‘The issue is not food, nor nutrients, so much as processing’. With this title, a commentary published in 2009 presented a new paradigm to relate diet and health. It proposed that food processing has become the main shaping force of the global food system and the main determinant of the nature of diets and related states of health and well-being( Reference Monteiro 1 ). As part of the new paradigm, a classification of foods based on the nature, extent and purpose of food processing was devised( Reference Monteiro 1 ) and further developed and called NOVA( Reference Monteiro, Cannon and Moubarac 2 – 4 ).
NOVA identifies as ultra-processed foods industrial food and drink formulations made mostly or entirely from substances derived from foods, together with additives. The ingredients, the various processing techniques and the sequences of stages used for the manufacture of ultra-processed foods (hence ‘ultra-processed’) are designed to create durable, accessible, convenient, hyper-palatable, highly profitable ready-to-eat, ready-to-drink or ready-to-heat products liable to displace all other NOVA food groups – natural or minimally processed foods, processed culinary ingredients and processed foods – and the dishes and meals made with them( Reference Monteiro, Cannon and Moubarac 2 – 4 ).
Examples of typical ultra-processed foods are soft drinks; sweet or savoury packaged snacks; confectionery, mass-produced packaged breads, buns, biscuits and cakes; hot dogs, poultry and fish ‘nuggets’ and other reconstituted meat products; ‘instant’ soups and noodles; industrialized desserts; and industrially pre-prepared pizzas, pies and other dishes and meals( Reference Monteiro, Cannon and Moubarac 2 – 4 ).
Analyses of national household food purchase surveys and national dietary surveys conducted in several countries( Reference Martinez Steele, Baraldi and Louzada 5 – Reference Marrón-Ponce, Sánchez-Pimienta and Louzada 13 ) show a great variation in the estimates of the dietary contribution of ultra-processed foods. These ranged from 21·5 % of total dietary energy in Brazil in 2008–2009( Reference Louzada, Martins and Canella 9 ) to 57·9 % in the USA in 2009–2010( Reference Martinez Steele, Baraldi and Louzada 5 ). In 2003, annual sales of selected ultra-processed foods in eighty countries also have shown great variation, ranging from 6·7 kg per person in India to 307·2 kg per person in the USA( 14 ). From 2000 to 2013, in the eighty countries taken together, the sales of these ultra-processed foods – carbonated soft drinks, sweetened breakfast cereals, sweet and savoury snacks, confectionery, ice cream, fruit juices, sports and energy drinks, spreads, sauces, and ready meals – increased by 43·7 %( 14 ).
Studies of national diets undertaken in the USA, Canada, Brazil and Chile have consistently shown that, as a group, ultra-processed foods have an obesogenic nutrient profile( Reference Martinez Steele, Baraldi and Louzada 5 , Reference Louzada, Martins and Canella 9 , Reference Crovetto, Uauy and Martins 10 , Reference Moubarac, Batal and Louzada 12 , Reference Louzada, Martins and Canella 15 – Reference Moubarac, Martins and Claro 17 ). Associations between the dietary content of ultra-processed foods and obesity have been shown in two cross-sectional studies undertaken in Brazil( Reference Canella, Levy and Martins 18 , Reference Louzada, Baraldi and Steele 19 ) and in one cohort study of middle-aged adults in Spain( Reference Mendonça, Pimenta and Gea 20 ). In twelve Latin American countries, a cross-sectional time-series analysis in the period 2000–2013 revealed a strong correlation between annual changes in sales of ultra-processed foods and annual changes in population-average BMI( 14 ). In Sweden, trends in sales of ultra-processed foods paralleled the rise of obesity prevalence between 1960 and 2010( Reference Juul and Hemmingsson 11 ).
The purpose of the present study was to assess household availability of NOVA food groups in a large number of European countries and to analyse the association between national availability of ultra-processed foods and national prevalence of obesity among adults.
Methods
The studied countries
The present study involved nineteen European countries for which we were able to obtain estimates for the same year, or within an interval of up to 5 years, for household availability of ultra-processed foods and also prevalence of obesity among adults. These countries were Austria, Belgium, Croatia, Cyprus, Finland, France, Germany, Greece, Hungary, Ireland, Italy, Latvia, Lithuania, Malta, Norway, Portugal, Slovakia, Spain and the UK.
