Research has documented a link between maternal postnatal depression and offspring depression. Reference Murray, Arteche, Fearon, Halligan, Goodyer and Cooper1–Reference Halligan, Murray, Martins and Cooper3 Research has focused less on the impact of depression during pregnancy on offspring depressive psychopathology. Nevertheless, a handful of longitudinal studies have demonstrated an association between maternal depression in pregnancy and the development of depressive psychopathology in exposed offspring, but the evidence so far is limited to adolescence, that is, from 13 through to 18 years of age. Reference Pawlby, Hay, Sharp, Waters and O'Keane4–Reference O'Donnell, Glover, Barker and O'Connor6 To our knowledge, no prospective study has examined the association between offspring exposure to maternal clinical depression in utero and depression in adulthood; moreover, the pathways underpinning this association have not yet been clarified. Indeed, most research to date has focused on the broader relationship between maternal prenatal stress and offspring neurodevelopmental and health outcomes in later life, such as stress physiology, brain plasticity, immunity and chronic metabolic diseases, in addition to psychopathology. Reference Talge, Neal and Glover7–Reference Barker10
Evidence has also shown that maternal affective psychopathology in pregnancy is associated with offspring vulnerability to adverse childhood experiences. Reference Pawlby, Hay, Sharp, Waters and Pariante11,Reference Lereya and Wolke12 Specifically, in a recent study, maternal depression and anxiety in pregnancy was found to predict offspring victimisation in middle childhood, whereby there was a significant direct effect, as well as significant indirect effects through parental maladaptive parenting and conflict. Reference Lereya and Wolke12 Moreover, we have previously reported a link between a mother's experience of depression in pregnancy and her offspring's experience of harsh parental discipline and sexual and physical abuse at 11 years. Reference Pawlby, Hay, Sharp, Waters and Pariante11 Notably, in these particular instances, mothers were not the main perpetrators of violence, and were never involved in any instances of sexual abuse. Rather, peers and other adults in the home were primary perpetrators. Offspring of prenatally depressed and anxious mothers also exhibit more emotional reactivity and difficult temperament. Reference O'Connor, Heron, Golding, Beveridge and Glover13–Reference Sharp, Pickles, Meaney, Marshall, Tibu and Hill17 Collectively, these data suggest that the link between maternal affective disorders in pregnancy and offspring maltreatment is likely underpinned by changes to mothers' caregiving and attachment behaviours and her ability to protect her child, the impact of aggregated domestic risks, as well as potential foetal programming of a more emotionally labile offspring temperament, all of which could increase vulnerability to being maltreated. Reference Lereya and Wolke12,Reference Plant, Barker, Waters, Pawlby and Pariante18,Reference Pariante19
Research has also identified a robust association between experience of child maltreatment and the later development of depression. Reference Norman, Byambaa, De, Butchart, Scott and Vos20–Reference Wise, Zierler, Krieger and Harlow25 Indeed, a range of types of abuse and neglect are associated with an increased risk for depression in adulthood. Reference Norman, Byambaa, De, Butchart, Scott and Vos20,Reference Widom, DuMont and Czaja22 Some studies have reported a ‘dose–response’ relationship between severity of maltreatment and depression, as well as a link with depression that is more difficult to treat and has a chronic course. Reference Nanni, Uher and Danese21,Reference Bifulco, Moran, Baines, Bunn and Stanford23,Reference Wise, Zierler, Krieger and Harlow25 Preclinical studies in rodents and non-human primates have also shown that prolonged separation during the early sensitive period of development leads to behavioural changes in the offspring that persist into adult life, and resemble depressive and anxious human symptomatology. Reference Nemeroff26 Collectively, these findings suggest that the impact of exposure to maternal depression in pregnancy and exposure to child maltreatment may be a part of the same pathway for the pathogenesis of depressive disorders. We sought to test this hypothesis by data recently collected through a new wave of assessment of offspring participants (now young adults) of the South London Child Development Study (SLCDS), a prospective longitudinal birth cohort study setup by recruiting pregnant women in 1986. Reference Pawlby, Hay, Sharp, Waters and O'Keane4,Reference Plant, Barker, Waters, Pawlby and Pariante18,Reference Sharp27–Reference Hay, Pawlby, Waters, Perra and Sharp29 We aimed to test the following hypotheses:
-
(a) there is an association between offspring exposure to maternal depression in pregnancy and depression in adulthood;
-
(b) child maltreatment mediates the effect of exposure to maternal depression in pregnancy on adulthood depression.
Method
Design
The SLCDS is a prospective longitudinal UK birth cohort study that was setup in 1986. Reference Pawlby, Hay, Sharp, Waters and O'Keane4,Reference Plant, Barker, Waters, Pawlby and Pariante18,Reference Sharp27–Reference Hay, Pawlby, Waters, Perra and Sharp29 All pregnant women who approached either of two South London National Health Service antenatal clinics between January 1st 1986 and December 31st 1986 were invited to take part in the SLCDS. One-to-one clinical interviews were carried out with expectant women at 20 and 36 weeks of pregnancy and 3 and 12 months postpartum, and with offspring and mothers at 4, 11, 16 and 25 years. Two hundred and fifty-two women participated in the first assessment visit at 20 weeks pregnant. Because of time constraints, a 75% randomised subsample (hereon referred to as ‘the random sample’) were selected for interview at 36 weeks pregnant and 3 months postnatal, with the remaining women completing postal self-report questionnaires only. The random sample did not differ statistically in any sociodemographic or clinical characteristics in comparison with the non-random sample, and is the sample of interest in this paper. Reference Sharp27 Figure 1 depicts the progress of participation for the random sample from SLCDS onset to 25 years. At each phase of the study independent researchers who were unaware of the content of previous interviews interviewed offspring and mothers.
