Background
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus was first identified in Wuhan, China, in December 2019 and has since spread widely across the globe; the World Health Organization (WHO) declared it a global pandemic in March of this year.1,Reference Huang, Wang and Li2 As more patients became ill with the disease, clinicians recognized that coronavirus disease 2019 (COVID-19) disproportionately affects the elderly, in particular long-term care facility (LTCF) residents.Reference Onder, Rezza and Brusaferro3,Reference Wu, Chen and Cai4 As of July 30, 2020, there have been 4,339,997 confirmed cases of COVID-19 and 148,866 associated fatalities in the United States.5 Although LTCF residents only make up 3.5% of all COVID-19 cases, this population has contributed to 64.9% of total mortalities due to COVID-19.6 A similar situation is occurring in other countries.Reference Danis, Fonteneau and Georges7,Reference Burki8 In this review, we have synthesized the epidemiology of COVID-19 in LTCFs, clinical presentations and outcomes in this population, containment interventions, and the role of LTCF healthcare workers in SARS-CoV-2 transmission.
Literature review methods
We examined relevant published studies in Medline and PubMed using the following key terms: COVID-19, SARS-CoV-2, assisted living, group home, and memory care. We also reviewed current Centers for Disease Control (CDC) and Centers for Medicare and Medicaid Services (CMS) COVID-19 guidelines for LTCFs.
Epidemiology
In LTCFs that have COVID-19 cases, SARS-CoV-2 positivity rates can vary widely (Table 1), with an average positivity rate of ~37%. Studies that examined COVID-19 outbreaks in LTCFs had higher attack rates on average (42.9%),Reference Arons, Hatfield and Reddy9–Reference Roxby, Greninger and Hatfield18 but 3 studies surveyed nursing homes without regard to outbreak status and found a SARS-CoV-2 prevalence between 6% and 23%.Reference Borras-Bermejo, Martínez-Gómez and San Miguel19–Reference White, Kosar and Feifer21 The highest SARS-CoV-2 positivity rate recorded was by McMichael et alReference McMichael, Currie and Clark15 at 77%, although this was a cumulative attack rate over a month.
Table 1. Summary of LTCF Studies Reviewed
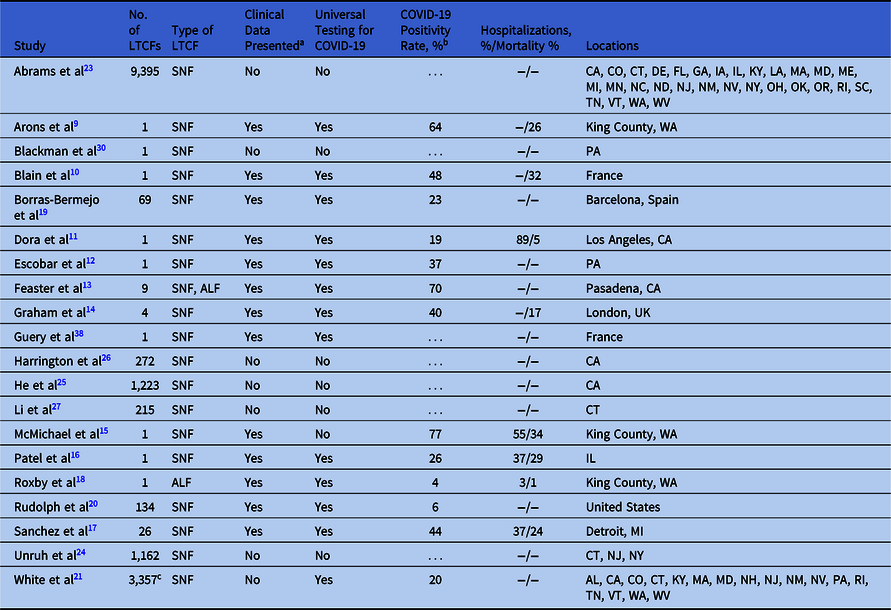
Note. LTCF, long-term care facility; SNF, skilled nursing facility; ALF, assisted-living facility; “…” and “–” indicate that data were not available for the corresponding entry.
a Yes = study presents data on prevalence of SARS-CoV-2, hospitalization rates, mortality rates, and/or symptoms of residents and/or staff. No = none of the data are presented.
b Positivity rate encompasses both attack rates and prevalence rates.
c 69 of the 3,357 LTCFs underwent universal testing.