Data sources on national household food availability
The data used to estimate the household availability of ultra-processed foods in the UK were extracted from the Living Costs and Food Survey (LCFS) conducted in the UK in 2008( 21 ). For the other countries, we extracted data from the Data Food Networking (DAFNE), a data depository of national household budget surveys conducted in Europe( 22 ). In this latter case, we always extracted data from the most recent survey available for each country.
The DAFNE databank
DAFNE consists of data collected through standardized national household budget surveys on all household expenditures to calculate consumer price indices and to analyse topics of social and economic interest( Reference Friel, Nelson and McCormack 23 ). Multistage stratified probability sampling procedures are used by the surveys. During data collection, the members of the participating households are asked to record all foods and drinks acquired (purchased, produced and gifts) during a certain period. The recording period is 14 d for all countries, except for Belgium, Germany and Sweden where it is 1 month. Foods and drinks consumed outside the house (e.g. in restaurants and canteens) are not recorded. In all countries, data collection is spread out over a year, which captures seasonal variations.
The national data sets are then analysed centrally( Reference Lagiou and Trichopoulou 24 ). Survey data are read, cleaned and managed to a format suitable for a between-countries analysis. To improve comparability, food, demographic and socio-economic data are subsequently classified under common groupings with the application of criteria and iterative cross-coding allowing the formation of operational classification schemes( Reference Lagiou and Trichopoulou 24 ).
The data collected by DAFNE in each country refer to quantities of foods (always including drinks) available for household member consumption. The national daily per capita household food availability is calculated by dividing the total household availability by the number of days of the referent time period and the total number of household members, without making allowances for waste or food given to domestic pets( Reference Lagiou and Trichopoulou 24 ). The results thus estimated are stored in the DAFNE databank( 22 ). Because the level of detail recorded in each survey varies among countries, ranging from very detailed records to those that are more aggregated, food items in DAFNE are categorized into fifty-six groups and average per capita household food availability (in grams or millilitres) for each group is provided for each country( 22 ).
The LCFS databank
The LCFS provides estimates of household expenditures in the UK. It is used primarily to provide information for the national Retail Prices Index. This survey is similar to the DAFNE surveys. The LCFS units of study are private households selected by multistage stratified random sampling. The reference period for data on food is 14 d and, as with DAFNE households, data collection is spread evenly over the year. We coded the LCFS food items into the same groups used by DAFNE and then the average daily per capita household food availability (in grams or millilitres and also in dietary energy) for each group was added to the LCFS database( 21 ).
Data sources on obesity
National estimates of the prevalence of obesity (BMI≥30·0 kg/m2) among adults (people aged 18 years or above, except for Belgium which includes people aged 15 years or above) for each of the nineteen countries were derived from national surveys and were obtained from peer-reviewed papers or official national reports (see Table 2). The obesity estimate chosen for each country was selected to match as close as possible the survey year of the national household food budget survey. In nine countries, the obesity estimate corresponded to the year of the food availability estimate; in three, there was a gap of 1 year between the two estimates; in four, the gap was of 2 years; in two, of 3 years; and in one, of 5 years (as detailed below, this gap was treated as a potential confounding factor in the association between national food availability and national obesity prevalence).
Other variables used in the present study included estimates of national gross domestic product (GDP) per capita( 25 ), prevalence of smoking( 26 ) and prevalence of physical inactivity( 27 ). Physical inactivity was defined as vigorous-intensity physical activity of less than 20 min/d on at least 3 d/week, or moderate-intensity physical activity of less than 30 min/d on at least 5 d/week. The prevalence of smokers in Cyprus was not available and was imputed using multiple imputation by chained equations( Reference Royston and White 28 , Reference White, Royston and Wood 29 ), using as predictors GDP per capita, proportion of population living in rural areas, proportions of individuals aged 0–14, 15–64 and 65 years or above, prevalence of obesity and prevalence of physical inactivity.
Food classification
We have classified each of the fifty-six food groups in DAFNE and LCFS databanks using NOVA. As said above, NOVA is based on the nature, extent and purpose of the industrial processing applied to foods before their consumption( Reference Monteiro 1 – 4 ). It includes four groups.
