Twin reversed arterial perfusion (TRAP) sequence is a rare anomaly in 1% of monochorionic twin pregnancies. A few TRAP sequence cases have a rudimentary heart with cardiac motion in the acardiac twin. Intertwin hemodynamics in TRAP sequence have been investigated using the arterial Doppler waveform, but not the venous Doppler waveform. We investigated the venous Doppler waveform in two cases of TRAP sequence in which the acardiac twin had a rudimentary heart with cardiac motion.
Case 1
A 32-year-old woman, gravida 3, para 1, was pregnant by natural conception. At 12 weeks of gestation, she was diagnosed TRAP sequence. The acardiac twin had a rudimentary heart with cardiac motion.
Blood from the pump twin flowed to the umbilical artery (UA) of the acardiac twin in the reverse direction. This reversed umbilical blood flowed to the heart tube via the descending aorta of the acardiac twin. Blood from the rudimentary heart flowed to the acardiac twin’s umbilical vein (UV) via the internal iliac vein, and the reversed blood flowed to the pump twin via veno-venous (VV) anastomoses.
The circulation is shown in Figure 1. The UA Doppler waveform of the pump twin was normal. In contrast, the Doppler waveform of the descending aorta in the acardiac twin revealed two opposite pulses: one with the same pattern as that of the normal UA from the pump twin and the other in the opposite direction, from the heart tube of the acardiac twin. The heart rate was 149 bpm in the pump twin and 81 bpm in the acardiac twin. The UV Doppler waveform in the acardiac twin was thus a fusion of the standing wave from the pump twin and the heartbeat from the acardiac twin. Furthermore, in the pump twin, the venous pulsation affected the Doppler waveform of the UV, but not of the ductus venosus (DV).
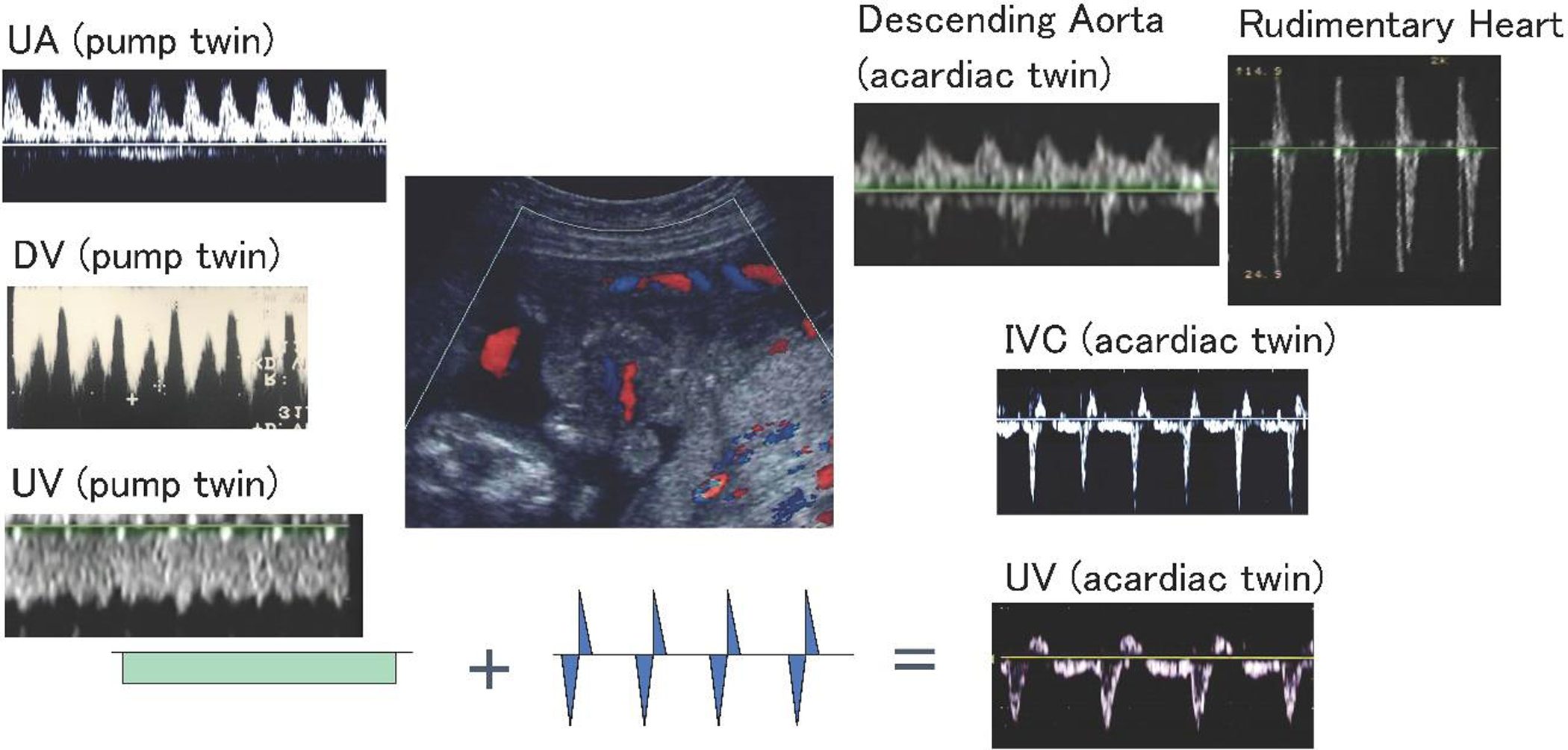
