Introduction
Crisis and emergency risk communication frameworks are currently being applied in the public health response to the coronavirus disease 2019 (COVID-19) pandemic to encourage public participation in disease prevention and containment. Common principles of these frameworks are to be correct, credible, and respectful, to promote action and to engage with communities in order to empower decision-making [Reference Reynolds and Lutfy1,2].
Effective application of risk communication frameworks depends, in part, on reaching vulnerable populations with a history of social injustice, health disparities, and limited access to health information. Racial minorities have been disproportionately impacted by COVID-19. For example, the age-adjusted death rate in New York City for blacks and Hispanics as of April 6, 2020, was approximately double the rate among whites [3]. Thus, there is an urgent need for effective channels of risk communication with vulnerable populations [Reference Berger, Evans, Phelan and Silverman4].
Vulnerable populations and minorities are more likely to have communication gaps due to socioeconomic disadvantage, low health literacy, immigration status, and limited English proficiency [Reference Blumenshine, Reingold, Egerter, Mockenhaupt, Braveman and Marks5], compounded by language and cultural discordance and mistrust of health institutions [Reference Bergstresser6]. The Centers for Disease Control and Prevention (CDC) Crisis and Emergency Risk Communication Manual describes three levels of community engagement (low, medium, high) and acknowledges that a high level of engagement that starts prior to any emergency is needed to reach vulnerable populations in times of crisis [Reference Reynolds and Lutfy1].
Community-engaged research (CEnR) partnerships are uniquely positioned to operationalize pandemic risk communication frameworks among vulnerable populations. CEnR partnerships, characterized by collaboration between community members and researchers through all phases of research, are increasingly ubiquitous in the United States across disciplines, population groups, and geography [Reference Ortiz, Nash and Shea7]. These partnerships have access to large networks of vulnerable groups through their focus on health equity, and community partners have organizational and technical capacity for interfacing with these populations in a research and evaluation context [Reference Wallerstein and Duran8]. CEnR partnerships have already laid the foundation for engagement through prior work, thereby addressing the risk communication principles of credibility, respect, and relationships that pre-date a crisis while empowering community decision-making. Likewise, CEnR partnerships empower community decision-making, which is a critical risk communication process [Reference Reynolds and Lutfy1].
This study aims to demonstrate the use of a CEnR health partnership with vulnerable populations leveraging its social networks, credibility, and technical expertise to promote bidirectional crisis and emergency risk communication for the COVID-19 pandemic.
Methods
Community and academic partners from Rochester Healthy Community Partnership (RHCP), a CEnR partnership with a 15-year history of participatory research with immigrant populations in Southeast Minnesota [9], adopted the CDC Crisis and Emergency Risk Communication framework for co-creation of an intervention framework aimed at populations with limited English proficiency. RHCP community partners observed that credible COVID-19 information was being produced, but it was not reaching immigrant communities.
Intervention Development
COVID-19 message maps were developed by RHCP community and academic partners. Message maps are a framework used to create compelling messages for specific audiences; each concise message is supported by 2–3 facts [Reference Covello10]. Message content was consistent with communication from regional and national public health officials and Mayo Clinic and focused on three constructs: COVID-19 prevention and containment; SARS Coronavirus-2 testing; and social and economic impacts of COVID-19 [11]. As COVID-19 facts changed, the same process was used to generate biweekly “reports” throughout the intervention that included new messages or refinements of previous messages. Materials were professionally translated into six languages by an institutional community partner.
Recruitment and Training of Communication Leaders
Communication Leaders were recruited by RHCP community partners to deliver messages based on their credibility and trustworthiness within subset communities. The majority of Leaders (22/24) had worked with RHCP in previous projects. A single virtual meeting was held with Communication Leaders and RHCP partners to review the intervention framework and messages.
Intervention
COVID-19 messages were delivered by 24 bilingual Communication Leaders within their social networks. Because of physical distancing, messages were mostly delivered electronically. There were no guidelines around communication mediums (e.g., voice calls, text messaging, social media) or mechanisms (e.g., video, text, audio). For example, some Communication Leaders sent the messages in full, others broke them up into smaller message components, and others used a device to record a video of themselves communicating the key components of each message. Recipients were encouraged to amplify the messages to their social networks. Additionally, Communication Leaders solicited community health and socioeconomic concerns through the same platforms. This bidirectional communication with vulnerable community members was used by RHCP to enhance subsequent messaging, leverage resources to meet community needs, and advise regional decision makers (Fig. 1).
