they have considerable overlap in respect of clinical presentation. It is well recognised that dementia is a major risk factor for developing delirium (and underpins delirium in about 50% of cases), but increasing evidence implicates delirium not only as a marker for emerging dementia, but also as an aggravating factor in dementia that accelerates its course and as an independent risk factor for long-term cognitive impairment, including dementia (**Reference MacLullich, Beaglehole and HallMacLullich 2009). In a recent review, Reference George, Long and VincentGeorge and colleagues (2013) highlight how patients with dementia in acute hospitals have many negative outcomes, such as falls, delirium, loss of function, increased length of stay and increased mortality. Importantly, they identify multiple contributory factors, including inadequate assessment and treatment, inappropriate intervention, discrimination, inadequate staffing levels and poor staff training.
Prevalence and impact
Prevalence
Prevalence rates for delirium in general medical in-patients range from 11 to 42%, increasing to more than 60% in specific groups, such as older patients with severe medical illness, patients with cognitive impairment or terminal illness and those admitted to intensive care facilities (**Reference Siddiqi, House and HolmesSiddiqi 2006). A recent study across an entire general hospital identified an 18% point prevalence for delirium, while studies in palliative care and intensive care indicate rates of up to 85% (**Reference Ryan, O'Regan and CaoimhRyan 2013). Although data regarding the epidemiology of delirium among patients attending primary care are lacking, it is known to be highly prevalent in community nursing homes (**Reference Boorsma, Joling and FrijtersBoorsma 2012). The day-to-day care of at-risk groups such as elderly people with multimorbidity and those at the end of life is key to minimising known risk factors (see below).
Impact
Delirium has a range of adverse outcomes for the individual and for healthcare services. The cost to the individual includes loss of independence and increased mortality. But most important is the growing recognition that the state of delirium may be more than the neuropsychiatric manifestation or ‘symptom’ of an underlying physiological disturbance: it might in fact be neurotoxic in itself (**Reference MacLullich, Beaglehole and HallMacLullich 2009; **Reference Witlox, Eurelings and De JongheWitlox 2010).
The costs of delirium to healthcare organisations are high, in terms of both economics (Table 1) and service use. The cost of a single admission of a patient with delirium has been estimated at £13 000 in the UK (**Reference Akunne, Murthy and YoungAkunne 2012) and between $16 000 and $64 000 in the USA (**Reference Leslie, Marcantonio and ZhanqLeslie 2008).
TABLE 1 Estimated direct 1-year healthcare costs in the USA

The need for cognitive-friendly hospitals
In view of the significant human, clinical and economic costs of delirium in the acute general hospital, cohesive and multifaceted programmes are required to meet the needs of in-patients with newly emerging and/or long-standing cognitive problems. Reference George, Long and VincentGeorge and colleagues (2013) have proposed a multilevel, multifactorial approach to this problem, aimed at increasing awareness, education and detection and promoting evidence-based management of cognitive problems. Their cognitive-friendly hospital programme focuses on seven levels of care: patient, task, staff, team, environment, organisation and institution.
What constitutes a cognitive-friendly hospital programme?
Cognitive-friendly hospital programmes must be considered in the context of the wider healthcare system, and should be universally sensitive and responsive to the needs of our ageing population. One prominent example is the ‘senior friendly health services’ in Ontario, Canada (**Reference Hart, Frank and HoffmanHart 2006; Senior Friendly Hospitals 2012). Within this clinical construct, cognitive-friendly hospitals are responsive to the needs of a wide range of patients with differing and potentially changing cognitive profiles. For example, a person with pre-existing dementia is ‘flagged’ at entry to hospital as someone who has a high risk of developing delirium and a worsening cognitive profile while in hospital. The individual is closely monitored throughout their hospital stay, with delirium prevention measures and rapid assertive intervention in the event of emerging delirium.
A cognitive-friendly hospital programme needs to consider the patient’s entire ‘journey’ while in hospital in terms of the different clinical areas and services from the point of access to care (e.g. via a medical assessment unit, emergency department or elective admission) through to continuing care (e.g. on medical, psychiatric or surgical wards, or in intensive care or palliative care). This can facilitate a cohesive and multicomponent intervention that is tailored to the patient’s needs at different points of the at-risk/episode/recovery spectrum. Finally, these efforts should link effectively with primary and community care, where possible before, and always during and after, the hospital admission.