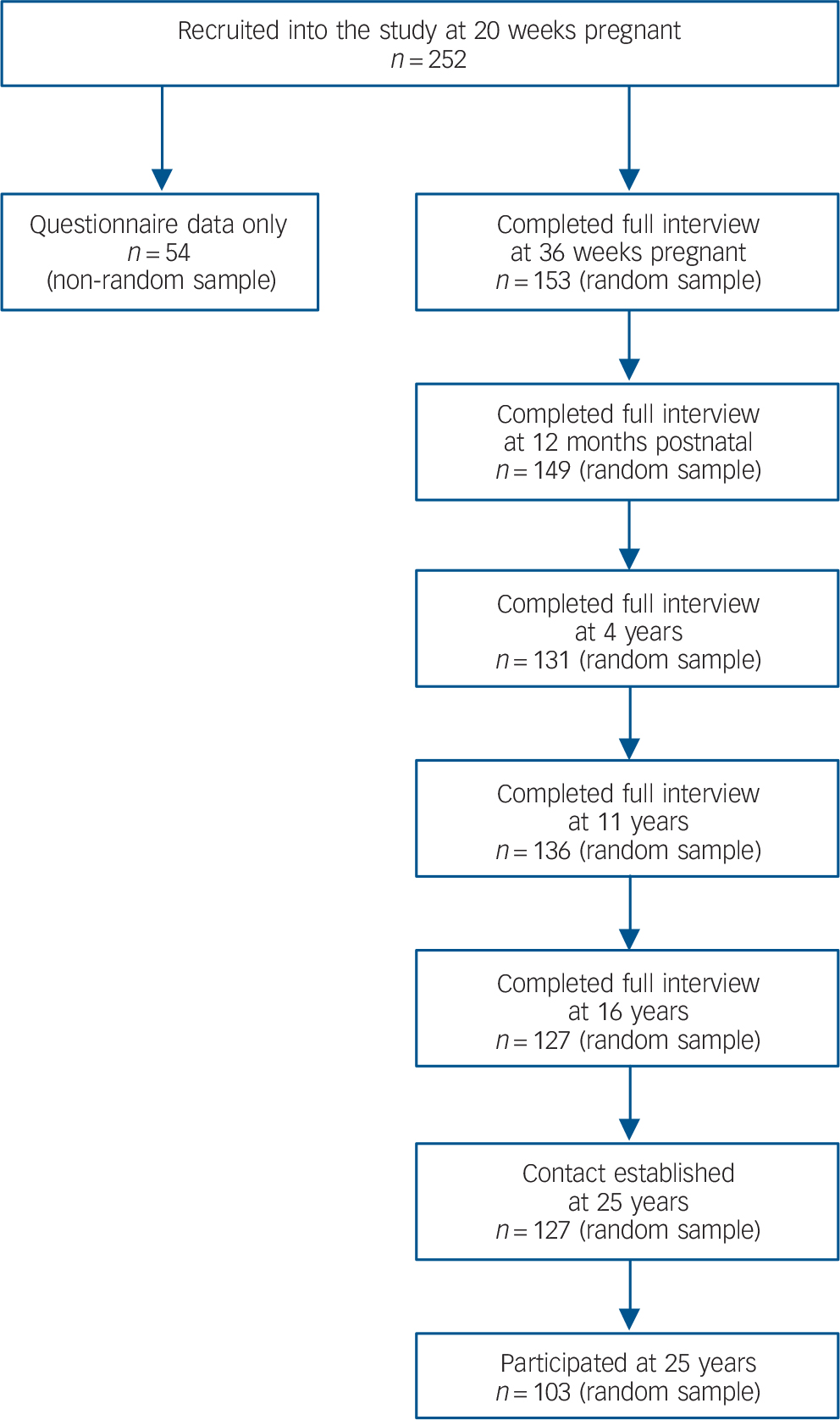
Fig. 1 Flowchart of study participation.
Sample
The sample comprised 103 offspring interviewed at age 25, and their mothers. This represents 76.3% of the offspring (n = 135) that were interviewed previously in childhood and adolescence. Characteristics of the sample at 25 years are presented in Table 1.
