Vitamin D has a wide range of physiological roles (e.g. anti-inflammatory and immune modulating effects) in our body(Reference Holick1,Reference Nair and Maseeh2) . During pregnancy, the mother needs more vitamin D than usual for the fetal development(Reference Pilz, Zittermann and Obeid3). It has been reported previously that vitamin D supplementation during pregnancy can be positively associated to improved fetal growth and better nutritional status of the newborn(Reference Gallo, McDermid and Al-Nimr4). On the contrary, vitamin D deficiency during pregnancy can result in several adverse outcomes including hyperparathyroidism and osteomalacia in mothers that may lead to neonatal hypocalcaemia(Reference Pilz, Zittermann and Obeid3,Reference Leere and Vestergaard5) . Moreover, vitamin D deficiency is also associated to preeclampsia, gestational diabetes, bacterial vaginosis, HIV transmission from mother to child and respiratory infection, etc(Reference Pilz, Zittermann and Obeid3–Reference Holick7). Furthermore, such a deficiency also plays a role in developing several kinds of polygenic and infectious diseases such as colon and breast cancer, CVD, type-1 diabetes, multiple sclerosis, rheumatoid arthritis and tuberculosis(Reference Holick1,Reference Nair and Maseeh2,Reference Huang, Wang and Liu8) . Consequently, a mother can be affected later in life with these diseases if she has vitamin D deficiency during or after pregnancy.
Vitamin D deficiency during pregnancy is prevalent worldwide(Reference Palacios and Gonzalez9). Such deficiency can have a wide range; 15 to 90 % has been reported among pregnant women in countries like Australia, Kuwait, Iran, Germany, UK, USA, China, Turkey, India and Pakistan(Reference Palacios and Gonzalez9). While such deficiency is common among pregnant women in both developed and developing countries, wide inter-country variation can be observed. For instance, a high prevalence of vitamin D deficiency has been reported for the pregnant women in the Middle Eastern countries like Iran and Kuwait (from 67 to 83 %). However, lower levels of deficiency are commonly reported in the Western countries like the USA and the UK prevalence usually ranges from 33 to 35 %(Reference Molla, Al Badawi and Hammoud10–Reference Maghbooli, Hossein-Nezhad and Shafaei13).
To explain this large variance in the status of vitamin D, a variety of factors have been highlighted in the literature as the potential underlying variables(Reference Holick1,Reference Nair and Maseeh2,Reference Mostafa and Hegazy14) . Among such factors, geographical location is one of the most important as it has direct implications with the intensity and duration of direct sunlight exposure for the mass population(Reference Yeum, Song and Joo15). Along with sunlight exposure, skin colour, attitude towards sunlight exposure, age, clothing practice, comorbidity, etc. are also commonly reported as the modulating factors to explain population-level variations of serum vitamin D(Reference Holick1,Reference Nair and Maseeh2,Reference Mostafa and Hegazy14) . Therefore, it is important from a public health perspective to understand the comparative variability among different countries in the context of the diversity of the prevailing factors that can potentially influence population-level vitamin D. At the same time, to understand the potential effects of such deficiency more precisely, the deficiency itself needs to be understood.
As per the current guidelines (proposed by the Clinical Practice Guideline of the Endocrine Society), vitamin D deficiency, insufficiency and sufficiency defined as serum level of vitamin D < 12 ng/ml (< 30 nmol/l), < 20 ng/ml (< 50 nmol/l) and > 20 ng/ml (> 50 nmol/l), respectively(Reference Giustina, Adler and Binkley16–Reference Smith, Sievert and Muttukrishna18). However, there is an ongoing discussion about the definition of vitamin D deficiency(Reference Giustina, Adler and Binkley16). Based on some of the newly published studies, the cut-off values for insufficiency and deficiency of serum vitamin D are being reviewed. As such, understanding the true extent of vitamin D deficiency and/or insufficiency prevailing in different countries and regions has become an important aspect.