Numerous studies have attempted to identify associations between LTCF characteristics and COVID-19 incidence. Studies using the CMS Five-Star Quality Rating System reported that increased nursing-home size and degree of occupancy appear strongly associated with higher likelihood of having at least 1 resident with COVID-19.Reference White, Kosar and Feifer21–Reference Unruh, Yun, Zhang, Braun and Jung24 LTCF resident demographics also influence the probability of having at least 1 COVID-19 case. Higher proportion of African-American residents, lower proportion of white residents, and higher Medicaid share were all associated with higher numbers of COVID-19 cases.Reference Abrams, Loomer, Gandhi and Grabowski23–Reference He, Li and Fang25 Staffing levels and CMS staffing rating of LTCFs may also affect COVID-19 spread. In California, lower nurse staffing hours per resident per day and lower Five-Star nursing score were both associated with increased risk of COVID-19 cases in the facilities.Reference Harrington, Ross, Chapman, Halifax, Spurlock and Bakerjian26 Similarly, in Connecticut, decreased nursing hours were associated with an increased number of COVID-19 cases.Reference Li, Temkin-Greener, Gao and Cai27 Among facilities with at least 1 death attributed to COVID-19, higher numbers of nursing hours were protective.Reference Li, Temkin-Greener, Gao and Cai27 Other factors associated with greater incidence of COVID-19 included higher levels of LTCF resident independence, higher number of CMS health deficiencies, and for-profit status.Reference White, Kosar and Feifer21,Reference Abrams, Loomer, Gandhi and Grabowski23–Reference Harrington, Ross, Chapman, Halifax, Spurlock and Bakerjian26 Li et al found that nurse staffing, CMS Five-Star rating, and concentrations of Medicaid and racial/ethnic minorities in the facilities were associated with COVID-19 in LTCFs that had least 1 case, even after controlling for county-level variables.Reference Li, Temkin-Greener, Gao and Cai27 White et alReference White, Kosar and Feifer21 reported that county-level transmission was the strongest predictor of COVID-19 cases in LTCFs across 31 states: for every increase in 1,000 COVID-19 cases per 100,000 residents in any county, there was an associated 33.6% greater likelihood of COVID-19 cases in the facility.Reference White, Kosar and Feifer21