TABLE 1 Characteristics of the sample at 25 years (n = 103)
| Characteristic | Statistic |
|---|---|
| Maternal age at index pregnancy, M (s.d.) | 26.2 (4.8) |
| Maternal social class, % middle class | 12.6 |
| Maternal marital status in pregnancy, % married | 63.1 |
| Offspring age at assessment, M (s.d.) | 25.1 (0.7) |
| Offspring gender, % female | 52.4 |
| Offspring ethnicity, % White British | 72.8 |
| Offspring education, % GCSEs or higher | 89.3 |
| Offspring marital status, % married | 8.7 |
Measures
Maternal depression in pregnancy
Maternal prenatal depression was assessed at 20 and 36 weeks of pregnancy by the Clinical Interview Schedule (CIS). Reference Goldberg, Cooper, Eastwood, Kedward and Shepherd30 International Classification of Diseases, Ninth Revision (ICD-9) diagnoses were made of the women's current mental state over the 2 weeks before each assessment. A dichotomous variable was created that detailed whether a mother had been clinically depressed at either time point in pregnancy (0 = non-depressed; 1 = depressed).
Maternal depression in the postnatal period (birth to 1 year)
At 3 and 12 months postnatal mothers were interviewed about their current mental state (past 2 weeks) by the CIS, from which ICD-9 depressive disorder diagnoses were rated. Mothers were also interviewed retrospectively at 4 years using the lifetime version of the Schedule for Affective Disorders and Schizophrenia (SADS-L) about their mental state during the entire first postnatal year, from which Research Diagnosis Criteria ratings of depression across the first postnatal year were generated. Reference Spitzer, Endicott and Robins31 Postnatal depression was defined by the combined 3-month, 12-month and retrospective interviews; if a mother met criteria for a depressive disorder on any one of these interviews, she was rated as having experienced postnatal depression (0 = non-depressed; 1 = depressed).
Maternal depression during the offspring's childhood (1–16 years)
At 4, 11 and 16 years mothers were interviewed about their current mental state and experience of depression retrospective to the previous assessment using the SADS-L. Current and “retrospective to last visit” data were used to assess the occurrence of maternal depression over the child's lifetime. Variables were created to measure the children's exposure to maternal depression during early (between 1 and 4 years), middle (between 4 and 11 years) and late childhood (between 11 and 16 years). For each time interval, depression was rated if a mother met criteria for depression currently or retrospective to the last visit. We generated a ‘chronicity’ variable which summed the number of periods a mother reported being depressed (0–3 periods); moreover, a binary variable of whether the mother had ever experienced depression in the period between the child's 1st and 16th birthday was also generated (0 = non-depressed; 1 = depressed).
Offspring child maltreatment
Offspring exposure to child maltreatment (physical abuse, sexual abuse, emotional abuse or neglect up to age 17), was rated based on two independent assessment measures: the Childhood Experience of Care and Abuse Questionnaire (CECA.Q) conducted with the offspring at 25 years, and the Child and Adolescent Psychiatric Assessment (CAPA) conducted with offspring and primary caregiver (in most cases the mother) at 11 and 16 years. Reference Bifulco, Bernazzani, Moran and Jacobs32–Reference Angold and Costello34 Physical and sexual abuse were rated based on offspring reports of severe incidents provided at 25 years by the CECA.Q (rated in accordance with cut-off guidelines published by Bifulco and colleagues), Reference Bifulco, Bernazzani, Moran and Jacobs32 combined with the joint offspring and parental reports of severe instances of sexual and physical abuse provided at 11 and 16 years by the CAPA. For CAPA recorded incidents, physical abuse was rated if respondents reported incidents of abuse that involved at least some physical injury or force with potential for such, whilst sexual abuse was defined as incidents in which a perpetrator involved the offspring in activities for the perpetrator's own sexual gratification, such as fondling, oral contact, genital or anal intercourse. Emotional abuse and neglect were indexed through offspring ratings of severe parental antipathy and severe parental neglect up to 17 years by the CECA.Q in accordance with the rating guidelines published by Bifulco and colleagues. Reference Bifulco, Bernazzani, Moran and Jacobs32 A binary variable of maltreatment was rated if any one of the three types of severe abuse (physical, sexual, emotional) or severe neglect were ever present (0 = non-maltreated, 1 = severe maltreatment). We also generated a continuous ‘severity’ variable that summed the number of forms of severe abuse and neglect the offspring ever experienced (0–4).
Offspring adulthood depression
Offspring depression (DSM-IV diagnoses of major depressive disorder (MDD), depressive disorder not otherwise specified (NOS) and dysthymic disorder) between ages 18 and 25 was assessed at 25 years by the Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version. Reference First, Spitzer, Gibbon and Williams35 Diagnoses were rated in conjunction with the study psychiatrist. A binary variable indicating a diagnosis of depression was generated (0 = non-depressed, 1 = depressed). A continuous ‘severity’ variable was also constructed from the highest number of DSM-IV depressive symptoms reported in any given episode.
Confounding variables
The following risk variables were included as potential confounders: Reference Thapar and Rutter36 maternal age in pregnancy (in years); maternal ethnicity (White British (0) versus not White British (1)); maternal social class (middle class (0) versus working class (1)); maternal education (basic qualifications (O-levels) or higher (0) versus no qualifications (1)); maternal marital status in pregnancy (married (0) versus unmarried (1)); maternal psychiatric history (depression, anxiety, substance abuse, psychosis; 0 = no history, 1 = history); maternal prenatal anxiety (mean score on the anxiety subscale of the Leeds Anxiety Scale in pregnancy); maternal prenatal smoking (mean cigarettes smoked per day); maternal prenatal drinking (mean number of alcohol units drunk per week); offspring gestational age (whole weeks); offspring birth weight (grams); offspring gender (male (0) versus female (1)); offspring ethnicity (White British (0) versus not White British (1)); offspring education (at least one GCSE grade A*–C (0) versus none (1)); offspring IQ (at 16 years).
