1. Introduction
Major challenges to global sustainability have been met with numerous calls to do things differently. The Sustainable Development Goals call for ‘bold and transformative steps’ (UN, 2015). The 2019 Global Sustainability Report concluded that, in order to achieve sustainability, ‘transformations’ will be needed across a range of different systems (IGS, 2019). The Financial Times believes it is ‘Time for a Reset’ – of capitalism itself – to ensure that corporations pursue profit with purpose rather than with undue costs to environment, society and health (Financial Times, 2019).
Many across business, government, civil society and academia now see the COVID-19 pandemic as the opportunity for change – to ‘build back better’. In their ‘Manifesto for a healthy recovery from COVID-19’, the World Health Organization (WHO) suggests that COVID-19 highlights the ‘false economy’ of short-term policymaking and argues that longer-term approaches are necessary for a ‘healthier, fairer, and greener world’ (WHO, 2020f). In the context of the inequalities revealed by COVID-19, the United Nations (UN) Secretary General is proposing a ‘New Social Contract’ (UN, 2020). On the basis that ‘the inconsistencies, inadequacies and contradictions of multiple systems – from health and financial to energy and education – are more exposed than ever’, the World Economic Forum echoes the Financial Times in appealing for ‘The Great Reset’ (World Economic Forum, 2020).
Yet what should such a reset look like? This Intelligence Briefing proposes that resetting systems to resolve long-term challenges will require five proactive changes to the way things are currently done. It identifies these changes from the evidence that solving major challenges – from pandemics to poverty, climate change to malnutrition – requires multiple systems to work synergistically (Atkinson & Nabarro, Reference Atkinson and Nabarro2020). Specifically, this Intelligence Briefing draws on the evidence that the causes, severity and effects of the COVID-19 pandemic emerged from the interconnections between different systems (Hawkes, 2020a). This Intelligence Briefing brings this evidence together and uses it to identify five vital steps needed to enable a global reset.
2. The role in multiple systems in COVID-19
Although numerous uncertainties remain, the evidence indicates that the causes, severity and effects of COVID-19 cut across multiple systems, as did the responses to it (Everard et al., Reference Everard, Johnston, Santillo and Staddon2020; Nicola et al., Reference Nicola, Alsafi, Sohrabi, Kerwan, Al-Jabir, Iosifidis and Agha2020). This Intelligence Briefing focuses on six such systems: environmental, health, political, social, economic and food systems (Figure 1). These systems can also be thought of as subsystems of one system. For example, health, the environment, society, politics and economics are all subsystems of the food system (Parsons et al., Reference Parsons, Hawkes and Wells2019).
Fig. 1. The role of multiple systems in the burden of COVID-19: examples of how multiple systems caused, responded to, were affected by and influenced the severity of COVID-19. PPE = personal protective equipment.
2.1. Environmental system
More evidence is needed to understand the exact origins of COVID-19. But it is clear that, broadly speaking, its origins lie in human impacts on the environmental system driven by economic concerns. Activities like deforestation, human settlement, mining and building transport infrastructure have led to closer interaction between animal pathogens and human populations, facilitating the transfer of viruses between animals and humans, as was the case for COVID-19 (Andersen et al., Reference Andersen, Rambaut, Lipkin, Holmes and Garry2020; Cheval et al., Reference Cheval, Mihai Adamescu, Georgiadis, Herrnegger, Piticar and Legates2020; UNEP & ILRI, 2020). Evidence shows that 71.3% of new infectious diseases, like COVID-19, have transferred to humans from wildlife, with the number increasing significantly over time (Jones et al., Reference Jones, Patel, Levy, Storeygard, Balk, Gittleman and Daszak2008). Researchers have concluded that the risk of transmission of these pathogens is higher when animals have had to adapt to human-dominated landscapes in the context of loss of habitat and biodiversity (UNEP & ILRI, 2020). Intensive agricultural production has also led to higher levels of interaction between wildlife and livestock, again increasing the probability of transfer from animals to humans (Jones et al., Reference Jones, Grace, Kock, Alonso, Rushton, Said and Pfeiffer2013). Human trade of wildlife has become more common, bringing humans into ever closer contact with animals, again facilitating the spill-over of viruses to humans (UNEP & ILRI, 2020).
Human disruption of the environmental system also appears to play a role in the severity of the disease: researchers have hypothesized that pollution may worsen the effects of COVID-19 for individuals by impairing the ‘first line of defence of the upper airways’ (Cheval et al., Reference Cheval, Mihai Adamescu, Georgiadis, Herrnegger, Piticar and Legates2020; Mehmood, Reference Mehmood, Saifullah and Abrar2020). At the same time, the reduction of economic activity in response to the pandemic appears to have benefitted air quality in built-up areas (Cheval et al., Reference Cheval, Mihai Adamescu, Georgiadis, Herrnegger, Piticar and Legates2020). There are also some predictions that greenhouse gas emissions are lower as a result (Le Quéré et al., Reference Le Quéré, Jackson, Jones, Smith, Abernethy, Andrew and Friedlingstein2020). On the other hand, the increased use of non-recyclable materials in protective equipment in the health system may worsen water pollution (Cheval et al., Reference Cheval, Mihai Adamescu, Georgiadis, Herrnegger, Piticar and Legates2020). Environmental systems thus play a key role in the origins and severity of COVID-19 and are, in turn, impacted by the responses to contain it.
2.2. Health system
Once the coronavirus arose and started to spread, the primary burden for responding to it lay with the health system. The WHO's diagnosis was that effectively managing the disease requires health system capacities to be in place to ‘detect, test, isolate and treat every case and trace every contact’ (WHO, 2020e). Their guidance on treatment called on countries to develop effective emergency response systems, build capacity to detect the disease and care for patients, ensure hospitals have the necessary staff and supplies and deliver life-saving medical interventions (WHO, 2020d). As it was put by the WHO Director General, ‘[T]he best defence against any outbreak is a strong health system’ (WHO, 2020g).
