In July 2016, a contained measles outbreak occurred in a London prison with more than 1500 inmates, of which two-thirds were sentenced and one-third constituted new influx. This was the second case of a reported measles outbreak in a custodial setting in England. The previous outbreak occurred in a Yorkshire prison in 2013 [Reference Crick1]. In both outbreaks, the source of infection originated from a member of staff and there was low known immunity of prisoners as well as staff at the time. However, in terms of characteristics, there were striking differences between the two prison settings: The prison in London housed about seven times as many inmates as the Yorkshire prison and their makeup was significantly different. Average custodial stay in this London male prison was around 6 weeks at the time of the outbreak. The majority of prisoners were between 18 and 39, two-thirds were Caucasian, with men from Black Caribbean origin the second largest group at just under 10%. Nearly half of the prisoners were foreign nationals, while in the Yorkshire prison outbreak 91% of inmates were of White British origin. Data on country of origin available to us was not consistent as it came from collected ethnicity data. We do, however, know that ‘Other White’ made up the largest group of inmates at around 70% of those who were foreign nationals. Almost a quarter had diagnosed mental ill health in the London prison.
In July 2016, Public Health England (PHE) confirmed two cases of measles amongst prison staff and declared it an outbreak. Transfers in and out of prisons were stopped and immunity of prisoners was assessed to be unknown for about 50% of the prison population. The risk was deemed to be confined to the segregation unit (n = 30), where the two staff members with measles worked. However, by day 6 of the outbreak, a further two cases (one probable, one possible) amongst staff had been identified and four possible cases amongst prisoners. At this point, a mass vaccination programme was decided and a National Health Service England (NHSE) IMMS01 response was employed. IMMS01 is the name of the commissioning response to outbreaks of vaccination preventable diseases in London only [2]. There is a rota of the NHSE (London) immunisation commissioners, which changes weekly with first and second on-call personal. The first on call commissioner is responsible for organising the acquirement of vaccine stocks and evoking a service provider response. This is done following an agreed protocol between PHE (London) and NHSE (London). A total of 1600 vaccines (Measles Mumps Rubella (MMR)) were ordered with the intention to vaccinate on Friday, and a check of pregnancy status in female vaccinees amongst prison staff was made (day 8). Vaccine supply was delayed coming from the manufacturer and no protocol currently exists with other institutions such as PHE to release some of their stock in the meantime in the case of a supply shortage. The prison healthcare service had a high vacancy rate amongst staff and there was a shortage of prison officers to accompany prisoners to vaccination. Due to the weekend and annual leave, it was difficult to organise vaccinators from the contracted NHS immunisation task force provider to proceed with vaccinations on day 8 as planned. Logistics of getting security clearance to enable community healthcare staff to enter the prison and lack officers to escort staff/prisoners within the establishment, alongside the lack of suitable infrastructure, conspired to make delivering mass vaccination difficult. Between days 8 and 14 a total of 4 nurses (who were sourced across the local community healthcare system) vaccinated 241 prisoners out of a possible 800 with unknown immunity status (30%). This contrasts with the Yorkshire prison, where over 90% of inmates were vaccinated. No further cases occurred. There was a high refusal rate among prisoners.
We conducted an evaluation of the service response to the outbreak with the purpose to share learning and to develop a protocol for future reactive responses to prison outbreaks of vaccine preventable diseases. All healthcare service participants were interviewed as part of a root-cause analysis using standard tools [3] including the nurses who delivered the vaccinations, NHSE (London) commissioners of health and justice system, the head of the prison healthcare service, heads of service at the contracted NHS immunisation task force provider, the commissioners of the National Offender Management Service (NOMS), the on-call IMMS01 commissioners and the PHE health protection team. A thematic analysis was conducted to elicit the key points of learning. These are illustrated in detail in Figure 1. There were a number of issues which delayed or prevented mass vaccination, only some of which can be easily pre-empted for future outbreaks. For example, ensuring adequate training for potential vaccination staff or creating sharing protocols to enable a swift sourcing of vaccinations in case of shortage could have helped in recruiting vaccinators and securing vaccines more quickly. However, even with adequate number of vaccinators and timely vaccine supplies it was clear that any future reactive mass vaccination response would be hindered by ongoing staff shortages in the prison workforce (health and non-health) and the design of the physical environment which was not conducive to vaccination provision (i.e. prisoners needed to be accompanied to a room for vaccination where adequate cold chain and sharps disposals could be maintained. Rooms and staff were not readily available to enable this). A further obstacle was the high refusal rate amongst prisoners, something which may be addressed with education campaigns but is less likely to be sustainable due to the rapid turnover of the prison population. The rapid turnover will also make proactive vaccination programmes suggested by the World Health Organisation Health in Prisons Programme (WHO HIPP) [Reference Engginst4] difficult and their cost effectiveness is unknown. A short programme of for example the measles vaccine offered over a period of weeks to prisoners may be less effective when there is high prison population churn. In addition, the challenges facing London prisons [5] may prohibit such pro-active vaccination initiatives at present.