Key programme components
A cognitive-friendly programme should focus on the following areas (Fig. 1):
-
• increasing general awareness and recognition of cognitive problems
-
• improving levels of education and training
-
• optimising the use of evidence-based management strategies
-
• discharge planning that reflects the individual’s cognitive profile during the hospital admission.
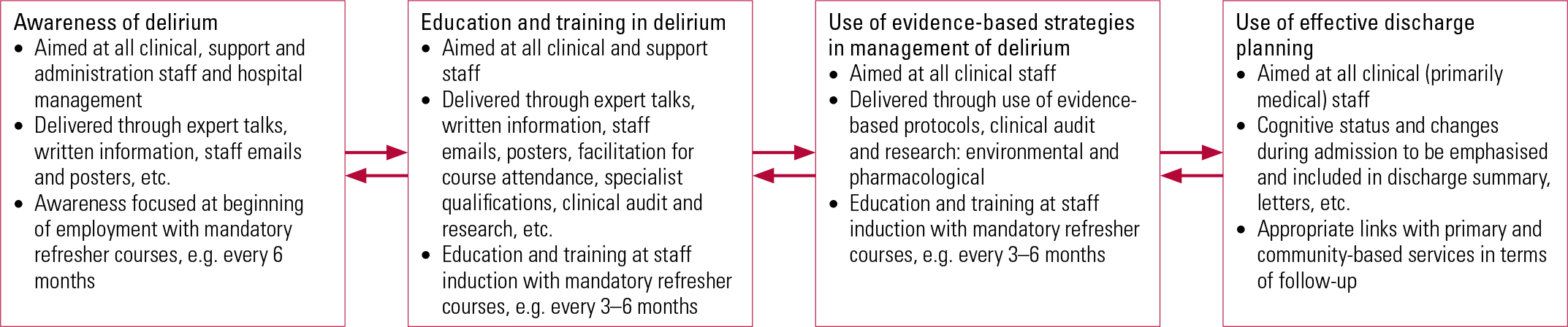
FIG 1 A cognitive-friendly hospital programme: components relating to delirium.
Increasing awareness
Increasing awareness of delirium and other cognitive problems and of their clinical importance is an essential first step in the development of a cognitive-friendly hospital programme. Although many patients with delirium experience difficulty in communicating their experiences and/or have diminished environmental awareness, studies indicate that many can themselves identify recent confusion and other synonyms for delirium (**Reference Ryan, O'Regan and CaoimhRyan 2013). All front-line clinical staff, such as doctors, nurses, allied healthcare professionals and care attendants, should be involved. Non-clinical staff with high levels of patient contact (e.g. cleaners and catering staff) should also be included, as subtle changes in eating and hygiene/self-care can assist in delirium detection and are often noticed by these staff members. In a UK qualitative study using normalisation process theory (**Reference Godfrey, Smith and GreenGodfrey 2013), staff, volunteers, patients and carers participated in developing a prevention of delirium programme that includes a multicomponent process that aims to introduce and embed delirium prevention into routine clinical practice. This research project led to the development of an integrated model of delirium prevention, known as the Prevention of Delirium (POD) Programme. Significant challenges were cited, including lack of understanding of delirium prevention and difficulties integrating a multifaceted programme into existing hospital systems. The authors have not as yet reported on the implementation of this programme.
Hospital executives should have a clear knowledge of the impact of delirium on factors such as clinical outcomes and length of stay in hospital, especially considering their financial implications (**Reference Leslie and InouyeLeslie 2011). Increasing awareness of delirium among hospital management and budget holders should encourage the development of delirium prevention and treatment programmes with proven cost-effectiveness. These include multicomponent preventive interventions (**Reference Akunne, Murthy and YoungAkunne 2012) such as the Hospital Elder Life Program (HELP). The latter can be tailored to individual hospitals and hospital networks to ensure that the needs of older patients are considered in all relevant aspects of service planning. Delirium diagnosis and associated clinical activity should be routinely captured (**Reference Rubin, Williams and LescisinRubin 2006).
The ‘cognitive MRSA’?
Using the analogy of infection control, delirium has been likened to a ‘cognitive superbug’ that is highly preventable but once established can have grave consequences (Reference MeagherMeagher 2009). Consequently, it can benefit from multicomponent control programmes similar to those that have substantially reduced rates of methicillin-resistant Staphylococcus aureus (MRSA) among hospital inpatients by engaging service users and providers in energetic prevention and treatment programmes (**Reference Dantes, Mu and BelflowerDantes 2013).
