Introduction
The well-documented lack of racial and ethnic diversity in studies across the research enterprise produces many and varied negative consequences for equity, ethics, and scientific rigor [Reference Knepper and McLeod1,Reference Oh, Galanter and Thakur2]. These consequences to scientific progress have been well understood for decades, propelling mandates for inclusion and reporting by major funders and the emergence of a sub-field of research recruitment and retention science [Reference George, Duran and Norris3,Reference Heller, Balls-Berry and Nery4]. Many barriers experienced by would-be participants have been reported including competing demands on time, financial constraints, lack of insurance, legal status, lack of transportation, and perhaps the most well-documented, distrust of researchers and health professionals [Reference George, Duran and Norris3–Reference Gilmore-Bykovskyi, Jin and Gleason6]. In response, strategies have been put forward to minimize barriers and increase inclusivity in research participation [Reference Gilmore-Bykovskyi, Jin and Gleason6–Reference Green-Harris, Koscik and Houston9]. Yet, meaningful improvements, and indeed even consistently measured progress toward that end, have not yet been realized [Reference Knepper and McLeod1,Reference George, Duran and Norris3,Reference Gilmore-Bykovskyi, Jin and Gleason6]. Such limited progress may be attributable in part to the predominance of focus on communities’ “willingness” or inability to participate and a relative paucity of focus on the roles that researchers and research staff play [Reference Corbie-Smith, Thomas and St George5,Reference Gleason, Dowling, Benton, Kaseroff, Gunn and Edwards10,Reference Passmore, Jamison and Hancock11].
While recognizing the importance of historical research abuse and current experiences of discrimination in healthcare settings in creating and reinforcing distrust, we argue that the framing of the problem as a “willingness” deficit of communities of color is troubling and, potentially, inaccurate. Initially, there is inconsistent evidence that historically excluded groups are indeed less willing to participate than others [Reference Corbie-Smith, Thomas and St George5,Reference Scharff, Mathews, Jackson, Hoffsuemmer, Martin and Edwards12]. Moreover, while there is a large body of literature on promising interventions to promote inclusive engagement [Reference Heller, Balls-Berry and Nery4,Reference Quinn, Butler and Fryer13], few focus on creating change in communities outside of academia. Rather, what has been shown to “work” to build inclusive research engagement has been the establishment of long-term, community-based relationships marked by overt efforts to “build trust” in underserved communities [Reference Quinn, Kass and Thomas14,Reference Kim, Cheney and Black15]. In such approaches, the change is not located in the community but in the researcher/team who transition away from traditional approaches towards a greater acceptance of community perspectives, work to build equitable relationships, and increased researcher trustworthiness.
To date, there is limited evidence of barriers to participation that exist on the researcher “side” of the relationship, such as bias and exclusionary recruitment practices [Reference Gilmore-Bykovskyi, Jackson and Wilkins16,Reference Niranjan, Martin and Fouad17]. However, such evidence is beginning to be collected [Reference Durant, Wenzel and Scarinci8,Reference Quinn, Butler and Fryer13,Reference Gilmore-Bykovskyi, Jackson and Wilkins16,Reference Niranjan, Durant and Wenzel18,Reference Bernadette, Heather and Southwick19]. Some of this recent research points to a lack of training in inclusive engagement strategies for researchers and research staff [Reference Durant, Wenzel and Scarinci8,Reference Niranjan, Durant and Wenzel18]. Others point to exclusionary practices such as requirements for English language proficiency, recruitment methods that prioritize convenience for researchers and similar approaches that exacerbate power imbalances [Reference Gilmore-Bykovskyi, Jackson and Wilkins16,Reference Damian and Gonzalez20]. Much of these recent contributions can be accurately viewed as situated within a wider exploration of the ways in which racism, discrimination, systems of oppression, and power within institutions shape the conduction of research and science [Reference Hardeman21,Reference Krieger22]. This manuscript fits within this discussion and presents a mixed-methods exploration of researcher and research team member attitudes, beliefs, and reported practices regarding the recruitment of underrepresented groups in research. Our purpose is to explore barriers within the experience of researchers to complement what we already know about barriers in the community. We present findings of a web-based survey and semi-structured, key informant interviews conducted with researchers and staff affiliated with our Clinical and Translational Science Award (CTSA) program hub.
