Introduction
Chronic rhinosinusitis is a common medical condition affecting up to 15 per cent of the Western population.Reference Fokkens, Lund, Mullol, Bachert, Alobid and Baroody1 Several therapeutic approaches are available for chronic rhinosinusitis treatment; however, in case of failure of medical treatment, endoscopic sinus surgery represents a valuable alternative.Reference Harvey, Goddard, Wise and Schlosser2 Endoscopic sinus surgery should not be considered as the only treatment, but rather as an adjuvant modality to remove the disease burden and increase the efficacy of post-operative medical therapy.Reference Mozzanica, Preti, Gera, Bulgheroni, Cardella and Albera3 Endoscopic sinus surgery improves the drainage of the nasal sinuses and the delivery of topical medication to the sino-nasal mucosa after surgery.Reference Harvey, Goddard, Wise and Schlosser2 For this reason, post-operative management represents a critical factor in treating chronic rhinosinusitis patients. Nasal irrigations are often prescribed (grade 1A recommendation) because it has been demonstrated that they promote cleansing of the nasal cavities, wound healing, and reduction of oedema and nasal discharge after surgery.Reference Low, Woods, Ullah and Carney4,Reference Tomooka, Murphy and Davidson5
Several factors may influence the efficacy of nasal irrigation in the post-surgical condition. Firstly, the extent of surgery has a major impact on the irrigant penetration into the sinuses. Previous studies suggest that sinus irrigation improves with the widening of the sinus ostia (as a result of endoscopic sinus surgery)Reference Harvey, Goddard, Wise and Schlosser2,Reference Singhal, Weitzel, Lin, Feldt, Kriete and McMains6 while unoperated patients have inconsistent and very limited sinus distribution.Reference Thomas, Harvey, Rudmik, Hwang and Schlosser7 Secondly, the device selected to irrigate the sinuses seems to significantly affect the efficacy of the nasal irrigation itself. High-volume devices have been demonstrated to be superior to low-volume devices in delivering solutions to the paranasal sinuses.Reference Harvey, Goddard, Wise and Schlosser2,Reference Valentine, Athanasiadis, Thwin, Singhal, Weitzel and Wormald8 No clear superiority among the different high-volume devices has been reported so far. Harvey et al.Reference Harvey, Goddard, Wise and Schlosser2 found that high-volume gravity-dependent devices offered the greatest distribution of irrigant after any surgery, whereas Brenner et al. Reference Brenner, Abadie, Weitzel, Thomas and McMains9 found that high-volume gravity-dependent devices were less effective than positive pressure devices in irrigating the maxillary sinus after balloon dilatation. Lastly, head position also seems to play a role in the distribution of irrigant into the sinuses. Many commercial products recommend the application with the head lowered in the ‘nose-to-sink’ position. Previous studies demonstrated that the efficacy of frontal distribution of the irrigant improves in a vertex down position, whereas the same position negatively affects the sphenoid irrigation.Reference Beule, Athanasiadis, Athanasiadis, Field and Wormald10,Reference de Paiva Leite and Douglas11
Even if the above-mentioned factors may influence the efficacy of nasal irrigation, the combined effect of these three factors was not studied at the same time in any of the previous studies. In the absence of this information, it appears difficult to correctly prescribe nasal irrigation in the post-treatment care of patients undergoing endoscopic sinus surgery. The aim of this study was to determine the effectiveness of topical delivery to the paranasal sinuses before and after endoscopic sinus surgery according to the extent of surgery, the irrigation device and the head position.
Materials and methods
The Department of Otorhinolaryngology, University of Insubria, Italy, provided institutional approval for the anatomical specimen use of human cadaver heads. All aspects of the study were performed within the sinus dissection laboratory of the Department of Otorhinolaryngology.
Specimen preparation
Cadaveric heads were initially evaluated by nasal endoscopy (0 and 30-degree 3 mm rigid endoscopes (Karl Storz, Tuttlingen, Germany) in order to rule out any anatomical anomalies that could interfere with the study.Reference Moffa, Costantino, Rinaldi, Sabatino, Trecca and Baptista12 Four adult cadaveric heads (two males and two females) without evidence of prior sinus surgery, nasal septum perforation, deviated nasal septum, aberrant nasal turbinates or sino-nasal disease were selected.