Fig. 1. Case 1. The circulation in a case of TRAP without a DV in the acardiac twin. The reversed umbilical blood flow perfuses the lower body via the internal iliac artery of the acardiac twin. The blood from the rudimentary heart flows to the umbilical vein of the acardiac twin via the internal iliac vein. The Doppler waveform of the UV from the acardiac twin is a fusion of the standing wave from the pump twin and the heartbeat from the acardiac twin.
Note: TRAP, twin reversed arterial perfusion; UV, umbilical vein; DV, ductus venosus; IVC, inferior vena cava.
Heart failure occurred in the pump twin at 27+2 weeks, so a Cesarean section was performed. The body weights of the pump twin and acardiac twin were 986 g and 608 g, respectively. The acardiac twin did not have a DV on a radiographic contrast study (Figure 2). After birth, we visually identified arterio-arterial (AA) and VV anastomoses.

Fig. 2. Arterio-arterial and veno-venous anastomoses in case 1. The acardiac twin did not have a ductus venosus on radiographic contrast study.
Case 2
A 33-year-old woman, gravida 3, para 1, was pregnant by in vitro fertilization–embryo transfer. At 10 weeks gestation, she was diagnosed with TRAP sequence. The acardiac twin had a rudimentary heart with cardiac motion.
Blood from the pump twin flowed to the UA of the acardiac twin in the reverse direction. The reversed umbilical blood flowed to the heart tube via the descending aorta of the acardiac twin. Blood from the heart tube flowed to the UV via a DV in the acardiac twin, and the reversed blood flowed to the pump twin via VV anastomoses.
The circulation is shown in Figure 3. The UA Doppler waveform of the pump twin was normal. In contrast, the Doppler waveform of the UA and the descending aorta in the acardiac twin revealed cyclic alternations in continuous heart cycles, reflecting a fusion of the pulses of the pump twin and acardiac twin. The UV Doppler waveform in the acardiac twin was a fusion of the standing wave from the pump twin and the heartbeat from the acardiac twin. Furthermore, venous pulsation from the heartbeat of the acardiac twin affected the UV and DV Doppler waveforms in the pump twin (Figure 4).