Yet many countries faced major challenges in testing, tracing, providing critical care and accessing sufficient human resource capacity to do so (Chersich et al., Reference Chersich, Gray, Fairlie, Eichbaum, Mayhew, Allwood and Haghighi2020). There were widespread reports from around the world that health systems were, as one WHO spokesperson put it, ‘collapsing under the pressure of too many cases’ (CNBC, 2020). Despite evidence that protective equipment is effective at preventing transmission to the health workforce (Liu et al., Reference Liu, Cheng, Xu, Yang, Zhu, Zhang and Yao2020), supplies have been inadequate (WHO, 2020b), and many healthcare workers have died. There is also concern that other necessary health services are being compromised as a result of capacity being taken by the COVID-19 response (WHO, 2020a). By being key to the response, health system capacity thereby influenced the severity of the disease within and between countries (Walker et al., Reference Walker, Whittaker, Watson, Baguelin, Winskill, Hamlet and Thompson2020).
2.3. Political system
Primary responsibility for implementing the response to COVID-19 lay with the political system. With a clear imperative to react, politicians everywhere were affected. Underpinning decisions at the international, national and municipal levels around how to respond were concerns about the human cost, the burden on health systems and the economic, political and social trade-offs involved. Along with policy choices about health systems, the primary policy to alleviate the severity of COVID-19 was ‘social distancing’ (WHO, 2020c). Policymakers in at least 160 countries imposed ‘lockdowns’ to limit person-to-person transmission (Hale et al., Reference Hale, Angrist, Kira, Petherick, Phillips and Webster2020). While lockdown policies varied significantly in their type, stringency and timing, common measures included restrictions in meeting people outside of the household, limits on public gatherings, closing schools, physical distance measures and travel restrictions (Hale et al., Reference Hale, Angrist, Kira, Petherick, Phillips and Webster2020).
Political leadership appeared to be key to influencing the effectiveness of the response (Forman et al., Reference Forman, Atun, McKee and Mossialos2020). In some countries, such as Brazil, the UK and the USA, policy responses were widely criticized for being inadequate and blamed for high numbers of deaths. By contrast, the rapid and comprehensive political response in countries such as Denmark, New Zealand and Vietnam appears to have mitigated the severity (Hinchman et al., Reference Hinchman, Ali, Goodwin, Gillie, Boudreaux and Laborde2020; Potter, Reference Potter2020). While empirically measuring the relationships between the lockdown response and incidence rates is tricky (Hale et al., Reference Hale, Angrist, Kira, Petherick, Phillips and Webster2020), political choices about the degree of social distancing measures do appear to have influenced the severity of the virus (Thu et al., Reference Thu, Ngoc and Hai2020). Geopolitical interests also played out at an international scale as national governments and UN agencies jostled for political power and influence.
2.4. Social system
The lockdown measures implemented to reduce the spread of COVID-19 had major effects on social systems, since people were unable to interact as before. It was already well established prior to the pandemic that social isolation is a major risk factor for a range of poor health outcomes (e.g., Leigh-Hunt et al., Reference Leigh-Hunt, Bagguley, Bash, Turner, Turnbull, Valtorta and Caan2017). Demand for mental health helplines reportedly surged during lockdown (e.g., Smith & Lim, Reference Smith and Lim2020), and evidence showed that enforced quarantine led to anxiety, depression and post-traumatic stress (Brooks et al., Reference Brooks, Webster, Smith, Woodland, Wessely, Greenberg and Rubin2020). Experts voiced concern about a ‘second pandemic’ of mental health problems (Choi et al., Reference Choi, Heilemann, Fauer and Mead2020). There were also reports of increased levels of domestic abuse and child abuse (Bradbury-Jones & Isham, Reference Bradbury-Jones and Isham2020; Taub, Reference Taub2020).
Yet the social system also responded positively to COVID-19. There are numerous examples of self-organized community groups and community kitchens, of neighbours supporting vulnerable people, carrying out food shopping and collecting medical prescriptions and of people connecting via electronic platforms. Another aspect of the social system, however, influenced its severity: social attitudes influenced whether people actually adhered to social distancing rules (Pedersen & Favero, Reference Pedersen and Favero2020). Reports from the USA, for example, indicate that social attitudes towards science affected the degree of compliance with lockdowns (Brzezinski et al., Reference Brzezinski, Kecht, Van Dijcke and Wright2020). Social systems were thus profoundly affected by COVID-19, but also played a role in influencing its severity and the response to it.
2.5. Economic system
As described in Section 2.1, human economic activity played a major role in the origins of COVID-19; it was also one of the systems most severely impacted. By cutting consumption and reducing people's ability to work and produce, social distancing measures sent economic shockwaves throughout the global economy (World Bank, 2020; Gopinath, Reference Gopinath2020b). In the USA, total retail sales fell 8.7% in March 2020 (Warren, Reference Warren2020). With clothing seeing the greatest decline (50.5%), this had major repercussions for economies that supply these clothes, with millions of jobs reported to be lost in Bangladesh, Cambodia, China and Vietnam (Nortajuddin, Reference Nortajuddin2020). China's economy is reported to have declined by 6.8% in the first 3 months of 2020 – this is the country's first recorded contraction (Kuo, Reference Kuo2020).
With global GDP growth falling by 3.0% in April and 4.9% in June 2020, the International Monetary Fund (IMF) is predicting losses to the global economy of over US$12 trillion in 2020–2021 (Gopinath, Reference Gopinath2020a) and the worst economic depression since the 1930s (Gopinath, Reference Gopinath2020b). In response, they are recommending that ‘fiscal policy should urgently provide sizable support for affected people and firms during the pandemic’ (IMF, 2020b). Governments everywhere have put in place fiscal stimulus packages and monetary policies (Hale et al., Reference Hale, Angrist, Kira, Petherick, Phillips and Webster2020; IMF, 2020a). Global fiscal support of over US$10 trillion and easing of monetary policy is reported to have prevented the fallout from being even worse, especially in higher-income nations (Gopinath, Reference Gopinath2020a). The negative consequences of lockdowns on economic activity were also a major driving force behind political decisions about how and when to ‘reopen’ economies.