Education and training
The evidence base
Evolving evidence supports the use of educational interventions in the prevention and treatment of delirium in care homes and acute hospitals. Stop Delirium, a complex intervention aimed at delirium prevention, was introduced in six UK care homes over 10 months in a mixed-methods before-and-after study (**Reference Siddiqi, Young and HouseSiddiqi 2011). Positive effects in respect of staff attitudes and practices were noted and preliminary evidence suggested potential improvements in clinical outcomes such as reduced falls and medication use.
In a UK single-blind case–control study based in two acute admissions wards and focusing on 250 in-patients over 70 years of age, a delirium educational package was delivered to the staff of one of the wards (the intervention ward) (**Reference Tabet, Hudson and SweeneyTabet 2005). The point prevalence of delirium on the intervention ward was reduced (9.8% v. 19.5% on the control ward) and clinical staff’s recognition of delirium was significantly higher. Similarly, a Spanish case–control study (**Reference Vidan, Sanchez and AlonsoVidan 2009) assessed a multicomponent educational and risk reduction intervention for delirium prevention among 170 hospital patients aged over 70 (compared with care as usual for 372 control patients). Delirium prevalence was significantly lower in the intervention group (11.7% v. 18.5%), as was incidence. When delirium did occur, there was no significant between-group difference in severity, length and recurrence of episodes, but the rate of functional decline was reduced in the intervention group.
In contrast, guidelines alone may be inadequate. A UK ‘before’ (211 patients) and ‘after’ (125 patients) study assessed the effectiveness of specially developed consensus guidelines for the management of delirium in the acute wards of five general hospitals. Patients were aged over 65 and admitted with delirium. Introduction of the guidelines did not significantly affect the process and outcomes of care, although effects were more marked with higher levels of intervention (i.e. formal distribution of the guidelines to doctors and nurses and reinforcement with teaching sessions) compared with medium- and low-intensity intervention. However, this difference was not statistically significant (**Reference Young and GeorgeYoung 2003).
A range of simple and inexpensive activities can promote delirium awareness: talks from expert clinicians, posters and distribution of written material and emails to staff. Once integrated into staff induction and training, these activities need to be repeated on a regular basis to encourage discussion and reinforce appropriate treatment (**Reference Godfrey, Smith and GreenGodfrey 2013). However, evidence highlights how such programmes need to be underpinned by operational changes and/or a variety of supports to copper-fasten attitudinal gains (**Reference Godfrey, Smith and GreenGodfrey 2013). At the core of this matter is the need for delirium to be recognised as a key condition within healthcare activities and for its impact on outcomes to be routinely monitored.
Recommendations
The National Institute for Health and Care Excellence (NICE) guidelines on delirium highlight the potential importance of an education programme for healthcare professionals, reporting evidence (albeit of poor quality) that such programmes can reduce the incidence of delirium (NICE 2010). It is possible that education programmes would lead to an initial increased documented incidence of delirium, as heretofore unrecognised cases are diagnosed. NICE recommends a cluster randomised trial, with whole hospitals randomised to the educational intervention and delirium incidence as the primary outcome.
Building on a heightened awareness of delirium among all hospital staff, formal education and training should be targeted at clinical and support staff. Clearly, different levels and types of education and training are required for different members of staff, depending on their professional background and the clinical profile of patients. For example, a nurse working in an intensive care unit will have very different profiles of patients and clinical scenarios from those of a physiotherapist working in an orthopaedic ward. However, a similar foundation in delirium education and training is essential for all healthcare professionals, with specialisation tailored to their particular field. We recommend that formal education and training should be delivered at the start of employment and repeated regularly thereafter, for example every 6 months (Fig. 1). Relevant professional bodies should also have an input into the development, approval and monitoring of such education and training initiatives. We also recommend that the effectiveness of staff education and training initiatives be monitored and evaluated on a regular basis (e.g. through surveys of staff knowledge, attitudes and clinical practices).
