‘Eating Attitude’ is a term used globally to describe the beliefs, thoughts, feelings and behaviours related to food(Reference Alvarenga Mdos, Scagliusi and Philippi1). People develop positive or negative attitudes leading to actions consistent with cognitions and emotions towards food. Diverse approaches to food might have consequences on general well-being, and psychological components of eating attitudes might be important determinants of health.
Rapid changes in food choices and behaviours have occurred lately, with people desiring to stay slim(Reference Fatima and Ahmad2–Reference Saleh, Salameh and Yhya5). Unhealthy eating attitudes, related to abnormal preoccupations with food and weight, such as continuous concerns about controlling and losing weight, food restriction and amplified anger and bad temper when hungry, had quickly emerged and resulted in severe eating disorders (Reference Griffiths, Murray and Krug6,Reference Cavazos-Rehg, Krauss and Costello7) . Eating disorders, defined as abnormal or disturbed eating behaviours, are highly encountered and include harmful eating attitudes with severe distress or concerns about body weight or shape(8). According to many studies, the prevalence of unfavourable eating attitudes varies between 10 and 16 % in America(Reference Jones, Bennett and Olmsted9,Reference Vilela, Lamounier and Dellaretti Filho10) , 3–13·7 % in Europe(Reference Preti, Girolamo and Vilagut11) and 4–30 % in Asia(Reference Fatima and Ahmad2,Reference Saleh, Salameh and Yhya5,Reference Musaiger, Al-Mannai and Tayyem12,Reference Yu, Lu and Tian13) . Arab countries, especially Lebanon, are affected by westernisation and tend to adopt western traditions in everything, including eating attitudes. Thus, Lebanese people (mostly women) favour fasting or restrained eating to lose weight(Reference Griffiths, Murray and Krug6).
Psychological factors and emotional status play very important roles in food choices and behaviours(Reference Babicz-Zielińska14). Negative emotions could have an impact on the behaviour of individuals by reducing their actions, which usually involves avoidance of the stimulus or the activity(Reference Babicz-Zielińska14). Emotional regulation can affect the eating attitude as it plays an influential role in daily food intake and may cause what is known as ‘emotional overeating’(Reference Gianini, White and Masheb15). Furthermore, stress (often coupled with depression and anxiety when chronic) and anxiety are also associated with disordered eating(Reference Farrow, Haycraft and Meyer16,Reference Yau and Potenza17) . Indeed, studies have shown that anxiety appears much earlier than eating disorders, making it a cause of binge eating(Reference Levinson and Rodebaugh18).
Moreover, anxiety showed some association with fasting, especially ‘social appearance anxiety’, where people get anxious about what society may think of their appearance. Studies have shown that a higher frequency of use of social media resulted in high rates of eating disorders: pressure may lead to body dissatisfaction, lowered self-esteem and urge to become extremely skinny, especially in women(Reference Griffiths, Murray and Krug6,Reference Cavazos-Rehg, Krauss and Costello7,Reference Barcaccia, Balestrini and Saliani19) . Consequently, the frequency of restrained eating is increasing worldwide; people stop eating voluntarily to lose weight and become skinny(Reference Yau and Potenza17), without knowing that this will increase the food intake after some time, leading to binge eating again.
Furthermore, studies have demonstrated that intense physical activity is linked to eating disorders(Reference Shroff, Reba and Thornton20,Reference Dalle Grave, Calugi and Marchesini21) . An excessive workout is often used as an approach to cope with emotional conditions, either by reinforcing mood or by avoiding destructive thoughts related to not exercising(Reference Taranis and Meyer22). On the other hand, people with food addiction are less active and prefer spending their leisure time sitting rather than walking or doing any physical activity(Reference Li, Pursey and Duncan23). Also, education level has an impact on food behaviours and attitudes(Reference Li and Powdthavee24–Reference Finger, Tylleskär and Lampert26): uneducated persons tend to consume large amounts of junk, high energetic content food(Reference Finger, Tylleskär and Lampert26), while more educated people read and analyse health facts and choose healthier lifestyles(Reference Li and Powdthavee24).
In Lebanon, there is a need to assess the risk of eating-related diseases and eating attitudes using appropriate tools; one of the most used is the Eating Attitude Test (EAT-26)(Reference Garner, Olmsted and Bohr27). The EAT-26 was designed to diagnose anorexia nervosa but has been found useful in non-clinical settings to screen for disordered eating attitudes, particularly atypical preoccupation with food and weight(Reference Garner, Olmsted and Bohr27). This test was validated in Mexico as a secondary prevention tool to modify public health programmes(Reference Arellano, Torres and Rivera28), and in Spain(Reference dos Santos Alvarenga, Francischi and Fontes29,Reference Castro, Toro and Salamero30) , where it is known as Disorder Eating Attitude Scale. It was also validated as a very sensitive method in Italy(Reference Dotti and Lazzari31), as a sensitive and specific useful tool in non-western countries(Reference Nasser32) and as the most reliable and commonly used self-report tool for eating disorders worldwide. Additionally, the EAT-26 was validated in Arabic among a representative sample of female students in Riyadh, Saudi Arabia(Reference al-Subaie, al-Shammari and Bamgboye33). However, it was not validated in the Lebanese dialect and among the general population; hence, the importance of its validation to use it as a screening tool for disordered eating attitudes.