Economic downturns also impacted heavily at the household level through loss of jobs and income (e.g., Tran et al., Reference Tran, Hensing, Wingfield, Atkins, Annerstedt, Kazibwe and Lönnroth2020), exacerbating existing inequalities, given that the risks were greater for poorer households (e.g., Qian & Fan, Reference Qian and Fan2020). The policy response has been a range of measures to support families financially. As of 12 June 2020, 173 countries had enacted 621 such measures, including cash transfers and in-kind food and voucher schemes (Gentilini et al., Reference Gentilini, Almenfi, Dale, Lopz, Mujica, Quintana and Zafar2020).
2.6. Food system
At the very start of the pandemic, consumer stockpiling in many countries led to food shortages in shops. While the impact was short term, social distancing measures then had longer-term ripple effects across the system. By shutting down food service outlets, small stores and markets, thereby limiting the movement of the food workforce, restricting transportation and influencing consumer demand, lockdowns affected the ability to produce and sell food (FAO, 2020; Haddad et al., Reference Haddad, Fanzo and Hawkes2020; Swinnen & McDermott, Reference Swinnen and McDermott2020). At the same time, innovations such as e-commerce and local direct producer–consumer marketing initiatives sprang up to keep supply chains moving (Hawkes, Reference Hawkes, Swinnen and McDermott2020b).
The impact on the food system was intimately connected to the impact on the economic system, in part because the food system is an economic system. In addition, the economic impact of the pandemic on the ability of households to afford food compounded problems of production and supply, affecting food access. In this context, national and local governments, businesses and community groups put in place food vouchers and meal schemes for people negatively affected economically and for vulnerable and self-isolating groups (C40, 2020). Despite these efforts, international bodies have voiced major concerns that COVID-19's dual economic and food system impacts could prompt a widespread food crisis. The Food and Agriculture Organization (FAO) and World Food Programme (WFP) predict a food crisis in at least 27 countries ‘as the pandemic's knock-on effects aggravate pre-existing drivers of hunger’ (FAO & WFP, 2020). Research suggests that there could be a 14.3% increase in the prevalence of children under age 5 with inadequate weight compared to their height (Headey et al., Reference Headey, Heidkamp, Osendarp, Ruel, Scott, Black and Walker2020). It is also being reported that the refocusing of health systems on the pandemic, combined with budget shortfalls, has reduced the capacity to deliver basic undernutrition interventions (FAO & WFP, 2020).
While much of the focus has been on the impact on the food system, the food system also played a major role in the severity of COVID-19. Before the pandemic, unhealthy diets were estimated to be the second leading single cause of global ill health and premature mortality in the world (Gakidou et al., Reference Gakidou, Afshin, Abajobir, Abate, Abbafati, Abbas and Abu-Raddad2017). During the pandemic, it emerged that conditions directly associated with unhealthy diets – obesity and non-communicable diseases – raise the risk of complications of COVID-19. Evidence indicates that obesity, especially more severe obesity, is associated with increased death rate and/or treatment requiring invasive ventilation (Busetto et al., Reference Busetto, Bettini, Fabris, Serra, Dal Pra’, Maffei and Vettor2020; Goyal et al., Reference Goyal, Ringel, Rajan, Choi, Pinheiro, Li and Chen2020, Palaiodimos et al., Reference Palaiodimos, Kokkinidis, Li, Karamanis, Ognibene, Arora and Mantzoros2020; PHE, 2020; Popkin et al., Reference Popkin, Du, Green, Beck, Algaith, Herbst and Shekar2020; Tan et al., Reference Tan, He and MacGregor2020). Hypertension, diabetes and heart diseases – all of which are influenced by diets – have also been found to increase the risk of complications and hospitalization (Cummings et al., Reference Cummings, Baldwin, Abrams, Jacobson, Meyer, Balough and Hochman2020; Wiersinga et al., Reference Wiersinga, Rhodes, Cheng, Peacock and Prescott2020). The food system was not simply affected by COVID-19: it played a major role in its severity.
3. Implications for a global reset
The evidence in this Intelligence Briefing illustrates how the existence and severity of COVID-19 was a function of activity in multiple systems and the interconnections between them. By bringing together the evidence on the original causes, cross-system effects, severity and response to COVID-19, it becomes possible to see how the different systems combined to influence the burden of COVID-19 (Figure 1). Two systems – economic and environmental – had an interconnected role in the origins of the pandemic. The economic system was the ‘first cause’ through disrupting the environmental system. All of the systems influenced the severity of the disease – how many people contracted it, the extent to which there were complications and mortality – indicating that every system has a role to play in mitigating it. All of these systems also affected each other: responses implemented to address problems in one system inevitably led to effects on others. Lockdowns, for example, had negative spill-over effects on economic, social and food systems. Political leaders thus had to make choices about trade-offs between one negative effect over another – choices that influenced the severity of the disease. Historically, political choices have favoured short-term over longer-term goals, as reflected by the prioritization of economic goals over reducing the risk the transfer of pathogens from animals to humans. Similarly, choices about the food system have failed to prioritize diet-related health, also influencing the severity of COVID-19.
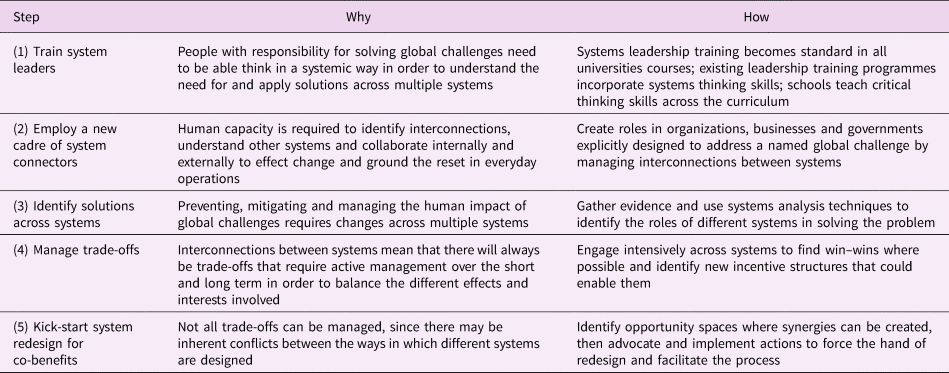
The role of multiple systems and the interconnections and contradictions between them over the short and long term provide important lessons on what is needed to effectively and sustainably manage global challenges more broadly. Five actions emerge as vital to enabling change (Table 1).