Eight studies evaluated the presence of comorbidities among LTCF resident with COVID-19 (Table 2). Residents with COVID-19 had high rates of hypertension, cardiac disease, diabetes, and cognitive impairment.Reference Arons, Hatfield and Reddy9,Reference Dora, Winnett and Jatt11,Reference Escobar, Lanzi and Saberi12,Reference McMichael, Currie and Clark15,Reference Roxby, Greninger and Hatfield18 Comparisons between COVID-19–positive and COVID-19–negative residents showed that renal disease (P < .001), pulmonary disease (P < .056), dementia (P = .023), severe cognitive impairment (P < .001), and obesity (P = .026) were associated with SARS CoV-2 positivity.Reference Blain, Rolland and Tuaillon10,Reference Graham, Junghans and Downes14,Reference Rudolph, Halladay and Barber20 Furthermore, cardiovascular disease was strongly associated with increased mortality (χ2 = 10.8; P = .001).Reference Graham, Junghans and Downes14
Table 2. Comorbidities in LTCF Residents With COVID-19 in Reviewed Studiesa
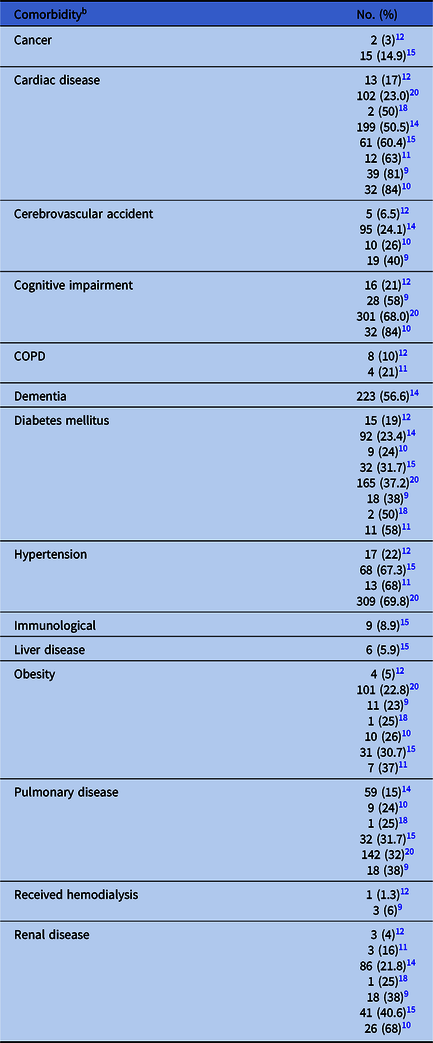
Note. COPD, chronic obstructive pulmonary disease.
a Only studies that preset clinical data are listed.
b Some comorbidity categories were consolidated.
Clinical presentation
Clinical presentation of COVID-19 can be variable in the LTCF population (Table 3). Four studies reported that between 69.7% and 93% of LTCF residents experienced typical COVID-19 symptoms such as fever, cough, dyspnea, or hypoxia.Reference Arons, Hatfield and Reddy9,Reference Blain, Rolland and Tuaillon10,Reference McMichael, Currie and Clark15,Reference Borras-Bermejo, Martínez-Gómez and San Miguel19 Other case reports have shown a high prevalence of fevers and cough alongside anorexia, headaches, diarrhea, and fatigue.Reference Dora, Winnett and Jatt11,Reference Patel, Chaisson and Borgetti16 Graham et alReference Graham, Junghans and Downes14 reported a strong association between anorexia, cough, and breathlessness and SARS-CoV-2 positivity. Given the low rate of fever among the elderly, it was not surprising that fever was not associated with increased odds of having a positive SARS-CoV-2 test. In fact, a study by Rudolph et alReference Rudolph, Halladay and Barber20 showed that only 26.6% of SARS-CoV-2 positive residents reached a fever of 38.0°C during their 28-day observation period. Neither anosmia or ageusia have been reported in the literature among this population.
Table 3. Signs and Symptoms Among COVID-19 LTCF Residents in Reviewed Studiesa
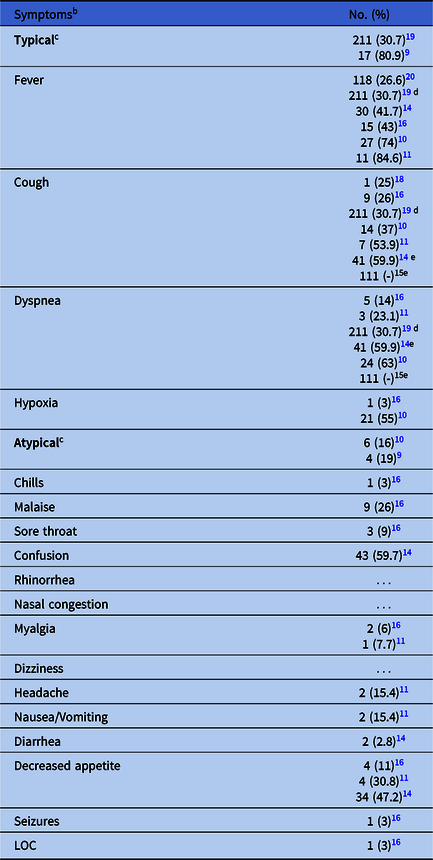
Note. LTCF, long-term care facility; LOC, loss of consciousness; “…” indicates that data was not available for the corresponding entry.
a Only studies that present clinical data are listed.
b Some symptom categories were consolidated.
c Categories of “typical” and “atypical” are based on the CDC symptom categorization.
d This study reported an aggregate incidence rate of fever, cough, and dyspnea.
e These studies reported aggregate incidence rates of cough and dyspnea.
