Introduction
In December 2019, a novel betacoronavirus, SARS-CoV-2, was isolated from hospitalised patients in Wuhan, China who were suffering from pneumonia with an unknown aetiology [Reference Zhu1]. As of 9 July 2020, there have been more than 11.6 million cases of COVID-19 (Coronavirus disease 2019), the disease caused by SARS-CoV-2, reported worldwide [2].
On 10 March 2020, the first case of COVID-19 was reported in the district of Tirschenreuth (TIR; 72 000 inhabitants). Within 1 week, the number of cases had increased dramatically. On 18 March 2020, the local administration ordered a lockdown of Mitterteich, the most affected town in the district. In the following weeks, a high crude case fatality ratio (CFR) was observed in the district (TIR: 11%; Germany: 4.3%).
The potential role of local beer festivals as super-spreading events gained wide public attention. The local government of the TIR district and the State of Bavaria invited the Robert Koch Institute (RKI) for a joint investigation. Together with state and local health departments, we aimed to identify exposures potentially responsible for the transmission during the outbreak and the underlying reasons for the high CFR.
Methods
In order to investigate reasons for the rapid increase of cases and the magnitude of the outbreak, we used national and local surveillance data on laboratory-confirmed, reported COVID-19 cases in TIR from 17 February to 11 May 2020. We used the standard case definition of the RKI to classify casesFootnote 1. In our study, all persons with SARS-CoV-2 infection confirmed by RT-PCR were included. We used epidemic curves to analyse cases over time. To this end, we used the date of onset of symptoms, or date of reporting where the onset of symptoms was not available. We calculated the 7-day reproduction number R from notification data by using a moving 7-day average [Reference an der Heiden and Hamouda3]. In order to detect events and exposures that may have led to the outbreak, we looked at the first 110 cases in TIR (by date of onset of symptoms) in more detail. These cases reported symptoms of COVID-19 before the second, large peak of cases occurred in the course of the outbreak. We gathered additional information on potential exposures of these cases (attendance at large public events, previous contact to known COVID-19 cases, travel history, especially skiing holidays in areas with high risk for acquiring COVID-19) in the period 17 February to 8 March 2020. To this end, we used available data from the local health department and conducted semi-standardised telephone interviews. The semi-standardised questionnaire was created by the authors in collaboration with the employees of the local health authority in Tirschenreuth. Local staff conducted the phone interview and data were collected in an Excel spreadsheet. Multiple answers per question were possible. In the course of the outbreak investigation, unfortunately there was not sufficient time to test the questionnaire in advance. The questionnaire used for the telephone interviews is provided in the Supplementary material of this study (S1).
To evaluate the measures taken in the course of the outbreak, we analysed cases in the whole TIR district and those living in the town of Mitterteich. We calculated the date of infection with SARS-CoV-2 by using the date of symptom onset minus the mean incubation period of 5 days [Reference Linton4]. We smoothed the generated curve of infections/day calculating the 3-day moving average. We used the day with the highest number of cases as the reference (100%).
In order to investigate the high crude CFR in TIR, we used surveillance data to compare the distribution of factors associated with infection between TIR and the rest of Germany. The factors included age, underlying medical conditions (cardiovascular diseases, chronic lung diseases, chronic liver diseases, diabetes, cancer and immunosuppression [5]) and the proportion of vulnerable persons (cases living in care facilities). We used German surveillance data to categorise cases as living in a community facility according to §36 of the German Infection Protection Act. To provide information on outbreaks in elderly care homes, we examined data documented at the local health authority. To determine if the crude CFR was distorted by the underlying age structure of the district, we calculated an age-standardised CFR. We used strata in 10-year-steps. To compare the age of different groups of cases, we used the Wilcoxon rank-sum test. All statistical analyses were performed in Stata SE 15.1. P-values <0.05 were considered statistically significant.
We contacted local laboratories to estimate the number of SARS-CoV-2 tests performed in the period of 7 March 2020 (first laboratory confirmation in TIR) and 13 May 2020 and compared the data with those reported for Germany [6].