Of these, Group 1 is of unprocessed or minimally processed foods, such as fresh, dry or frozen fruits and vegetables; packaged grains and pulses; grits, flakes or flours made from corn, wheat, rye; pasta, fresh or dry, made from flours and water; eggs; fresh or frozen meat and fish; fresh or pasteurized milk. Group 2 is of processed culinary ingredients, including sugar, oils, fats, salt and other substances extracted from foods or nature, used in kitchens to season and cook unprocessed or minimally processed foods and to make dishes and meals. Group 3 is of processed foods, such as vegetables preserved in brine, fruits in syrup, salted meat and fish, cheese, freshly made unpackaged breads and other similar ready-to-consume products manufactured with the addition to unprocessed or minimally processed foods of salt, sugar, oil or other substances of culinary use.
Group 4, of particular interest in the present study, is of ultra-processed foods. These are industrial formulations manufactured mostly or entirely from sugar, salt, oils and fats, starches and many substances derived from foods but not normally used in kitchens, and additives including those used to imitate the sensory qualities of natural foods or to disguise undesirable qualities of the final product. Ultra-processed foods include sweet, fatty or salty packaged snack products; ice cream, chocolate, candies; mass-produced packaged breads, cookies, pastries, cakes; breakfast cereals; ‘energy’ bars; preserves; margarines; carbonated drinks, ‘energy’ drinks; milk drinks, including ‘fruit’ yoghurts; cocoa drinks; infant formulas, follow-on milks, other baby products; ‘health’ and ‘slimming’ products such as powdered or ‘fortified’ meal and dish substitutes; and many ready-to-heat products including pre-prepared pies and pizza dishes, burgers, hot dogs, poultry and fish ‘nuggets’, and other reconstituted meat products, and powdered and packaged soups, noodles and industrial desserts. A detailed definition of each NOVA food group, examples of food items classified in each group and the rationale underlying the classification are shown elsewhere( Reference Monteiro 1 – 4 , Reference Moodie, Stuckler and Monteiro 30 , Reference Ludwig 31 ).
Bread, frequently consumed by Europeans, may be either processed or ultra-processed. Processed breads include those made often by hand essentially from flour, yeast, water and salt (nuts, dried fruits, vegetable oils, butter and other culinary ingredients may also be added). Ultra-processed breads are industrialised, and include substances not used in kitchens, such as hydrogenated fat, high-fructose corn syrup, emulsifiers, preservatives, and flavours, colours and other additives used to make the product more appealing. Since household budget surveys do not describe the list of ingredients of food items, we could not assess directly the shares of processed and ultra-processed breads consumed in each country. We used as a proxy the proportion of sales in each country of ‘artisanal bread’ and ‘industrial bread’, respectively, as estimated by the Low Energy Ovens Market Study( 32 ).
Data analysis
As a first step, we converted the national average daily per capita household food availability (in grams or millilitres) of each food item in each country, except the UK, into energy values using the official US food composition tables( 33 ). In the case of the UK, all the food items in the database were already converted to energy using the official UK food composition table( 22 ). Then we aggregated similar items, such as different types of meat, of vegetable oils, of cheeses, of sweetened drinks, and so on. This aggregation resulted in nine subgroups within NOVA Group 1, three within Group 2, four within Group 3 and five within Group 4 (see Table 1). Due to the lack of information related to the household availability of milk and vegetable oils for Slovakia, the values for the average daily per capita household availability of these two items were imputed considering the median value of their availability (kcal/person per d) in the other eighteen countries.
Table 1 Distribution (%) of total household food availability (kcal/person per d) according to NOVA food groups in nineteen European countries (1991–2008)

* To convert to kJ/person per d, multiply kcal/person per d values by 4·184.
† Includes other cereals, legumes, nuts, eggs.
‡ Includes honey and syrups.
§ Includes salty snacks, breakfast cereals, margarine, sauces and spreads, and ready meals.
The household availability of NOVA groups and subgroups in each country was expressed as a percentage of total purchased dietary energy. The household availability of ultra-processed foods in each country was plotted against the estimate of the prevalence of obesity in the same country, and models of crude and adjusted linear regressions were then used to test the association between these two variables. Potential confounding factors for this association included countries’ GDP per capita, squared GDP per capita, difference in years between the year of the obesity survey and the household food budget survey, a dummy variable for the method to assess obesity (measured=0; self-reported=1), prevalence of physical inactivity and prevalence of smoking.
All analyses used the statistical software package Stata version 14.1.
Results
Table 1 shows the contribution of NOVA food groups and subgroups to the average household food availability in each of the nineteen countries.