South Asia (SA) is composed of eight countries – Bangladesh, India, Pakistan, Nepal, Bhutan, Maldives, Sri Lanka and Afghanistan. SA countries together occupy an area of 5131·1 thousand square kilometres with a population of about 1·8 billion(19,Reference Ryabchikov, Sivaramamurti and Yefremov20) . The people of this area, both ethnically and culturally, share some common features, while differences are also observed regarding geography, culture, customs, religion, etc(Reference Barai21,Reference Fatema and Lariscy22) .
Due to generally poor socio-economic conditions, maternal health and nutritional deficiencies are highly prevalent in this region(Reference Fatema and Lariscy22). This contributes to disease burdens (many of which are attributable to hypovitaminosis D) and pregnancy-related complications in SA countries(23–Reference Siegel, Patel and Ali28).
Given the likelihood that vitamin D could be a possible risk factor for many of the health problems in the SA countries, we found only one systematic review on the pregnant women in this region (on the Pakistani pregnant women only yet conducted on a small population, and no meta-analysis was performed)(Reference Nasir, Imran and Zaidi29). Due to this lack of systematic reviews, understanding of the extent of hypovitaminosis D (vitamin D insufficiency) in the SA region (and in the individual countries) is incomplete.
In this study, we assessed the prevalence of vitamin D insufficiency by performing a systematic review and meta-analysis among pregnant women in SA.
Methodology
We used recommendations and guidelines provided by Preferred Reporting Items for Systematic Reviews and Meta-Analyses to conduct this study(Reference Moher, Shamseer and Clarke30).
Data source and search strategy
The three main databases (PubMed, Scopus and Google Scholar) were used in this study (a search was performed after signing out of all Google accounts, to avoid personalised outcomes). Two researchers (BB and MMR) explored these three databases independently from 19 October 2019 until 19 January 2020. The details of the search strategy, list of original MeSH terms and the alternative terms (to minimise the chance of exclusion) used in this study are provided in the supplementary file (online Supplementary Table S1).
The searches were conducted in English. For information on ongoing and unpublished work, regarding insufficiency of vitamin-D, the author’s personal profiles (corresponding author) available online and their profiles on Google Scholar, ResearchGate and ORCID were further explored.
To ensure that grey literature is included in this study, we go through online archives of newspapers that have been published in English from SA countries such as The Telegraph, New Age, The Nation, Daily Bhutan, Maldives Times, Himalayan Times, Sunday Observer, etc. We also explored governments’ reports and published abstracts (in electronic media) as relevant sources from the conference held in SA countries.
Study selection criteria
In this review, we define vitamin D insufficiency as per the current guidelines mentioned above. The inclusion criteria were if they reported vitamin D insufficiency (cut-off < 20 ng/ml) in SA pregnant women; conducted in SA countries during 1st January 2001 to 31 December 2019 and published in peer reviewed journals; conducted on apparently healthy pregnant women in both community level and hospital level whose physical condition was not associated with any chronic illness (chronic kidney, liver and heart disease, cancer, diarrhoea, anaemia, diabetes, etc.) or disease related to any coexisting morbidity (body aches and pain, proximal muscle weakness, osteoporosis, etc.);. studies (cross-sectional, longitudinal, case–control, randomised clinical trial) were included in this review if baseline data were available. However, we took the placebo data for a randomised clinical trial when baseline data were not available.
Studies were excluded if they had a sample size of <50(Reference Jeyakumar and Shinde31); did not mention the prevalence of vitamin D insufficiency and mean level of serum vitamin D; reported vitamin D levels after some form of intervention or supplementation; reported prevalence of vitamin D insufficiency associated to any kind of chronic diseases or any co-morbidity; did not mention prevalence of vitamin D insufficiency and mean level of serum vitamin D; letter to the editor, review article, editorial article; studies that satisfied selection criteria but were not able to obtain full text from the authors after request were also excluded.
Mendeley Desktop program (version 1.19.4) was used to monitor the references and to prevent duplications. After the elimination of duplicates, two researchers (MHS and URS) independently reviewed all papers before selection for final meta-analysis. Disagreements between researchers were resolved by discussion with co-authors.