Visualisation ports were created in order to evaluate the lumen of frontal, maxillary and sphenoid sinuses using a 4 mm 30-degree endoscope. The anterior table of the frontal sinus was drilled at the level of the supraorbital rim, 1.5 cm from the midline, in order to visualise its lumen. For the maxillary sinus, a Caldwell–Luc approach was performed. Finally, the cranium and the brain were removed and the planum sphenoidale was drilled in order to visualise the interior of the sphenoid sinus (Figure 1). Each cadaver head underwent four stepwise endoscopic dissections performed by a single surgeon. The four levels of dissection ranged from ‘undissected’ to ‘maximal dissection’ (see Table 1).
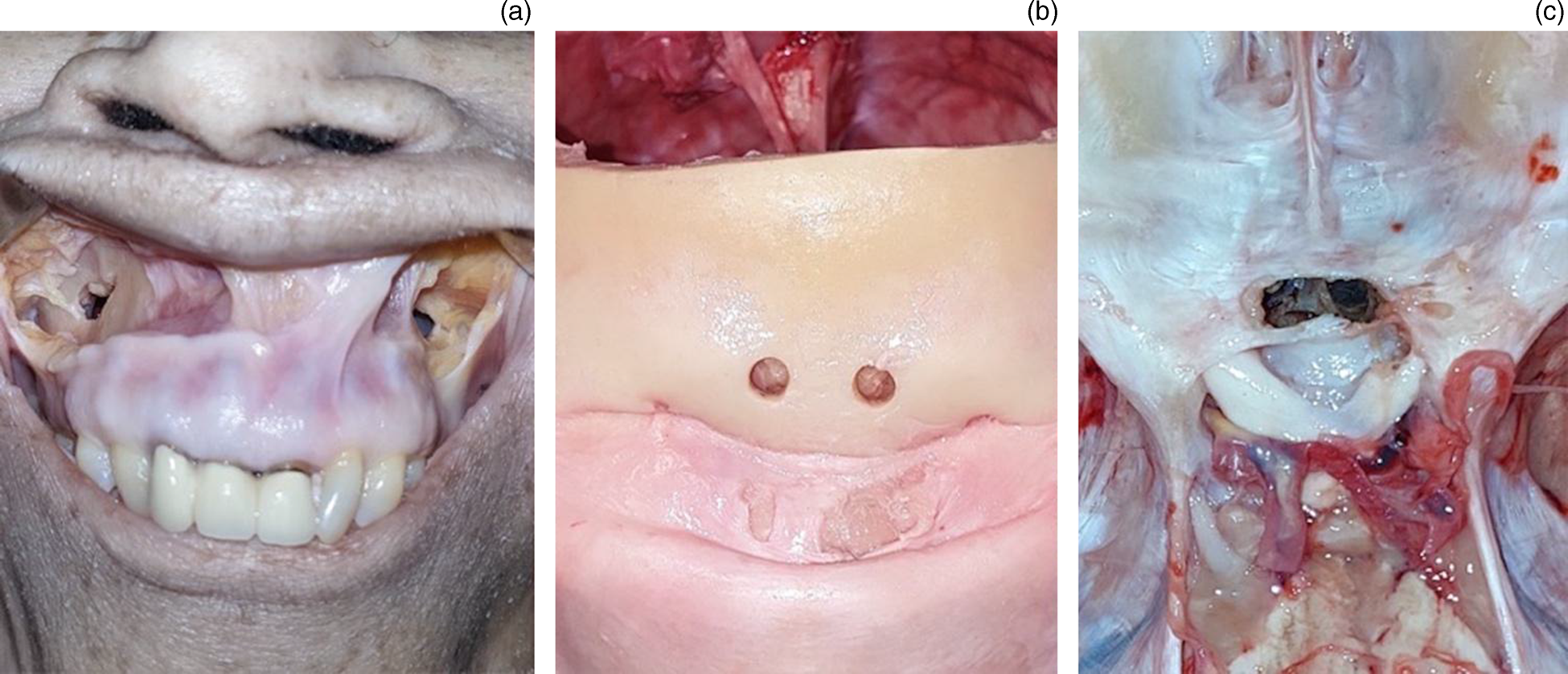
Fig. 1. Specimen preparation. (a) Visualisation port for the maxillary sinus was performed using a Caldwell–Luc approach. (b) For the frontal sinus, the anterior table of the frontal sinus was drilled at the level of supraorbital rim, 1.5 cm off the midline. (c) For the sphenoid sinus, the cranium and the brain were removed, and the planum sphenoidale was drilled.