Materials and Methods
This study adopted a sequential exploratory mixed-methods design to allow for a focused examination of salient factors first identified from an initial quantitative investigation (survey) with qualitative methods (key informant interviews) [Reference Creswell and Clark23]. Preliminary findings of the survey have been reported recently in the Journal for Clinical and Translational Science where readers can find additional details on the delivery of the survey, item construction, and a copy of the survey instrument [Reference Passmore, Edwards, Sorkness, Esmond and Brasier24]. All materials and procedures were approved by the UW Madison Institutional Review Board (#2019-1211).
Survey Methods
Participants/sampling
Study participants were health researchers and research team members identified as users of the CTSA’s research support infrastructure between 2017 and 2019. Initial emails (1456) and subsequent reminders produced 279 participants who finished at least 90% of the survey (response rate of 21.5%).
Item development
The survey consisted of items designed to (1) identify “types” of participants based on role in research, type of research funding, years of experience in research, etc., and (2) determine knowledge, attitudes, and practices regarding participant recruitment with a specific focus on members of underrepresented groups. The survey instrument consisted of 23 items (some including subitems). Of these, Likert-type items were used to assess attitudes and knowledge regarding research inclusion “theoretically” without reference to their own work (i.e. “how important is it that people of diverse racial and ethnic backgrounds participate in research?") as well as these same attitudes and knowledge items with reference to participants’ specific research activities (i.e. “how much is recruiting racial and ethnic minority participants a priority in your research?”).
Survey analysis
Analyses consisted of the exploration of patterns relative to inclusive recruitment attitudes, knowledge, and practices. To further these analyses, we constructed two composite scales regarding inclusive best practices derived from the literature (use of a community advisory boards, partnership with community-based organizations, racial/ethnic concordance of research staff and participants, and devoting extra time to recruit typically underrepresented participants) [Reference Heller, Balls-Berry and Nery4]. The developed scales were as follows: (1) Best Practices – knowledge (7 items; α 0.907) and (2) Best Practices – implementation (5 items; α 0.825). Basic descriptive statistics were computed for the demographic variables, individual survey items, and the two composite scales. Mann-Whitney U tests [Reference Sullivan and Artino25] were computed to determine whether there were differences between two groups on our ordinal (Likert type) dependent variables and t-tests for continuous variables.
Key Informant Interview Methods
Participants/sample
Our intent was to recruit participants to contribute to our understanding and interpretation of survey findings through key informant interviews. Potential participants were contacted through a recruitment email sent to CTSA affiliated researchers and staff (similar to survey recruitment). This process produced a few initial participants, and from that base, we used a snowball sampling approach to garner a larger sample [Reference Valerio, Rodriguez and Winkler26]. We sought to “oversample” experienced clinical research coordinators to dig more deeply into on the ground barriers to the implementation of specific strategies to promote inclusive recruitment. Some initial interviews were conducted face-to-face in February 2020. However, the majority were conducted by telephone to comply with public health restrictions imposed by the COVID-19 pandemic. At 26 interviews, the team increasingly observed a level of saturation in the data.
Interview guide
Consistent with the exploratory sequential approach, interviews were designed to provide a deeper understanding and clarify survey findings. A key domain of inquiry was “on the ground” barriers to inclusive recruitment as well as best practices/solutions. (See Fig. 1: Interview Protocol.)

Fig. 1. Interview protocol.
Interviews lasted between 30–45 minutes. All interviews were audio-recorded and transcribed verbatim for analysis.
Analysis
Analysis was team-based and included two independent coders using NVivo 12 software to facilitate qualitative data management and analysis. The initial stage of analysis consisted of immersion in the data set. At this point, an initial coding frame was established. However, we also were open to emergent themes and concepts. In order to ensure intercoder reliability, portions of the transcripts were double-coded and compared [Reference O’Connor and Joffe27]. Coders met frequently to develop new codes, clarify concepts, and resolve discrepancies in coding. The work took place in two phases: first beginning with open coding to label and identify categories, followed by axial coding which aimed to identify connections across and between categories [Reference Strauss and Corbin28,Reference Sbaraini, Carter, Evans and Blinkhorn29]. In this later phase, codes were sorted, clustered, and compared frequently with the use of mapping to explore relationships and identify themes. Interpretation of qualitative findings and connections between codes was also team-based.