Ethics
Full ethical approval was obtained for all stages of the study. At 25 years from London – Camberwell St Giles National Research Ethics Service Committee (reference number: 11/LO/0812).
Data analysis
Analysis proceeded in three main steps. First, we performed univariate analyses to assess the relationships between maternal prenatal depression, offspring childhood factors (i.e. child maltreatment, maternal depression in offspring childhood), offspring adulthood depression and other risk variables. Next, we used hierarchical regression analyses to test for independent association between maternal depression in pregnancy and offspring adulthood depression. Finally, mediation analysis was performed to test whether environmental factors mediated the association between maternal depression in pregnancy and offspring adulthood depression.
All statistical analyses were conducted in IBM SPSS Statistics Version 21 (IBM Ltd., Portsmouth, UK). Log transformations were applied to improve the normality of the data. For data that did not benefit from transformation, non-parametric statistical tests were applied. Mediation analysis was conducted using PROCESS for SPSS Version 2.041. Reference Hayes37 Ordinary least squares (OLS) regression was used to calculate path estimates and estimates of the size of the direct and indirect effects. Bootstrap confidence intervals were generated as an inferential statistical test of the indirect effect. Reference Hayes37 In all analyses the number of bootstrap samples was set to 10 000 and 95% bias-corrected bootstrap confidence intervals (CIs) generated.
Results
Descriptives
Thirty-nine (37.9%) offspring met criteria for a diagnosis of DSM-IV depression in adulthood. Twenty-nine (74.4%) of the offspring with a diagnosis of depression had experienced at least one MDD episode, five (12.8%) experienced dysthymia and five (12.8%) depressive disorder NOS; the mean number of DSM-IV depressive symptoms amongst depressed offspring was 6.0, s.d. = 1.6. Thirty-five offspring (34.0%) were exposed to maternal depression in pregnancy, 20 (57.1%) of whom were further exposed in the first postnatal year. Overall, 36 (35.0%) mothers experienced postnatal depression and 64 (62.7%) mothers experienced at least one depressive episode during the offspring's childhood (1–16 years).
Thirty-six (35.0%) offspring were rated as having experienced child maltreatment. Twenty-three (22.3%) offspring experienced one form of maltreatment, three (2.9%) experienced two forms of maltreatment, six (5.8%) experienced three forms of maltreatment and four (3.9%) offspring experienced all four forms of maltreatment. Parents were observed to be perpetrators of the majority (90.0%, n = 18) of cases of physical abuse, but were not perpetrators of any instances of sexual abuse; stepparents, other family members, peers and non-related individuals accounted for all instances of sexual abuse. Regarding parental emotional abuse and neglect, mothers accounted for 52.9% (n = 9) of cases of emotional abuse and 33.3% (n = 5) of cases of neglect.
Associations between maternal depression and offspring adulthood depression
As predicted by our first hypothesis, offspring exposed to maternal depression in pregnancy were 3.4 times (95% CI (1.5, 8.1), χ2(1) = 8.4, P = 0.004) more likely than those not so exposed to be depressed in adulthood. Of the 35 offspring exposed to maternal depression in utero, 20 (57.1%) met DSM-IV criteria for a depression diagnosis; in contrast, of the 68 non-exposed offspring, only 19 (27.9%) met criteria for a depression diagnosis. The mean number of depressive symptoms was also significantly higher amongst prenatally exposed offspring (M = 3.4, s.d. = 3.0) compared to non-prenatally exposed offspring (M = 1.7, s.d. = 2.8, z = −2.8, P = 0.004). There was a high degree of association between maternal depression in pregnancy and depression in the first postnatal year (χ2(1) = 11.5, P = 0.001, OR = 4.3, 95% CI (1.8, 10.4)). Yet, we did not find any association between maternal depression in the postnatal period and offspring depression in adulthood (χ2(1) = 2.1, P = 0.15, OR = 1.8, 95% CI (0.8, 4.2)).
However, offspring exposure to maternal depression during childhood (1–16 years) was associated significantly with offspring adulthood depression (OR = 4.2, 95% CI (1.8, 10.2), χ2(1) = 11.1, P = 0.001). Analysis suggested a ‘chronicity’ effect, whereby offspring exposed to maternal depression over a greater number of developmental periods experienced more severe depression in adulthood (n = 100, r s = 0.31, P<0.01). The mean number of depressive symptoms amongst offspring exposed to maternal depression across 1 developmental period was 3.0 (s.d. = 3.1), amongst those exposed across two developmental periods (M = 3.3, s.d. = 3.5) and amongst offspring exposed across all three developmental periods (M = 3.6, s.d. = 3.4). Mothers depressed during the offspring's childhood were significantly more likely to have been depressed during pregnancy, 77.1%, compared to mothers not depressed during the offspring's childhood years, 22.9% (OR = 4.8, 95% CI (1.9, 12.2), χ2(1) = 12.0, P<0.001).