Therefore, the primary objective of the study is to validate the Arabic version of the EAT-26 and identify factors (such as depression, stress, anxiety, emotion regulation and body dissatisfaction) that might be associated with disordered eating among a sample of the Lebanese population.
Methods
Participants
This cross-sectional study conducted between January and May 2018, enrolled 811 community dwelling participants using a proportionate random sample from all Lebanese governorates (Beirut, Mount Lebanon, North, South and Bekaa). Each governorate is divided into Caza (stratum). Two villages were randomly selected from the list of villages provided by the Central Agency of Statistics in Lebanon. Participants were randomly selected from each village. Prior to participation, individuals were briefed on the study objectives and methodology and were assured of the anonymity of their participation. No financial reward was given to the participants, and they had the right to accept or refuse to participate in the study. Those who agreed to participate were asked to read and sign a written consent form.
All participants above 18 years of age were eligible to participate. Excluded were those who refused to fill out the questionnaire and those suffering from cognitive impairment as reported by a family member. Data collection was performed through personal interviews with participants by a trained study-independent clinical psychologist, who clinically evaluated the level of psychiatric illness to exclude participants with psychiatric problems. The same methodology was used in previous papers from this project(Reference Haddad, Obeid and Akel34–Reference Sfeir, Haddad and Salameh36).
Minimal sample size calculation
According to Comrey and Lee(Reference Comrey and Lee37), ten observations are needed for each scale item for the validation process. Since the EAT includes twenty-six items, a minimal sample of 260 participants was deemed necessary.
Procedure
Study-independent trained clinical psychologists collected data by performing personal interviews with the participants that required approximately 60 min. Completed questionnaires were collected back by the interviewer and sent for data entry. During the data collection process, the anonymity of the participants was guaranteed.
The full sample was randomly divided into two separate samples (406 for the first sample and 405 for the second sample). To ensure the validity of the results from sample 1, the score of the EAT scale used in sample 1 was tested on another sample (sample 2).
Questionnaire
The questionnaire used during the interview was in Arabic, the native language of Lebanon. The first part assessed the socio-demographic details of the participants. The BMI was calculated as follows: weight (kg) divided by the square of the height (metres), as self-reported by each participant. Consumption of alcohol, caffeinated beverages and tobacco was categorised into dichotomous variables (yes/no). The physical activity index is a frequently used indicator of physical activity at the population level. This index is based on responses to a series of questions about the intensity, frequency and duration of participation in physical activity during leisure time. The Total Physical Activity Index was calculated by multiplying the intensity, duration and frequency of daily activity(Reference Weary-Smith38). The education level was categorised into four groups: primary, complementary, secondary and university; however, when stratifying over education, the four groups were reduced to two, low level of education (illiterate, primary and complementary) and high level of education (secondary, university).
The second part of the questionnaire consisted of the perception of eating habits among participants. The questions were selected from previous articles about eating disorders(Reference Salafia, Jones and Haugen39–Reference Bosi, Çamur and Güler41). The final part included the following scales.
Eating Attitude Test
The EAT is used to assess disordered food attitude(Reference Garner and Garfinkel42). The questionnaire comprises twenty-six questions each with six response options, varying from infrequently/almost never/never (0) to always (3). The total score is calculated by summing all questions answers and can vary from 0 to 78. A score of 20 or above indicates possible disordered food attitudes(Reference Garner, Olmsted and Bohr43). In the current study, the Cronbach’s α was 0·908.
Body dissatisfaction subscale of the Eating Disorder Inventory second version
In the present study, body dissatisfaction subscale of Eating Disorder Inventory second version was used to measure body disturbance. The body dissatisfaction subscale contains nine items assessing levels of dissatisfaction with their overall body shape as well as specific body parts. A four-point Likert scale was used ranging from 0 (sometimes, rarely and never) to 3 (always). Higher scores indicate more body dissatisfaction(Reference Garner44). In the current study, the Cronbach’s α was 0·779.
Perceived Stress Scale
The questions in the Perceived Stress Scale ask about feelings and thoughts during the last month(Reference Cohen, Kamarck and Mermelstein45). The Perceived Stress Scale is a ten-item scale, with answers ranging from never (0) to almost always (4). Items 4, 5, 7 and 8 are reversed items. The total score is calculated by summing the ten items with higher scores indicating more perceived stress(Reference Cohen, Kamarck and Mermelstein45). In the current study, the Cronbach’s α was 0·709.
Hamilton Anxiety Rating Scale
The Hamilton Anxiety Rating Scale, validated in Lebanon(Reference Hallit46), consists of fourteen symptom-defined elements and targets both psychological and somatic symptoms. Each item is scored on a basic numeric scoring of 0 (not present) to 4 (severe). The total score ranging from 0 to 56, with higher scores indicating higher anxiety(Reference Thompson47). In the current study, the Cronbach’s α was 0·912.