Table 1. Five vital steps for a global reset.
3.1. Step 1: train systems leaders
If people with responsibility for solving global challenges cannot think in a systemic way, they will not be able to understand nor apply solutions across multiple systems. Systems leadership skills are thus paramount in moving the reset forward (Nabarro, Reference Nabarro2020). Systems leadership is ‘a set of skills and capacities that any individual or organization can use to catalyse, enable and support the process of systems-level change’ (Dreier et al., Reference Dreier, Nabarro and Nelson2019, p. 4). It requires an ‘understanding of the complex systems shaping the challenge to be addressed’, an ability to ‘see and explain whole systems as well as their components’, and ‘to engage with systems from multiple perspectives at the same time’ (Atkinson & Nabarro, Reference Atkinson and Nabarro2019). This mind-set is necessary to enable working across system boundaries ‘with the explicit goal of creating change on complex, systemic issues’ (Dreier et al., Reference Dreier, Nabarro and Nelson2019, pp. 4, 7). Such an approach is not typical among decision-makers and managers. Rather, the focus of past decades has been on linear, competitive and often inward-looking leadership, with maximizing organisational performance as its main goal. Building systems thinking skills thus emerges as a crucial role for universities and leadership training programmes everywhere.
3.2. Step 2: employ a new cadre of systems connectors
Without the human capacity in organizations, businesses and governments to engage and connect with other systems, the ability to implement change will be severely limited. Building this function into existing jobs will not be sufficient owing to the evident complexity of the work. What is needed instead are a new cadre of professional ‘system connectors’ whose job it is to make connections across multiple systems at the middle management level. These ‘system connection managers’ can be thought of as the double-headed arrows in diagrams of complex systems. They would be charged with solving specific problems, not fixing systems per se. Food systems, for example, contain multiple problems (e.g., diet-related ill health, malnutrition, climate change, water, livelihoods, etc.), each of which needs a connector to work across subsystems to discuss and manage ways to align systems to solve the problem.
3.3. Step 3: identify solutions across systems
The first task of the systems connector is to identify what needs to change in each system to prevent, mitigate and treat the problem across all relevant systems/subsystems. Given the build-up of evidence in recent years, many of these solutions will already be known; the task is to bring them together and place them within a multi-systems context. This step is important for establishing the roles each system would ideally play in solving the problem. However, because acting in one system has effects on others, an ideal solution in one system may have negative knock-on effects in another, as shown very clearly in the case of COVID-19. The next step is thus to identify and manage trade-offs.
3.4. Step 4: manage trade-offs
Managing trade-offs involves making hard choices about the relative costs and benefit of one impact over another. The huge challenge for reset will be how to take the longer-term view for sustainability and human well-being when there are so many short-term political and economic interests at play. In the case of COVID-19, fiscal stimulus packages have mitigated some of the negative economic consequences. Yet their goal has tended to be to re-stimulate demand (i.e., to get people consuming again). While this will have short-term benefits, over the long term it places further pressures on the environmental system.
Managing trade-offs also extends beyond making tough decisions about costs and benefits to recognizing and managing a minefield of vested interests, power relations, contradictions and conflicts between different systems. For example, government regulation in the food system of the marketing of foods associated with obesity makes sense as an action to increase resilience to COVID-19 over the longer term. Yet this threatens the economic system in terms of food businesses attempting to recover in the shorter term. The dilemma here is that the trade-off involves other systems managed by a different set of people and interests (thus the need for systems connectors). New ways of acting will be needed to engage intensively in order to find win–win situations where possible, identifying what incentive structures are needed and negotiating compromises where necessary using system leadership skills.
Still, there will be cases where trade-offs are intractable. For instance, the current economic system is inherently reliant on consumers consuming more than is sustainable for the environment, health and society. As it has been put by the Global Sustainability Report 2019, ‘[C]reating economic growth just by increasing consumption of material goods is no longer a viable option at the global level’ (UN DESA, 2019). Here, there can be no ultimate win–wins over the long term; there is an inherent and intractable conflict, an indicator that the design of the economic system is fundamentally flawed and cannot be managed by trade-offs alone. Rather, the system needs to be redesigned so that it inherently produces co-benefits for other systems.
3.5. Step 5: kick-start systems redesign for co-benefits
The lack of feasibility in managing trade-offs is an indicator that, for sustainable, longer-term solutions, systems need to be redesigned to achieve different goals in synergy with one another (Parsons & Hawkes, Reference Parsons and Hawkes2018). Policymakers, businesses and organizations need to ‘proactively act to identify potential co-benefits during the [policy] design stage and shape implementation criteria to maximise impact’ (Hepburn, Reference Hepburn, O'Callaghan, Stern, Stiglitz and Zenghelis2020). Crucial in this regard is identifying opportunity spaces that can be leveraged in the short term to force the hand of a systems redesign in the longer term. One example to kick-start the process now would be imposing conditionalities on businesses in return for COVID-19 financial support packages. For example, in the USA, politicians proposed that the economic rescue package require airline companies to cut emissions by 2050 to 50% below 2005 levels (a goal to which the industry is already committed) (Tollefson, Reference Tollefson2020). It was not adopted by US Congress, showing the limitations imposed by a lack of political leadership. Nevertheless, there are many opportunity spaces; a key role of systems leaders and connectors is to identify them and to act within their own powers, recognizing that part of systems leadership is recognizing ‘it's up to us’ and ‘I can make a difference’ (Dreier et al., Reference Dreier, Nabarro and Nelson2019).
***
The lessons drawn from the evidence on the role of multiple systems in COVID-19 are not necessarily new. The importance of addressing root causes and social determinants of health has been part of the dialogue for decades (CSDH, 2008). Much of the sustainability conversation has been about the need to give greater priority to longer-term goals. Indeed, this was the core of the Sustainable Development Goals (UN, 2015). The call for systems leadership and managing trade-offs likewise preceded COVID-19 (Dreier et al., Reference Dreier, Nabarro and Nelson2019; IGS, 2019).