Table 1. Dissection steps

Delivery devices
A total of three different delivery devices for nasal irrigation were used. The same solution was used for all the devices. Similar to the study of Moffa et al.,Reference Moffa, Costantino, Rinaldi, Sabatino, Trecca and Baptista12 the solution was prepared using methylene blue dye diluted in a balanced saline solution at a concentration of 12.5 per cent (1:8 dilution). This was done in order to tint the solution dark blue so that it could be visualised endoscopically but not so dark as to stain the sino-nasal mucosa. The tested delivery devices were: a 20 ml syringe without a needle; a 240 ml high-volume, high-pressure squeeze bottle; and a 250 ml high-volume, low-pressure gravity-dependent douching device.
Head position
The ‘nose-to-sink’ and the ‘vertex down’ positions were tested. In the ‘nose-to-sink’ position, the head was placed with the nose facing 45° downward. In the ‘vertex down’ position the head was put with the nose facing 90° downward.
Nasal irrigation and measurement of penetration
Irrigation was performed according to the following sequence: syringe, squeeze bottle and high-volume gravity-dependent device. To minimise bias, a single investigator performed all irrigations. The heads were irrigated with tap water between irrigations until previously administered dye was completely removed.
Measurement of the irrigant penetration into each sinus was video recorded using an endoscope which was inserted through the visualisation ports. Assessment of the irrigant penetration using digital videos, stored in an anonymous form and presented in a random fashion, was conducted by two investigators, blinded to the delivery device, extent of surgery and head position. None of the investigators were involved in specimen preparation or nasal irrigation. Similar to the study of Chen et al.,Reference Chen, Murphy, Alloju, Boase and Wormald13 an ordinal 4 point scale (0 = no irrigation; 1 = bubbling at the ostia; 3 = trickle through the ostia; 4 = free flow) was used to evaluate the amount of irrigant entering each sinus. In case a difference of more than one occurred between the two investigators, a third investigator assessed the videos and decided on the two ratings.
Statistical analysis
The inter-rater reliability was evaluated with two-way mixed-effects model (consistency definition) intraclass correlation coefficients. Intraclass correlation coefficient values were interpreted as follows: equal to or less than 0.20 = poor agreement; 0.21–0.40 = fair agreement; 0.41–0.60 = moderate agreement; 0.61–0.80 good agreement; and 0.81–1.00 very good agreement.Reference Altman14 The chi-square test was used to evaluate the effect of surgery, delivery device and head position on irrigant penetration within the sinuses. In order to control the increased risks of type 1 errors because of the large number of comparisons assessed with the chi-square test, Bonferroni corrections were performed when needed. Statistical analysis was performed using SPSS® (version 25) statistical software.
Results
Four cadaveric heads were used in this study. A total of 288 irrigations were performed and documented in digital videos. Twenty-one of the total number of irrigations were excluded because of incorrect camera positioning which resulted in difficulty rating these cases. The remaining 267 videos were evaluated. The overall concordance among investigators was very good (r = 0.88 at intraclass correlation coefficient).
Effect of surgery on sinus penetration
Distribution of the irrigant within the unoperated paranasal sinuses was limited, regardless of the head positioning and the delivery technique employed. The frontal sinus, in particular, was not penetrated at all by the irrigant in the unoperated state. However, a significant effect of surgery on irrigation was demonstrated with the chi-square test (p = 0.001, p = 0.001 and p = 0.001 for the sphenoid, maxillary and frontal sinus, respectively; Figure 2). As far as the maxillary and sphenoid sinuses are concerned, the chi-square test demonstrated a positive effect for each one of the surgical steps (Table 2). For the frontal sinus, the chi-square test demonstrated a positive effect of surgery, but no difference between step 2 and step 3 in the distribution of irrigant inside the sinus was demonstrated.
