In 2008, the Department of Health commissioned a review of the benefits and harms of antipsychotic drugs in people with dementia.Reference Banerjee1 This report, suggestively called Time for Action, concluded that in the UK around 144 000 people with dementia (18%) receive antipsychotics inappropriately, and that these drugs are responsible for around 1000 deaths every year.
Antipsychotics are associated with an increased risk of harm in older people with dementia. There is an up to threefold increased risk of stroke or stroke-like events over placebo and an increased risk of death.Reference Ballard, Hanney, Theodoulou, Douglas, McShane and Kossakowski2 There is also evidence that these drugs are associated with increased cognitive decline, falls, fractures and deep vein thrombosis.Reference Ballard, Hanney, Theodoulou, Douglas, McShane and Kossakowski2–Reference Herrmann and Lanctot5 The target symptoms and behaviours for antipsychotic prescribing are assumed to be those of behavioural and psychological symptoms of dementia (BPSD) but specific data related to this are rarely available or reported. Behavioural and psychological symptoms of dementia include agitation, psychosis, depression, wandering, resisting care, verbal and physical aggression, and are a major cause of both caregiver burden and institutional care.Reference Black, Brandt, Rabins, Samus, Steele and Lyketsos6 These symptoms are common, affecting nearly all patients with dementia at some point during their illness (point prevalence estimate 60–80% and cumulative risk 90%),Reference Banerjee1 and are more prevalent as the illness progresses.Reference Savva, Zaccai, Matthews, Davidson, McKeith and Brayne7
Further, it is perceived that antipsychotics are overused in this population at the expense of non-pharmacological strategies and pharmacological alternatives to antipsychotics that may be associated with less potential for harm.Reference Banerjee1 A range of non-pharmacological interventions for the management of BPSD are available but evidence of their effectiveness is mixed.Reference O'Neil, Freeman, Christensen, Telerant, Addleman and Kansagara8 A review found only few (cognitive stimulation, selected behaviour management therapies, and specific types of caregiver and residential care staff education) to have some evidence of lasting effectiveness.Reference Livingston, Johnston, Katona, Paton and Lyketsos9 Their implementation requires often significant resources (highly trained staff, time, equipment, etc.) and they cannot usually be used when the symptoms are severe.
The Time for Action report made a number of recommendations including that the use of antipsychotics in people with dementia should be audited. This was adopted as a local Commissioning for Quality and Innovation (CQUIN) target, the aim of which is to reward excellence in English health services by linking a proportion of a provider's income to the achievement of quality improvement goals.
This survey is part of an audit that sought to determine the frequency of use of antipsychotics in people with dementia who were in contact with Oxleas NHS Foundation Trust, for what indications they were used, and whether alternatives to antipsychotics were routinely considered and tried. We also looked at how often and in what way their use is reviewed.
Method
In June 2010, we conducted a retrospective cross-sectional survey using the Trust's electronic clinical record system (RiO). We set out to identify all patients with a confirmed diagnosis of dementia, F00-F03 of the ICD-10.10 We found 1106 such patients and accessed the electronic record of each to obtain information on age, gender, subtype and severity of dementia (according to clinical judgement of treating clinician), other psychiatric diagnoses, rationale for antipsychotic use, and duration of antipsychotic treatment. The rationale for antipsychotic use was selected from a pre-set list (drawn up after a discussion with local clinicians) which included known or assumed psychotic symptoms, depression, anxiety, verbal aggression, physical aggression, disinhibited behaviour, resisting care, wandering or unclear. Patients with a diagnosis of a schizophrenia-spectrum or other psychotic illness diagnosed before the onset of dementia were excluded from our sample as such patients could reasonably be expected to require treatment with antipsychotic medication. Where the required data were not found in the electronic patient record, the patient's care coordinators or consultant psychiatrist were contacted by email or/and telephone. This ensured that the data-set was as complete and accurate as possible. The clinical records of all patients who had started treatment with antipsychotics in the past 3 months were examined in detail to determine whether there was any documented evidence that non-antipsychotic interventions had been considered or tried before treatment with an antipsychotic was initiated. For the patients who had been on antipsychotics for longer than 3 months, we checked whether there had been clinical reviews and any side-effects considerations recorded.
The data collected were initially recorded on paper, then entered into and analysed using SPSS version 15 for Windows. Simple descriptive statistics were used.
Results
Sample
Of the 1106 patients identified, 41 were removed from our sample because they had a comorbid psychotic illness (schizophrenia, bipolar disorder or psychotic depression) or an unconfirmed diagnosis of dementia; a further 54 had moved out of the area or were no longer in contact with services; and 65 were deceased; this left a final sample of 946. Of these, 48.4% had a diagnosis of dementia in Alzheimer's disease, 31.7% had vascular dementia, 8.1% dementia in Parkinson's disease or with Lewy bodies, 4.3% dementia in Alzheimer's disease atypical or mixed, 3.8% unspecified dementia and 3.8% other subtypes of dementia such as dementia in Huntington's disease and alcohol-related dementia.