But the context is new. So if businesses, organizations, governments and international agencies are really serious about a global reset, now is the time to put these five steps to work, regardless of who else is doing so. The steps essentially provide a mechanism to hold them accountable: if they are not taking them, they are not doing enough. Nevertheless, with the short-term imperative to recover, this will be extraordinarily challenging. Given how hard it will be, those who are already taking such steps should share their experiences to enable others to learn from them, so advancing the collective courage needed to press the global reset button.




1. Introduction
Major challenges to global sustainability have been met with numerous calls to do things differently. The Sustainable Development Goals call for ‘bold and transformative steps’ (UN, 2015). The 2019 Global Sustainability Report concluded that, in order to achieve sustainability, ‘transformations’ will be needed across a range of different systems (IGS, 2019). The Financial Times believes it is ‘Time for a Reset’ – of capitalism itself – to ensure that corporations pursue profit with purpose rather than with undue costs to environment, society and health (Financial Times, 2019).
Many across business, government, civil society and academia now see the COVID-19 pandemic as the opportunity for change – to ‘build back better’. In their ‘Manifesto for a healthy recovery from COVID-19’, the World Health Organization (WHO) suggests that COVID-19 highlights the ‘false economy’ of short-term policymaking and argues that longer-term approaches are necessary for a ‘healthier, fairer, and greener world’ (WHO, 2020f). In the context of the inequalities revealed by COVID-19, the United Nations (UN) Secretary General is proposing a ‘New Social Contract’ (UN, 2020). On the basis that ‘the inconsistencies, inadequacies and contradictions of multiple systems – from health and financial to energy and education – are more exposed than ever’, the World Economic Forum echoes the Financial Times in appealing for ‘The Great Reset’ (World Economic Forum, 2020).
Yet what should such a reset look like? This Intelligence Briefing proposes that resetting systems to resolve long-term challenges will require five proactive changes to the way things are currently done. It identifies these changes from the evidence that solving major challenges – from pandemics to poverty, climate change to malnutrition – requires multiple systems to work synergistically (Atkinson & Nabarro, Reference Atkinson and Nabarro2020). Specifically, this Intelligence Briefing draws on the evidence that the causes, severity and effects of the COVID-19 pandemic emerged from the interconnections between different systems (Hawkes, 2020a). This Intelligence Briefing brings this evidence together and uses it to identify five vital steps needed to enable a global reset.
2. The role in multiple systems in COVID-19
Although numerous uncertainties remain, the evidence indicates that the causes, severity and effects of COVID-19 cut across multiple systems, as did the responses to it (Everard et al., Reference Everard, Johnston, Santillo and Staddon2020; Nicola et al., Reference Nicola, Alsafi, Sohrabi, Kerwan, Al-Jabir, Iosifidis and Agha2020). This Intelligence Briefing focuses on six such systems: environmental, health, political, social, economic and food systems (Figure 1). These systems can also be thought of as subsystems of one system. For example, health, the environment, society, politics and economics are all subsystems of the food system (Parsons et al., Reference Parsons, Hawkes and Wells2019).
Fig. 1. The role of multiple systems in the burden of COVID-19: examples of how multiple systems caused, responded to, were affected by and influenced the severity of COVID-19. PPE = personal protective equipment.
2.1. Environmental system
More evidence is needed to understand the exact origins of COVID-19. But it is clear that, broadly speaking, its origins lie in human impacts on the environmental system driven by economic concerns. Activities like deforestation, human settlement, mining and building transport infrastructure have led to closer interaction between animal pathogens and human populations, facilitating the transfer of viruses between animals and humans, as was the case for COVID-19 (Andersen et al., Reference Andersen, Rambaut, Lipkin, Holmes and Garry2020; Cheval et al., Reference Cheval, Mihai Adamescu, Georgiadis, Herrnegger, Piticar and Legates2020; UNEP & ILRI, 2020). Evidence shows that 71.3% of new infectious diseases, like COVID-19, have transferred to humans from wildlife, with the number increasing significantly over time (Jones et al., Reference Jones, Patel, Levy, Storeygard, Balk, Gittleman and Daszak2008). Researchers have concluded that the risk of transmission of these pathogens is higher when animals have had to adapt to human-dominated landscapes in the context of loss of habitat and biodiversity (UNEP & ILRI, 2020). Intensive agricultural production has also led to higher levels of interaction between wildlife and livestock, again increasing the probability of transfer from animals to humans (Jones et al., Reference Jones, Grace, Kock, Alonso, Rushton, Said and Pfeiffer2013). Human trade of wildlife has become more common, bringing humans into ever closer contact with animals, again facilitating the spill-over of viruses to humans (UNEP & ILRI, 2020).
Human disruption of the environmental system also appears to play a role in the severity of the disease: researchers have hypothesized that pollution may worsen the effects of COVID-19 for individuals by impairing the ‘first line of defence of the upper airways’ (Cheval et al., Reference Cheval, Mihai Adamescu, Georgiadis, Herrnegger, Piticar and Legates2020; Mehmood, Reference Mehmood, Saifullah and Abrar2020). At the same time, the reduction of economic activity in response to the pandemic appears to have benefitted air quality in built-up areas (Cheval et al., Reference Cheval, Mihai Adamescu, Georgiadis, Herrnegger, Piticar and Legates2020). There are also some predictions that greenhouse gas emissions are lower as a result (Le Quéré et al., Reference Le Quéré, Jackson, Jones, Smith, Abernethy, Andrew and Friedlingstein2020). On the other hand, the increased use of non-recyclable materials in protective equipment in the health system may worsen water pollution (Cheval et al., Reference Cheval, Mihai Adamescu, Georgiadis, Herrnegger, Piticar and Legates2020). Environmental systems thus play a key role in the origins and severity of COVID-19 and are, in turn, impacted by the responses to contain it.
2.2. Health system
Once the coronavirus arose and started to spread, the primary burden for responding to it lay with the health system. The WHO's diagnosis was that effectively managing the disease requires health system capacities to be in place to ‘detect, test, isolate and treat every case and trace every contact’ (WHO, 2020e). Their guidance on treatment called on countries to develop effective emergency response systems, build capacity to detect the disease and care for patients, ensure hospitals have the necessary staff and supplies and deliver life-saving medical interventions (WHO, 2020d). As it was put by the WHO Director General, ‘[T]he best defence against any outbreak is a strong health system’ (WHO, 2020g).