Univariate associations between offspring adulthood depression and other risk factors
Next we tested for associations between offspring adulthood depression and other potential risk factors. Table 2 summarises these univariate analyses. Notably, offspring exposure to child maltreatment was associated significantly with offspring depression in adulthood (diagnoses) (OR = 2.6, 95% CI (1.1, 6.1), χ2(1) = 5.2, P = 0.022). There was a positive correlation between severity of child maltreatment and severity of adulthood depression (symptoms) (r s = 0.30, P<0.01). Analysis revealed that offspring exposed to one form of maltreatment had the lowest number of depressive symptoms (M = 2.6, s.d. = 3.3), whilst offspring exposed to three forms experienced the greatest number of depressive symptoms (M = 5.5, s.d. = 3.2), indicative of a ‘dose–response’ relationship.
TABLE 2 Group differences between depressed versus non-depressed adult offspring
| Non-depressed adult offspring (n = 64) |
Depressed adult offspring (n = 39) |
Group effect |
|
|---|---|---|---|
| Maternal depression in pregnancy, % | 23.4 | 51.3 | P = 0.004 |
| Maternal characteristics | |||
| Age at index pregnancy, M (s.d.) | 26.5 (4.8) | 25.8 (4.9) | P = 0.47 |
| Ethnicity, % White British | 79.7 | 74.4 | P = 0.53 |
| Social class, % middle class | 17.2 | 5.1 | P = 0.12 a |
| Education, % some qualifications | 79.9 | 69.2 | P = 0.23 |
| Marital status in pregnancy, % married | 73.4 | 51.3 | P = 0.02 |
| Previous psychiatric history, % b | 25.4 | 33.3 | P = 0.39 |
| Maternal perinatal factors | |||
| Prenatal anxiety, M (s.d.) | 4.7 (3.1) | 5.6 (3.6) | P = 0.25 |
| Prenatal smoking, M (s.d.) | 3.7 (5.8) | 4.1 (6.8) | P = 0.90 |
| Prenatal drinking, M (s.d.) | 0.8 (1.5) | 1.1 (2.0) | P = 0.19 |
| Postnatal depression, % | 29.7 | 43.6 | P = 0.15 |
| Offspring obstetric factors | |||
| Birth weight, M (s.d.) | 3399.1 (432.3) | 3355.4 (582.3) | P = 0.66 |
| Gestational age, M (s.d.) | 40.1 (1.5) | 39.6 (2.0) | P = 0.27 |
| Childhood factors | |||
| Maternal depression 1–16 years | |||
| % exposed | 40.6 | 74.4 | P = 0.001 |
| Chronicity of exposure, M (s.d.) c | 0.7 (0.9) | 1.3 (1.0) | P = 0.002 |
| Offspring child maltreatment | |||
| % exposed | 26.6 | 48.7 | P = 0.02 |
| Severity, M (s.d.) | 0.4 (0.7) | 1.0 (1.3) | P = 0.007 |
| Offspring characteristics | |||
| Gender, % female | 45.3 | 64.1 | P = 0.06 |
| Ethnicity, % White British | 76.9 | 66.7 | P = 0.27 |
| Education, % some qualifications | 92.2 | 84.6 | P = 0.33 a |
| IQ, M (s.d.) d | 95.8 (16.1) | 94.1 (13.8) | P = 0.56 |
Note. The independent samples t-test was used for group comparisons comprising continuous parametric data, whilst the Mann–Whitney test was applied to non-parametric continuous data. Pearson's chi-square test for independence was used for the analysis of categorical data.
a. Fisher's exact test applied because of one contingency table cell showing an expected cell count less than five.
b. n = 102 (well = 63, depressed = 39).
c. n = 100 (62, 38).
d. n = 98 (61, 37).
Predicting offspring depression in adulthood
Hierarchical multiple logistic and linear regression models were applied to assess whether mothers' depression during pregnancy predicted their offspring's adulthood depression diagnoses and symptoms, respectively. When maternal postnatal depression and associated sociodemographic risks (i.e. maternal marital status in pregnancy, offspring gender) were entered into the models at the first step, maternal prenatal depression predicted significantly both offspring adulthood depression diagnoses and symptoms, respectively (Wald statistic 5.7, P = 0.02, OR = 3.1, 95% CI (1.2, 7.7), model χ2(3) = 12.5, P = 0.006; B = 1.6, t = 2.5, P = 0.015, 95% CI (0.3, 2.9), model R 2 = 0.14, F(4, 98) = 4.0, P = 0.005). However, when childhood factors (i.e. child maltreatment, maternal depression 1 to 16 years) were entered at the second steps, prenatal maternal depression no longer predicted significantly offspring depression. We did not find any evidence of statistical moderation of maternal depression in pregnancy on offspring depression in adulthood by either child maltreatment or maternal depression during the offspring's childhood.