Interestingly, typical COVID-19 symptoms were observed in SARS-CoV-2–negative residents, ranging from 10.6% to 54%.Reference Arons, Hatfield and Reddy9,Reference Blain, Rolland and Tuaillon10,Reference Graham, Junghans and Downes14,Reference Roxby, Greninger and Hatfield18,Reference Borras-Bermejo, Martínez-Gómez and San Miguel19 Asymptomatic SARS-CoV-2 infections were also identified, with rates from 16% to 69.7%.Reference Arons, Hatfield and Reddy9,Reference Blain, Rolland and Tuaillon10,Reference Escobar, Lanzi and Saberi12-Reference Graham, Junghans and Downes14,Reference Patel, Chaisson and Borgetti16,Reference Sanchez, Biedron and Fink17,Reference Borras-Bermejo, Martínez-Gómez and San Miguel19 In studies by Arons et alReference Arons, Hatfield and Reddy9 and Escobar et al,Reference Escobar, Lanzi and Saberi12 88%–92% of residents with asymptomatic infections developed symptoms during subsequent follow up. By contrast, Graham et alReference Graham, Junghans and Downes14 and Patel et alReference Patel, Chaisson and Borgetti16 reported only 3% to 10% of asymptomatic infections developing subsequent symptoms among nursing-home residents.
Prognosis
Following COVID-19 diagnosis, many LTCF residents required subsequent hospitalization or expired (Table 1). The average hospitalization rate of SARS-CoV-2–positive residents across all studies was 44% and the average mortality rate was 21%.Reference Arons, Hatfield and Reddy9-Reference Dora, Winnett and Jatt11,Reference Graham, Junghans and Downes14–Reference Roxby, Greninger and Hatfield18 The highest hospitalization rate was reported by Dora et alReference Dora, Winnett and Jatt11 at 89%; however, these researchers stated that transfers to acute-care settings were primarily driven early in the pandemic by the need to isolate these residents from others in the facility. The highest fatality rate reported to date was 33.7% in a 130-bed LTCF in Washington State.Reference McMichael, Currie and Clark15
Containment interventions
A wide array of interventions have been used by LTCFs to prevent and/or halt outbreaks of COVID-19 (Table 4). Surveillance and social distancing were used almost universally, with group activities cancelled and daily screening of residents, staff, and visitors effected.Reference Arons, Hatfield and Reddy9,Reference McMichael, Currie and Clark15 Visitation restrictions were also enacted upon recommendation