Data extraction
A standardised Excel sheet was used for data extraction of the selected articles that met eligibility criteria. The following information has been collected for each study: publication details (e.g. first author, publication date, journal name and publisher); research setting, participants’ characteristics and assay method (e.g. country, study area, study design, socio-economic status, method of measurements and sample size) and major findings (e.g. mean level of vitamin D and prevalence). Through revisiting the included papers, all investigators checked the accuracy of the collected data.
In this review, where values of serum level of vitamin D (25-hydroxyvitamin D or 25(OH) D) were presented in nanomol per litre (nmol/l) unit(Reference Sahu, Bhatia and Aggarwal35,Reference Sudhanshu, Upadhyay and Sahu39,Reference Krishnaveni, Veena and Winder41,Reference Sahu, Das and Aggarwal43,Reference Nagendra, Chhina and Shenoi45,Reference Marwaha, Tandon and Chopra46,Reference Anwar, Iqbal and Azam51,Reference Jiang, Christian and Khatry54) , they were converted to nanogram per millilitre (ng/ml) by dividing with 2·5 (according to the international system of unit conversion).
Evaluation of study quality
A checklist of 10 criteria validated by Hoy et al in 2012 was used to determine (as low, moderate and high) the risk of bias for the selected studies(Reference Hoy, Brooks and Woolf32). Regarding this checklist, studies with scores 0–3 were considered low risk of bias, scores between 4 and 6 moderate risk and studies with scores 7–9 are considered as high risk of bias. The risk of bias was assessed on all original papers.
Statistical analysis
The mean value of the serum vitamin D levels and the prevalence of vitamin D insufficiency among pregnant women in SA are considered as summary measurements. The weighted mean level of vitamin D was calculated by using Microsoft Excel (version 2016). The weighted pooled prevalence was calculated with a CI of 95 % using a random-effect model. To assess heterogeneity, the Cochran Q test and the I2 Statistics were used(Reference Chowdhury, Rahman and Akter33). The impact of geography was also demonstrated in analyses according to participants with vitamin D insufficiency. Significant heterogeneity was indicated with an I2, more than 75 %(Reference Higgins, Thompson and Deeks34). The analyses were performed using the Stata version 15 (Stata Corp) ‘metaprop’, ‘metabias’, ‘metafunnel’ commands.