Results
Between 10 March and 11 May 2020, 1122 COVID-19 cases were notified to the local health authorities, 129 (11%) of whom had died by the time of this analysis (11 May 2020; Table 1).
Table 1. Demographics and case fatality ratio (CFR) of COVID-19 cases in TIR and in the rest of Germany (until 11 May 2020)
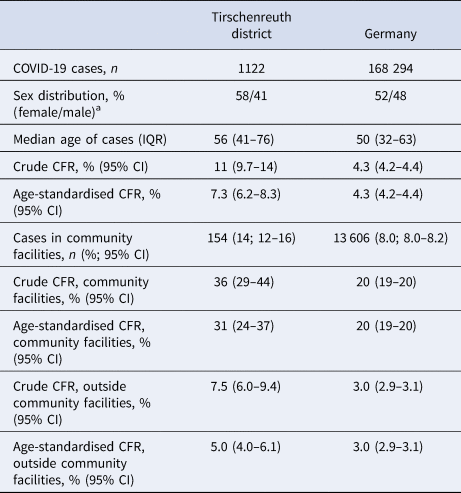
IQR, interquartile range, 95% CI, 95% confidence interval.
a Sex was not reported for one case in TIR.
The epidemic curve is shown in Figure 1. The first laboratory-confirmed case in the region was notified to the local health authorities on 10 March 2020 with disease onset on 8 March 2020. Investigations and interviews with cases revealed that there were sporadic cases with disease onset in February and early March, the first peak with 28 cases occurred on 10 March 2020. A second and even higher peak was observed on 16 March 2020 with 55 cases. The number of cases started to continuously decline at the end of March. At the beginning of May, only sporadic cases were notified. The 7-day reproduction number R declined steadily from 2.7 on 24 March to below 1.0 on 5 April. Overall, 80% of cases were symptomatic, especially in the earlier weeks of the outbreak, while in the later stages the proportion of asymptomatic cases increased.
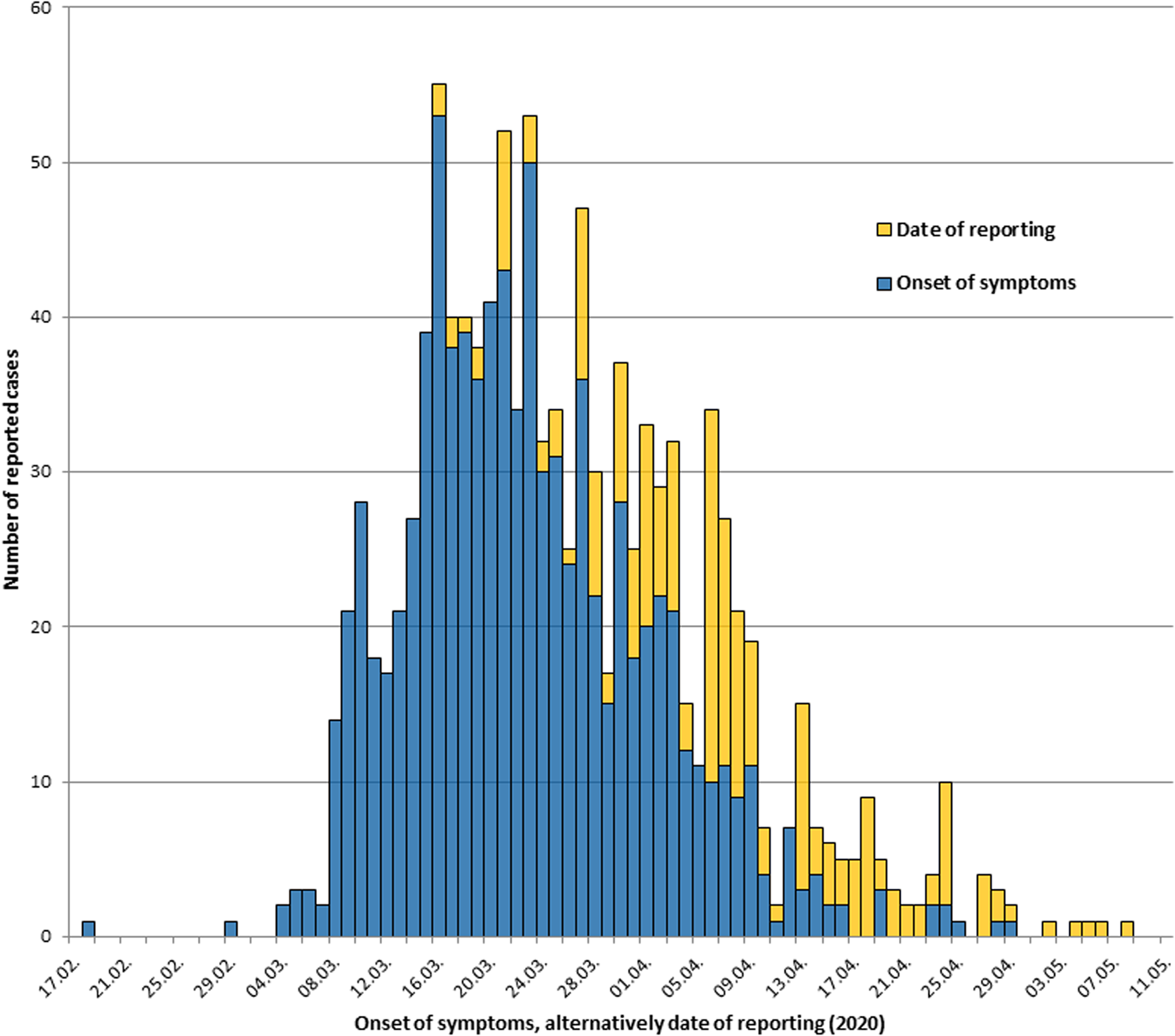