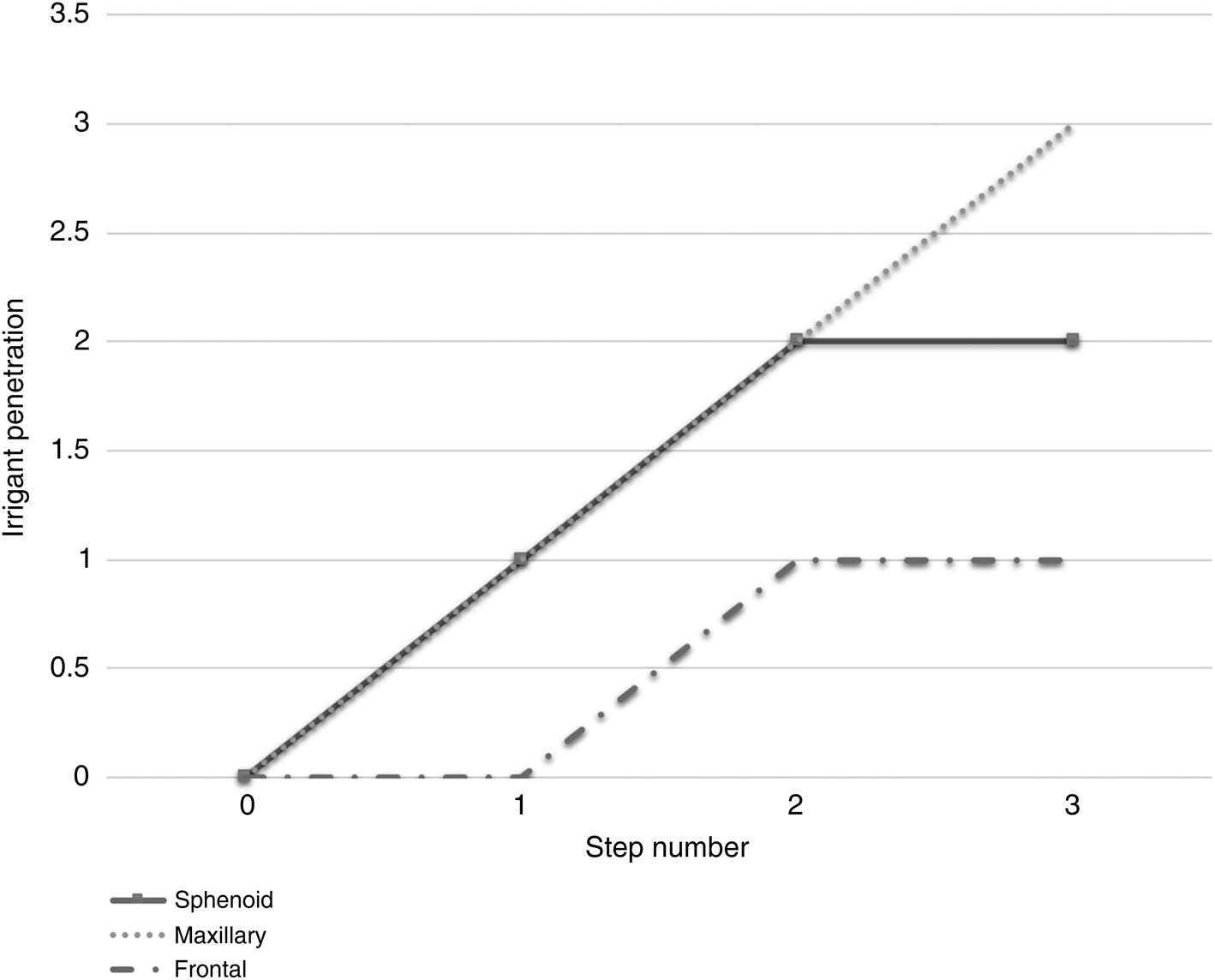
Fig. 2. Sinus irrigant delivery according to surgery. The results are reported as median value of irrigant penetration.
Table 2. Results of chi-square analysis on the sinus delivery score regardless of head position and delivery device

The statistically significant level for this comparison was set at 0.05
Effect of delivery device on sinus penetration
When considering the effect of delivery device alone, regardless of surgery and head position, the chi-square test demonstrated a significant effect of delivery device on the irrigant distribution inside the sinuses (p = 0.001, p = 0.001 and p = 0.001 for the sphenoid, maxillary and frontal sinus, respectively). In particular, the irrigant distribution score obtained using the syringe was significantly lower than those obtained using the squeeze bottle and the gravity-dependent device in all three sinuses. On the other hand, when considering the combined effect of delivery device and surgery, no differences in the irrigant distribution between the squeeze bottle and the gravity-dependent device were demonstrated at the chi-square test for the maxillary and frontal sinus in all the surgical steps, while the squeeze bottle assured a better irrigation of the sphenoid sinus at step 3 of surgery (Table 3 and Figure 3).

Fig. 3. Sinus delivery according to surgery and delivery device in each of the paranasal sinuses: (a) sphenoid, (b) maxillary and (c) frontal. The results are reported as median value of irrigant penetration.