of the CDC and CMS to prevent introduction of COVID-19 from the community into LTCFs.28,29 Although no studies have examined this issue directly, reports by Graham et alReference Graham, Junghans and Downes14 and Blackman et alReference Blackman, Farber, Feifer, Mor and White30 show that, even with stringent visitation restrictions, COVID-19 can still be introduced to LTCFs. Once an outbreak occurred, cohorting was universally used in an attempt to mitigate the spread of COVID-19. However, due to limited supplies of SARS-CoV-2 rRT-PCR tests, universal testing among residents and staff was not performed, thereby limiting the effectiveness of cohorting interventions.Reference Blackman, Farber, Feifer, Mor and White30,Reference Shear, Kaplan, Fink, Thomas and Weiland31 As tests became more widely available and evidence emerged of asymptomatic transmission, universal testing during LTCF outbreaks was recommended.Reference Arons, Hatfield and Reddy9,Reference Wei, Li, Chiew, Yong, Toh and Lee32 Cohorting and universal testing have proven effective; facilities in California and Illinois that utilized these methods saw a significant reduction in incidence and fatality rate when compared to earlier studies that did not use universal testing to guide cohorting.Reference Arons, Hatfield and Reddy9,Reference Dora, Winnett and Jatt11,Reference McMichael, Currie and Clark15,Reference Patel, Chaisson and Borgetti16,Reference Blackman, Farber, Feifer, Mor and White30 In May 2020, the CDC recommended that all nursing-home residents and healthcare workers (HCWs) should be tested if a case of COVID-19 is detected, followed by weekly testing of negative residents until no new cases are detected.33 Subsequent studies have reinforced the value of this approach.Reference Blain, Rolland and Tuaillon10,Reference Escobar, Lanzi and Saberi12,Reference Sanchez, Biedron and Fink17
Table 4. Containment Interventions Utilized by LTCF in Reviewed Studiesa
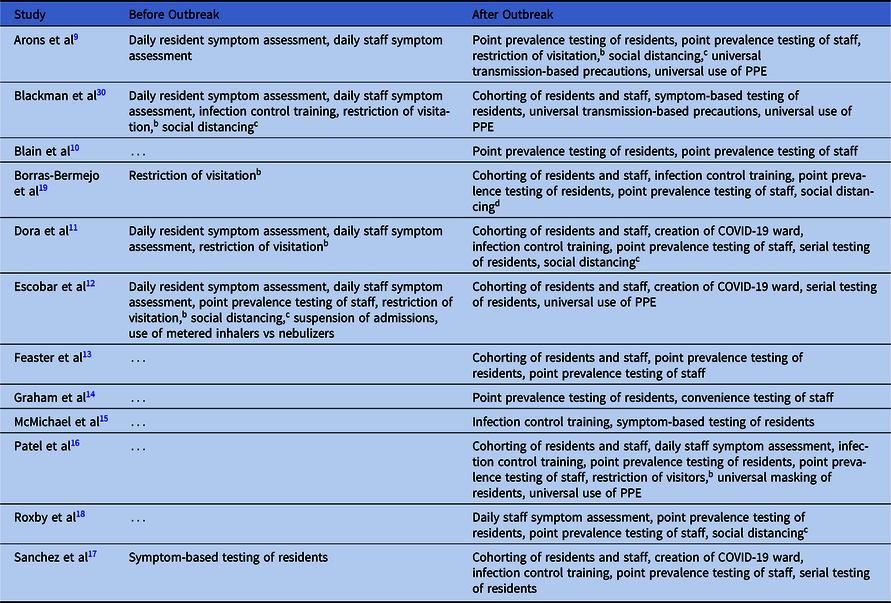
Note. LTCF, long-term care facility; PPE, personal protective equipment; “…” indicates that a containment intervention was not listed for the corresponding period.
a Only studies describing containment interventions are listed.
b All visitors restricted from entering the facility.
c Communal dining and activities cancelled.
d Communal dining and activities cancelled but residents continued to share rooms.
