Non-communicable diseases (NCD) are the major cause of morbidity and mortality in most countries of the Middle East, representing more than 60 % of total annual deaths( Reference Musaiger 1 , Reference Yusuf, Hawken and Ounpuu 2 ). Currently 80 % of deaths from NCD are in developing countries, indicating that NCD are not simply diseases of developed countries. The first global ministerial conference on healthy lifestyles and NCD control in Moscow, in April 2011, led to the Moscow Declaration calling for the global health community to address the seriousness and growing problem of NCD( 3 ). It also identified actions to address obesity and NCD at the whole-of-government level by ministries of health in countries. Further, the UN high level meeting in September 2011 resulted in the adoption of a political declaration to address the global burden of NCD( 4 ). Both of these meetings have greatly increased the profile of NCD and the importance of governments taking NCD into account during long-term health planning.
It is well documented that obesity is a key risk factor for NCD, particularly type 2 diabetes, CVD, osteoarthritis and some types of cancer. Across the Middle Eastern region the prevalence of obesity ranks among the highest in the world. A recent review reported that the prevalence of overweight and obesity among adults ranged from 50 to 80 %, with higher prevalence among women than men( Reference Musaiger 1 ).
One study covering fifty-two countries from eight geographical regions worldwide showed that adult men and women in the Middle East have the highest mean BMI after the USA( Reference Yusuf, Hawken and Ounpuu 2 ). Additionally, the women in this region have the highest waist-to-hip ratio compared with all other regions( Reference Yusuf, Hawken and Ounpuu 2 ) and similar results were reported by the Chronic Disease Collaborating Group in a study covering 199 countries( Reference Finucane, Stevens and Cowan 5 ). Although the Middle Eastern region is characterized by different socio-economic levels, the prevalence in high-income countries (such as Arab Gulf states) and middle-income countries (such as Iran, Egypt, Jordan and Lebanon) was very similar, indicating that cultural rather than economic factors determine obesity in this region( Reference Monteiro, Moura and Conde 6 ). Further, costly energy subsidies of food and fuel are widespread in the region. In 2011, these were estimated to cost $US 212 billion (7·2 % of Gross Domestic Product)( 7 ). These subsidies are likely to promote the consumption of highly energy-dense foods as well as the use of mechanized transport( Reference Asfaw 8 ).
Higher availability and consumption of highly energy-dense foods (the nutrition transition) in conjunction with epidemiological transition (rapid population growth with modernization and advances in medicine improving fertility and reducing mortality) has led to considerable changes in dietary habits and lifestyle of the populations of this region. Shifts to more westernized diets, characterized by high fat, sugar and salt, have been apparent. Low intakes of fruit, vegetables and complex carbohydrates have been reported in all countries in the Middle Eastern region( Reference Musaiger 1 ). Large-scale urbanization, labour market changes from manual work to office work and increasingly sedentary lifestyles have led to marked decreases in physical activity. These changes, as well as other socio-economic factors, have contributed to the high prevalence of obesity and its co-morbidities in the Middle East( Reference Musaiger 1 , Reference Ghassemi, Harrison and Mohammad 9 , Reference Galal 10 ).
Despite the recognition of obesity as a significant worldwide problem, in-depth analysis of population trends in obesity and its consequences are lacking in both developed and developing countries( Reference Musaiger 1 ). Therefore, the present study aimed to model the effects of obesity in the population and predict the potential impact of raised BMI on future disease burden. While forecasts can only be predictive and not absolute, they are vital if countries are to adequately prepare for a tide of NCD morbidity and mortality. Micro simulation modelling was used to examine the effect of interventions that successfully reduce population BMI on future disease burden, extending current knowledge of the obesity epidemic in the Middle Eastern region.
Methods
Search strategy
A review of studies including data on BMI and obesity for the adult population in the Middle Eastern region between 1990 and 2010 was carried out using PubMed and Google Scholar search engines. Annex 1 (Supplementary Materials) provides specific details of the search strategy. The WHO BMI global database( 11 ) and hand-searches of article reference lists were also used in the review. The inclusion criteria were: (i) availability of data on BMI and obesity by age and sex and (ii) representative adult population (i.e. not specific groups). Data on children and adolescents were excluded because of lack of data and where data exist, the use of several reference standards for defining overweight and obesity made the findings hard to compare. Studies based on self-reported BMI and those with a non-representative sample of the general population such as data on a specific group were also excluded. Nevertheless, some sub-national studies represented urban populations only and were included because of the lack of sufficient numbers of national studies in these countries. The common BMI cut-offs recommended by WHO for defining overweight (BMI = 25·0–29·9 kg/m2) and obesity (BMI ≥ 30·0 kg/m2) were used. Table 1 provides the references and study details of each BMI data point included for each country.