Table 3. Results of chi-square analysis on the sinus delivery score according to device and surgery step

Table shows the results of chi-square analysis on the sinus delivery score according to the three different delivery devices (syringe, squeeze bottle and gravity dependent device) and the four steps of surgery. Due to the large number of comparisons assessed with the chi-square test, Bonferroni corrections were performed, and the p-value was set at 0.017.
Effect of head position on sinus penetration
When considering the effect of head position alone on irrigant distribution in the sinus, the chi-square test demonstrated a significant effect of the head position only for the frontal sinus (p = 0.239, p = 0.331 and p = 0.003 for the sphenoid, maxillary and frontal sinus, respectively). When evaluating the combined effect of head position, delivery device and extent of surgery on the distribution of irrigant in the sinus, the vertex down position significantly improved the frontal distribution of irrigant with both the squeeze bottle (p = 0.001 and p = 0.002 for step 2 and 3 of surgery, respectively) and the gravity dependent device (p = 0.003 and p = 0.003 for step 2 and 3 of surgery, respectively; Figure 4).

Fig. 4. Sinus delivery according to surgery, delivery device and head position. (a) sphenoid sinus NtS (nose-to-sink position), (b) sphenoid sinus vertex down position (VD), (c) maxillary sinus NtS, (d) maxillary sinus VD, (e) frontal sinus NtS and (f) frontal sinus VD. Step 0 was not reported because the irrigant penetration was 0 in each trial.
Discussion
In the present study, the combined effect of surgery, delivery device and head position on the irrigant penetration into the sinuses was studied using direct intra-sinus endoscopic visualisation. According to our results, a high level of concordance among the investigators was demonstrated suggesting high internal validity of the irrigation scoring system used. This data is in accordance with data reported by Roxbury et al.Reference Roxbury, Tang, Shah, McBride, Woodard and Sindwani15 who studied the irrigation distribution within the frontal sinus using a five-point scale and reported high inter-observer agreement.
The extent of surgery significantly affects distribution of the solution inside the paranasal sinuses. Similar to the study of Wormald et al.,Reference Wormald, Cain, Oates, Hawke and Wong16 a limited distribution of irrigant within the unoperated sinuses was demonstrated. Specifically, the frontal sinus was not irrigated at all in the unoperated stage. These findings are in agreement with those of Zhao et al.Reference Zhao, Craig, Cohen, Adappa, Khalili and Palmer17 who studied sinus irrigation before and after surgery using a computational fluid dynamics simulation, demonstrating that the frontal sinuses were not penetrated by any irrigation pre-operatively.
On the other hand, a significant improvement of sinus penetration was demonstrated as the sinus ostia became wider. Similar results were reported by several previous studies. Harvey et al.,Reference Harvey, Goddard, Wise and Schlosser2 who studied the effect of endoscopic sinus surgery on paranasal sinus distribution of topical solutions in 10 cadaver sinus systems, demonstrated that endoscopic sinus surgery greatly enhanced delivery of nasal solutions, regardless of delivery device type. Singhal et al.Reference Singhal, Weitzel, Lin, Feldt, Kriete and McMains6 studied the sinus penetration of irrigant according to 3 steps of surgical dissection in 10 cadaver heads and found that a wider sinus ostium resulted in better penetration of irrigant. In addition, in a recent review, de Paiva Leite and DouglasReference de Paiva Leite and Douglas11 concluded that functional endoscopic sinus surgery improves the reach and delivery of irrigation solutions to the paranasal sinuses.
Interestingly, in the present study, no difference was demonstrated between step 2 and 3 in the distribution of solution within the frontal sinus, thus suggesting that a Draf III procedure does not assure a better distribution of irrigant than a Draf IIa procedure. This finding is counterintuitive since, as opposed to the sphenoid and maxillary sinus, penetration of the irrigant into the frontal sinus is not proportional to the size of sinus ostium. It is possible that this phenomenon might be related to the removal of the upper portion of nasal septum which shunts the flow of solution before it reaches the frontal sinus. This hypothesis is in accordance with the findings of Zhao et al.,Reference Zhao, Craig, Cohen, Adappa, Khalili and Palmer17 who analysed the impact of removal of the superior nasal and interfrontal septum during the Draf III procedure through computational fluid dynamics and reported a premature spillage of the irrigant across the resected septum thus reducing its frontal penetration. Moreover, Roxbury et al.Reference Roxbury, Tang, Shah, McBride, Woodard and Sindwani15 did not find any significant improvement in distribution of irrigation when a larger septectomy was performed during Draf III.