E-learning is likely to be an important component of education and awareness programmes. Using a stepped-wedge cluster randomised trial methodology, an e-learning course on delirium aimed at nursing staff was introduced to medical and surgical wards in 18 Dutch hospitals (**Reference Van de Steeg, IJkema and LangelaanVan de Steeg 2014). The course was demonstrated to have significant positive effects on delirium screening, other aspects of care, improved knowledge of delirium and increased adherence to a quality improvement project in delirium care.
In a UK qualitative study exploring the learning needs of hospital staff relating to care of confused older patients in acute settings, 15 participants from a variety of healthcare backgrounds were interviewed (**Reference Teodorczuk, Mukaetova-Ladinska and CorbettTeodorczuk 2013). Five focus groups were conducted with patients, carers and mental health professionals. Eight categories of practice gap emerged that revealed hierarchically related learning needs best met by interventions initially addressing ownership of confused patients, negatives attitudes towards them and patients’ fear.
Overall, we conclude that the success of complex delirium prevention programmes is linked to systems factors that include:
-
• involvement of clinical leaders
-
• support from senior management
-
• linking the implementation of programmes to periods of systems change (e.g. realignment of care pathways)
-
• educational elements that are sustained and engaging
-
• mechanisms to support decision-making that are integrated into everyday routines (e.g. electronic care pathways)
-
• monitoring procedures to promote continued adherence.
In general, improving delirium care through formalised interventions is best achieved where it is supported by activities that promote enthusiasm, support implementation, remove barriers and allow for progress monitoring.
The workload and cost implications of interventions are further considerations. For example, HELP (www.hospitalelderlifeprogram.org/public/public-main.php) requires skilled inter disciplinary staff and trained volunteers to implement standardised protocols, and the use of its copyrighted protocols involves a fee. However, preliminary studies suggest that proactively addressing delirium risk can be cost neutral (**Reference Leslie, Marcantonio and ZhanqLeslie 2008) and reduces nursing workload caused by disturbed behaviour (**Reference Pretto, Spirig and MilisenPretto 2009). Given the evidence that delirium results in longer hospital stays and the need for interventions to address complications (**Reference Fick, Kolanowski and WallerFick 2005), better management of delirium and its complications should reduce healthcare costs.
Risk factors and delirium prevention
A key objective and quality-defining principle for a cognitive-friendly hospital is its ability to minimise exposure to risks that can result in delirium, and UK guidelines detail a range of evidence-based interventions that can reduce these risks (NICE 2010). Delirium is highly predictable, as a range of predisposing patient, illness and treatment factors interact with acute precipitating insults to produce the acute brain failure of delirium. Many of these factors (including a number with a significant iatrogenic element) are preventable and better service organisation can allow for preventive measures to produce better patient outcomes and reduced healthcare costs.
Reference Inouye and CharpentierInouye & Charpentier’s (1996) model of delirium causation among elderly hospital in-patients predicted a seventeen-fold variation in the relative risk of developing delirium. The model has been validated in elderly patients undergoing hip surgery (**Reference Kalisvaart, De Jonghe and BogaardsKalisvaart 2005). Baseline risk is especially important, as patients with high baseline vulnerability can develop delirium in response to even minor precipitants.
Certain factors are more relevant in particular settings and patient groups, but age extremes (very young and very old), pre-existing cognitive problems, severe comorbid illness and psychotropic medication are robust predictors of delirium risk across populations. All of these risks factors are readily identifiable and many are modifiable. Others can inform the risk–benefit analysis of surgical and other interventions in deciding on optimal care, especially for frail elderly patients with cognitive impairments (Box 1).