Table 1 References of BMI data used for projecting obesity trends

M, males; F, females; STEPS, STEPwise approach to Surveillance; DHS, Demographic and Health Survey; CADISS, Coronary Artery Disease in Saudis Study.
With a second literature review we looked for age- and sex-specific data on the incidence, survival and mortality from ten obesity-related diseases in the Middle East (CHD, stroke, type 2 diabetes, and breast, colorectal, pancreatic, oesophageal, endometrial, liver and kidney cancer). Keyword searches through PubMed revealed that the required disease data were not available for most of the countries under study, so in several cases we used the best available data from the region and applied it with some adjustments to the other countries. For fatal diseases, a proxy country's incidence data were adjusted using a known, target country's mortality rate: the ratio of the target-to-proxy countries’ mortality rates was used to scale the proxy country's incidence rates. For non-fatal diseases, proxy country data were adjusted for the different population BMI distributions. CHD and stroke incidence data were available only for Iran (personal communication from M Talaei, Isfahan Cardiovascular Research Institute, Isfahan University of Medical Science, May 2011). For all other countries CHD incidence data for Iran were used but were adjusted by the ratios of country-specific age-standardized CHD and stroke mortality rates. Stroke incidence from Iran( Reference Azarpazhooh, Etemadi and Donnan 12 ) was similarly adjusted by stroke mortality rate ratios. The only study of type 2 diabetes incidence found for the region was also from Iran( Reference Harati, Hadaegh and Saadat 13 ). To use it for the other countries, diabetes incidence was adjusted by the country-specific obesity rates, as the disease is treated as non-terminal in the analysis. For cancer, incidence and mortality data for each country were extracted from GLOBOCAN( 14 ). For each disease, one set of survival data for the terminal disease was collected from the best available studies in the region due to the scarcity of country-specific studies. Annex 2 (Supplementary Materials) provides the references of each disease for each country.
The obesity-related relative risks for each disease were obtained from a review conducted by the DYNAMO-HIA (DYNAmic MOdel for Health Impact Assessment) report on data collection for overweight and obesity prevalence and related relative risks( 15 ).
Statistical analysis
A two-step modelling process was developed by Foresight( Reference McPherson, Marsh and Brown 16 ) and has been used for analysis of obesity in the UK and USA( Reference Wang, McPherson and Marsh 17 ), Eastern Europe( Reference Webber, Kilpi and Marsh 18 ) and Latin America( Reference Webber, Kilpi and Marsh 19 ). The same method was applied in the present study. In module 1 the data were fitted with non-linear, multivariate, categorical regression models with outliers removed, revealing the age- and sex-specific obesity trends. For each country at least two time points of data were necessary. The results were fed into a micro simulation program (module 2), which produces longitudinal projections of the associated burden of disease. The Monte Carlo method was used to create a cohort of individuals (here set to one million for each country), which has the demographic characteristics determined by population data from UN and WHO statistics for each country. For each individual in the cohort, a BMI value gets probabilistically assigned as a function of age, sex and calendar year. The individuals of the cohort proceed through the simulation with BMI, age and sex determining their risk of getting any of the ten diseases. Relative risks of disease due to obesity are included in the model. A comprehensive description of the micro simulation method can be found in Annex 3 (Supplementary Materials). The micro simulation was repeated for each country with two alternative scenarios of obesity trends. In comparison with the baseline assumption of unchecked obesity trends, we examined the effect of 1 % and 5 % reductions in population BMI across the region.
Results
From the databases and articles searched, thirty-five data points for BMI were suitable for inclusion. Nine countries had two or more years of appropriate data (Bahrain, Egypt, Iran, Jordan, Kuwait, Lebanon, Oman, Saudi Arabia and Turkey). Egypt, Jordan and Lebanon only had two years of data, and for Jordan they were both from urban samples. A combination of sub-national and national data was used for trends in Iran, Kuwait, Oman and Turkey. Israel, Morocco, Tunisia and the United Arab Emirates were not included as not enough suitable data were available at the time of analyses. According to these studies the highest levels of obesity to begin with were in Kuwait. Obesity was least pronounced in Iran, with a decrease over time observed in men. Annex 4 (Supplementary Materials) presents the current prevalence of obesity and projected trends in each country based on past and present data.