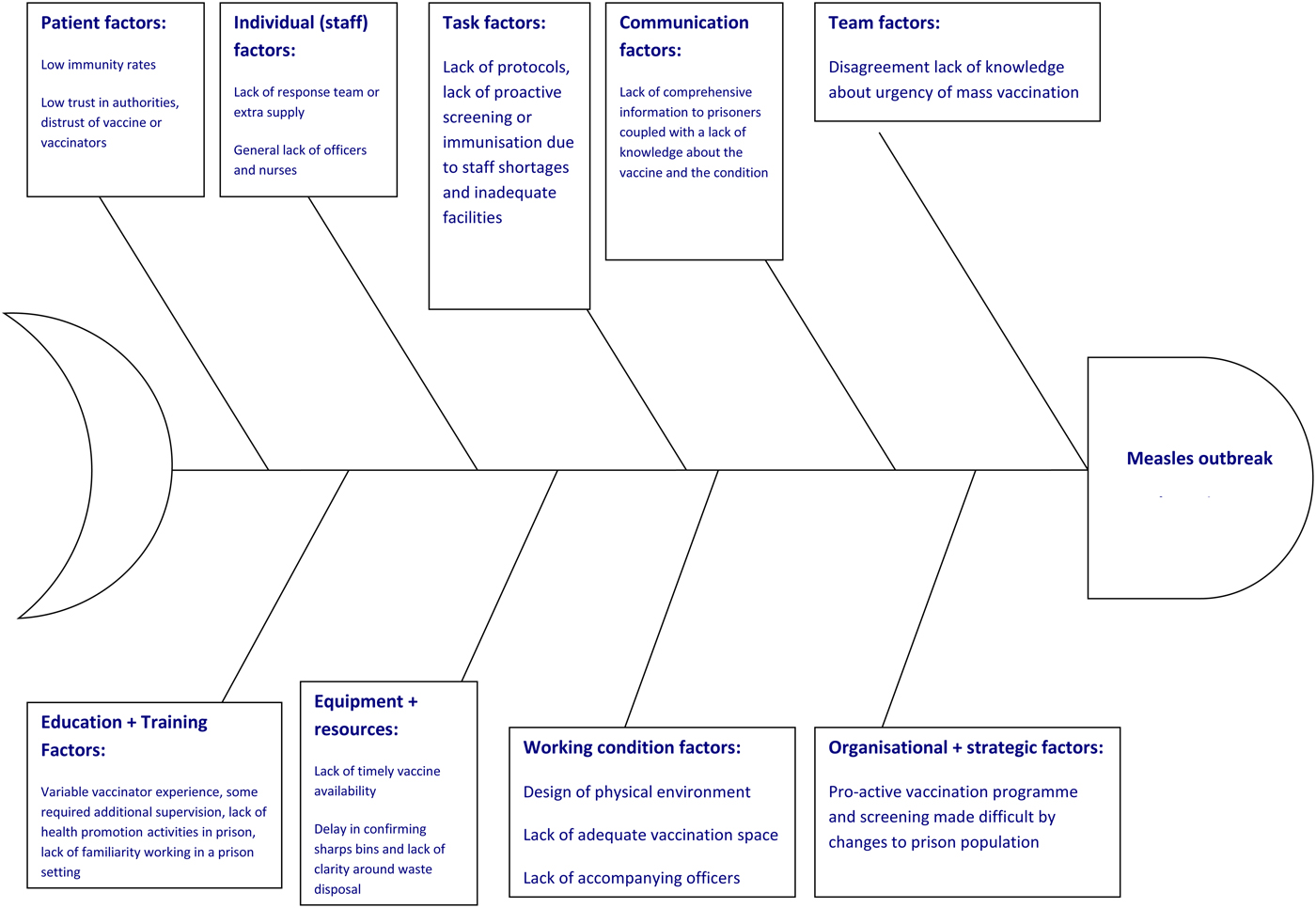
Fig. 1. Fishbone diagram of factors contributing to the delay in delivery and low uptake of mass vaccination.