Hamilton Depression Rating Scale
The Hamilton Scale for Depression, validated in Lebanon(Reference Obeid, Hallit and Haddad48), is used to evaluate the severity of depression in patients who are already diagnosed as depressed. The total score is based on the sum of the first seventeen items only. Higher scores indicated higher depression(Reference Hamilton49). In the current study, the Cronbach’s α was 0·879.
Emotion Regulation Questionnaire (ERQ)
The Emotion Regulation Questionnaire is used to measure respondents’ tendency to regulate their emotions in two ways: (1) cognitive reappraisal and (2) expressive suppression. The cognitive reappraisal facet is a way of managing and controlling attention and cognitively changing the meaning of emotionally stimulating stimuli(Reference Gross50). It is considered a healthy emotion regulation strategy(Reference Gross50). The expressive suppression involves inhibition of emotional expressive behavior, thereby changing the emotional impact of a situation(Reference Gross and Levenson51). It is considered a less healthy emotion regulation strategy(Reference Gross and Levenson51). A ten-item scale ranging from 1 (strongly disagree) to 7 (strongly agree). Items 1, 3, 5, 7, 8 and 10 make up the cognitive reappraisal facet and items 2, 4, 6 and 9 make up the expressive suppression facet. Each facet’s scoring is kept separate. The higher the scores, the greater the use of the emotion regulation strategy(Reference Gross and John52). In the current study, the Cronbach’s α values for the cognitive reappraisal facet and the expressive suppression facet were 0·744 and 0·732, respectively.
The emotional eating, restrained eating, orthorexia nervosa and binge eating scales were used to test the convergent validity of the EAT scale.
Emotional Eating Scale
The Emotional Eating Scale, validated in Lebanon(Reference Rahme, Obeid and Sacre53) is a twenty-five-item scale with three-factor analytically derived subscales: anger, anxiety and depression. Participants rate the extent to which certain feelings lead to the urge to eat using a five-point Likert scale ranging from 0 (no desire to eat) to 4 (an overwhelming urge to eat). Higher scores indicate a reliance on using food to help managing emotions(Reference Arnow, Kenardy and Agras54). In the current study, the Cronbach’s α was 0·957.
Dutch Restrained Eating Scale
Recently, Dutch Restrained Eating Scale, validated in Lebanon(Reference Saade, Hallit and Haddad55), is composed of ten items scored using a five-point Likert scale, varying from 1 (never) to 5 (always). By dividing the total items score by the total number of items, the score for this scale was acquired. A greater score would show higher degree of restrained eating(Reference Van Strien, Frijters and Van Staveren56) (Cronbach’s α = 0·928).
Orthorexia Nervosa Scale – ORTO-15
The Orthorexia Nervosa Scale, validated in Lebanon(Reference Haddad, Hallit and Akel57), is a measure instrument comprising fifteen multiple-choice items. Orthorexia Nervosa Scale is a self-reported questionnaire(Reference Donini, Marsili and Graziani58) with a four-point Likert scale (never, sometimes, often and always). Lower scores would indicate higher levels of orthorexia tendencies and behaviours. In the current study, the Cronbach’s α was 0·822.
Binge Eating Scale
The Binge Eating Scale, validated in Lebanon(Reference Zeidan, Haddad and Hallit59), was originally developed to identify binge eaters within an obese population(Reference Gormally, Black and Daston60). It does not specify a time frame and presents a series of differently weighted statements for each item, from which respondents select the statement that best describes their attitudes and behaviours. This yields a continuous measure of binge eating pathology of 0–46. The severity of binge eating was divided into three categories as follows: < 17 as non-binging, between 18 and 26 as moderate binging and ≥ 27 as severe binging(Reference Greeno, Marcus and Wing61). The Binge Eating Scale has good test–retest reliability (r = 0·87, P < 0·001). In the current study, the Cronbach’s α was 0·862.
Forward and back translation procedure
Forward translation was first conducted by a single bilingual translator, whose native language is Arabic and fluent in English. An expert committee formed by healthcare professionals and a language professional verified the Arabic-translated version. A backward translation was then performed by a native English speaker translator, fluent in Arabic and unfamiliar with the concepts of the scales. The back-translated English questionnaire was subsequently compared with the original English one, by the expert committee, aiming to discern discrepancies and to solve any inconsistencies between the two versions. The process of forward-back translation was repeated until all ambiguities disappeared.
Statistical analysis
SPSS software version 25 was used to conduct data analysis. A descriptive analysis was done using the counts and percentages for categorical variables and mean and sd for continuous measures. We checked the distribution normality for the EAT scale using the Shapiro Wilk test. Since the assumption of normality was not normally distributed, the comparison of means was performed using the non-parametric tests (Kruskal–Wallis and Mann–Whitney tests). Spearman correlation was used for the linear correlation between continuous variables. For categorical variables, the χ 2 and Fisher exact tests were used.
A stepwise linear regression was conducted, taking the EAT score as the dependent variable. All variables that showed a P < 0·1 in the bivariate analysis were considered important variables to be entered in the model in order to eliminate potentially confounding factors as much as possible. Afterwards, other stepwise linear regressions taking the EAT as the dependent variable but stratified over education level were conducted (stratification analysis).