BOX 1 Risk factors for delirium in hospital setting
Patient-related
-
• Age ≥70 years
-
• Pre-existing cognitive impairment
-
• Previous episode of delirium
-
• CNS disorder
-
• Increased blood–brain barrier permeability
-
• Poor nutritional status
-
• Number and severity of comorbid illnesses
Illness-related
-
• Illness severity
-
• Dehydration
-
• Infection, e.g. urinary tract infection
-
• Fracture
-
• Hypothermia or fever
-
• Hypoxia
-
• Metabolic/electrolyte disturbances, e.g. low sodium
-
• Pain
-
• HIV/AIDS
-
• Organ insufficiency
-
• Burns
-
• Nicotine withdrawal
Environment-related
-
• Social isolation
-
• Sensory extremes
-
• Visual deficit
-
• Hearing deficit
-
• Immobility
-
• Use of restraints
-
• Novel environment
-
• Stress
Intervention-related
-
• Peri-operative
-
• Type of surgery, e.g. hip, cardiac
-
• Duration of operation
-
• Catheterisation
-
• Emergency procedure
Medication-related
-
• Polypharmacy
-
• Drug or alcohol dependence
-
• Benzodiazepine use
-
• Addition of ≥3 new medications
-
• Psychoactive drug use
-
• Certain drugs: e.g. anticholinergics
Minimising exposure to modifiable factors has been the focus of intervention studies that demonstrate that delirium is highly preventable (**Reference O'Hanlon, O'Regan and MacLullichO’Hanlon 2014). Many elements simply reflect good medical and nursing care (e.g. avoiding unnecessary polypharmacy, correcting sensory deficits). That these relatively simple practices need to be protocolised within a formal ‘intervention’ model reflects the challenges to the provision of routine care in most hospitals: delirium is often a marker of the dysfunction within our healthcare systems and processes.
Management of delirium
Although most of the literature reporting on the treatment of delirium derives from secondary care, the key messages are equally germane to healthcare professionals working in primary care. Delirium management can be thought of broadly in terms of prevention and treatment. These overlap and include both environmental and pharmacological approaches. Fundamental to these efforts is the identification of patients at high risk of developing delirium as well as the timely recognition of delirium when it occurs. However, these efforts must be aligned to meaningful interventions, as identification of patients with delirium does not always translate into better care. Several studies have identified substantial challenges to the management of delirium once identified, not least the knowledge and skills of healthcare workers (**Reference Godfrey, Smith and GreenGodfrey 2013; **Reference Teodorczuk, Mukaetova-Ladinska and CorbettTeodorczuk 2013).
Despite our increased understanding of delirium as a cohesive clinical entity, its presentation, severity and course can be highly variable, for example involving both syndromal and subsyndromal levels of severity and varying degrees of persistence or residual features over time. These factors highlight the complex clinical nature of delirium and associated difficulties in ensuring timely detection and treatment.
Given the number and complexity of biopsychosocial triggers of delirium, it is unsurprising that simple one-dimensional interventions (e.g. consensus guidelines, education) have limited impact (**Reference Young and GeorgeYoung 2003; **Reference Gagnon, Allard and GagnonGagnon 2010) and that multifaceted interventions that are sensitive to the complexities of individual patients’ needs are required.
Routine screening
Routine cognitive and delirium screening should be performed on all older patients admitted to hospital. The most efficient approach is to adopt a two-stage process: an initial screening phase using highly sensitive and brief tools such as the Confusion Assessment Method (CAM; **Reference Inouye, van Dyck and AlessiInouye 1990) or the Nursing Delirium Screening Scale (NuDESC; **Reference Gaudreau, Gagnon and HarelGaudreau 2005) identifies patients who require clarification of delirium diagnosis by more detailed and expert assessment. If delirium is diagnosed, the imperative is to assess and address clinical factors contributing to its onset using a detailed clinical history, clinical examination and a range of first-line (for all cases of delirium) and second-line (for particular cases) investigations. A collateral history clarifying baseline cognitive function should be sought as early as possible. Many patients with delirium do not require specific pharmacological treatment for their symptoms, but benefit from a multicomponent, patient-centred approach applying gerontological nursing principles to address their needs (Box 2). Unnecessary movement of patients between different clinical areas should be avoided and patients’ symptoms should be reviewed at regular intervals (tailored to the individual patient’s clinical status and risk factors for delirium) to ensure they are not deteriorating.
BOX 2 Multicomponent non-pharmacological management of symptoms of delirium
Educate patient and family/carer on delirium and prognosis
Involve family/carer in hospital care routine
Repeatedly reorient and reassure the patient
Normalise sleep patterns
Prevent complications, e.g. falls, constipation
Ensure adequate hydration
Ensure adequate pain relief
Encourage general activity, mobility and activities of daily living
Use visual/hearing aids to facilitate communication
Nurse with familiar staff in relaxed environment
Non-pharmacological management
Acute care for the elderly (ACE) units that include a specialised four-bed ‘delirium room’ have been introduced in some US hospitals. Delirium rooms provide 24-hour nursing care focusing on non-pharmacological approaches completely free of physical restraints, and they are designed to optimise cognitive and adaptive functioning while minimising factors that aggravate delirium. Reports of over a decade of clinical experience at two hospitals in the USA found reduced levels of adverse outcomes associated with delirium, including loss of function, length of stay and mortality rates (**Reference Flaherty and LittleFlaherty 2011). However, they acknowledge a lack of randomised controlled trials and difficulties in identifying the most effective components of this package.