Result
A total number of 997 articles were retrieved from different databases by using the search strategy which describes above. Among these, 977 were excluded because of not matching our inclusion criteria. Finally, twenty study articles were selected for our analysis. The study article’s selection process is shown in Fig. 1.
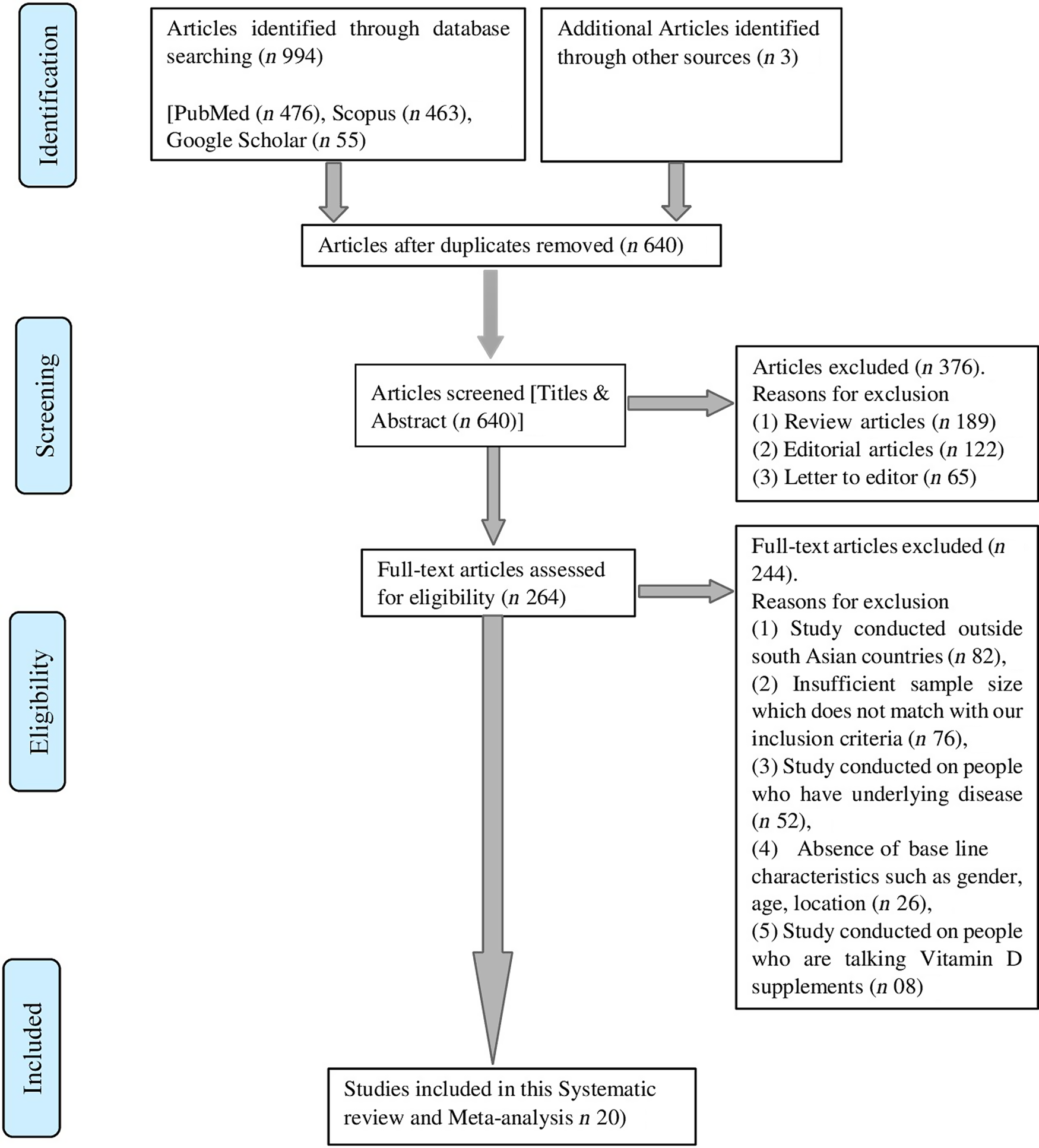
Fig. 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram showing the summary of search result and selection of studies for final analysis.
More than half of the studies (11 out of 20) mention demographic areas for the study population, and socio-economic status for the study population was not mentioned in most of the studies (8 out of 20). The study design was cross-sectional for more than half of our studies (11 out of 20). Only three studies were case control and the rest of them were randomised control trials. Several kinds of measurement methods were used to determine serum vitamin D levels like ELISA, RIA, chemiluminescence immunoassay, chemiluminescent microparticle immunoassay, etc. Among these measurement methods, RIA and ELISA were mostly used (9 out of 20). A summary outlining the features of selected studies was available in Table 1.
Table 1. Characteristics of selected study articles

RCT, randomised control trial; CC, case control; CS, cross sectional; ECLIA, electrochemiluminescence immunoassay; HPLC-MS, high-performance liquid chromatography – tandem mass spectroscopy; AFBM, analytical facility for bio active molecule; CLIA, chemiluminescence immunoassay; RIA, radioimmunoassay; ELISA, enzyme linked immune sorbent assay; CMIA, chemiluminescent micro particle immune assay; NM, not mention.
The studies selected in this systematic review consisted of 7804 pregnant women. Participants were 18 years or above in all studies. In five studies they did not mention participant’s age(Reference Sudhanshu, Upadhyay and Sahu39–Reference Krishnaveni, Veena and Winder41,Reference Sahu, Das and Aggarwal43,Reference Roth, Al Mahmud and Raqib49) . Prevalence of insufficiency and the average level of vitamin D were mentioned in all studies. Prevalence of insufficiency ranged from 9 to 97 % and the average vitamin D level were ranged from 9 to 24·86 ng/ml. The overall pooled prevalence of vitamin D insufficiency was 65 % (95 % CI: 51 %, 78 %) (Fig. 2). The weighted mean level of serum vitamin D was 16·36 ng/ml, and the weighted standard deviation (weighted sd) was 7·12 ng/ml.