Yet many countries faced major challenges in testing, tracing, providing critical care and accessing sufficient human resource capacity to do so (Chersich et al., Reference Chersich, Gray, Fairlie, Eichbaum, Mayhew, Allwood and Haghighi2020). There were widespread reports from around the world that health systems were, as one WHO spokesperson put it, ‘collapsing under the pressure of too many cases’ (CNBC, 2020). Despite evidence that protective equipment is effective at preventing transmission to the health workforce (Liu et al., Reference Liu, Cheng, Xu, Yang, Zhu, Zhang and Yao2020), supplies have been inadequate (WHO, 2020b), and many healthcare workers have died. There is also concern that other necessary health services are being compromised as a result of capacity being taken by the COVID-19 response (WHO, 2020a). By being key to the response, health system capacity thereby influenced the severity of the disease within and between countries (Walker et al., Reference Walker, Whittaker, Watson, Baguelin, Winskill, Hamlet and Thompson2020).
2.3. Political system
Primary responsibility for implementing the response to COVID-19 lay with the political system. With a clear imperative to react, politicians everywhere were affected. Underpinning decisions at the international, national and municipal levels around how to respond were concerns about the human cost, the burden on health systems and the economic, political and social trade-offs involved. Along with policy choices about health systems, the primary policy to alleviate the severity of COVID-19 was ‘social distancing’ (WHO, 2020c). Policymakers in at least 160 countries imposed ‘lockdowns’ to limit person-to-person transmission (Hale et al., Reference Hale, Angrist, Kira, Petherick, Phillips and Webster2020). While lockdown policies varied significantly in their type, stringency and timing, common measures included restrictions in meeting people outside of the household, limits on public gatherings, closing schools, physical distance measures and travel restrictions (Hale et al., Reference Hale, Angrist, Kira, Petherick, Phillips and Webster2020).
Political leadership appeared to be key to influencing the effectiveness of the response (Forman et al., Reference Forman, Atun, McKee and Mossialos2020). In some countries, such as Brazil, the UK and the USA, policy responses were widely criticized for being inadequate and blamed for high numbers of deaths. By contrast, the rapid and comprehensive political response in countries such as Denmark, New Zealand and Vietnam appears to have mitigated the severity (Hinchman et al., Reference Hinchman, Ali, Goodwin, Gillie, Boudreaux and Laborde2020; Potter, Reference Potter2020). While empirically measuring the relationships between the lockdown response and incidence rates is tricky (Hale et al., Reference Hale, Angrist, Kira, Petherick, Phillips and Webster2020), political choices about the degree of social distancing measures do appear to have influenced the severity of the virus (Thu et al., Reference Thu, Ngoc and Hai2020). Geopolitical interests also played out at an international scale as national governments and UN agencies jostled for political power and influence.
2.4. Social system
The lockdown measures implemented to reduce the spread of COVID-19 had major effects on social systems, since people were unable to interact as before. It was already well established prior to the pandemic that social isolation is a major risk factor for a range of poor health outcomes (e.g., Leigh-Hunt et al., Reference Leigh-Hunt, Bagguley, Bash, Turner, Turnbull, Valtorta and Caan2017). Demand for mental health helplines reportedly surged during lockdown (e.g., Smith & Lim, Reference Smith and Lim2020), and evidence showed that enforced quarantine led to anxiety, depression and post-traumatic stress (Brooks et al., Reference Brooks, Webster, Smith, Woodland, Wessely, Greenberg and Rubin2020). Experts voiced concern about a ‘second pandemic’ of mental health problems (Choi et al., Reference Choi, Heilemann, Fauer and Mead2020). There were also reports of increased levels of domestic abuse and child abuse (Bradbury-Jones & Isham, Reference Bradbury-Jones and Isham2020; Taub, Reference Taub2020).
Yet the social system also responded positively to COVID-19. There are numerous examples of self-organized community groups and community kitchens, of neighbours supporting vulnerable people, carrying out food shopping and collecting medical prescriptions and of people connecting via electronic platforms. Another aspect of the social system, however, influenced its severity: social attitudes influenced whether people actually adhered to social distancing rules (Pedersen & Favero, Reference Pedersen and Favero2020). Reports from the USA, for example, indicate that social attitudes towards science affected the degree of compliance with lockdowns (Brzezinski et al., Reference Brzezinski, Kecht, Van Dijcke and Wright2020). Social systems were thus profoundly affected by COVID-19, but also played a role in influencing its severity and the response to it.
2.5. Economic system
As described in Section 2.1, human economic activity played a major role in the origins of COVID-19; it was also one of the systems most severely impacted. By cutting consumption and reducing people's ability to work and produce, social distancing measures sent economic shockwaves throughout the global economy (World Bank, 2020; Gopinath, Reference Gopinath2020b). In the USA, total retail sales fell 8.7% in March 2020 (Warren, Reference Warren2020). With clothing seeing the greatest decline (50.5%), this had major repercussions for economies that supply these clothes, with millions of jobs reported to be lost in Bangladesh, Cambodia, China and Vietnam (Nortajuddin, Reference Nortajuddin2020). China's economy is reported to have declined by 6.8% in the first 3 months of 2020 – this is the country's first recorded contraction (Kuo, Reference Kuo2020).
With global GDP growth falling by 3.0% in April and 4.9% in June 2020, the International Monetary Fund (IMF) is predicting losses to the global economy of over US$12 trillion in 2020–2021 (Gopinath, Reference Gopinath2020a) and the worst economic depression since the 1930s (Gopinath, Reference Gopinath2020b). In response, they are recommending that ‘fiscal policy should urgently provide sizable support for affected people and firms during the pandemic’ (IMF, 2020b). Governments everywhere have put in place fiscal stimulus packages and monetary policies (Hale et al., Reference Hale, Angrist, Kira, Petherick, Phillips and Webster2020; IMF, 2020a). Global fiscal support of over US$10 trillion and easing of monetary policy is reported to have prevented the fallout from being even worse, especially in higher-income nations (Gopinath, Reference Gopinath2020a). The negative consequences of lockdowns on economic activity were also a major driving force behind political decisions about how and when to ‘reopen’ economies.