Pharmacological management
Ideally, there should be a specified and limited role for antipsychotic agents in the management of delirium. Although no single agent is licensed in either Europe or North America for the prevention or treatment of delirium, antipsychotics have long been used in the management of delirium that is characterised by problem behaviours or distressing psychotic symptoms. These practices are supported by open-label studies, but evidence from randomised placebo-controlled trials is limited and for procholinergic agents the evidence has been largely negative (**Reference Van Eijk, Roes and HoningVan Eijk 2010). Studies have demonstrated positive effects for haloperidol, olanzapine and risperidone when used prophylactically in high-risk populations, but routine use is not yet justified (**Reference Larsen, Kelly and SternLarsen 2010; **Reference Wang, Li and WangWang 2012). The NICE guidelines advocate targeted and judicious use of haloperidol or olanzapine (NICE 2010), whereas two small placebo-controlled studies involving elderly medical and intensive care patients indicate more rapid symptom resolution with quetiapine (**Reference Devlin, Roberts and FongDevlin 2010; **Reference Tahir, Eeles and KarapareddyTahir 2010).
Thus, the role of pharmacological agents is primarily limited to management of delirious patients with severe behavioural or emotional disturbance causing them significant distress, placing them or others at risk, or interfering with essential investigations or treatment and where symptoms cannot be managed using non-pharmacological methods. The decision to use antipsychotic medication should involve careful consideration of whether the patient has adequate monitoring and supervision and whether potential exacerbating factors have been addressed. Short-term and carefully monitored use of an antipsychotic may be indicated if these criteria are met.
There is reasonable evidence to support the safe and supervised use of antipsychotics in managing delirium in acute hospitals (**Reference Hatta, Kishi and WadaHatta 2014). A Cochrane review found insufficient evidence to support the use of benzodiazepines for delirium and, in view of their deliriogenic potential, they should be reserved for delirium that is related to withdrawal states or seizures (**Reference Lonergan, Luxenberg and Areosa SastreLonergan 2009). Clear policies regarding pharmacotherapy – in relation to both avoiding non-essential polypharmacy and treating delirium – can contribute substantially to better management of delirium risk and adverse consequences where it occurs.
Reference Alexopoulos, Jeste and ChungAlexopoulos and colleagues (2005) found consensus among elderly care experts that treatment in delirium should be continued for at least a week after response. However, in reality many delirious patients are discharged before full resolution of symptoms, and continued monitoring and treatment are often overlooked in post-discharge planning. Transfer of patients with active delirium to therapeutic settings that are less equipped to cater for the many challenges of delirium is common, even though delirium is frequently a marker of severe and urgent physical morbidity. Addressing this failure to consider delirium care as an ongoing challenge is a key element in enhancing the cognitive friendliness of our services.
Discharge planning and delirium management post-discharge
Despite the high prevalence of delirium in the general hospital and its significant impact on long-term general and cognitive health and subsequent mortality, delirium occurrence is frequently omitted from discharge planning and in communications with primary care and other community services. There is evidence that the use of structured discharge reports can increase the reporting of delirium in discharge summaries (**Reference Van Zyl and DavidsonVan Zyl 2003).
The occurrence of delirium has important implications for post-acute care, where ongoing risk factors can be minimised and any residual functional deficits or psychological sequelae can be addressed. A substantial number of patients experience long-term cognitive and functional difficulties after resolution of the initial delirium event. One study, involving 433 older adults, found that 83% of those who were discharged from hospital with persistent delirium, and 68% of those whose episode of delirium had resolved before discharge home, required long-term care or had died within a year; these figures compared with 42% for patients who were never delirious (**Reference McAvay, van Ness and BogardusMcAvay 2006). Furthermore, an episode of delirium accelerates cognitive decline in patients with a pre-existing dementia (**Reference Fong, Jones and ShiFong 2009), emphasising the need for community care partners to be aware of the potential need for increased support for such individuals.