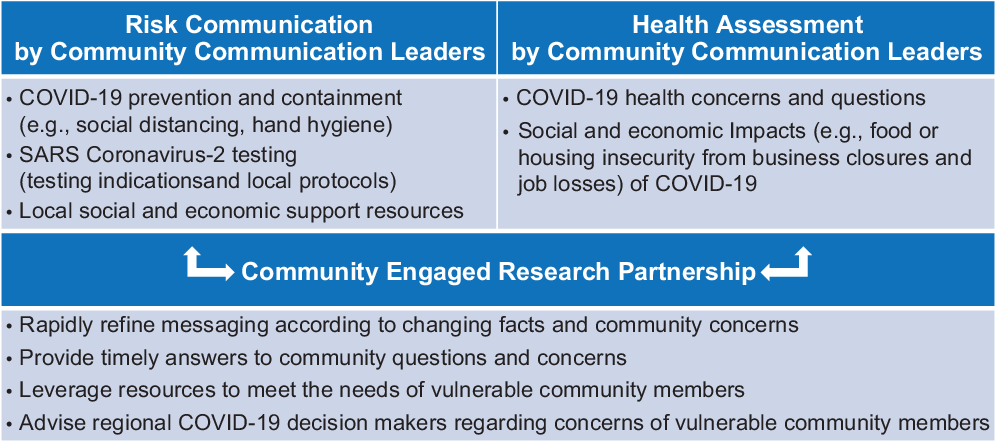
Fig. 1. Intervention framework.
Communication Leaders and RHCP partners met daily via an hour-long teleconference for three purposes. First, Communication Leaders shared their progress for all to learn emerging best practices from others. Second, message refinement and generation of new messages were achieved in real time in response to community feedback as well as rapidly changing COVID-19 facts and resources. Third, questions were answered in real time by infectious disease experts (academic partners) or community resource experts (community partners). In-between phone calls, Communication Leaders and RHCP partners communicated by text messages and email.
Examples of new messages or message modifications based on community feedback included specific COVID-19 “myth-busters,” advice for funeral practices, and advice for physical distancing while outdoors. Examples of bidirectional communication that informed community resource allocation included targeted distribution of food and face coverings to vulnerable community members identified by Communication Leaders. Finally, feedback from community members was used to inform regional decision makers regarding COVID-19 testing procedures so that messaging was consistent regardless of where the individual received their usual healthcare.
Evaluation
Rapid evaluation and assessment methods [Reference McNall and Foster-Fishman12] were used for participatory evaluation of the intervention, which informed continuous intervention refinement. The evaluation interval was the first 14 days of intervention implementation: March 27 to April 10, 2020. We assessed intervention reach, acceptability, and feasibility. We also used qualitative data to map findings to the CDC Crisis and Emergency Risk Communication framework.
Sources of data for evaluation were (1) collated tracking sheets from Communication Leaders documenting daily outreach numbers and communication mechanisms, (2) summary notes from daily teleconferences with Communication Leaders, and (3) summaries of semi-structured interviews with Communication Leaders who provided status updates on what strategies were working, how they had adapted the intervention, and suggestions for improvement. Acceptability and feasibility of the intervention were assessed by the interviews with Communication Leaders and by summary notes from daily teleconferences.
Tracking data were reported as frequencies to assess intervention reach. Content analysis conducted on notes from teleconferences and interviews was entered in NVivo 12 software (QSR International, Pty. Ltd.). Codes were assigned to note text representing concepts in the data to facilitate queries for analysis. Analysis was completed across subgroups and mapped to the CDC Crisis and Emergency Risk Communication framework.
Results
The intervention was delivered by 24 Communication Leaders (11 Somali, 6 Hispanic, 2 Cambodian, 3 South Sudanese, 1 Anuak, 1 Ethiopian). In addition to the three main message maps, eight COVID-19 updates were translated and disseminated. In addition to bidirectional communication between all partners on daily telephone conferences, 40 emails, text messages, or phone calls were sent to Communication Leaders in response to new COVID-19 developments or community concerns.
Intervention Reach
A total of 9882 individuals received messages from Communication Leaders through 9 different communication platforms over a 14-day interval (Table 1). The most common communication platforms were Facebook, voice telephone calls, and text messaging (conventional, WhatsApp, and Viber).
Table 1. Number of individuals to whom COVID-19 messages were distributed and communication mediums used

Acceptability and Feasibility
All of the Communication Leaders judged the intervention to be highly relevant and responsive to community needs in a time of crisis. This led to a perception of empowerment for Communication Leaders and their communities in facing the pandemic. Feasibility of applying the framework during the initial 14-day interval was demonstrated to be high in the context of very motivated community partners. Some Communication Leaders reflected that the logistics of applying the intervention framework would have to be flexible in order to sustain momentum in the future. For example, as the economy begins to re-open, meeting times and frequency may have to change to accommodate Communication Leaders’ increasingly busy lives.
