Crossref Citations
This article has been cited by the following publications. This list is generated based on data provided by
Crossref.
Sincomb, S.J.
Coenen, W.
Criado-Hidalgo, E.
Wei, K.
King, K.
Borzage, M.
Haughton, V.
Sánchez, A.L.
and
Lasheras, J.C.
2021.
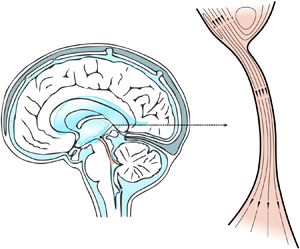
Transmantle Pressure Computed from MR Imaging Measurements of Aqueduct Flow and Dimensions.
American Journal of Neuroradiology,
Sincomb, S.
Coenen, W.
Gutiérrez-Montes, C.
Martínez Bazán, C.
Haughton, V.
and
Sánchez, A.L.
2022.
A one-dimensional model for the pulsating flow of cerebrospinal fluid in the spinal canal.
Journal of Fluid Mechanics,
Vol. 939,
Issue. ,
Wang, Danny JJ
Hua, Jun
Cao, Di
and
Ho, Mai-Lan
2023.
Neurofluids and the glymphatic system: anatomy, physiology, and imaging.
The British Journal of Radiology,
Vol. 96,
Issue. 1151,
Zhang, Daibo
and
Lindsey, Stephanie E.
2023.
Recasting Current Knowledge of Human Fetal Circulation: The Importance of Computational Models.
Journal of Cardiovascular Development and Disease,
Vol. 10,
Issue. 6,
p.
240.
Kelley, Douglas H.
and
Thomas, John H.
2023.
Cerebrospinal Fluid Flow.
Annual Review of Fluid Mechanics,
Vol. 55,
Issue. 1,
p.
237.
Peruzzo, Paolo
2023.
Theoretical and numerical analysis of the flow through a diffuser/nozzle element in pulsatile laminar conditions.
Physics of Fluids,
Vol. 35,
Issue. 10,
Maeda, Shusaku
Otani, Tomohiro
Yamada, Shigeki
Watanabe, Yoshiyuki
Ilik, Selin Yavuz
and
Wada, Shigeo
2023.
Biomechanical effects of hyper-dynamic cerebrospinal fluid flow through the cerebral aqueduct in idiopathic normal pressure hydrocephalus patients.
Journal of Biomechanics,
Vol. 156,
Issue. ,
p.
111671.
Balasundaram, Hemalatha
2023.
Impact of thermodynamical rotational flow of cerebrospinal fluid in the presence of elasticity.
BMC Research Notes,
Vol. 16,
Issue. 1,
Karki, Pragalv
Sincomb, Stephanie
Murphy, Matthew C.
Gunter, Jeffrey L.
Senjem, Matthew L.
Graff-Radford, Jonathan
Jones, David T.
Botha, Hugo
Cutsforth-Gregory, Jeremy K.
Elder, Benjamin D.
Huston, John
and
Cogswell, Petrice M.
2024.
Quantifying CSF Dynamics disruption in idiopathic normal pressure hydrocephalus using phase lag between transmantle pressure and volumetric flow rate.
Brain Multiphysics,
Vol. 7,
Issue. ,
p.
100101.
Báez-Amador, J.
Baños, R.
Arcos, J.
Méndez, F.
and
Bautista, O.
2024.
Flow enhancement produced by a pulsatile flow of shear-thinning fluids in circular and concentric annular tubes.
Journal of Non-Newtonian Fluid Mechanics,
Vol. 334,
Issue. ,
p.
105346.
Sincomb, S.
Moral-Pulido, F.
Campos, O.
Martínez-Bazán, C.
Haughton, V.
and
Sánchez, A.L.
2024.
An in vitro experimental investigation of oscillatory flow in the cerebral aqueduct.
European Journal of Mechanics - B/Fluids,
Vol. 105,
Issue. ,
p.
180.
Liu, Pan
Owashi, Kimi
Monnier, Heimiri
Metanbou, Serge
Capel, Cyrille
and
Balédent, Olivier
2025.
Transmantle pressure under the influence of free breathing: non-invasive quantification of the aqueduct pressure gradient in healthy adults.
Fluids and Barriers of the CNS,
Vol. 22,
Issue. 1,