Delirium is a distressing experience for patients and their caregivers. Patients who have recovered from delirium may be uncomfortable discussing it because they equate delirium with senility or being ‘mad’. Reference Breitbart, Gibson and TremblayBreitbart et al (2002) explored perceptions of the experience of delirium among patients with a resolved delirium episode and their spouses. They found that distress correlated with severity of perceptual disturbances for the patients and functional loss for their spouses. In elderly patients without dementia who experienced delirium, more than half could recall their psychotic symptoms and many were still distressed by their recollections 6 months later (**Reference O'Malley, Leonard and MeagherO’Malley 2008).
Persistent psychological disturbances are a particular target for interventions as they can affect subsequent help-seeking behaviour. Formal followup visits can facilitate post-delirium adjustment by allowing for discussion of the meaning of delirium and planning of how to minimise future risk (e.g. by addressing risk factors such as medication exposure and sensory impairments).
A plan for improved delirium care
A cognitive-friendly hospital environment depends on a holistic approach to the identification, prevention and management of delirium. It requires patient-centred clinical care and system-wide support. The cost-effectiveness of such interventions and programmes should be evaluated and demonstrated. The evidence in support of the development of delirium care pathways already exists and can be embedded into the everyday practice of all hospitals. While the general principles for complete delirium care are well described, these care pathways should be developed with the specific pressure points of each institution in mind.
Particular challenges include:
-
• promoting awareness of delirium by including its detection and management as a key educational component of medical and nursing programmes at undergraduate and postgraduate level
-
• ensuring that delirium risk status monitoring becomes embedded into daily routines across all healthcare settings, including hospitals and community care
-
• systematic application of preventive measures, particularly for high-risk patients
-
• earlier and more consistent detection of delirium through formal systematic screening in everyday practice across healthcare settings, using computer-assisted and other technologies to facilitate more accurate assessment
-
• linking diagnosis of delirium to evidence-based action through protocolised management based on a more coherent understanding of how best to manage specific clinical presentations of delirium, the optimal duration of treatment and associated risk/benefit ratios
-
• implementation of formal strategies to promote the active management of the post-delirium phase, including the risk of subsequent episodes and the prevention of secondary psychological sequelae; this should include liaison between primary and secondary care especially in the post-discharge follow-up of patients diagnosed with delirium while in hospital
-
• monitoring the frequency of delirium and its impact on outcomes as a routine performance indicator within services
-
• conducting studies to clarify how non-pharmacological and pharmacological interventions for delirium management interact across populations.
Conclusions
Delirium has unrivalled penetration across healthcare services and, despite its predictability and preventability, is a major source of health and economic burden (Reference MeagherMeagher 2009). The introduction of cognitive-friendly in-patient programmes for delirium that continue into post-discharge care can significantly improve patient outcomes and reduce healthcare costs.
MCQs
Select the single best option for each question stem
-
1 Delirium:
-
a occurs in approximately 1% of acute general hospital admissions
-
b is routinely recorded within healthcare activity statistics
-
c is usually caused by MRSA infection
-
d is missed or misdiagnosed in approximately 50% of cases
-
e can be readily identified by neuroimaging techniques.
-
-
2 ‘Cognitive-friendly’ hospitals:
-
a are the norm in high-income countries
-
b can produce better clinical and economic outcomes
-
c can be facilitated by faster patient throughput
-
d are linked to longer durations of hospital stay
-
e can be achieved with simple educational interventions.
-
-
3 Dementia:
-
a is uncommonly present in patients with delirium
-
b is a more urgent clinical diagnosis than delirium
-
c is characterised by more profound disturbance of awareness than delirium
-
d always follows an episode of delirium
-
e can undergo an accelerated course after an episode of delirium.
-
-
4 In the treatment of delirium:
-
a benzodiazepines are never indicated
-
b NICE guidelines support the use of olanzapine and haloperidol where delirium is associated with risk or distress
-
c environmental measures are ineffective
-
d procholinergic agents are effective in prophylaxis
-
e polypharmacy is usually warranted.
-
-
5 In the aftermath of delirium:
-
a patients usually cannot recall psychotic symptoms
-
b recurrence is uncommon
-
c long-term cognitive problems are rare
-
d modifiable risk factors can be usually identified
-
e antipsychotic agents should be continued for 3 months.
-
MCQ answers

| 1 | d | 2 | b | 3 | e | 4 | b | 5 | d |





eLetters
No eLetters have been published for this article.