The contribution of unprocessed or minimally processed foods ranged from 26·4 % of total purchased energy in Belgium and 27·6 % in Germany to 39·9 % in Cyprus and 43·4 % in Portugal. Most purchased items in this group were meat (from 4·9 % of total energy in Finland to 10·4 % in France), milk (from 0·6 % of total energy in Croatia to 10·7 % in Ireland), and pasta and wheat and other flours (ranging from 2·0 % in Spain to 13·4 % in Croatia).
Processed culinary ingredients contributed from 8·9 % of total purchased energy in Belgium and 10·4 % in the UK to 26·8 % in Greece and 28·0 % in Italy. Most purchased items were vegetable oils (from 0·7 % in Norway to 23·0 % in Greece) and table sugar (from 2·8 % in Belgium to 9·2 % in Slovakia).
Processed foods contributed from 8·7 % of total purchased energy in Ireland and 10·2 % in the UK to 26·9 % in France and 27·9 % in Slovakia. Most purchased items were fresh breads (from 2·5 % in the UK to 22·4 % in Croatia) and cheese (from 0·8 % in Ireland to 8·0 % in France).
Ultra-processed foods contributed from 10·2 % of total purchased dietary energy in Portugal and 13·4 % in Italy to 46·2 % in Germany and 50·7 % in the UK. The most commonly consumed ultra-processed foods were packaged breads (ranging from 1·6 % in Malta and Portugal to 16·3 % in Ireland), cakes, cookies and other baked products (ranging from 0·4 % in Croatia to 11·1 % in Belgium), reconstituted meat products (ranging from 1·5 % in Greece to 14·0 % in Germany) and sugar-sweetened beverages (ranging from 0·1 % in Italy to 11·0 % in Latvia).
Across the nineteen countries, the median average household availability amounted to 33·9 % of total purchased dietary energy for unprocessed or minimally processed foods, 20·3 % for processed culinary ingredients, 19·6 % for processed foods and 26·4 % for ultra-processed foods (data not shown).
Table 2 shows the prevalence of obesity among adults (men and women together) in the nineteen countries in the same year of (or close to) the assessment of household food availability. Prevalence of obesity ranged from 7·1 % in France and 8·2 % in Italy to 22·4 % in Finland and 24·5 % in the UK.
Table 2 Prevalence of obesity among adults in nineteen European countries (1991–2008)

Figure 1 shows the regression of the national prevalence of obesity v. the national average household availability of ultra-processed foods (percentage of total dietary energy).
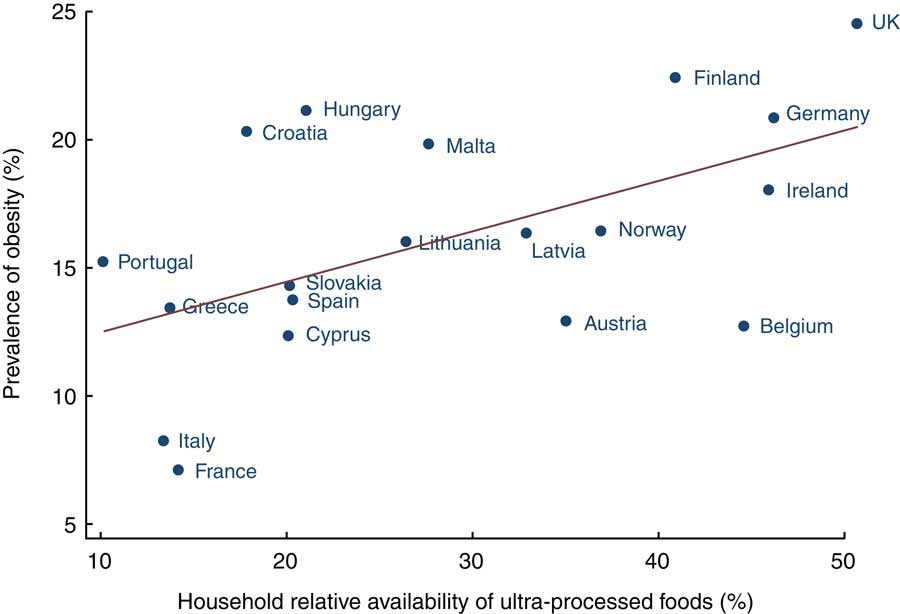
Fig 1 Regression of prevalence of obesity among adults v. household availability of ultra-processed foods (percentage of total energy) in nineteen European countries (1991–2008)
Table 3 shows regression coefficients for the association between the two variables. Both crude and adjusted coefficients were positive and statistically significant (P<0·05). The adjustment for potential confounders of the association between ultra-processed food household availability and obesity prevalence increased the regression coefficient.