Fig. 1. COVID-19 cases in Tirschenreuth district, Germany, until 11 May 2020, by date of onset of symptoms, alternatively by date of reporting (n=1122).
Due to the magnitude of the outbreak and limited resources during March 2020, mainly close contacts of known COVID-19 cases with acute symptoms were tested for SARS-CoV-2. By 13 May 2020, the total number of laboratory tests in TIR (8422 tests/100 000 inhabitants) had exceeded those performed in all of Germany (3787 tests/100 000) by a factor of 2.2. Nevertheless, 17% of all tests in TIR were positive for SARS-CoV-2, while only 6.3% of all tests were positive in Germany as a whole.
In order to identify early drivers of transmission, we analysed the first 110 cases with the onset of symptoms between 18 February and 12 March 2020. The most frequently reported exposures included having been guests at the small local beer tradition between 3 March and 7 March 2020 (13%), skiing vacation in Austria or Italy in February/March (11%), and the big, 1-day beer event in Mitterteich (9%) (Fig. 2). Both traditional beer festivities attract large numbers of local and regional visitors. Three cases had been skiing and guests at the smaller beer festival; one had been skiing and went to the big 1-day beer event. Twenty-seven (25%) cases reported other possible exposures with large numbers such as attending birthday parties, funerals or religious services. For 38 (35%) cases, no known exposure could be determined.