Results
Survey
The majority of our survey respondents were engaged in clinical research (72.4%) and reported that they received some to all of their research funding from federal sources (75.6%). Reflective of the demographics of faculty and staff at the institution where the research took place, respondents overwhelmingly self-identified as White (81.4%) [30] (See Table 1).
Table 1. Survey participant characteristics
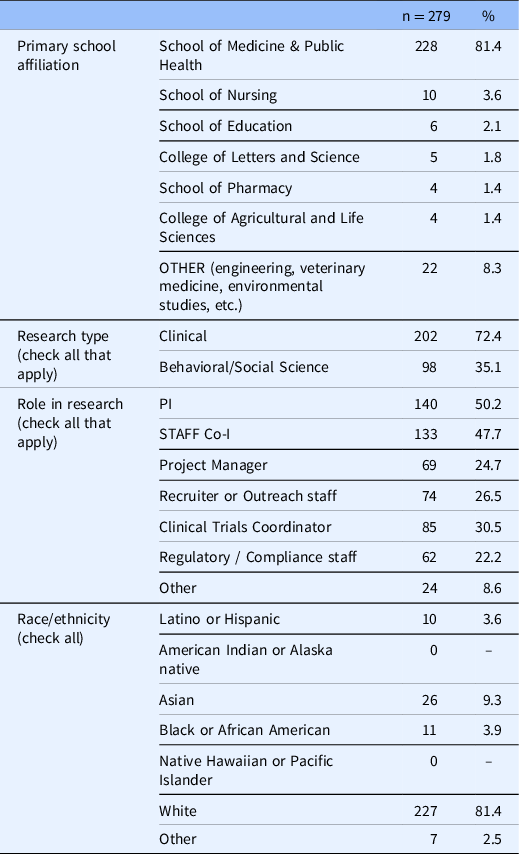
Co-I, co-investigator; PI, principal investigator.
As preliminary findings are available in an earlier publication [Reference Passmore, Edwards, Sorkness, Esmond and Brasier24], we will not repeat full results here but will focus on the aspects of the survey findings that have implications for the mixed-methods analysis and interpretation. This is that there exists for a majority of respondents a gap between knowledge of the importance of diversity in research and the implementation of strategies to address that gap. 87.1% of respondents reported that they saw diversity in research samples to be very important/extremely important in the abstract. However, when asked how much diversity was a priority in their specific research program, only 38.3% responded with “a lot” or “a great deal.” The general difference between ideals and practices was also revealed in the averages of Best Practices – knowledge (BP knowledge) and Best Practice – implementation (BP implementation) scales which were measured on a 1–5 scale with 5 as the highest. Average scores for these scales were 4.0, 2.9, respectively. While overall, investigators and research staff agreed on many items, staff expressed somewhat weaker feelings about diversity as a priority in their work, 36% vs. 40% (investigators) (p = 0.02) (See Fig. 2).

Fig. 2. Comparison of belief in value of inclusivity and practice.
Key Informant interviews
As noted, interviews were intended to provide additional insight into unresolved or partially resolved questions from the initial phase of the survey. Of these, most important was the finding that while respondents recognize the importance of diversity in research, this knowledge did not translate into the implementation of strategies to increase diversity for the majority of participants.
Our interview sample (n = 26) included investigators and staff from same population as survey respondents. As noted, we sought out a larger proportion of clinical research coordinators which resulted in greater engagement of clinical researchers (92%) and research staff (77%) than the sample that participated in the survey. Like our survey and the population of researchers and staff at our institution, our interview sample was predominantly White (73%) (See Table 2).
Table 2. Interview participant characteristics

Co-I, co-investigator; PI, principal investigator.
Participants had much in common but differed in terms of the effort they put into strategies to increase inclusivity in research. On this point, participants formed two groups: those who reported currently implementing inclusive recruitment strategies (8) and those reporting no such efforts (18). All interview participants recognized the lack of diversity in research samples across the research enterprise, and all recognized the problem that this situation poses for scientific and ethical reasons. The following quotes are illustrative of the sentiment expressed in many interviews.