Two different methods were used to confirm the EAT questionnaire construct validity. First, a factor analysis was run using the principal component analysis technique, run on sample 1. Since the extracted factors were found to be significantly correlated, the promax rotation technique was used. To ensure the model’s adequacy, the Kaiser–Meyer–Olkin measure of sampling adequacy and Bartlett’s test of sphericity were calculated. Factors with an eigenvalue higher than one were retained. Moreover, Cronbach’s α was recorded for reliability analysis for each scale.
Second, a confirmatory factor analysis was carried out in sample 2. To assess the structure of the instrument, the maximum likelihood method for discrepancy function was used. Several goodness-of-fit indicators were reported: relative chi-square (χ 2/df), root mean square error of approximation, goodness of fit index and the adjusted goodness of fit index. The goodness of fit index was calculated by the value of χ 2/df (cut-off values <2–5). The root mean square error of approximation tests the fit of the model to the covariance matrix. As a guideline, values of <0·05 indicate a close fit and values below 0·11 an acceptable fit. The goodness of fit index and adjusted goodness of fit index are χ 2-based calculations independent of df. The recommended thresholds for acceptable values are ≥0·90(Reference Marsh, Hau and Wen62). A P < 0·05 was considered significant.
Results
Out of 1000 questionnaires distributed, 811 (81·1 %) were completed and collected. The socio-demographic characteristics of the participants in the first sample are summarised in Table 1. The results from sample 1 showed that disordered eating attitudes was found in 95 (23·8 %) (95 % CI 0·152–0·323) participants, whereas 305 (76·2 %) participants had appropriate eating attitudes (95 % CI 0·715–0·810). No significant difference was found between samples 1 and 2 for all the variables (socio-demographic variables, smoking, alcohol and carbonated beverages intake, and physical activity).
Table 1 Socio-demographic characteristics of the study sample
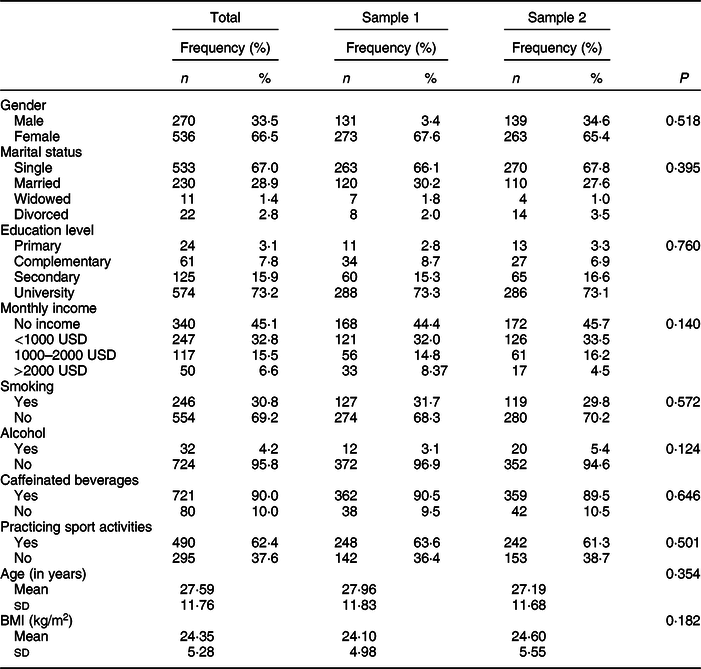
The χ 2 and Fisher exact tests were used to evaluate the association between categorical variables, and the Mann–Whitney test was used to evaluate the association between the age, body mass index (BMI) and the sample group.
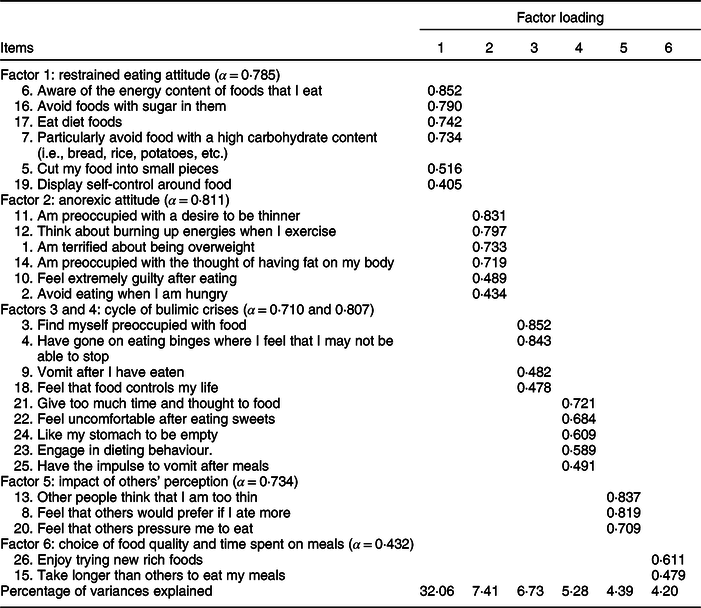
Exploratory factor analysis on sample 1
Out of all the items of EAT-26 scale, none of the items was removed since no one over-correlated to each other (r > 0·9), or had a low loading on factors (<0·3) or even had a low communality (<0·3). The factor analysis for the EAT scale was run over half of the original sample (total n 403). The EAT-26 scale items converged over a solution of six factors that had an eigenvalue over 1 (factor 1 = restrained eating attitude, factor 2 = anorexic attitude, factors 3 and 4 = cycle of bulimic crises, factor 5 = impact of others’ perception and factor 6 = choice of food quality and time spent on meals; total variance explained = 60·07 %, Kaiser-Meyer-Olkin = 0·911, Bartlett’s test of sphericity P < 0·001 and Cronbach’s α = 0·895) According to the promax rotated matrix, the components are summarised in Table 2.