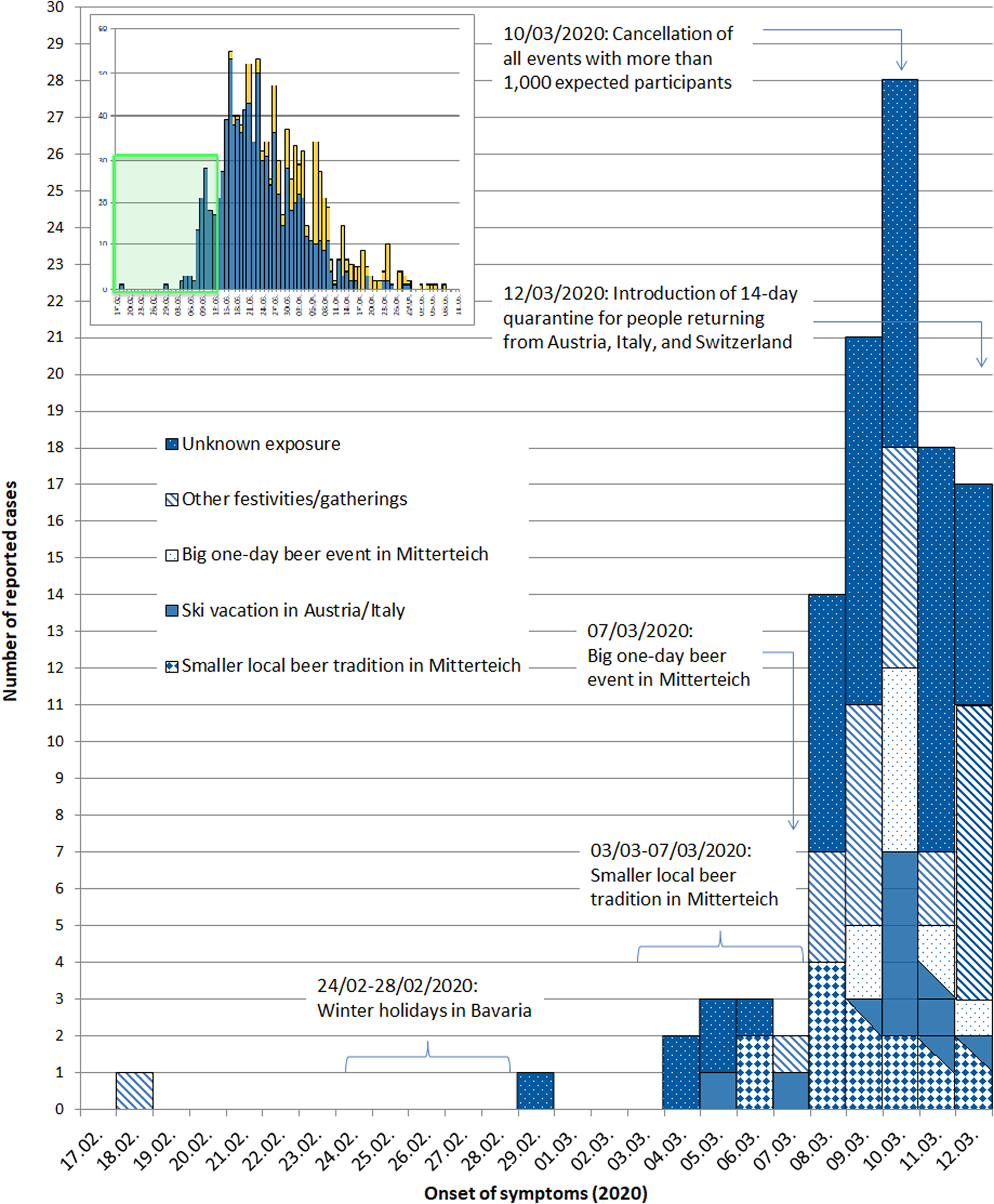
Fig. 2. Possible exposures of the first 110 cases and dates of events and implemented measures in Tirschenreuth district, Germany, 2020. Shown is a section (17 February–12 March 2020) of the epidemiological curve.
We looked at public health measures taken in TIR, the Bavarian state and Germany and analysed the impact of those measures on the course of the outbreak. A series of measures were implemented between 10 March and 18 March (Fig. 3, highlighted area). On the national level, events with more than 1000 participants were banned on 10 March 2020. In TIR, an extensive information campaign was initiated, including the establishment of a ‘Corona hotline’ on 13 March 2020. Kindergartens and schools were closed starting from 11 March 2020 in Mitterteich, the most affected town in the district. The state of Bavaria announced the intention to declare a state of emergency on 15 March 2020. During this period, when looking at the date of symptom onset, case numbers in TIR were still increasing, however appeared to reach a plateau (TIR) or even decreased (Mitterteich) when looking at the date of infection (Fig. 3). On 18 March, a complete lockdown was implemented in Mitterteich, followed by a partial lockdown for the entire state of Bavaria on 21 March 2020. When looking at the date of symptom onset, the numbers of cases started to decrease on 22 March, and had already begun to decrease shortly before the lockdown of Mitterteich.