Pathways from maternal depression in pregnancy to offspring adulthood depression
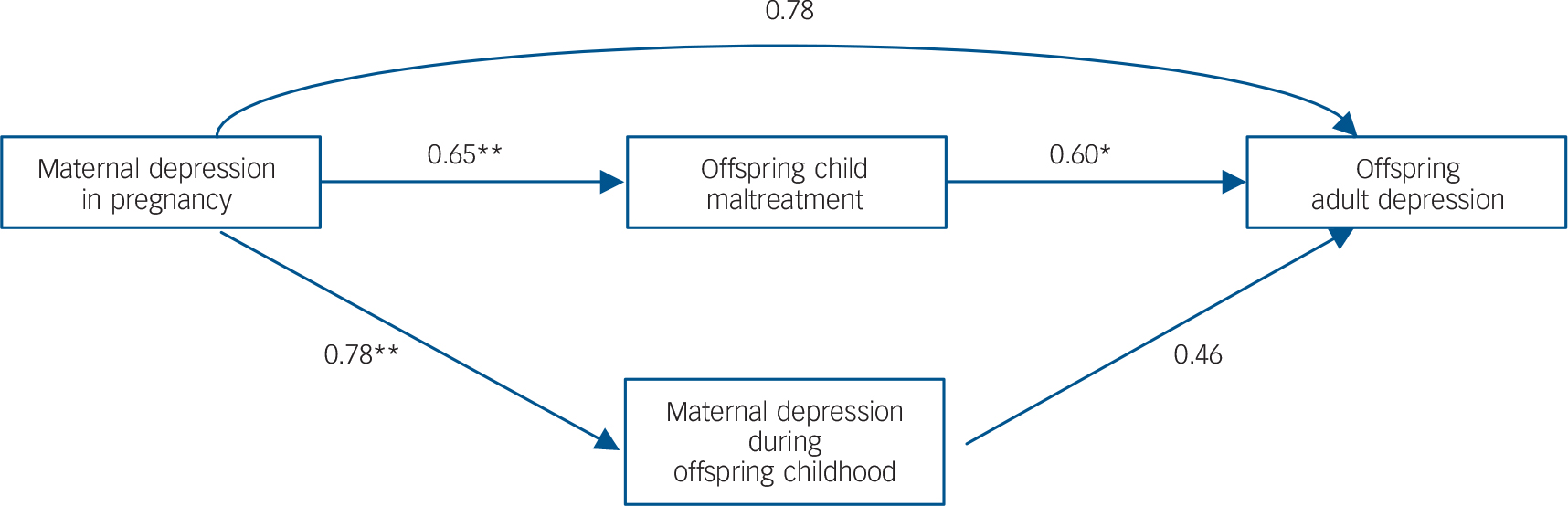
The prevalence of child maltreatment was significantly higher amongst offspring of mothers depressed in pregnancy, 48.6% in comparison with 27.9% of offspring of non-prenatally depressed mothers (OR = 2.4, 95% CI (1.0, 5.7), χ2(1) = 4.3, P = 0.038). To investigate our second hypothesis, that offspring experience of child maltreatment mediates the association between an offspring's exposure to maternal depression in pregnancy and their experience of depression in adulthood, we conducted mediation analysis using OLS path analysis. We tested a multiple mediation model in which maternal depression in pregnancy was entered as the antecedent variable, adult offspring depressive symptoms were entered as the outcome variable, and (a) offspring child maltreatment severity and (b) maternal depression during the offspring's childhood were entered as mediator variables. Figure 2 depicts this path analytic model. In all regression models, confounding variables associated significantly with adult offspring depressive symptoms (i.e. maternal marital status in pregnancy, offspring gender) were entered as covariates.
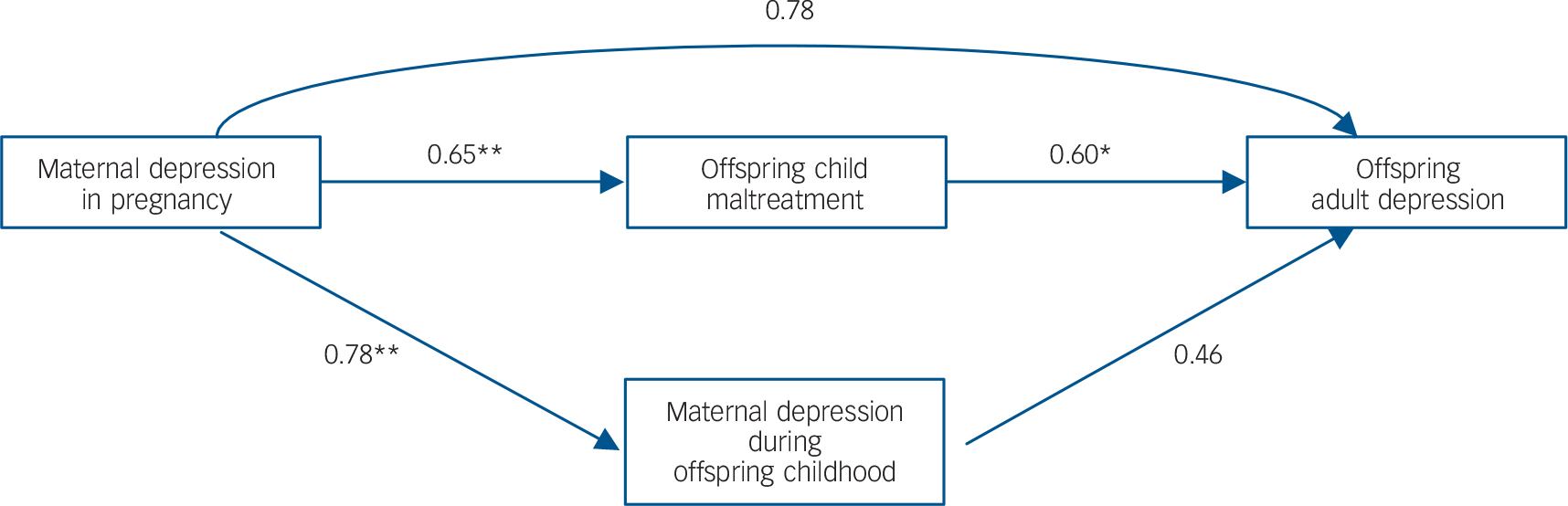
Fig. 2 Path estimates for the multiple mediation model of the effect of maternal depression in pregnancy on offspring adulthood depression mediated by childhood risks.