Figures 1 and 2 show the trends for combined overweight and obesity (BMI ≥ 25·0 kg/m2) prevalence (termed ‘overweight’) for men and women of all ages in each country. Kuwaiti men and women come out on top; overweight and obesity reaches exceedingly high levels in both men and women by 2030. Saudi Arabian men and women also have consistently high levels of overweight, but the expected increase in overweight appears particularly steep for men in Oman. Bahrain and Jordan all have high levels of overweight, with moderate increases over time. The data for Egypt, on the other hand, suggest decreasing overweight for both men and women. Decreases are also shown for men in Iran, which in general seems to have one of the lowest levels of overweight for men and women of the nine countries. Nevertheless, for Iranian women the proportion with BMI ≥ 25·0 kg/m2 is still more than half of the female population and set to stay that way. A slight decrease in overweight was also observed for Turkish women.
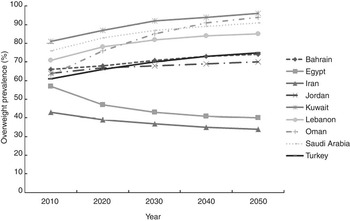
Fig. 1 Longitudinal projections of overweight prevalence (BMI ≥ 25·0 kg/m2) in men in the Middle East using multivariate non-linear regression
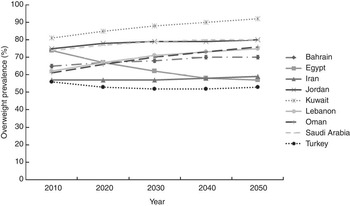
Fig. 2 Longitudinal projections of overweight prevalence (BMI ≥ 25·0 kg/m2) in women in the Middle East using multivariate non-linear regression
Figure 3 shows the extent of disease cases avoided if population-level BMI was to decrease by even a small percentage. In scenario 1, a 1 % reduction in obesity leads to a considerable amount of disease cases avoided in all countries. For example, in Bahrain, Kuwait, Lebanon, Oman and Saudi Arabia, by 2030 over a thousand cases of diabetes are avoided per 100 000 of the population. A substantial number of CHD and stroke cases are also prevented in this scenario, particularly in Lebanon, Oman and Iran. Cancer rates do not reach levels where a 1 % obesity reduction would have a noticeable effect. Incidence, mortality and survival data for each country are referenced in Annex 5 (Supplementary Materials).
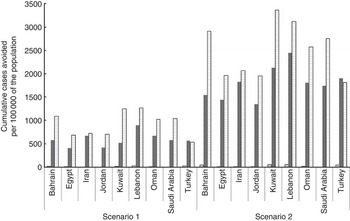
Fig. 3 Cumulative incidence cases of obesity-related non-communicable diseases (![]() , cancers;
, cancers; ![]() , CHD and stroke;
, CHD and stroke; ![]() , diabetes) avoided in Middle Eastern countries (per 100 000 population in 2010) by 2030, estimated using micro simulation modelling. Note: scenario 1 refers to a 1 % decrease in population BMI; scenario 2 refers to a 5 % decrease in population BMI
, diabetes) avoided in Middle Eastern countries (per 100 000 population in 2010) by 2030, estimated using micro simulation modelling. Note: scenario 1 refers to a 1 % decrease in population BMI; scenario 2 refers to a 5 % decrease in population BMI
If a 5 % reduction in population BMI is achieved as per scenario 2, the number of CHD, strokes and diabetes cases prevented becomes even higher. The number of CHD and stroke cases avoided ranges from 1400 to 2500 (per 100 000 population in 2010) for these Middle Eastern countries, with the highest numbers in Lebanon. However, the numbers of cancer cases avoided are still modest for all countries.
Based on the total population in Kuwait in 2010( 20 ), 1032, 39 905 and 63 217 incidence cases of cancer, CHD and stroke, and type 2 diabetes, respectively, will be avoided given a 5 % decrease in obesity. Based on the total population in Saudi Arabia in 2010( 20 ), over 115 000 cases of CHD and stroke and over 200 000 cases of type 2 diabetes will be avoided with a 1 % decrease in obesity by 2030, whereas with a successful intervention to reduce obesity by 5 %, 350 000 cases of CHD and stroke and 550 000 cases of type 2 diabetes could be avoided by 2030. A reduction in obesity will have less effect upon avoided cancer incidence in the total population.