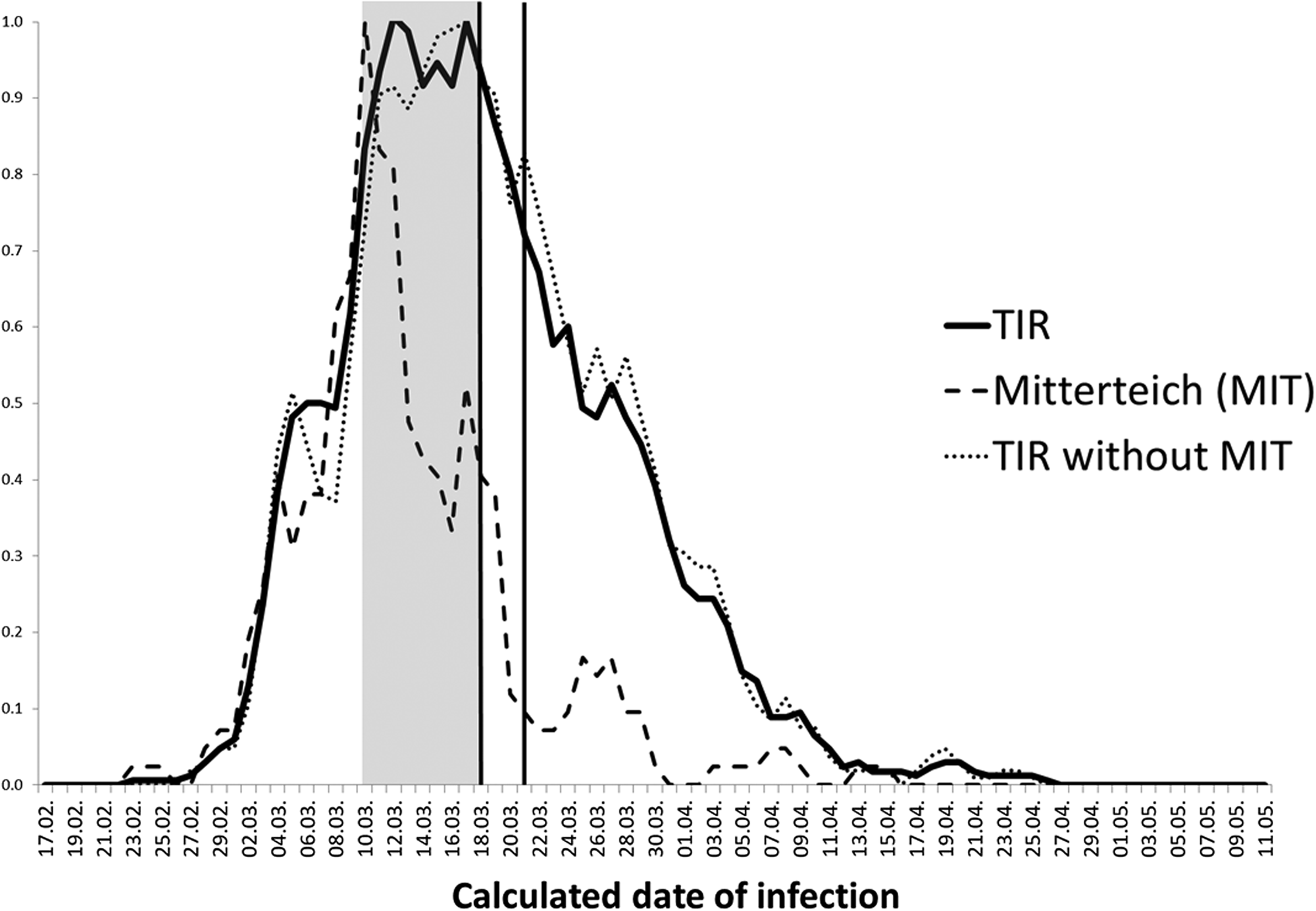
Fig. 3. Symptomatic cases in TIR (n = 895, continuous black curve), Mitterteich only (n = 147, dotted grey curve) or TIR without Mitterteich (n = 748, dotted black curve) by calculated date of infection. Shown are a series of early measures on local, regional and national levels (grey highlighted area), time point of lockdown in Mitterteich (first black line, 18 March) and the time point of the partial lockdown in Bavaria (second black line, 21 March).