Crick et al. [Reference Crick1] in their analysis of the outbreak in Yorkshire concluded that the outbreak would have been unlikely to have been stalled by mass vaccination of prisoners. It was recommended to have comprehensive documentation of the immune status of staff and prisoners. We concur with the authors and go further in our recommendations. We found that mass vaccination was difficult to implement. In the Yorkshire prison, the majority of prisoners born after 1987 had a vaccination status reported in a retrospective data gathering exercise. However, 91% of inmates were White British, while the population of inmates in London was to a large extend made up of foreign nationals where vaccination cannot assume to be as consistent as in the UK. In addition, the majority of inmates in Yorkshire were vaccinated following the outbreak, while in London only a minority consented to vaccination. Language barriers, differing understanding or knowledge, lower immunisation rates in countries of origin as well as the high number of prisoners with mental health problems may have contributed to this.
Going forward, we suggest that since the measles outbreak in the London and Yorkshire prisons originated with prison staff, it is first important to ensure that all staff are vaccinated with MMR and have their annual influenza vaccine. Vaccination provision by Her Majesty's Prison and Probation Service (HMPPS) occupational health service would help avoid potential future outbreaks being brought into prisons. Whilst not uncontroversial, one could argue that the proven immunisation status of prison staff should be part of the occupational health assessment at employment similar to health workers. Had infected staff been exposed to the entire prison as in Yorkshire and not predominantly the segregation unit, a mass outbreak may well have occurred. All adults born from 1970 onwards are entitled to the two doses of MMR for free on the NHS and this can be obtained through general practice. Influenza vaccine can also be received from participating pharmacies.
Second, we would also argue that the only way to avoid mass outbreaks, in the long run, is to ensure recording of vaccination status and offer of a vaccine along with education during the admissions process for prisoners. There should be a reliable secondary assessment in prison settings to establish immunity and utilising the initial health assessment at reception or comprehensive second assessment following a first reception for identification and/or provision of opportunistic vaccinations. An opt-out approach to testing was shown to be highly effective and could be adopted to test for measles immunity [6].
Finally, one could also conclude that instead of testing for immunity first in the event of an outbreak, a proactive vaccine could be given, saving time and resources. Whilst the London Region advocates for opportunistic vaccines during outbreaks, particularly in schools, this is not part of the Health Protection Team (HPT) plan at present, which tends towards treating the outbreak disease. It might be worth reviewing the opportunistic approach in the light of this outbreak.
In summary, this was the second outbreak of measles in a custodial setting and both times the outbreak started with a member of staff. Our root-cause analysis revealed that many of the factors identified are those that cannot be easily changed, including challenges facing prisons such as inadequate infrastructure, staff shortages and a high turnover of inmates. A low immunisation rate and low uptake during mass vaccination are also factors that do not lend themselves to rapid correction. It is unlikely that mass vaccination at the time, even in the absence of some of the more easily rectifiable issues such as staff training, vaccinator availability and vaccine supply, could have fully avoided further cases in the event of a mass outbreak. A three pronged approach of ensuring full immunisation of prison staff, detailed recording, opt-out testing and/or empirical vaccination of prisoners as well as the offer of the opportunistic vaccine in the event of an outbreak may help prevent a mass outbreak in the future.
Acknowledgements
The authors thank the health and non-health staff of the affected prison, the vaccinators and other stakeholders for their valuable insights and time.
Declaration of interest
None.