It’s definitely something that Iʼve observed…In my 11 years, I can count in my head, the fact that I can do this, I can count the number of African-American participants who have participated on trials, honestly … the number of African-American participants that Iʼve even spoken with, whether they participate or not, and also same for Latino. (Research staff, clinical)
And,
It’s just that, unfortunately, it is the fact of it when it comes to research which is unfortunate, really unfortunate, actually. (Research staff, clinical)
Across the two groups, participants perceived barriers to recruitment of underrepresented groups including transportation, multiple family/work responsibilities, language, and cultural barriers. Most frequently noted was a perception that there is too small of a population of underrepresented groups in the region of our center. Another theme across the interviews was a reported lack of skills and training around inclusive research recruitment strategies. For example, one investigator noted,
I donʼt think we have good ways of explaining kind of what research is in communities of color and Native American communities. (Investigator, clinical research)
Similarly, a staff member working in research for over 10 years observed that,
…it’s harder (inclusive recruitment strategies) …and it’s also not something we train people to do at all. (Research staff, clinical research)
Finally, all participants recognized barriers caused by a lack of trust of science and health professionals in underrepresented communities. For example,
They’re more hesitant to participate in research. And I totally understand why, just given the history… (Investigator, clinical)
Lastly, all participants recognized that inclusive research strategies took more time, effort, and involved more costs. For example, several participants, including the one quoted below, noted the cost and time involved in the translation of study materials or consent forms.
So because of the cost, it makes it a little bit harder to enroll certain populations who are English language learners. (Research staff, clinical research)
Participants implementing inclusive strategies
While all participants saw barriers to recruitment, the eight who reported having moved past barriers to implement strategies were unique in other ways as well. All participants who identified as Latino or Black were in this group, and each was specifically hired to do outreach among underrepresented communities. An additional two, White participants, were the only two participants who reported working within NIH-supported research centers. Such centers, they noted, afford specific resources for community engagement. For example,
So here at the [CENTER], weʼre spending a lot more time planning events in the community, and that has been a tremendous, successful effort, and it’s a way of giving back and building rapport and good will. And it’s, again, it’s very resource-intensive, and, but it’s been very successful. (Research staff, clinical research)
Of the remaining three participants engaged in specific strategies to reach diverse groups, two identified themselves as health disparity investigators engaged in community-based research. The final participant reported the use of community-based recruitment strategies despite a lack of training in response to a desire of the team and, specifically, the principal investigator (PI) to increase diversity in response to NIH guidelines.
Participants not implementing inclusive strategies
The remaining and larger portion of interview participants (18) reported no current specific effort to increase diversity in participation despite expressed beliefs in the principle of inclusion and scanty success in the recruitment of members of underrepresented groups. These participants saw barriers to inclusive engagement as inherently “insurmountable.” As one participant noted,
I think there are…, I truly believe in research [that] there are some barriers that are insurmountable. (Research staff, clinical)
Moreover, several noted that this belief was shared by others. For example,
I think everybody is in it for the good, for good reasons, you know. Everybody Iʼve talked to really cares about and believes, that research can make a difference, you know. So there’s definitely that. And, but I think that people feel like there’s a lot of barriers, and I think they feel like theyʼre insurmountable a lot of times. I donʼt know. Maybe that’s a little too strong, but… (Research staff, clinical)
Some also presented this perception as expressed by principal investigators. For example,
I would say PIs donʼt generally bring it up just because… the perception is there’s not much we can do about it. Like, the population we get is the population we get. (Research staff, clinical)
This conceptualization of the lack of diversity in research as an “insurmountable” problem was frequently accompanied by a perception that there are no patients or not enough patients of underrepresented communities to recruit. For example,
… our patient [participant] population is pretty representative of who’s coming into clinic. And unfortunately, it’s, like, pretty white and old. (Research staff, clinical)
Other participants noted that because non-English speakers make up only a small portion of the patient population, the work and cost of translation are not “worth it.”
We donʼt routinely translate our consents into any other language, just because we donʼt have like a broad, like it’s not consistently like, oh, like 50% of our patients that are referred speak Spanish as their primary language. You know, then we would probably translate them into Spanish up front, but we donʼt. (Research staff, clinical)
A research staff member with more than 10 years of experience recounted an experience with a previous effort for inclusivity that, while successful, was eventually abandoned. In this example, as well, the PI played a key role.