We compared age, sex and predisposing chronic diseases of cases in TIR with cases from the rest of Germany (Table 1). Among cases in TIR, 58% were female compared to 52% in the rest of Germany. Cases in TIR were significantly older with a median age of 56 years (interquartile range (IQR): 41–56) compared to 50 years (IQR: 32–63) in the rest of Germany. However, there was no age difference among deceased cases, with a median of 83 years (IQR: 77–88) in TIR vs. 82 years (IQR: 76–88) in the rest of Germany. The crude CFR for TIR was 11% (95% CI 9.7–14) compared to 4.3% (95% CI 4.2–4.4) in the rest of Germany, while the age-standardised CFR was 7.3% (95% CI 6.2–8.3) in TIR and 4.3% (95% CI 4.2–4.4) in Germany (Table 1).
The higher median age and the high percentage of cases with underlying medical conditions were in agreement with the high number of cases in TIR living in retirement homes. In the rest of Germany, 8.0% of all cases were reported to live in a community facility, compared to 14% of all cases in TIR (Table 1). Of note, community facilities also include other institutions such as prisons, asylum centres or homes for disabled persons. In TIR however, 145/154 cases living in community facilities were residents of elderly care homes. Looking only at cases reported in community facilities, the CFR in the district of TIR was 36% (95% CI 29–44) (age-standardised: 31%; 95% CI 24–37) and 20% (age-standardised: 20%; for both 95% CI 19–20) in the rest of Germany. On the other hand, looking only at cases outside of community facilities, cases were still significantly older in TIR (median age: 54 years, IQR: 38–69; Germany: 49 years, IQR: 32–60) and crude and age-standardised CFR were still elevated (TIR: crude: 7.5% (95% CI 6.0–9.4), standardised: 5.0% (95% CI 4.0–6.1)) compared to the rest of Germany (crude and standardised: 3.0% (95% CI 2.9–3.1)) (Table 1).
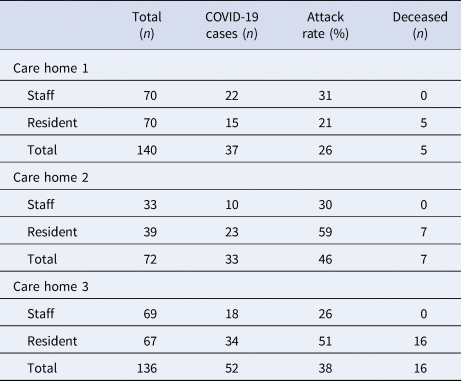
Three elderly care homes in the district were affected early in the COVID-19 outbreak, with attack rates of 21–59% among residents, and 29–31% among staff (Table 2). Care home 1 was the first affected facility, with the first cases among personnel. A member of staff tested positive for SARS-CoV-2 on 16 March 2020 but had been symptomatic from 8 March 2020. Since the symptoms were only mild, the case worked in the facility until the date of the test. Symptom onset for the first resident was on 16 March 2020. After the outbreaks in the three described elderly care homes, enhanced protective measures and a general screening strategy were applied for all 15 community homes in the district (14 elderly care homes and one home for the disabled) from 9 April onwards.
Table 2. Residents, staff, cases and deceased cases in three elderly care facilities in the Tirschenreuth district affected by COVID-19 outbreaks (until 11 May 2020)
Discussion
This report describes one of the first, severe community outbreaks of COVID-19 in Germany and in the history of the pandemic in Europe. SARS-CoV-2 may have been introduced to TIR from high-risk areas in Austria and Italy, the latter being severely affected by the epidemic starting February/March 2020 [7]. From 25 February 2020 onwards, the RKI declared several regions in northern Italy and Austria as COVID-19 risk areas, including popular ski regions mentioned as exposure sites of German cases [8, 9]. Several outbreaks in Germany and Europe have been linked to exposure during skiing holidays in Austria or Italy [Reference Gudbjartsson10, Reference Frank11]. At the time, measures such as cancelling of social events, wearing protective masks or reduced contact in the community in general were not yet established in Germany and the virus was able to spread rapidly in the community.