Regarding the delivery device, a significant effect on sinus irrigation was demonstrated. In particular, the squeeze bottle and the gravity-dependent devices demonstrated a better sinus penetration than the syringe in each of the different surgical steps analysed. These findings are in agreement with previous reports. Harvey et al.Reference Harvey, Goddard, Wise and Schlosser2 found that high-volume devices greatly enhanced ability to deliver solutions to the paranasal sinuses. Valentine et al.Reference Valentine, Athanasiadis, Thwin, Singhal, Weitzel and Wormald8 studied the efficacy of nasal douching after endoscopic sinus surgery by means of a squeeze bottle and pulsed nebuliser. They reported that the squeeze bottle was more efficient in delivering saline to the nose and paranasal sinuses. Thomas et al.Reference Thomas, Harvey, Rudmik, Hwang and Schlosser7 concluded in their review of literature that a high-volume delivery device is the optimal technique of penetrating any particular sinus. Interestingly, in our sample, no differences were demonstrated in the irrigant distribution obtained by the gravity-dependent device and squeeze bottle for the frontal and maxillary sinuses. However, the squeeze bottle assured a better irrigation of the sphenoid sinus as opposed to the gravity-dependent device at step 3 of surgery. It is possible that these differences might be related to characteristics of the devices. The solution is delivered from the squeeze bottle by positive pressure. Hence, we can speculate that removal of the superior nasal and interfrontal septum during the Draf III procedure (with consequent flow of solution through the septal window and out the contralateral nostril) might be less relevant if the irrigant is delivered by positive pressure. This hypothesis is in accordance with the findings of de Paiva Leite and DouglasReference de Paiva Leite and Douglas11 who reported that Draf III procedures may reduce irrigation of the other sinuses.
It is important to note that head position significantly affects sinus irrigation. Distribution of the irrigant within the frontal sinus improved in the vertex down position. These data are in accordance with those of Beule et al.Reference Beule, Athanasiadis, Athanasiadis, Field and Wormald10 who found that the head down and forward position assured a clear superiority in distribution to the frontal sinus. Interestingly, there was no significant advantage of the head position for maxillary and sphenoid sinuses. Also, Singhal et al.Reference Singhal, Weitzel, Lin, Feldt, Kriete and McMains6 did not find any significant effect of head position on the irrigant distribution within the sphenoid and maxillary sinuses.
This study has several limitations. First of all, only four cadaveric heads were used because of limited availability and cost. Consequently, only limited information regarding inter-subject variability related to the nasal cavity anatomy (an important factor of medication distribution) could be inferred, thus limiting the generalisability of our results. In addition, use of the cadaveric specimens further limits the clinical generalisation since no information regarding the patient's comfort using the devices could be collected. Also, due to use of cadaveric specimens, we were unable to analyse the effect of breathing, mucosal inflammation and mucociliary clearance on the distribution of solution in the sinuses. The use of methylene blue may be considered an additional limitation of this study because residual staining following its administration could not be entirely removed from the specimens by rinsing with water and therefore the extent and intensity of sinus irrigation might be overestimated. In addition, the order of irrigation was always the same, and it is consequently possible that this could have affected the results (order effect). Moreover, the investigators were not fully blinded because the extent of surgery might be inferred through intra-sinus visualisation. Finally, the methodology chosen only permits the irrigant volume that reaches the sinuses to be assessed semi-quantitatively and does not permit evaluation of the real dynamics of the nasal irrigation flow.
• Nasal irrigation represents the key element in post-operative care after endoscopic sinus surgery
• Several factors may influence the efficacy of nasal irrigation including extent of surgery, head position and delivery device
• Nasal irrigation was more effective as the sinus ostia became wider through surgery
• The vertex down position facilitates the irrigation of the frontal sinus
• High-volume devices offer better irrigation than syringes
• The squeeze bottle offers a better irrigation of the sphenoid sinus than the gravity-dependent device after DRAF III
Conclusion
Nasal irrigation represents a mainstay of the post-operative treatment of chronic rhinosinusitis that provides cleansing of the nasal and paranasal cavities and delivery of topical drugs. The current study further confirms the efficacy of high-volume devices in irrigating the sinuses after surgery. A vertex down position during the irrigation could improve delivery to the frontal sinus. Furthermore, widening of the ostia by means of endoscopic sinus surgery improves irrigant access to the sinuses.
Acknowledgements
Andrea Preti is a PhD student of the ‘Sperimental and translational medicine’ course at Università degli studi dell’ Insubria, Italy.
Competing interests
None declared