Table 3 Results from linear regression models of obesity prevalence among adults (%) v. household availability of ultra-processed foods (% of total energy) in nineteen European countries (1991–2008)

GDP, gross domestic product.
* Adjusted for the countries’ per capita GDP, squared per capita GDP, time lag in years between the estimates on obesity and availability of ultra-processed foods, and measurement method of obesity (self-reported or directly measured).
† Adjusted as in model 1 plus for prevalence of physical inactivity and of smoking.
In the adjusted models, each percentage point increase in the household availability of ultra-processed foods resulted in an increase of 0·25 percentage points in obesity prevalence.
Discussion
In the current ecological study conducted with nationally representative data from nineteen European countries we found a significant positive association between household availability of ultra-processed foods and prevalence of obesity among adults. The association remained significant, and its magnitude increased, after adjustment for potential confounders. These included indicators of national income, prevalence of physical inactivity, prevalence of smoking, measured or self-reported prevalence of obesity, and time lag between the assessment of food availability and of obesity prevalence.
After adjustment for potential confounders, our regression model predicted that each percentage point increase in the energy share of ultra-processed foods would result in an increase of 0·25 percentage points in obesity prevalence. This means that a difference of 40 percentage points in the average contribution of ultra-processed foods to total household dietary energy, such as that existing between Portugal in 2005 and the UK in 2008, would determine a difference of 10 percentage points in obesity prevalence. This is not far from the difference between the actual prevalence of obesity in Portugal and the UK (15·2 and 24·5 %, respectively).
Previous population-based studies undertaken in Europe and other parts of the world also have shown positive associations between the consumption of ultra-processed foods and obesity and other diet-related chronic non-communicable diseases.
Dietary intake of ultra-processed foods was found to be positively associated with 9-year incidence of overweight and obesity( Reference Mendonça, Pimenta and Gea 20 ) and of hypertension( Reference Mendonça, Lopes and Pimenta 34 ) in a prospective cohort of Spanish middle-aged adult university graduates, after adjustment for potential confounders (age, sex, marital status, education level, baseline BMI, physical activity, hours of television watching, sleeping/siesta, smoking, snacking between meals and following a special diet) and after sensitivity analyses that excluded participants with a family history of obesity or hypertension and those with >3 kg weight gain in the 5 years before entering the cohort.
A cross-sectional time-series analysis of nationally representative data from twenty-five high-income countries (twenty of them European) in the period 1999–2008 found a positive association between per capita annual changes in average fast-food transactions (mostly of ultra-processed foods) and annual changes in age-standardized mean BMI, after adjustment for GDP, urban population, openness to trade, foreign direct investment, motor vehicle use, physical activity, and vegetables and fruits consumption( Reference De Vogli, Kouvonen and Gimeno 35 ). A similar analysis conducted in twelve Latin American countries in the period 2000–2013 showed a strong correlation between changes in national per capita sales of ultra-processed foods and changes in national population-mean BMI( 14 ).
In Brazil, greater household availability of ultra-processed foods was positively associated with higher prevalence of excess weight and obesity in all age groups, after control for several sociodemographic variables and percentage of expenditures on eating out of home( Reference Canella, Levy and Martins 18 ). Another Brazilian study reported that adolescents and adults in the highest quintile of intake of ultra-processed foods had significantly higher average BMI and higher odds of being obese than those in the lowest quintile, after control for several socio-economic variables and physical activity( Reference Louzada, Baraldi and Steele 19 ). Also in Brazil, a cohort study that followed children from 3–4 to 7–8 years of age found that intake of ultra-processed foods was associated with higher increases in total and LDL cholesterol, after control for several socio-economic variables, energy intake and BMI( Reference Rauber, Campagnolo and Hoffman 36 ). A cross-sectional study found an association between intake of ultra-processed foods and the metabolic syndrome in Brazilian adolescents after adjustment for potential confounders (energy intake, smoking and family history of dyslipidaemia)( Reference Tavares, Fonseca and Garcia Rosa 37 ).