Mass-gathering events such as the carnival in Germany in February enhanced the spread of SARS-CoV-2 in communities [12]. In TIR, possible accelerators of the pandemic might have been the local beer festivals at the beginning of March. However, the steep increase observed in the epidemiological curve is likely due to a variety of factors rather than by mass gatherings alone. It can be speculated that unnoticed transmission occurred at the end of February in TIR. Böhmer et al. and others showed that cases may be infectious even before symptom onset and the virus can be transmitted by cases with only mild symptoms, leading to unrecognised transmission [Reference Böhmer13]. Our data show that the first case reported the onset of symptoms on 18 February 2020. Retrospectively however, it is not clear if these early symptoms were due to COVID-19 as the case was only tested in March after a second episode of respiratory symptoms.
We used a calculated date of infection, assuming a mean incubation period of 5 days to evaluate public health measures implemented in TIR, Bavaria and Germany, respectively. Our data suggest that the extensive information campaigns at the local level, particularly in Mitterteich, were valuable to avoid a further increase of cases in the whole district of TIR. The lockdown of Mitterteich and the partial lockdown in the Bavarian state probably contributed to dropping case numbers and the combined measures most likely allowed control of the outbreak by mid-April. We calculated the reproduction number R from dates of reporting due to the completeness of these data. However, considering the delay of disease onset and reporting as well as our analysis of symptomatic cases, measures were most likely effective earlier.
Our data showed that cases in TIR were older than in the rest of Germany, but age alone cannot explain the higher CFR. No analysis of underlying medical conditions was possible in our study. However, a report of the WIdO scientific institute stated that 31% of the general population in TIR suffers from at least one underlying medical condition aggravating the course of COVID-19, while this is the case for 26% of the general German population [Reference Schröder14]. The combination of vulnerable populations hit by the pandemic and applied testing strategies, primarily focusing on acute cases and thus missing asymptomatic and mildly symptomatic transmitters, has been shown to lead to high CFR in other regions [Reference Onder, Rezza and Brusaferro15]. Starting from the first reported cases in TIR, testing of all close contacts of cases regardless of symptoms was performed in accordance with the testing strategy of the Bavarian state (valid until 19 March 2020). However, due to the large number of cases and limited resources, primarily acute cases were tested at the height of the TIR outbreak as suggested by national and international guidelines [16, 17].
Even though individual measures such as usage of antiviral disinfectant in elderly care homes had already been implemented at the end of February; these did not prove to be enough to prevent initial transmission into and within these facilities. Extensive measures in elderly care homes, including a complete ban on visitors from mid-March, extensive use of personal protective equipment, a thorough screening strategy and isolation of positive cases were likely effective strategies to prevent transmission in further care homes in TIR.
In conclusion, the combination of exposures in high incidence areas and undiagnosed infections followed by intense transmission may have led to accelerated community transmission in TIR. Subsequent spreading of SARS-CoV-2 to vulnerable populations, including people in care homes for elderly, resulted in a high CFR. We could show that local and regional public health capacities are essential for the response. Measures at the local level allowed a timely response and were particularly helpful to control the outbreak.
We recommend strengthening of local public health capacities in Germany, as these were crucial in implementing targeted measures in a timely manner. Immediate support of local public health authorities from the regional and national level should be guaranteed in cases of emergency. Public health measures implemented in the course of the COVID-19 epidemic should be evaluated thoroughly to allow a targeted and effective response in similar situations in the future.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0950268820002460.
Acknowledgements
We would like to thank all employees of the local health district in Tirschenreuth involved in interviewing cases and in contributing to data collection. We thank Simon Packer (Public Health England), Jan Walter (RKI), Christina Frank (RKI) and Viviane Bremer (RKI) for their helpful comments.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
None.
Data availability
Aggregated data from a limited version of the German notification system database can be retrieved via SurvStat@RKI 2.0 https://survstat.rki.de/. Detailed data are confidential and protected by German law and are available from the corresponding author upon reasonable request.