Weʼve tried, weʼve made efforts. In one past [project], we really wanted, and I give my PI kudos, she really wanted to have Spanish speakers also enrolled, and we did…It ended up being 20-something out of a 450 sample, you know, so it’s small…and it was just two sites that did it, because, again, the logistics, the expense of getting all the materials translated, you know, professionally translated, printing multiple sets of materials, how do you know who to mail which materials to?… So it’s just like the logistics kind of did us in on that one. But then it ended up being such a meaningful subsample that pool of data was really, really fascinating and will be a separate paper and really identified a shocking need and disservice occurring within that group. So it was really fascinating, and I wish we had had more, but, I mean, it was just a ton of work…(Research staff, clinical)
Researchers and team members also expressed hesitancy in inviting participants of underrepresented groups to join studies as they assumed a lack of willingness to participate, ineligibility, or an inability to compete study requirements. This also played into the idea that inclusive research engagement is an unattainable goal.
[African Americans have] jobs that wonʼt let them take off work for, you know, follow-up visits, not having the capability, you know, to maybe use a private car, having to take a bus… (Research staff, clinical)
And,
Or they bring their, you know, five grandchildren… I mean, just the dynamics that go on in the underrepresented families is different than the Caucasian-based sample. (Research staff, clinical)
Some participants were candid about feelings of discomfort or anxiety about recruiting members of underrepresented groups. For example,
I guess too it’s like a comfort…a comfort thing too. I am always amazed at the fear people have of the unknown. There’s just a discomfort associated with working with people that arenʼt like themselves. I mean, it’s still, I mean, I know I have it. (Research staff, clinical)
And,
I still mostly feel like I donʼt know the right way to do this. Like that’s the overwhelming feeling that I have about thinking about recruiting participants from populations that have those kinds of histories and experiences in healthcare. So, yeah, I think there’s just like a lot of, I donʼt know if it’s, I donʼt know what the right word is, if it’s anxiety or doubt or like being unsure about the right kinds of approaches or ways to manage all that… there’s just a lot more apprehension before you walk into the room to recruit the patient. (Investigator, clinical)
Other participants expressed anxiety about discussing the topic of diversity and inclusion even when they did not directly tie their anxiety to a hesitancy to approach participants. Often, this was expressed in struggling with language and apprehension around saying the “right” thing in interviews. For example,
….and I kind of, I want to circle back to your question about minorities and research. I feel like sometimes I get really caught up in what specific words that I use, and what is, you know, socially acceptable in using certain terms… I donʼt want those to come off as if Iʼm stereotyping certain populations… (Research staff, clinical)
Similarly, in the following quote, a research team member repeatedly “checked in” with the interviewer to get their approval about their use of language regarding the recruitment of participants from underrepresented communities.
RESPONDENT: Yeah. How am I doing so far?
INTERVIEWER: It’s not a test. Good. Yeah, good. (Research staff, clinical)
This difficulty with language, anxiety, and making assumptions about willingness or ability to participate suggests that issues of race and bias influence recruitment activities. Indeed, a few researchers directly recognized the role of implicit bias as a problem. For example,
Whether it’s gender, socioeconomic status, race and ethnicity, cultural differences, all of those things bias how we, you know, understand the world. And so we really got to get out of that space and have other people help us understand how to do our work better and in a meaningful way…(Investigator, Behavioral)
This too was seen as “insurmountable.” As one, White identified outreach staff member noted, “how do you call that out and, like, actively fight it? Because the problem with unconscious bias is you donʼt know youʼre doing it.” (Research staff, clinical)
Discussion
Our findings point to the existence of a disconnect between awareness of the importance of diversity in research and the actual implementation of strategies to promote the inclusion of participants from underrepresented groups. We have also been able to reveal some factors that play into this observed disconnect. While all the researchers and researcher staff we interviewed saw barriers to inclusive engagement, as indeed have many other researchers [Reference Durant, Wenzel and Scarinci8,Reference Niranjan, Martin and Fouad17–Reference Bernadette, Heather and Southwick19], only some reacted by implementing specific strategies to promote diversity in their work. These researchers were motivated by goals of social or health equity, used community-based methodologies, and/or benefitted from the infrastructure of NIH-funded research center. It is important to note that we are not the first to suggest that health researchers may fall into one of two “camps” regarding inclusive engagement. Quinn et al similarly describe “comprehensive” (using community-based and multiple strategies for recruitment) and “traditional” researchers in a much larger and national survey [Reference Quinn, Butler and Fryer13]. A key factor inhibiting efforts for inclusivity for a majority of researchers is the widely held belief that increasing diversity in research is near impossible, a problem that is “insurmountable.” This belief, among others, feeds into a “cost/benefit” analysis which results in the decision not to pursue recruitment of underrepresented population even when strategies are known and possible.