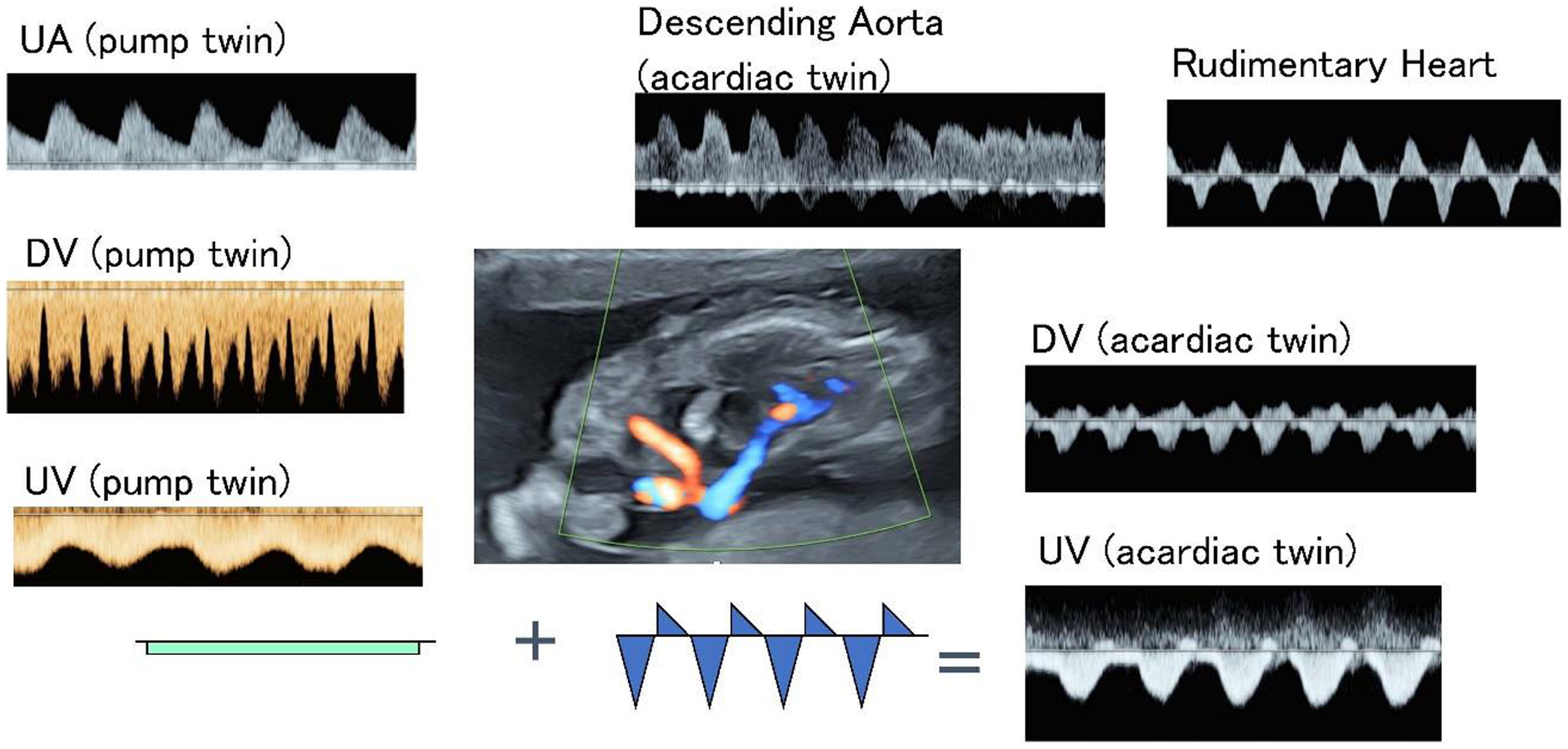
Fig. 3. Case 2. The circulation in a case of TRAP sequence with a DV in the acardiac twin. The reversed umbilical blood flow perfuses the lower body via the internal iliac artery of the acardiac twin. The blood from the rudimentary heart flows to the umbilical vein of the acardiac twin via a DV. The Doppler waveform of the UV from the acardiac twin is a fusion of the standing wave from the pump twin and the heartbeat from the acardiac twin.
Note: TRAP, twin reversed arterial perfusion; UV, umbilical vein; DV, ductus venosus.

Fig. 4. The venous pulsation of the acardiac twin affected the Doppler waveform of the DV and UV in the pump twin before RFA. The heart rate was 147 bpm in the pump twin and 124 bpm in the acardiac twin before RFA. The DV Doppler waveform in the pump twin shows a cyclic pattern, and the UV Doppler waveform in the pump twin reflects the pulsation in the acardiac twin before RFA. The venous Doppler waveform in the pump twin improved to normal after RFA.