The association between consumption of ultra-processed foods and obesity is consistent with the obesogenic nutritional profile of these foods. Population-based studies conducted in several countries have shown that, when compared with the fraction of the diet made of non-ultra-processed foods, ultra-processed foods overall have higher energy density( Reference Louzada, Martins and Canella 9 , Reference Crovetto, Uauy and Martins 10 , Reference Moubarac, Batal and Louzada 12 , Reference Marrón-Ponce, Sánchez-Pimienta and Louzada 13 , Reference Louzada, Martins and Canella 15 – Reference Moubarac, Martins and Claro 17 ), higher content of free sugars( Reference Martinez Steele, Baraldi and Louzada 5 , Reference Louzada, Martins and Canella 9 , Reference Crovetto, Uauy and Martins 10 , Reference Moubarac, Batal and Louzada 12 , Reference Marrón-Ponce, Sánchez-Pimienta and Louzada 13 , Reference Louzada, Martins and Canella 15 – Reference Moubarac, Martins and Claro 17 ) and of total fats( Reference Louzada, Martins and Canella 9 , Reference Crovetto, Uauy and Martins 10 , Reference Moubarac, Batal and Louzada 12 , Reference Marrón-Ponce, Sánchez-Pimienta and Louzada 13 , Reference Monteiro, Levy and Claro 16 , Reference Moubarac, Martins and Claro 17 ), and also lower content of dietary fibre( Reference Louzada, Martins and Canella 9 , Reference Crovetto, Uauy and Martins 10 , Reference Moubarac, Batal and Louzada 12 , Reference Marrón-Ponce, Sánchez-Pimienta and Louzada 13 , Reference Louzada, Martins and Canella 15 – Reference Moubarac, Martins and Claro 17 ).
Also, ultra-processed foods are typically less satiating and often have high glycaemic loads compared with other foods( Reference Fardet 38 ). They are also aggressively marketed often in big portion sizes and are typically designed to be consumed as snacks rather than as regular meals. All these factors induce energy overconsumption and thus overweight and obesity( Reference Cairns, Angus and Hastings 39 – 41 ).
The current paper presented results from the first cross-national ecological study of the association between ultra-processed food household availability and obesity in Europe. The strength of the study is the reliance on standardized data, the use of population-based, actual (non-modelled) estimates of the prevalence of obesity, and the consideration of multiple confounding factors.
The study has some limitations. First, close to half of the national estimates of obesity relied on self-reported data which are liable to underestimate the true prevalence of obesity. To reduce this potential bias, the method used to assess obesity (self-reported or directly measured) was included as a confounder in the adjusted linear regression model. Second, food purchase surveys do not include food consumed outside the home and do not allow for food wastage in the home. This limitation was reduced but not eliminated by use of a relative measure of food consumption: the proportion of ultra-processed foods in total dietary energy. Another limitation is that the times when the household budget survey and the obesity survey were conducted, although close, were not the same for all countries. To minimize this limitation, the number of years between the two surveys in each country was entered into the model as a potential confounding variable. An additional limitation was the use of a proxy to assess the share of processed and ultra-processed breads in each country. Sensitivity analyses undertaken after the exclusion of Slovakia, for which some food data were imputed, did not change the regression coefficients for the relationship between national ultra-processed food household availability and national prevalence of obesity.
The fact that national estimates for household food availability and obesity cover a large period of time (1991–2008) and that some estimates are relatively old, should not be considered a limitation of the study; its objective was not to assess the association between the two variables at one particular moment in time. Actually, the use of estimates that covered a long period contributed to increase the variability of both variables and this increases the power of the study to examine the association between them.
The present study contributes to a growing literature showing that the consumption of ultra-processed foods is associated with an increased risk of diet-related non-communicable diseases. Its findings reinforce the need in Europe, and in other parts of the world, for public policies and actions designed to promote consumption of unprocessed or minimally processed foods and dishes and meals made with these foods, and to make ultra-processed foods less available and affordable.
Acknowledgements
Acknowledgements: The authors thank the UK Data Service and the DAFNE – Data Food Networking for making possible access to the data and the information used in this study. Financial support: This work was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq; grant number 443477/2014-0) and the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP; grant number 2015/14900-9). CNPq and FAPESP had no role in the design, analysis or writing of this article. Conflict of interest: The authors declare that there are no conflicts of interest. Authorship: C.A.M., J.-C.M. and R.B.L. designed the research. J.-C.M., R.B.L., D.S.C. and M.L.d.C.L. took care of data management. C.A.M., R.B.L., D.S.C. and M.L.d.C.L. analysed the data. C.A.M. and G.C. drafted the paper with contributions from the other authors. All the authors read and approved the final manuscript. Ethics of human subject participation: Not applicable.