On the “cost” side of inclusive research engagement, we find money and time as well as the anxiety or discomfort White researchers and staff may experience approaching members of underrepresented groups. Possible benefits are viewed as extremely limited given the belief in a paucity of diversity in the patient population. Further, assumptions about patients’ unwillingness or inability to participate in research make success seem undoubtful even if one could find members of underrepresented groups. Such factors have been partially described by others working in academic health centers [Reference Niranjan, Martin and Fouad17,Reference Bernadette, Heather and Southwick19] and may lead to researchers withholding the opportunity to participate from patients from underrepresented groups.
For those working in contexts of limited diversity, the perception that inclusion is “not worth the effort” is itself paradoxical [Reference Durant, Wenzel and Scarinci8]. We would argue that the demographics are not at the basis of the problem. Certainly, there is substantial evidence that globally, participation rates do not reflect either proportionality in the population or prevalence of rates of disease [Reference Knepper and McLeod1,Reference Gilmore-Bykovskyi, Jackson and Wilkins16,Reference Duma, Vera Aguilera and Paludo31,Reference Weigmann32]. We would argue that the barrier is not the lower proportionality but rather the tendency to see low proportionality as a reason that inclusive research practices are “not worth the effort.” Even if we accept a low level of diversity in the patient population, it is not logical to forgo outreach to underrepresented groups. Rather, it could be seen as a reason to redouble and intensify efforts to meaningfully connect with local communities. These are solutions that have been demonstrated to work [Reference Heller, Balls-Berry and Nery4,Reference Green-Harris, Coley and Koscik33]. We would argue that the work our participant reported doing to include “20-something [Spanish speakers] out of a 450 sample” (4%) was not only worth the effort but a central part of the work of research recruitment.
The underlying perception of inclusive research strategies as ancillary, optional, or at least “not central” to the work of recruitment ties to the wider socio-cultural context of the research teams, the direction provided by the investigators that lead them, the institution, and the society to which they all belong. Indeed, similar conceptualizations have been described with relevance to other fields. In education, for example, the view of Black children as “other” has been shown to pose barriers to equity in educational attainment [Reference Delpit34]. In healthcare settings, similar outcomes are found related to systems designed around “regular” patients [Reference Maina, Belton, Ginzberg, Singh and Johnson35–Reference FitzGerald and Hurst38]. Such “othering” of communities is a component of systemic racism [Reference Bonilla-Silva39–Reference Tarman and Sears41]. Indeed, we can describe much of our findings through Bonilla-Silva’s basic components of a “color-blind” ideology underlying race-based hierarchy in American society – abstract liberalism, naturalization, and cultural racism[Reference Bonilla-Silva39]. Initially, researchers and research staff in both the web-based survey and interviews accept the problem of a lack of diversity in research in abstract terms even while not connecting it directly to their own work (abstract liberalism). The conceptualization of the lack of diversity in research as unsolvable (“there’s not much we can do” or “the population you get is the population you get”) parallels Bonilla-Silva’s concept of “naturalization” in which the problem is inherently unsolvable. Cultural racism may also be found in a priori assumptions about the willingness or ability of patients from underrepresented groups to participate in research [Reference Durant, Wenzel and Scarinci8,Reference Niranjan, Martin and Fouad17,Reference Taft, Weir, Kramer and Facelli42–Reference Howerton, Gibbons and Baffi44]. Further, evidence of the role of race in research recruitment practices can be found in the apprehension, hesitancy, and anxiety researchers expressed on the topic of inclusion.