Prevalence of antipsychotic prescribing
Of the 946 patients, 186 (20%) were prescribed an antipsychotic drug, but this prevalence varied widely with the severity of dementia (Table 1). Half of the patients prescribed antipsychotics (53%) were living in care homes.
TABLE 1 Prevalence of antipsychotic use by severity of dementia

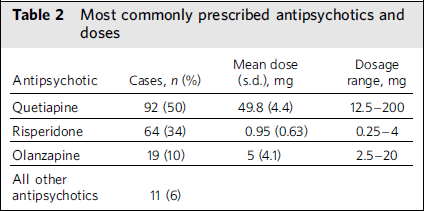
Which antipsychotics were prescribed?
The most commonly prescribed antipsychotic was quetiapine, which was used in 50% of cases (Table 2). The doses prescribed were low: 86% of quetiapine prescriptions were for ⩽75 mg. At low dosages (usually 12.5–100 mg) quetiapine acts as a sedative, hypnotic or anti-anxiety agent rather than an antipsychotic. For olanzapine, 84% of prescriptions were for ⩽5 mg/day and 80% of risperidone prescriptions were for ⩽1 mg/day (Table 2 has further information). Seven patients were prescribed a first-generation antipsychotic: haloperidol (n = 3), sulpiride (n = 2), trifluoperazine (n = 2).
TABLE 2 Most commonly prescribed antipsychotics and doses
Why were antipsychotics prescribed?
Indications for antipsychotic treatment, as recorded by the treating clinician in the patients’ clinical records, varied and those applied most often are shown in Table 3. The mean number of indications per patient was 2.6, with some patients having as many as 6 indications for use. In only one case was the reason for prescribing an antipsychotic unclear. To illustrate the complex nature of the patients for whom antipsychotic treatment was prescribed, over two-thirds of those with psychotic symptoms, verbal aggression or physical aggression were also agitated/distressed. Where resisting help with self-care or wandering was documented as part of the clinical presentation (n = 79), only 3 people with dementia had a sole documented indication of resisting self-care. No patient had the sole indication of wandering. All the rest (n = 76) had other indications for antipsychotic use, including distress, psychotic symptoms and aggression.
TABLE 3 Most common clinical reasons for initiating treatment with an antipsychotic drug in people with dementia
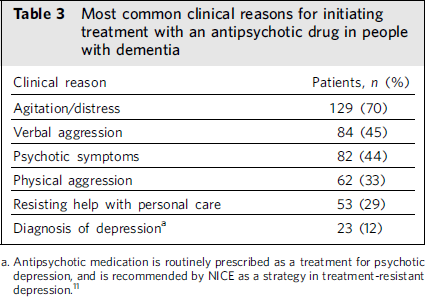
a. Antipsychotic medication is routinely prescribed as a treatment for psychotic depression, and is recommended by NICE as a strategy in treatment-resistant depression.11
Were other strategies tried before initiating antipsychotic treatment?
Of the 186 patients who were prescribed an antipsychotic, 21 (11%) had started treatment within the past 3 months. One of these patients had a diagnosis of psychotic depression. With respect to the other 20 patients, it was documented that other causes for the behaviour were considered and strategies other than antipsychotics tried in 10 individuals (50%). Most frequently, these involved treatment of physical symptoms such as constipation or pain. Changes to the environment or staff approach and engagement in activities were also documented. No patient received aromatherapy.
Were antipsychotics reviewed?
Of the 165 patients who had been treated with an antipsychotic for more than 3 months, 5 had a diagnosis of psychotic depression. Clinical review of treatment effectiveness (efficacy and side-effects) for the remaining 160 patients is presented in Table 4. In 140 cases (85%), the outcome of the most recent clinical review was clearly documented but in some of these cases this did not cover both efficacy and side-effects.
TABLE 4 Frequency of clinical review of effectiveness against target symptoms and side-effects in the past 3 and 6 months before the survey

a. The figure includes the patients reviewed at 3 months.
Were carers involved?
Of the 160 patients being treated with an antipsychotic for over 3 months, 136 (82%) had recorded evidence that the carers were involved in a discussion about the treatment plan.
Discussion
In the past few years, despite widespread criticism and numerous recommendations issued by responsible bodies,12–16 psychiatrists and general practitioners have continued to prescribe antipsychotics to people with dementia.14,Reference Haw, Yorston and Stubbs17 The UK government pledged a two-thirds’ reduction in 2011 in the number of patients with dementia who are prescribed antipsychotics.Reference Sutherland18 The current National Institute for Health and Clinical Excellence (NICE) guidance on prescribing antipsychotics to people with dementia recommends clear evidence of targeted symptoms which have to be of more than moderate severity, a documented risk-benefit analysis involving the patient and/or carer where appropriate, the use of small dosages and careful titration as well as regular reviews of medication and side-effects. Reports have highlighted distress as an important indication for treatment.Reference Treloar, Crugel, Prasanna, Solomons, Fox and Paton19
Our survey revealed appropriate motivations for initiating antipsychotics in the great majority of cases: patients’ distress and agitation (70%), aggressive behaviours and psychotic symptoms (44%), with high co-occurrence of multiple symptoms and behaviours. The view that antipsychotics are used primarily to manage resistive behaviours and wandering was not substantiated in our sample.