Note: UV, umbilical vein; DV, ductus venosus; RFA, radiofrequency ablation.
Radiofrequency ablation (RFA) of the acardiac twin was performed at 18+0 weeks, and the DV and UV Doppler waveforms of the pump twin improved to normal status (Figure 4). Premature rupture of the membranes and miscarriage occurred at 20+6 weeks. After birth, we visually identified AA and VV anastomoses (Figure 5).

Fig. 5. Arterio-arterial and veno-venous anastomoses in case 2.
Discussion
TRAP sequence develops due to AA anastomoses between the pump and acardiac twin (van Allen et al., Reference van Allen, Smith and Shepard1983). Blood from the pump twin flows through the UA of the acardiac twin in the reverse direction. Reversed umbilical blood flow usually perfuses the lower body via the internal iliac artery in the acardiac twin. Blood with low oxygen content flows from the acardiac twin back to the pump twin. The present study demonstrates that, in some cases, the heart pulse of an acardiac twin with a rudimentary heart with cardiac motion can affect the venous Doppler waveform of the pump twin.
Intertwin hemodynamics have been investigated using the arterial Doppler (Shih et al., Reference Shih, Shyu, Hunag, Jou, Su and Hsieh1999; Wataganara et al., Reference Wataganara, Phithakwatchara, Pooliam, Jaingam, Thongkloung, Mongkolchat, Viboonchart and Nawapun2020), but not the venous Doppler waveform. Shih et al. (Reference Shih, Shyu, Hunag, Jou, Su and Hsieh1999) previously categorized the UA Doppler waveforms in TRAP sequences. The author reported that flow patterns in acardiac twins were determined by the existence of a primitive heart and the nature of the vascular anastomoses between the twins.
The cyclic pattern reflecting two pressure waveforms in opposite directions was originally described in the AA anastomoses of monochorionic twins (Hecher et al., Reference Hecher, Jauniaux, Campbell, Deane and Nicolaides1994; Joern et al., Reference Joern, Klein, Schmid-Schoenbein and Rath1999). The same pattern was observed in the UA of case 2 in the present study (Figure 3). In addition, the heartbeat from the rudimentary heart had a greater impact on the UV Doppler waveform in the acardiac twin in case 2 than in case 1, indicating stronger cardiac output in the acardiac twin in case 2.
Furthermore, the venous Doppler waveform pattern in case 2 showed a cyclic change in blood flow velocity similar to that of AA anastomoses, and the heartbeat of the acardiac twin affected the Doppler waveform of the DV in the pump twin (Figures 3 and 4 about here). This Doppler waveform indicated a cyclic pattern, reflecting the fusion of the pump twin’s DV waveform and the UV waveform from the heartbeat of the acardiac twin. This pattern was demonstrated using computerized recordings (Figure 6).

Fig. 6. The DV Doppler waveform of the pump twin reflects a fusion of the ductus venosus wave from the pump twin and the umbilical vein wave from the heartbeat of the acardiac twin. The cyclic pattern of the DV Doppler waveform in the pump twin is demonstrated using computerized recordings.
Cardiac motion was observed in the acardiac twin in both cases; however, the UA Doppler waveform in the acardiac twins differed. In case 1, the UA Doppler waveform had two opposite pulses, one reflecting the pump twin and the other reflecting the acardiac twin. Although the UV Doppler waveform in the pump twin contained the heartbeat of the acardiac twin, the DV waveform was not affected in the pump twin in case 1.
The main difference between the acardiac twins in the two cases is that case 2 had a DV and a stronger heart output. Thus, we speculated that these differences affected the venous Doppler waveform in the pump twin. Although the specific mechanisms remain unknown, the existence of a DV, or greater heart pulse power, in the acardiac twin might impact the venous Doppler waveform in the pump twin. Future studies are needed to determine whether cyclic changes in the venous Doppler waveform in the pump twins could affect their prognosis, including their cardiac function, compared to that in pump twins without such changes.
Author contributions
HK designed this study and drafted the manuscript. TM contributed to the concept and helped to draft the manuscript. All authors read and approved the final manuscript.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.