Note. Estimates are presented as unstandardised B coefficients. All path estimates were calculated whilst controlling for associated covariates. *P<0.05, **P<0.01.
As shown in Fig. 2, maternal depression in pregnancy predicted significantly offspring child maltreatment (B = 0.65, P = 0.002), and maternal depression during the offspring's childhood, B= 0.78, P<0.0001; moreover, offspring child maltreatment predicted significantly adult offspring depression (B = 0.60, P = 0.04). In contrast, the path between maternal depression during the offspring's childhood and offspring adulthood depression was not significant (B = 0.46, P = 0.15) indicating that the abovementioned univariate association is no longer significant when taking into account the effects of offspring child maltreatment. Table 3 summarises the regression coefficients for tests of the direct and indirect effects of offspring adulthood depression regressed on maternal depression in pregnancy. We found a significant indirect effect of maternal depression in pregnancy on offspring adulthood depression mediated by offspring child maltreatment (B = 0.39, 95% CI (0.04, 1.05)).
TABLE 3 Regression coefficients for the direct and indirect effects of offspring adulthood depression regressed on maternal depression in pregnancy
| Direct effect | Indirect effect | |||||
|---|---|---|---|---|---|---|
| Offspring child maltreatment | Maternal depression in offspring childhood | |||||
| B (s.e.) | 95% CI | B (s.e.) | 95% CI | B (s.e.) | 95% CI | |
| Maternal depression in pregnancy → offspring adulthood depression |
0.78 (0.67) | −0.55, 2.11 | 0.39 (0.25) | 0.04, 1.05 | 0.36 (0.29) | −0.09, 1.10 |
Note. n = 100. Boldface type indicates significant effect, i.e. the 95% bootstrap confidence intervals do not cross zero. Regression coefficients presented are unstandardised B coefficients. All path estimates were calculated whilst controlling for associated covariates. All regression models were significant at the P<0.01 level.
Discussion
In the present study we used a 26-year prospective longitudinal design to demonstrate, for the first time, that exposure to maternal depression during pregnancy increases offspring vulnerability to developing clinical depression in adulthood. Moreover, we find that maternal depression in pregnancy is also associated with increased vulnerability for child maltreatment in the offspring, and that this is a mediating mechanism linking exposure to maternal depression in pregnancy and depression in early adulthood. When the SLCDS started in 1986, it was the first UK longitudinal birth cohort to investigate clinical depression in pregnancy prospectively, and thus it is the only such cohort today with data available on offspring psychopathology in adulthood. Reference Pawlby, Hay, Sharp, Waters and O'Keane4,Reference Plant, Barker, Waters, Pawlby and Pariante18,Reference Sharp27–Reference Hay, Pawlby, Waters, Perra and Sharp29
Maternal depression during pregnancy and offspring adulthood depression
Our finding that offspring exposure to maternal depression during pregnancy is associated with depression in adulthood extends previous findings from the SLCDS showing that exposure to maternal depression in pregnancy predicts offspring depression at 16 years, Reference Pawlby, Hay, Sharp, Waters and O'Keane4 as well as recent findings from the Avon Longitudinal Study of Parents and Children (ALSPAC) showing that exposure to maternal depression in pregnancy predicts depression at age 18. Reference Pearson, Evans, Kounali, Lewis, Heron and Ramchandani5 Notably, we did not find that exposure to maternal depression after birth contributes to this association. This suggests that exposure to maternal depression specifically during pregnancy represents a unique setting for the intergenerational transmission of risk for depression, which is independent from further exposure to maternal depression after birth.