Discussion
The latest national data from the Middle East reveal worryingly high obesity rates in many countries and the projections from the present analysis demonstrate how the obesity epidemic is not abating. In particular, our results for Kuwait, Oman, Saudi Arabia, Lebanon, Turkey, Bahrain and Jordan show that the problem of obesity is growing. Given that obesity is a risk factor for many NCD, this has major implications for the public health systems of these countries. The present study builds on past research by Finucane et al.( Reference Finucane, Stevens and Cowan 5 ) by estimating future trends and testing the impact of effective interventions.
Life expectancy is expected to increase remarkably during the coming four decades in the Middle Eastern region. The regional average percentage of life expectancy increase will be 15 % from 2000–2005 to 2045–2050, ranging from 5·8 % to 25·7 %( 21 ). Most if not all Middle Eastern countries will experience an increase in ageing populations, but the extent of the demographic transition varies. According to UN Population Reference Bureau data available online (http://www.un.org/esa/population/), Turkey and Lebanon have the highest proportions of people over the age of 65 years in the region, reaching 7 %, and fertility is below replacement level in Iran (1·74) and Lebanon (1·85). Age-specific trends indicate rapid increases in obesity in middle-aged or older adults and a sharp increase in ageing and NCD. Young adults in most countries do not show very steep obesity trends (Annex 6, Supplementary Materials). The ageing population combined with the BMI trends in older adults therefore represent a growing public health concern (Annex 6, Supplementary Materials presents the population distribution of each country).
It is unclear why Egypt and Iran show decreasing trends in overweight and obesity. It is possible that the mix of early sub-national and later national data in Iran biased the trends observed. Detailed BMI trends can be difficult to ascertain when the quality of the data is poor. Particularly the data for older adults were based on very limited samples or were non-existent. Moreover, analysis with just two data points gives only indicative results. Some studies did not have samples representative of the national population. Regional studies often have urban samples, which usually have higher relative BMI rates than would be found in a rural population. In countries such as Iran, with a large and diverse society, regional studies do not tell the whole picture and may also somewhat distort trends.
Furthermore, for a more complete picture of population health, the simulation would also need to incorporate the trends for children. Obesity is highly prevalent among children and adolescents in this region (excluding low-income countries), where the prevalence of overweight and obesity ranges from 20 to 45 %( Reference Musaiger 1 ). Including the young population in projections of future NCD rates would likely further increase the estimated size of the epidemic levels of morbidity and mortality. However, it was not possible to analyse the trends in children and adolescents due to lack of applicable data.
The increase of obesity during the past two decades in the Middle East has paralleled rises in diabetes, CVD and cancer. For example, the prevalence of diabetes in Jordan increased by 31·5 % during 1994–2006( Reference Ajlouni, Khader and Batieha 22 ). It was reported that five countries in the region were among the ten countries with the world's highest diabetes rates, namely Bahrain, Kuwait, Oman, Saudi Arabia and the United Arab Emirates. The Middle East has been projected to experience one of the highest relative increases in the burden of diabetes in the world by 2030( Reference Shaw, Sicree and Zimmet 23 ). A systematic review on stroke in Arab countries showed that the annual stroke increase ranged from 27·5 to 63 per 100 000 population. Ischaemic stroke was the most common subtype of all series. Hypertension, diabetes, hyperlipidaemia and cardiac diseases were the main risk factors( Reference Benamer and Grosset 24 ). In Iran, it was found that the annual stroke incidence in various age groups ranged from 23 to 103 per 100 000 population( 25 ). Several types of cancer are linked with obesity such as breast and colon cancers. These cancers are highly prevalent in most countries of the Middle East and cancer ranks as the fourth leading cause of death. The WHO reported that the highest increase in cancer incidence among WHO regions in the next 15 years is likely to be in the Middle East( 25 ).
The rapid change in food habits and lifestyle plays an important role in the high prevalence of obesity in the Middle East. During 1971–2005, FAO reported that there was an increase in per capita energy intake in all countries in the region. In this period, the percentage of energy which came from animal foods increased markedly( 26 ). The high intakes of fast foods and sugar-sweetened beverages have continued to rise as has the frequency of eating outside the home across the region, especially in high-income countries such as Arab Gulf states. A sedentary lifestyle and lack of physical activity were reported in most countries in the Middle East( Reference Musaiger, Hassan and Obeid 27 ). In Saudi Arabia, for example, the prevalence of inactivity among adults reached 96 %( Reference Al-Nozha, Al-Hazzaa and Arafah 28 ). However, the aetiology may be complicated by interaction between socio-cultural factors and lifestyle factors. Women, for example, might be experiencing conflicts of body image. Women have also been suggested to face greater barriers to practising physical activity than men, who in general have more freedom and places to exercise and participate in other recreational activities than women( Reference Yusuf, Hawken and Ounpuu 2 ). The comparatively higher rates seen in the Middle Eastern countries compared with Asia may be partly related to cultural factors that limit women's mobility. Other explanations include the existence of subsidies for energy-dense foods. The subsidization of wheat flour, rice, oils and sugar in many countries in the region may increase their intake, leading to higher consumption of energy. For example, in Egypt subsidized foods account for over 30 % of the overall per capita energy availability( 26 ).