Table 2 Promax rotated matrix of the eating attitude eating scale items
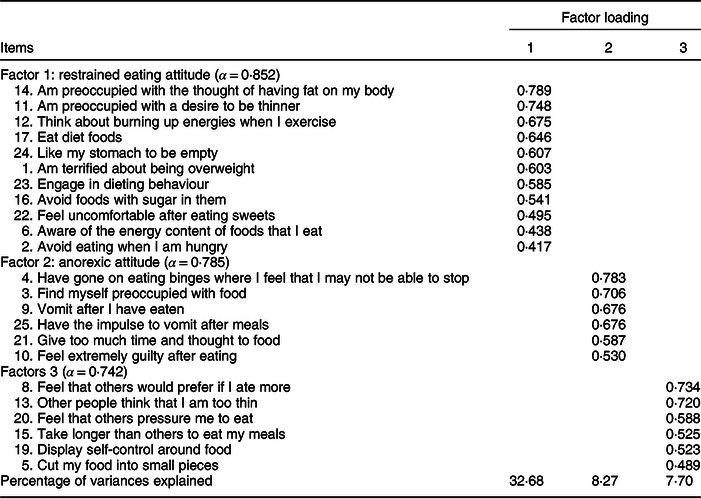
Another factor analysis was run by forcing a rotation over a three-factor solution instead of six; three items (2, 18 and 26) were removed, leaving a total of 23 items (total variance explained = 48·73 %, Kaiser–Meyer–Olkin = 0·904, Bartlett’s test of sphericity P < 0·001). According to the promax rotated matrix, the components are summarised in Table 3.
Table 3 Promax rotated matrix of the eating attitude eating scale items using a forced three-factor solution
Confirmatory factor analysis on sample 2
A confirmatory factor analysis was run on sample 2, using the structure obtained in sample 1. The following results were obtained: the maximum likelihood χ 2 = 723 and df = 300, which gave a χ 2/df = 2·4. For non-centrality fit indices, the Steiger–Lind root mean square error of approximation was 0·13 (0·131–0·142). Moreover, the Joreskog goodness of fit index equaled 0·767 and adjusted goodness of fit index equaled 0·711.
Bivariate analysis conducted on the whole sample
A significantly higher mean of EAT score was found in participants following a diet (18·85 v. 11·66, P < 0·001), exercising (16·66 v. 12·06, P < 0·001), vomiting (25·83 v. 12·49, P < 0·001), taking diet pills (23·43 v. 12·74, P < 0·001), starving to lose weight (21·26 v. 11·84, P < 0·001) in the last 30 d and weighing daily (20·09 v. 12·49, P = 0·005) compared with those who do not follow these eating habits. Also, a significantly higher mean of EAT score was found in participants who received comments from their family members about losing weight (16·75 v. 12·48, P < 0·001), those who have been insulted (21·84 v. 12·79, P < 0·001), those who have been in a bad relationship (15·35 v. 13·16, P = 0·027), had a family history of eating disorders (17·18 v. 12·82, P = 0·001) and felt pressure from media to lose weight (19·68 v. 12·45, P < 0·001) compared with those who do not agree with these statements.
In addition, a higher body dissatisfaction (r = 0·135), higher restrained eating (r = 0·229), higher anxiety (r = 0·285), higher depression (r = 0·302), higher physical activity (r = 0·092), higher binge eating (r = 0·277) and higher emotional eating (r = 0·143) were significantly but weakly associated with higher EAT scores. However, higher orthorexia scores (lower orthorexia tendencies and behaviours) (r = −0·256) were significantly associated with lower EAT scores (more appropriate eating) (Tables 4 and 5).
Table 4 Spearman correlation between Eating Attitude Test (EAT) and other scales
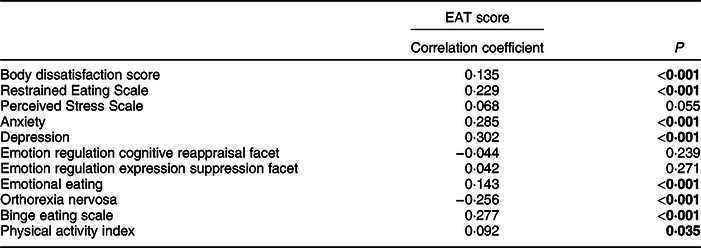
Numbers in bold indicate significant P-values. Pearson correlation coefficient was used to evaluate the association between the EAT score and the continuous variables.