In our sample of people with dementia, 20% were on antipsychotics. The Banerjee reportReference Banerjee1 estimated that around 25% of people with dementia in the UK population will be on antipsychotics at any time. Taking into account that we looked at a secondary care case-load and that half of our patients were living in care homes, we found this figure better than expected. The proportion of patients prescribed antipsychotics increased with the severity of dementia and this follows the expected incidence of BPSD over the course of the illness.Reference Savva, Zaccai, Matthews, Davidson, McKeith and Brayne7
The choice of antipsychotic was, in the great majority of cases, one of the second-generation antipsychotics. This suggests that prescribing clinicians considered the risks associated with first-generation antipsychotics to be greater and this is in consensus with the literature.Reference McMurdo, Witham and Gillespie3 Although risperidone is the only antipsychotic currently licensed for short-term treatment of BPSD in dementia (maximum 6 weeks), in our sample, quetiapine, the least potent and most sedative antipsychotic in its class, was by far the preferred choice. This could be attributed to the fact that the initial recommendation from the Committee on Safety of Medicines had identified only olanzapine and risperidone as increasing the risk of stroke.12 Other audits carried out more recently have identified similar changes in prescribing practices.Reference Wittmann, Hausner, Hajak and Haen20,Reference Shah21
Antipsychotic dosage was in the great majority of cases low or very low. We found no patients on two or more antipsychotics.Reference Barnes and Paton22
The 15 patients with a diagnosis of Lewy bodies or Parkinson's dementia who had been prescribed antipsychotics were all on quetiapine. In nine of the cases there was evidence of psychosis documented in the notes. Owing to the lower incidence of extrapyramidal side-effects, quetiapine has become the antipsychotic of choice in dementia with Lewy bodies and Parkinson's disease dementia but its use is lacking evidence from randomised controlled trials.Reference Zahodne and Fernandez23
We found antipsychotic review rates to be unsatisfactory. Out of the 186 patients identified as being on antipsychotics, 58% had been on antipsychotics for more than 1 year and a third had not been reviewed in the past 6 months.
Our survey suggests that some caution may be needed when implementing the requested reduction in antipsychotic use for people with dementia as the rationale for initiation of these medicines was in the great majority of cases built around agitation and distress. It is true that the risks associated with antipsychotic drugs must inform our decisions, but so must benefits. There is a place for antipsychotics in the treatment of severe and distressing symptoms of dementiaReference Banerjee1,Reference Ballard, Hanney, Theodoulou, Douglas, McShane and Kossakowski2,Reference Treloar, Crugel, Prasanna, Solomons, Fox and Paton19,Reference Ballard and Waite24 and declining treatment to that subpopulation could cause more harm than good. To illustrate, in the past few years, concerns have been raised that the reduction in antidepressant prescriptions for adolescents following safety warnings by the US Food and Drug Administration (FDA), the Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMEA) was followed by an increase in the number of suicides.Reference Gibbons, Hur, Bhaumik and Mann25
Furthermore, it is important that the current antipsychotic overprescribing is replaced by other, safer means to manage the problematic symptoms and more support for patients and their carers, and not just the refusal of intervention. Thus, careful implementation and individualised care plans are essential. It is also crucial that drugs which we know to be toxic are reviewed, and our survey does not give comfort on this issue. Clear plans to fund antipsychotic reviews in care homes are indicated. It must be hoped that the introduction of National Decision support tools will enable both primary and secondary care to improve practice on these medicines.26
Limitations
An obvious limitation to the generalisability of our findings is that we only looked at secondary care prescribing, whereas antipsychotics are also being prescribed in primary care and acute hospitals to patients who are not on psychiatric secondary care case-loads. Also, our findings reflect the clinical practice in one trust only and it is expected that practice in other parts of the country may be different.
Further, RiO is a clinical management system rather than a data management system and it is known that the number of patients with dementia who were identified for the purposes of this survey is considerably lower than the number of patients with dementia who are currently in contact with the trust. Also, as all data were collected from RiO, the survey reflects only the clinical documentation and might not provide the true clinical picture and the interventions.
Implications for clinical practice
Our survey showed that antipsychotic use in dementia may be rational, based on careful consideration of indication and risks, and supported by discussion with family (which is achievable). Ongoing clinical review of antipsychotic effects and side-effects is important and may represent one of the greatest challenges.







eLetters
No eLetters have been published for this article.