Reducing obesity is an important strategy for lessening the future burden of disease. The simulation method is ideal for testing the effect of any scenario. It is possible to examine the consequence of any intervention with a known effect on BMI in a specific subset of the population. We modelled two scenarios of moderate reductions in obesity across the whole population. Considerable numbers of diabetes and of CHD and stroke cases were prevented in both scenarios for all countries. Of course the further the obesity problem has reached, the more critical the interventions become. Unchecked obesity trends are our best guess of how the epidemic will proceed without intervention. Undeniably, critical circumstances may change, for example food availability and prices. Even the political unrest of the Arab Spring may prove to have far-reaching consequences on lifestyles and health. Despite this, forecasts are necessary in planning the allocation of future resources for health.
The greatest limitation to our analysis is the paucity of the BMI and disease data available from each country, highlighting the need for improving systems of health surveillance. We were unable to include some countries such as the United Arab Emirates and Morocco since there were no suitable data available in the format necessary for the model. In addition, disease data were absent from many countries so we often had to make assumptions and often extrapolate from other countries in the region. Less robust conclusions can be drawn regarding the direction and speed of change in obesity where only a few (three or less) years of data were available; however, the exercise is still important since it emphasizes the necessity of population surveillance in health. Furthermore, the model now exists and can easily be updated when new data are made available. Good-quality national data on diseases can inform policy as well as facilitate international comparisons.
Further analyses might incorporate data on the social determinants of health including education level and asset-based wealth to take into account the dynamic relationship between socio-economic status (SES) and excess weight. There is strong evidence that as economic transition occurs, the burden of obesity shifts down the socio-economic gradient( Reference Monteiro, Moura and Conde 6 ). This pattern is observed earlier among women compared with men, particularly along the education gradient, such that women with low education experience a rapidly increasing obesity risk. The SES–excess weight associations will modify risk estimates for obesity-related diseases by age and gender depending on how wealth and education are distributed in these groups. Recent analyses of Egyptian national data show different SES–obesity associations by SES indicator( Reference Aitsi-Selmi, Chandola and Friel 29 ). An accurate understanding of how the social distribution of excess weight changes over time will aid in interpreting the results of further micro simulations and is essential in devising any intervention strategies in order to address the appropriate risk factors and target the vulnerable groups.
The UN high-level summit in September 2011 enabled the opportunity for global action against NCD. The Lancet NCD action group proposed five priority actions for the response to the NCD crisis: leadership, prevention, treatment, international cooperation, and monitoring and accountability. These actions, the NCD action group proposed, should be made on five priority interventions which include tobacco control, improved diets and physical activity, alcohol intake, essential drugs and technologies, and salt reduction( Reference Beaglehole, Bonita and Horton 30 ).
Conclusion
The obesity epidemic has the Middle East in its grip, bringing along a tide of chronic disease that will severely affect population well-being and test national health systems. People and resources need to be mobilized to manage the burdens of disease that may be expected with the current obesity trends. Exploring different BMI scenarios with the micro simulation method shows how even modest reductions in obesity prevent illness and lessen the health-care burden.
Acknowledgements
Source of funding: This study was funded by an unconditional educational grant from GlaxoSmithKline (grant number 27875780). Ethics: Ethical approval was not required. Conflicts of interest: There are no conflicts of interest to declare. Authors’ contribution: F.K. and L.W. made a substantial contribution to the literature search, data collection, analysis and interpretation of the data, drafting and editing of the article, preparing the article for submission and approval of the final version. A.M. and A.A.-S. made a substantial contribution to the drafting and revising of the manuscript for important intellectual content and gave approval for the final version to be published. K.R. made a substantial contribution to the literature search, analysis and interpretation of the data, drafting and redrafting the article and approval of the final version. M.B. made a substantial contribution to the analysis, conception and design of the study, interpretation of the data, revising the article critically for important intellectual content and approval of the final version. T.M. and K.M. made a substantial contribution to conception and design of the study, acquisition of the data, revising the article critically for intellectual content and approval of the final version.