Conclusion
Ultimately, institutions, funders, and PIs are responsible for setting in motion a shift to place inclusivity as central in the work of research engagement. Our findings indicate that teams may need support for community engagement activities from funders and through specific opportunities for training. However, we must work to counter tendencies to present such trainings as “add-ons” or specializations. The goal of inclusivity must be integrated into all research-related trainings and, thereby, presented as an essential skill set of researchers and research staff [Reference Niranjan, Durant and Wenzel18,Reference Passmore, Edwards, Sorkness, Esmond and Brasier24]. The solution lies in consciously and systematically positioning strategies to make research rewarding, safe, and accessible to members of underrepresented groups, who are disproportionately burdened by participation barriers (i.e. lack of time, limited transportation, language-related barriers). Relatedly, we must move away from framing the issue as a lack of community “willingness” towards one of researcher “trustworthiness” as the former obfuscates the features of the researcher, team, institution, and research design contributing to the ongoing lack of diversity in research.
It is imperative not to interpret our findings or those of others [Reference Niranjan, Martin and Fouad17,Reference Niranjan, Durant and Wenzel18] as evidence of a solely individual-level problem of interpersonal racism. The issue exists in systems and that is where the solution will ultimately lie. This is not new. The impact of systemic racism in science has been demonstrated with many examples through our history [Reference Nelson45,Reference Gould46]. Indeed, the dynamics of race underly the very research abuses, such as the Tuskegee Syphilis Study, that are accepted as the basis of mistrust in underrepresented communities [Reference Scharff, Mathews, Jackson, Hoffsuemmer, Martin and Edwards12,Reference Freimuth, Quinn, Thomas, Cole, Zook and Duncan47,Reference Garrison48]. The recognition of bias as a factor in research engagement is a step forward in our pursuit to strengthen the ethical and scientific basis of health research. It also does much to explain why the overrepresentation of White participants exists across the research enterprise. With the acceptance of bias as a factor in research engagement, as it is found in so many other contexts, comes the ability to address it through education, resource allocation, and the diversification of the scientific workforce itself [Reference Bennett, Salinas, Locascio and Boyer49]. Certainly, we cannot conclude that there is “nothing we can do” nor can we exclude researchers working in predominantly White communities from obligations to collect data and conduct analysis on diverse samples. Our path forward is in facing barriers on both the researcher and community sides of the problem and developing new solutions and innovative approaches. The alternative is not viable. As Gilmore-Bykovskyi et al suggest,
Unaddressed, research injustices will continue to translate into downstream disparities in the efficacy, safety, and accessibility of treatments and interventions developed with, and, thus, for, predominantly white, privileged populations for conditions that disproportionately impact minorities, as observed across many health conditions [Reference Gilmore-Bykovskyi, Jackson and Wilkins16].
If the problem, as so much research has indicated, is a lack of trust, addressing bias in the research enterprise is a good first step toward building our trustworthiness [Reference Gilmore-Bykovskyi, Jackson and Wilkins16].
Limitations
Our focus in this study was researcher and staff perceptions. Thus, we cannot say what ultimately is the most powerful cause of the lack of diversity in research. Indeed, it is likely to be multicausal involving all the barriers indicated above as well as a well-documented hesitancy to participate among patients of underrepresented groups. It should also be noted that this discussion is overly simplistic as it focuses on a singular dimension of inclusion and does not incorporate issues of intersectionality. Finally, this study and our related findings are affected by limitations in sample size, response rate, and the representativeness of our sample. Our sample was over overwhelmingly White. While this adequately represents the research community at our institution, these findings are not generalizable to more diverse research communities. Indeed, a possible direction for future studies might be a comparison with a more diverse sample. We believe, however limited our findings, they are indicative of general barriers to inclusivity on the “researcher side of the equation” which has been understudied to date. We hope that this work will inspire further exploration and solutions.
Acknowledgements
We would like to thank our participants who offered their experience honestly and candidly. We also acknowledge the University of Wisconsin Survey Center who assisted in item development and administration of the web-based survey. The overall study was financially supported by the Collaborative Center for Health Equity as well as the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR002373, at the University of Wisconsin-Madison. Additional support was received by the National Institute on Aging of the National Institutes of Health under Award Number K76AG060005 (Gilmore-Bykovskyi).
Disclosures
The authors have no conflicts of interest to declare.