Economic downturns also impacted heavily at the household level through loss of jobs and income (e.g., Tran et al., Reference Tran, Hensing, Wingfield, Atkins, Annerstedt, Kazibwe and Lönnroth2020), exacerbating existing inequalities, given that the risks were greater for poorer households (e.g., Qian & Fan, Reference Qian and Fan2020). The policy response has been a range of measures to support families financially. As of 12 June 2020, 173 countries had enacted 621 such measures, including cash transfers and in-kind food and voucher schemes (Gentilini et al., Reference Gentilini, Almenfi, Dale, Lopz, Mujica, Quintana and Zafar2020).
2.6. Food system
At the very start of the pandemic, consumer stockpiling in many countries led to food shortages in shops. While the impact was short term, social distancing measures then had longer-term ripple effects across the system. By shutting down food service outlets, small stores and markets, thereby limiting the movement of the food workforce, restricting transportation and influencing consumer demand, lockdowns affected the ability to produce and sell food (FAO, 2020; Haddad et al., Reference Haddad, Fanzo and Hawkes2020; Swinnen & McDermott, Reference Swinnen and McDermott2020). At the same time, innovations such as e-commerce and local direct producer–consumer marketing initiatives sprang up to keep supply chains moving (Hawkes, Reference Hawkes, Swinnen and McDermott2020b).
The impact on the food system was intimately connected to the impact on the economic system, in part because the food system is an economic system. In addition, the economic impact of the pandemic on the ability of households to afford food compounded problems of production and supply, affecting food access. In this context, national and local governments, businesses and community groups put in place food vouchers and meal schemes for people negatively affected economically and for vulnerable and self-isolating groups (C40, 2020). Despite these efforts, international bodies have voiced major concerns that COVID-19's dual economic and food system impacts could prompt a widespread food crisis. The Food and Agriculture Organization (FAO) and World Food Programme (WFP) predict a food crisis in at least 27 countries ‘as the pandemic's knock-on effects aggravate pre-existing drivers of hunger’ (FAO & WFP, 2020). Research suggests that there could be a 14.3% increase in the prevalence of children under age 5 with inadequate weight compared to their height (Headey et al., Reference Headey, Heidkamp, Osendarp, Ruel, Scott, Black and Walker2020). It is also being reported that the refocusing of health systems on the pandemic, combined with budget shortfalls, has reduced the capacity to deliver basic undernutrition interventions (FAO & WFP, 2020).
While much of the focus has been on the impact on the food system, the food system also played a major role in the severity of COVID-19. Before the pandemic, unhealthy diets were estimated to be the second leading single cause of global ill health and premature mortality in the world (Gakidou et al., Reference Gakidou, Afshin, Abajobir, Abate, Abbafati, Abbas and Abu-Raddad2017). During the pandemic, it emerged that conditions directly associated with unhealthy diets – obesity and non-communicable diseases – raise the risk of complications of COVID-19. Evidence indicates that obesity, especially more severe obesity, is associated with increased death rate and/or treatment requiring invasive ventilation (Busetto et al., Reference Busetto, Bettini, Fabris, Serra, Dal Pra’, Maffei and Vettor2020; Goyal et al., Reference Goyal, Ringel, Rajan, Choi, Pinheiro, Li and Chen2020, Palaiodimos et al., Reference Palaiodimos, Kokkinidis, Li, Karamanis, Ognibene, Arora and Mantzoros2020; PHE, 2020; Popkin et al., Reference Popkin, Du, Green, Beck, Algaith, Herbst and Shekar2020; Tan et al., Reference Tan, He and MacGregor2020). Hypertension, diabetes and heart diseases – all of which are influenced by diets – have also been found to increase the risk of complications and hospitalization (Cummings et al., Reference Cummings, Baldwin, Abrams, Jacobson, Meyer, Balough and Hochman2020; Wiersinga et al., Reference Wiersinga, Rhodes, Cheng, Peacock and Prescott2020). The food system was not simply affected by COVID-19: it played a major role in its severity.
3. Implications for a global reset
The evidence in this Intelligence Briefing illustrates how the existence and severity of COVID-19 was a function of activity in multiple systems and the interconnections between them. By bringing together the evidence on the original causes, cross-system effects, severity and response to COVID-19, it becomes possible to see how the different systems combined to influence the burden of COVID-19 (Figure 1). Two systems – economic and environmental – had an interconnected role in the origins of the pandemic. The economic system was the ‘first cause’ through disrupting the environmental system. All of the systems influenced the severity of the disease – how many people contracted it, the extent to which there were complications and mortality – indicating that every system has a role to play in mitigating it. All of these systems also affected each other: responses implemented to address problems in one system inevitably led to effects on others. Lockdowns, for example, had negative spill-over effects on economic, social and food systems. Political leaders thus had to make choices about trade-offs between one negative effect over another – choices that influenced the severity of the disease. Historically, political choices have favoured short-term over longer-term goals, as reflected by the prioritization of economic goals over reducing the risk the transfer of pathogens from animals to humans. Similarly, choices about the food system have failed to prioritize diet-related health, also influencing the severity of COVID-19.
The role of multiple systems and the interconnections and contradictions between them over the short and long term provide important lessons on what is needed to effectively and sustainably manage global challenges more broadly. Five actions emerge as vital to enabling change (Table 1).
Table 1. Five vital steps for a global reset.
3.1. Step 1: train systems leaders
If people with responsibility for solving global challenges cannot think in a systemic way, they will not be able to understand nor apply solutions across multiple systems. Systems leadership skills are thus paramount in moving the reset forward (Nabarro, Reference Nabarro2020). Systems leadership is ‘a set of skills and capacities that any individual or organization can use to catalyse, enable and support the process of systems-level change’ (Dreier et al., Reference Dreier, Nabarro and Nelson2019, p. 4). It requires an ‘understanding of the complex systems shaping the challenge to be addressed’, an ability to ‘see and explain whole systems as well as their components’, and ‘to engage with systems from multiple perspectives at the same time’ (Atkinson & Nabarro, Reference Atkinson and Nabarro2019). This mind-set is necessary to enable working across system boundaries ‘with the explicit goal of creating change on complex, systemic issues’ (Dreier et al., Reference Dreier, Nabarro and Nelson2019, pp. 4, 7). Such an approach is not typical among decision-makers and managers. Rather, the focus of past decades has been on linear, competitive and often inward-looking leadership, with maximizing organisational performance as its main goal. Building systems thinking skills thus emerges as a crucial role for universities and leadership training programmes everywhere.