Role of HCWs
Nosocomial transmission in medical settings is often driven by HCWs unknowingly transmitting illnesses to the patients they care for.Reference Vos34 Given that HCWs have been found to be asymptomatic carriers of SARS-CoV-2, current recommendations stress the use of personal protective equipment to prevent viral spread within LTCFs.28,Reference Contejean, Leporrier and Canouï35,Reference Mani, Budak and Lan36 Three studies presented epidemiological evidence of such transmission. In a Pennsylvania LTCF, 2 HCWs who lived together but worked on different units concurrently tested positive for SARS-CoV-2, causing clusters of cases on their respective units.Reference Blackman, Farber, Feifer, Mor and White30 In King County, Washington, interfacility spread of COVID-19 was facilitated via shared HCWs who worked at multiple facilities.Reference McMichael, Currie and Clark15 In addition, genetic sequencing data collected during an outbreak in a London LTCF showed similar SARS-CoV-2 sequence data among a group of residents and a single HCW who cared for them.Reference Graham, Junghans and Downes14
A prevalence study of SARS-CoV-2 infection among general practitioners and nurses from primary-care centers and nursing homes in León, Spain, reported that the prevalence of SARS-CoV-2 was higher in nursing homes than in primary-care centers (9.5% vs 5.5%). However, no statistically significant differences were observed by sex, type of professional, level of exposure, or compliance with preventative measures.Reference Martín, Fernández-Villa and Lamuedra Gil de Gomez37 In other studies that measured COVID-19 prevalence among LTCF HCWs, values ranged from 2.2% to 62.6%.Reference Arons, Hatfield and Reddy9-Reference Feaster and Goh13,Reference McMichael, Currie and Clark15,Reference Patel, Chaisson and Borgetti16,Reference Roxby, Greninger and Hatfield18,Reference Borras-Bermejo, Martínez-Gómez and San Miguel19,Reference Guery, Delaye and Brule38 Positive SARS-CoV-2 cases in LTCF studies included both frontline nursing staff as well as ancillary workers. Although most SARS-CoV-2–positive cases have occurred among LTCF nursing staff, other personnel, such as physicians, physical, speech and occupational therapists, case managers, health information officers, and environmental services, have also been affected.Reference Arons, Hatfield and Reddy9,Reference McMichael, Currie and Clark15
Identification of positive HCWs via symptom screening can be problematic because HCWs in LTCFs can be asymptomatic, with only 19% to 55.8% of staff exhibiting symptoms such as cough, fever, sore throat, dyspnea, headaches, or myalgias.Reference Arons, Hatfield and Reddy9,Reference Patel, Chaisson and Borgetti16,Reference Roxby, Greninger and Hatfield18,Reference Borras-Bermejo, Martínez-Gómez and San Miguel19 Further complicating infection prevention measures, 9.75% to 40% of HCWs with negative SARS-CoV-2 test results had symptoms characteristic of COVID-19, and 4% to 55.8% were asymptomatic with a positive test.Reference Arons, Hatfield and Reddy9,Reference Blain, Rolland and Tuaillon10,Reference Feaster and Goh13,Reference Graham, Junghans and Downes14,Reference Roxby, Greninger and Hatfield18,Reference Borras-Bermejo, Martínez-Gómez and San Miguel19,Reference Martín, Fernández-Villa and Lamuedra Gil de Gomez37,Reference Guery, Delaye and Brule38
Many COVID-19 infection prevention measures are focused on staff use of personal protective equipment (PPE) and, therefore, can be hindered by shortages of these supplies. In a survey of US LTCFs early in the pandemic, 72% reported having inadequate access to PPE, 88% of surveyed facilities reporting a shortage of face shields, and 64% of surveyed facilities reporting a shortage of surgical masks.Reference Quigley, Dick, Agarwal, Jones, Mody and Stone39 HCWs in LTCFs have continued to work despite having symptoms consistent with COVID-19. In a study of 50 HCWs who tested positive during the initial cluster of COVID-19 in Washington State, 64% reported working while exhibiting symptoms.Reference Chow, Schwartz and Tobolowsky40
In conclusion, our review of recent studies and guidelines for COVID-19 in LTCFs has identified several key observations as well as areas for further investigation. First, emerging data indicate that certain facility characteristics are associated with increased likelihood of having at least 1 COVID-19 case in an LTCF: Five-Star rating, resident demographics, staffing levels, and county-level transmission. In addition, once SARS-CoV-2 is introduced into an LTCF, it can quickly spread, leading to high rates of morbidity, hospitalization, and mortality. Infection control interventions, such as cohorting and universal testing of staff and residents, appear to be effective. Many studies have indicated the effectiveness of these strategies to mitigate COVID-19 outbreaks. Given the disproportionate transmission, morbidity, and mortality in the nursing-home population, more studies are needed that incorporate novel containment interventions in LTCFs.
Acknowledgments
Financial support
This work was supported by funding from the Advancing a Healthier Wisconsin Endowment (to A.H.W.).
Conflicts of interest
All authors report no conflicts of interest relevant to this article.