Risk Communication Framework
Table 2 summarizes evaluation findings mapped to the CDC Crisis and Emergency Risk Communication phases of preparation, initial messaging, maintenance, and resolution. In the preparation phase, credibility of RHCP as a partnership and preexisting trust by vulnerable communities was identified as an important intervention facilitator. In the initial implementation phase, action-oriented messages were generated in a participatory way with RHCP partners. This process was perceived as adding credibility to the messages by fully incorporating community voice while staying true to the facts. In the maintenance phase of implementation, daily bidirectional communication was important to revise message content, generate new messages in response to community concerns, and connect community groups to existing resources. RHCP served as a source of strength for Communication Leaders, which enabled community ownership of the intervention.
Table 2. Strategies for implementation of centers for disease control and prevention communication and emergency risk communication phases with vulnerable populations in the COVID-19 pandemic by a community engaged research partnership

Abbreviations: COVID-19, coronavirus disease 2019; CEnR, community engaged research; CDC, Centers for Disease Control and Prevention; WHO, World Health Organization.
* Task force members included community and academic leaders, Communication Leaders, other volunteers and representatives from regional community-based organizations.
Discussion
This study describes the ways an existing CEnR partnership leveraged its credibility and trust with vulnerable populations for risk communication in the COVID-19 pandemic. By adopting a risk communication framework, co-creating messages with community leaders and health experts, and modifying messages daily, Communication Leaders felt supported in disseminating accurate COVID-19 messages to their networks. Rapid evaluation and assessment methods through tracking, daily teleconferences, and weekly interviews allowed the team to adapt the messages and connect community members to resources in real time. Community concerns were used to influence local testing policies and practices by healthcare partners. In these ways, the intervention is one example of how previously articulated best practices for pandemic risk communication to vulnerable populations may be applied [Reference Vaughan and Tinker13].
CEnR partnerships have grown rapidly in recent years within the health equity space [Reference Ortiz, Nash and Shea7]. This study demonstrated that CEnR partnerships are uniquely poised to respond to pandemic risk communication needs with at-risk communities through ready access to disease content expertise from academic partners and community expertise from community partners. Furthermore, this study described the ways in which a CEnR partnership leveraged community capacity for rapid evaluation and data collection through past research experiences. Processes and products from this intervention may be adapted by other CEnR partnerships for local contexts. For example, two additional CEnR partnerships within the Mayo Clinic enterprise are in the early stages of applying components of the intervention framework in Minnesota and Florida. Finally, implementation of the RHCP intervention framework has continued into its second month with engaged Communication Leaders and community partners, which provides preliminary evidence for the sustainability of the intervention.
The study has limitations. We did not assess dissemination of the messages beyond the initial distribution from Communication Leaders. Therefore, the full intervention reach cannot be assessed across social networks (message amplification). The number of individuals reached by Communication Leaders may have been overestimated if individuals received messages from more than one Communication Leader via overlapping networks. Engagement data from social media platforms were not collected. Furthermore, risk-related behaviors and outcomes were not assessed. Finally, CEnR partnership work is highly contextual, so this process may not be generalizable to some partnerships.
Conclusion
By leveraging existing networks and credibility, CEnR partnerships may effectively implement crisis and emergency risk communication to vulnerable populations in the COVID-19 pandemic.
Acknowledgments
RHCP COVID-19 Task Force Collaborators include Omar Nur, Hindi Elmi, Graciela Porraz Capetillo, Kim Sin, Marissa Thach, Mohamud Nur, Miguel Valdez Soto, Omot Bawar, Elizabeth Mayor, Murayad Hasan, Anab Mohamed, Biyod Shakie, Hawo Hilowle, Musse Abdisalam, Armin Budimlic, Athieei Lam, Nyanjok Lam, Selamawit Unger, Rebecca Sedarski, Gloria Herbeck, Ahmed A. Mohammed, Leah Espinda-Brandt, Deborah Trahan, and Jennifer A. Weis. Institutional partners include Intercultural Mutual Assistance Association; Somali American Social Service Association; Alliance of Chicanos, Hispanics, and Latin Americans; Cambodian Association of Rochester Minnesota; and Olmsted County Public Health Services; all from Rochester, Minnesota. The authors thank LaPrincess C. Brewer, MD, MPH, and Richard O. White, MD, for their leadership in adapting the intervention framework with other CEnR partnerships.
This publication was supported by CTSA Grant No. UL1 TR000135 from the National Center for Advancing Translational Science (NCATS) to Mayo Clinic. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCATS. The funding bodies had no role in study design; in the collection, analysis, and interpretation of data; writing of the manuscript; and in the decision to submit the manuscript for publication.
Disclosures
The authors have no conflicts of interest to declare.