3.2. Step 2: employ a new cadre of systems connectors
Without the human capacity in organizations, businesses and governments to engage and connect with other systems, the ability to implement change will be severely limited. Building this function into existing jobs will not be sufficient owing to the evident complexity of the work. What is needed instead are a new cadre of professional ‘system connectors’ whose job it is to make connections across multiple systems at the middle management level. These ‘system connection managers’ can be thought of as the double-headed arrows in diagrams of complex systems. They would be charged with solving specific problems, not fixing systems per se. Food systems, for example, contain multiple problems (e.g., diet-related ill health, malnutrition, climate change, water, livelihoods, etc.), each of which needs a connector to work across subsystems to discuss and manage ways to align systems to solve the problem.
3.3. Step 3: identify solutions across systems
The first task of the systems connector is to identify what needs to change in each system to prevent, mitigate and treat the problem across all relevant systems/subsystems. Given the build-up of evidence in recent years, many of these solutions will already be known; the task is to bring them together and place them within a multi-systems context. This step is important for establishing the roles each system would ideally play in solving the problem. However, because acting in one system has effects on others, an ideal solution in one system may have negative knock-on effects in another, as shown very clearly in the case of COVID-19. The next step is thus to identify and manage trade-offs.
3.4. Step 4: manage trade-offs
Managing trade-offs involves making hard choices about the relative costs and benefit of one impact over another. The huge challenge for reset will be how to take the longer-term view for sustainability and human well-being when there are so many short-term political and economic interests at play. In the case of COVID-19, fiscal stimulus packages have mitigated some of the negative economic consequences. Yet their goal has tended to be to re-stimulate demand (i.e., to get people consuming again). While this will have short-term benefits, over the long term it places further pressures on the environmental system.
Managing trade-offs also extends beyond making tough decisions about costs and benefits to recognizing and managing a minefield of vested interests, power relations, contradictions and conflicts between different systems. For example, government regulation in the food system of the marketing of foods associated with obesity makes sense as an action to increase resilience to COVID-19 over the longer term. Yet this threatens the economic system in terms of food businesses attempting to recover in the shorter term. The dilemma here is that the trade-off involves other systems managed by a different set of people and interests (thus the need for systems connectors). New ways of acting will be needed to engage intensively in order to find win–win situations where possible, identifying what incentive structures are needed and negotiating compromises where necessary using system leadership skills.
Still, there will be cases where trade-offs are intractable. For instance, the current economic system is inherently reliant on consumers consuming more than is sustainable for the environment, health and society. As it has been put by the Global Sustainability Report 2019, ‘[C]reating economic growth just by increasing consumption of material goods is no longer a viable option at the global level’ (UN DESA, 2019). Here, there can be no ultimate win–wins over the long term; there is an inherent and intractable conflict, an indicator that the design of the economic system is fundamentally flawed and cannot be managed by trade-offs alone. Rather, the system needs to be redesigned so that it inherently produces co-benefits for other systems.
3.5. Step 5: kick-start systems redesign for co-benefits
The lack of feasibility in managing trade-offs is an indicator that, for sustainable, longer-term solutions, systems need to be redesigned to achieve different goals in synergy with one another (Parsons & Hawkes, Reference Parsons and Hawkes2018). Policymakers, businesses and organizations need to ‘proactively act to identify potential co-benefits during the [policy] design stage and shape implementation criteria to maximise impact’ (Hepburn, Reference Hepburn, O'Callaghan, Stern, Stiglitz and Zenghelis2020). Crucial in this regard is identifying opportunity spaces that can be leveraged in the short term to force the hand of a systems redesign in the longer term. One example to kick-start the process now would be imposing conditionalities on businesses in return for COVID-19 financial support packages. For example, in the USA, politicians proposed that the economic rescue package require airline companies to cut emissions by 2050 to 50% below 2005 levels (a goal to which the industry is already committed) (Tollefson, Reference Tollefson2020). It was not adopted by US Congress, showing the limitations imposed by a lack of political leadership. Nevertheless, there are many opportunity spaces; a key role of systems leaders and connectors is to identify them and to act within their own powers, recognizing that part of systems leadership is recognizing ‘it's up to us’ and ‘I can make a difference’ (Dreier et al., Reference Dreier, Nabarro and Nelson2019).
***
The lessons drawn from the evidence on the role of multiple systems in COVID-19 are not necessarily new. The importance of addressing root causes and social determinants of health has been part of the dialogue for decades (CSDH, 2008). Much of the sustainability conversation has been about the need to give greater priority to longer-term goals. Indeed, this was the core of the Sustainable Development Goals (UN, 2015). The call for systems leadership and managing trade-offs likewise preceded COVID-19 (Dreier et al., Reference Dreier, Nabarro and Nelson2019; IGS, 2019).
But the context is new. So if businesses, organizations, governments and international agencies are really serious about a global reset, now is the time to put these five steps to work, regardless of who else is doing so. The steps essentially provide a mechanism to hold them accountable: if they are not taking them, they are not doing enough. Nevertheless, with the short-term imperative to recover, this will be extraordinarily challenging. Given how hard it will be, those who are already taking such steps should share their experiences to enable others to learn from them, so advancing the collective courage needed to press the global reset button.
Acknowledgements
With thanks to Gavin Wren for designing Figure 1. Thank you also to David Nabarro for inspiring some of the thinking in this paper and to him and The George Institute for Global Health for publishing the idea behind this paper in the blog: Our life support system: COVID-19 shows multiple systems are vital for global health.
Author contributions
Corinna Hawkes was solely responsible for conducting the research and writing the paper.
Conflict of interest
None.
Financial support
None.