Table 5 Bivariate analysis of the factors associated with the Eating Attitude Test (EAT) score
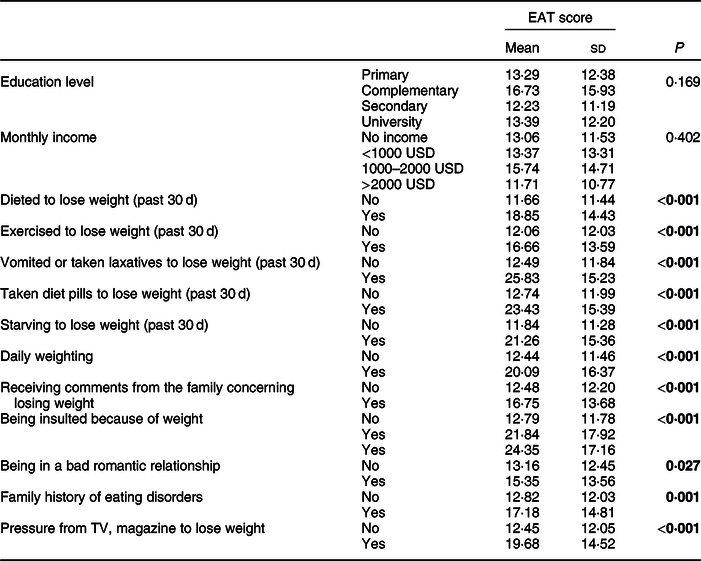
Numbers in bold indicate significant P-values; the Mann–Whitney test was used to evaluate the association between the EAT score and dichotomous variables, whereas the Kruskal–Wallis test was used to evaluate the association between the EAT score and the categorical variables.
Multivariable analysis conducted on the whole sample
The results of a first linear regression, taking the EAT score as the dependent variable and the socio-demographic characteristics only as independent variables, showed that secondary (β = −5·87) and university level of education (β = −5·26) were significantly associated with lower EAT score (appropriate eating attitudes) (Table 6, model 1).
Table 6 Multivariable analysis
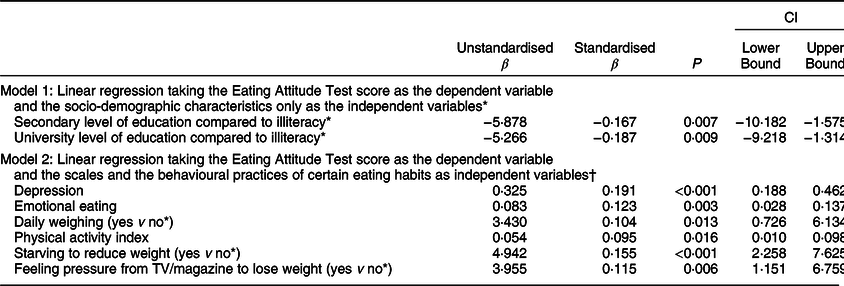
* Reference group; Variables entered in model 1: age, BMI, gender, marital status, monthly income and education level.
† Variables entered in model 2: age, BMI, gender, marital status, monthly income, education level, body dissatisfaction, anxiety, depression, emotional eating, binge eating, physical activity index, dieted to lose weight, exercised to lose weight, vomited or taken laxatives to lose weight, taken diet pills to lose weight, starving to lose weight, daily weighting, receiving comments from the family concerning losing weight, being insulted, being physically abused, being sexually abused, being in a bad romantic relationship, family history of eating disorders, pressure from TV, magazine to lose weight. Nagelkerke R 2 = 26.5 %.
The results of a second stepwise linear regression, considering the EAT score as the dependent variable and the scales and the opinion about eating habits as independent variables, showed that higher depression (β = 0·325), higher emotional eating (β = 0·083), daily weighing (β = 3·430), higher physical activity (0·05), starving to reduce weight (β = 4·94) and receiving pressure from TV/magazine to lose weight (β = 3·95) were significantly associated with higher EAT scores (disordered eating attitudes) (Table 6, model 2).
Stratification over education level conducted on the whole sample
A first linear regression, taking the EAT-26 as the dependent variable and the socio-demographic characteristics as independent variables, stratified over education level, showed that low income (β = 11·21) was significantly associated with higher EAT-26 scores (disordered eating attitudes) in the low-educated group. Higher BMI (β = 0·24) and intermediate income (β = 3·86) were significantly associated with higher EAT-26 scores (disordered eating attitudes), whereas increase age (β = −0·11) was significantly associated with lower EAT-26 scores (appropriate eating attitudes) in the high-educated group.
A second linear regression analysis taking the EAT-26 as the dependent variable and the scales and the opinion about eating habits as independent variables, stratified over education level, showed that starving to reduce weight (β = 14·00) was significantly associated with higher EAT-26 scores (disordered eating attitudes) in the low-educated group. Daily weighting (β = 3·17), higher depression (β = 0·30), receiving pressure from the TV/magazine to lose weight (β = 4·24) and physical activity (β = 0·07) were significantly associated with higher EAT scores (disordered eating attitudes) in the high-educated group (Table 7).