This account is in line with the theoretical premise of foetal programming, which postulates that offspring exposed to an adverse intrauterine environment, especially exposure to elevated levels of maternal glucocorticoids, can result in changes in foetal brain development in regions relevant to stress reactivity, such as the hypothalamic-pituitary-adrenal (HPA) axis, inflammatory response system and amygdala. Reference Glover8,Reference Barker10,Reference Seckl and Holmes38–Reference Buss, Davis, Shahbaba, Pruessner, Head and Sandman42 Indeed, HPA axis dys-regulation and inflammation are routinely observed in depressed individuals, Reference Pariante and Lightman43–Reference Nemeroff and Vale46 and studies have shown that pregnancy per se is associated with increased maternal HPA axis activity and inflammation, which can be further exacerbated by the experience of depression during this time. Reference O'Keane, Lightman, Marsh, Pawlby, Papadopoulos and Taylor47–Reference Jung, Ho, Torpy, Rogers, Doogue and Lewis49
Mediating mechanisms: the influence of child maltreatment
Our second set of findings relate to the links between maternal depression during pregnancy, offspring child maltreatment, and offspring adulthood depression. We find that offspring of mothers who were depressed during pregnancy are at increased risk of experiencing maltreatment during childhood, and – crucially – that this insult is a mediator in the association between exposure to maternal depression during pregnancy and offspring adulthood depression. These results confirm and extend our previous findings that exposure to maternal depression during pregnancy predicts childhood physical and sexual abuse as well as harsh discipline, as well as findings that maternal depression and anxiety during pregnancy predict peer victimisation. Reference Pawlby, Hay, Sharp, Waters and Pariante11,Reference Lereya and Wolke12,Reference Plant, Barker, Waters, Pawlby and Pariante18
The relationship between a mother experiencing depression during pregnancy and the increased vulnerability of her offspring to experience maltreatment may be explained by reduced maternal capacity for care, a poor maternal-offspring attachment relationship, the influence of exposure to aggregated environmental risks, such as maladaptive parenting and inter-parental conflict, and foetal programming of an emotionally labile offspring temperament. Reference Lereya and Wolke12,Reference Plant, Barker, Waters, Pawlby and Pariante18,Reference Pariante19,Reference Alhusen50–Reference Feldman, Weller, Zagoory-Sharon and Levine52 It is likely that these mechanisms co-occur, thereby culminating in elevated vulnerability for offspring maltreatment.
Indeed, a review summarised that maternal low mood during pregnancy was associated with lower maternal-foetal attachment. Reference Alhusen50 Furthermore, rates of child-mother secure attachment have been shown to be lower amongst maltreated preschool children in comparison with non-maltreated children. Reference Stronach, Toth, Rogosch, Oshri, Manly and Cicchetti51 Harsher maladaptive parenting in conjunction with poorer maternal-offspring attachment could account for the high rates of maternal physical and emotional abuse that we observed. Moreover, the fact that the perpetrators of sexual abuse and of neglect were others than the mothers themselves could be accounted for by the impact of a compromised ability of depressed pregnant mothers to protect their young from other perpetrators both in the home and the wider environment. Reference Pariante19 A more emotionally labile and reactive temperament among the offspring could contribute directly to their being more vulnerable to maltreatment as well as eliciting further detrimental parenting practices. Reference Ge, Conger, Cadoret, Neiderhiser, Yates and Troughton53 Taken together, our findings support the notion that exposure to maternal depression during pregnancy and exposure to child maltreatment are likely part of a single pathway to adulthood depression.
Strengths and limitations
The study has numerous strengths, such as the use of a prospective design starting in pregnancy through 26 years, the collection of data through one-to-one interviews and assessment of psychopathology at a clinically significant level. However, there are certain limitations. First, the small sample size did not allow for the analysis of more specific effects of individual risks, such as type of maltreatment. Second, the SLCDS is drawn from an urban, predominantly working class population of families of white ethnic origin. Whilst this could be deemed a high-risk population with high prevalence rates of psychopathology, a recent epidemiological study demonstrated prevalence of common mental disorders to be four-fold higher amongst urban London residents compared to residents of other UK cities, Reference Hatch, Woodhead, Frissa, Fear, Verdecchia and Stewart54 suggesting the cohort to indeed be representative of larger urban populations. Nevertheless, it is also possible that our high prevalence rates could also reflect genetic transmission of depression from parent to offspring. Reference Silberg, Maes and Eaves55 Finally, the majority of mothers were diagnosed with ICD-9 neurotic depression during pregnancy. As this diagnosis states that anxiety can also be present along with depressed mood, it is possible that our observed effects could be attributed to anxiety, or mixed anxiety and depression, rather than depression alone. 56
Implications
Our study shows that exposure to maternal depression during pregnancy increases offspring vulnerability for developing depression in adulthood. We find that child maltreatment is a putative mediating mechanism in this trajectory. These findings support the notion that exposure to maternal depression during pregnancy and exposure to child maltreatment are part of a single trajectory linking early life insults to risk for adulthood depression. By intervening during pregnancy, rates of both child maltreatment and depressive disorders in the young adults could potentially be reduced. All expectant women could be screened for depression and those identified offered prioritised access to psychological therapies – as indeed is currently recommended by the UK guidelines on perinatal mental health. 57 Moreover, our findings will inform the current debate on the use of antidepressants during pregnancy, by highlighting the adverse consequences of not treating depression. Reference Ross, Grigoriadis, Mamisashvili, Vonderporten, Roerecke and Rehm58
Acknowledgements
We thank Ms J. Wertz, Dr T. Chua, Ms H. Allen, Dr A. Mills and Dr G. Schmücker (King's College London), and Dr C. Waters and Prof D. Hay (Cardiff University) for their research contribution to the SLCDS, and we are especially grateful to the families of the SLCDS who continue to give so generously of their time.







eLetters
No eLetters have been published for this article.