Table 7 Stratification over the education level*
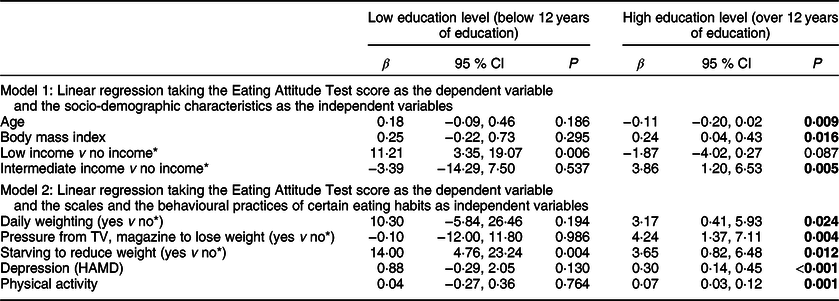
* Reference group; Low education level includes illiterate, primary and complementary categories, whereas the high education level includes the secondary and university categories; numbers in bold indicate significant P-values.
Discussion
To the best of our knowledge, this is the first study to assess factors associated with the eating attitude among a representative Lebanese population sample. Our results showed that 23·8 % of participants had disordered eating attitudes, whereas 76·2 % had appropriate eating attitudes and are in line with other studies: a study carried out among young women from Brazil (2003) showed a clinically significant disturbed eating behaviour in 16·5 % of women, with more disordered eating attitudes among those aged 16–19 years and among overweight/obese women(Reference Nunes, Barros and Anselmo Olinto63). The prevalence of disorder eating attitudes in western countries varies from 0·4 % in Spain(Reference Ballester Ferrando, De Gracia Blanco and Patino Maso64) to 33 % in Australia(Reference Grigg, Bowman and Redman65).
In our study, EAT scale items converged over a solution of six factors explaining a total of 60·07 % of the variance and leading to an internal consistency of Cronbach’s α = 0·895. The validation of the EAT in Mexico showed five factors (constituting a total of 46·6 % of the variance): ‘dietary restraint’, ‘bulimia’, ‘drive of thinness’, ‘food preoccupation and perceived social pressure’ and with an internal consistency of Cronbach’s α = 0·9(Reference Alvarez-Rayón, Mancilla-Díaz and Vázquez-Arévalo66). The Spanish validation in its turn yielded three factors explaining 41 % of the variance, with a reliability coefficient of 0·93(Reference Castro, Toro and Salamero30). This test was also validated in Italy and consisted of four phases: ‘Item generation, internal consistency and reliability analysis, normative data generation, and validity analysis’, with an internal consistency Cronbach’s α values of 0·90 and 0·93(Reference Schindler, Mozzanica and Monzani67). Thereby, Cronbach’s α values show a very small variation between different countries: this is due to the fact that the Cronbach’s α is not a characteristic for the whole test but for the sample took in the test; it might vary if the test is done on a general population or a sample composed of people having a specific characteristic, for example. However, these obtained values were almost similar, meaning these populations share very close eating attitudes.
Receiving pressure from TV or magazines to lose weight, starving to reduce weight (in the past 30 d), higher depression and higher physical activity were associated with higher EAT scores (disordered eating attitudes) in the better educated group. Previous studies revealed that physical activity levels explained the relationship between prudent dietary patterns, depressive symptoms(Reference Jacka, Cherbuin and Anstey68) and severity of anxiety symptoms(Reference Bittencourt, Lucena-Santos and Moraes69); specifically, lower scores of the healthy dietary pattern and higher scores of the unhealthy dietary pattern independently predicted increased depressive symptoms across time without establishing any correlation with educational level. Furthermore, social media exposure was associated with eating pathology, independent of direct media exposure and other cultural exposures. The different variables explored were not directly correlated with the level of education in the literature. Thus, our findings, related to the stratification by level of education, warrant further investigation to better understand the relation between the level of education and the different variables associated at the same time with the score of EAT.
In the current study, higher depression levels were found to be significantly associated with more disordered eating attitudes (higher EAT scores), similarly to other studies(Reference Yau and Potenza17,Reference Barcaccia, Balestrini and Saliani19,Reference Costarelli and Patsai70) , knowing that depression is often due to an anxiety feeling over a long period of time(Reference Cole, Peeke and Martin71). These unwanted feelings are usually accompanied by an intensified need for eating high-sugar food or high-fat food as a self-medication(Reference Yau and Potenza17). This might be attributed to a greater body concern of women nowadays for having an ideal social media body to look ‘beautiful and attractive’(Reference Griffiths, Murray and Krug6). In fact, the desire to become similar to TV characters increased the anxiety and depression among women(Reference Barcaccia, Balestrini and Saliani19), and these unpleasant feelings resulted sometimes in excessive eating(Reference Gan, Nasir and Zalilah72). Clearly, peer pressure and social media stars have a bad influence on individuals, especially women, to the point where body image dissatisfaction became a ‘normative discontent’(Reference Farrow, Haycraft and Meyer16). Studies show that a higher frequency of social media use, especially the image-centric platforms, resulted in greater body dissatisfaction concern(Reference Griffiths, Murray and Krug6). Effectively, these social media platforms tend to promote disordered eating behaviours by always encouraging the ‘thin ideal’ leading to disastrous weight loss tendencies(Reference Cavazos-Rehg, Krauss and Costello7), fasting, higher depression, daily weighing, etc.
Therefore, people are tending to adapt starving methods such as fasting, purging, chronic dieting(Reference Barcaccia, Balestrini and Saliani19) or the daily weighing method, thinking that it would help them lose weight. Although daily weighting might help them manage their weight by always keeping an eye on it(Reference Vanwormer, French and Pereira73), starvation for example, will lead to even more weight gain, because our body does not recognise the difference between this procedure and dieting.
In return, emotional eating was proven to be strongly related to disordered eating attitudes, which is consistent with the results of other studies(Reference Gianini, White and Masheb15). Many factors were evaluated in the literature to highlight the effect of emotions on eating attitudes. Individuals suffering from a lack of attention from parents or friends(Reference Tasca and Balfour74), and sexual and emotional abuse, showed higher levels of eating disorders, due to the compensation of affection in food, and for those people, food is known to be their ‘comfort zone’. Nowadays, people are exposed to numerous criticisms which creates among adolescents a huge personal irritation and a lower self-esteem, making it a crucial cause for restrained eating, followed by binge eating or over eating.
High education level had been found to be related with appropriate eating attitudes; thus, a stratification by level of education was found to be important. A low education level was related to unhealthy dietary habits: low-educated people tend to consume dense food, whereas high-educated people have more positive attitudes in choosing foods as they acquire adequate health information that improves ability in choosing the right foods. A study conducted in 2013(Reference Le, Dallongeville and Wagner75) revealed that more educated people were more compliant with dietary guidelines and expressed more frequently positive attitudes towards healthy eating than low-educated people. Our results showed that low income was associated with higher disordered eating behaviour among low-educated groups. Less educated and low-income people have less healthy dietary habits, in part because of their higher priority for price and familiarity and their lower priority for health as a reason for buying food. A Finnish study showed that the level of education is related to individual priorities in the choice of food, where the more educated consume fewer energy-rich foods than those with less education(Reference Konttinen, Sarlio-Lähteenkorva and Silventoinen76). However, the association between the level of education and eating attitudes is not fully understood, and further studies are needed to investigate the attitudes and motives for making food choices.
Clinical implications
Healthcare professionals and dietitians should take into consideration the factors affecting a person’s eating attitude before prescribing a diet plan. Reasons differ from one person to another, as for some, eating disorders are a response to a major impact that affected their lives (early separation, stress, depression, anxiety, etc.), while for others, a non-balanced diet occurs following a low self-esteem and a self-objectification, due to the major influence of social media and TV programmes. Therefore, healthcare professionals should not only be responsible for prescribing trendy diet plans but also change their approach with patients and understand the reasons behind such disordered attitudes towards eating, then adapt the diet plan accordingly.
Limitations
An information bias might have occurred during the data collection since it was based on a self-report questionnaire. Our data could not be generalised to the entire population, since the group of well-educated female participants was more represented; this led us to conduct the stratified analysis and show differential results between high- v. low-educated subgroups. We would assume some kind of self-selection bias: maybe from each randomly selected household, younger and more educated individuals (e.g., students) participated in the study more often than older and less educated individuals. One additional limitation is the absence of an evaluation tool for obsessive-compulsive disorder and anorexic behaviours. It will be interesting to evaluate these behaviours among persons with disordered eating attitudes.
Conclusion
The current study found a high prevalence of disordered eating attitudes in the Lebanese population. Yet, the obtained results are considered preliminary, and further research should be conducted to prove it. Disordered eating attitudes and disorders will remain a controversial issue with respect to their relationship with psychological health and mental disorders. Future studies should point out at the importance of raising the awareness about social media, peer pressure and psychological influence on eating attitudes, since these are the main causes of eating disorders nowadays.
Acknowledgements
Acknowledgements: The authors would like to thank Marwan Akel, Karl Honein and Maria Akiki for their help in the data entry and all the participants who helped us during this project. Financial support: None. Conflict of interest: The authors have no conflicts of interest to report. Authorship: S.O. and S.H. conceived and designed the survey. C.H., S.H. and P.S. were involved in the statistical analysis and data interpretation. C.H. and C.K. wrote the manuscript. H.S., R.H. and N.K. reviewed the manuscript. All authors read the manuscript, critically revised it for intellectual content and approved the final version. Ethics of human subject participation: The current study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Psychiatric Hospital of the Cross Ethics and Research Committee. Written informed consent was obtained from all subjects/patients. Consent for publication: All authors gave their consent for publication. Availability of data and material: The authors do not have the right to share any data information as per their institutions policies.