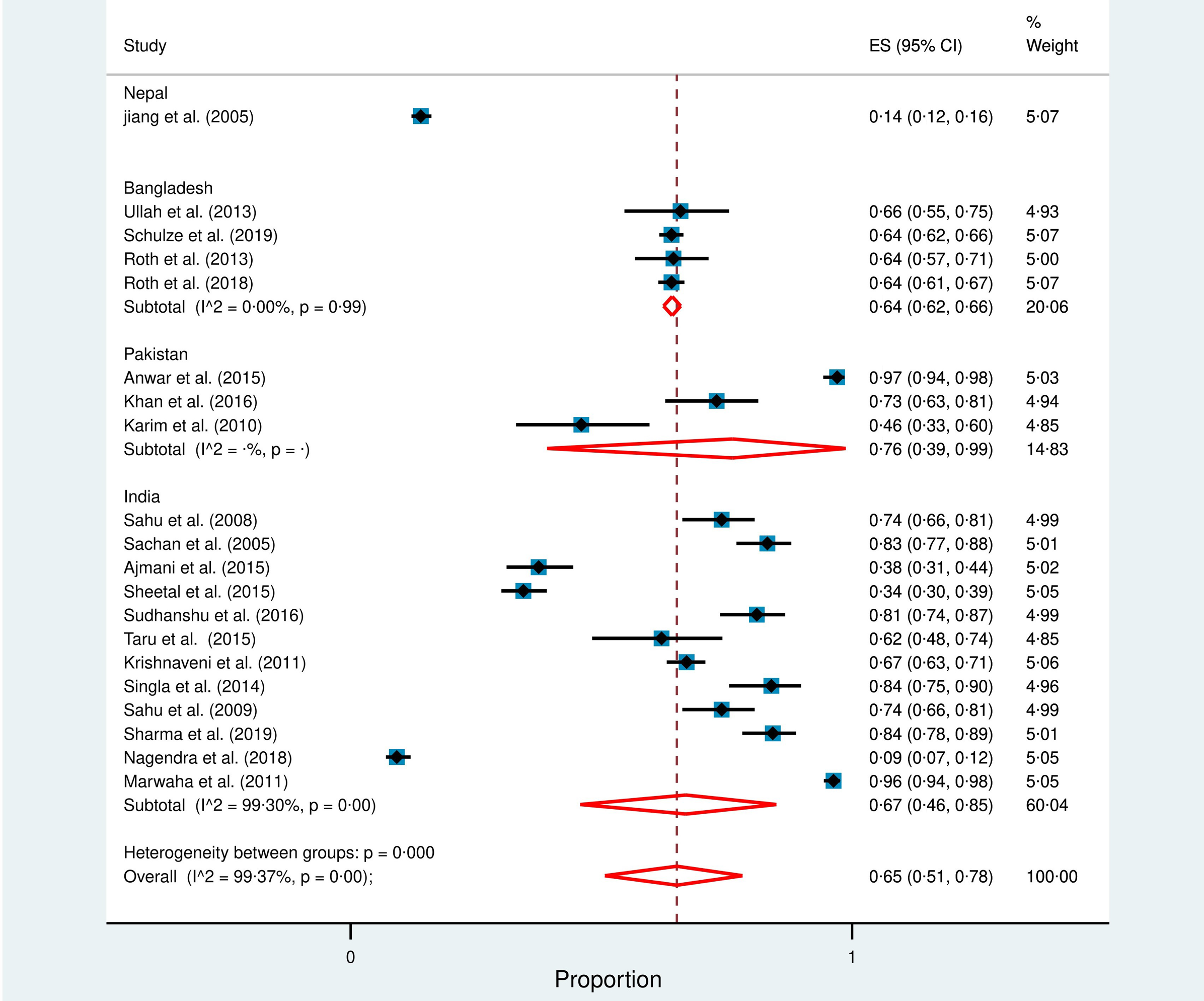
Fig. 2. Forest plot represent overall and country wise prevalence of vitamin D insufficiency among South Asian Pregnant women. In this forest plot, all the diamonds, except the last one (overall pooled prevalence), represents polled prevalence for individual country: (1) Nepal (2) Bangladesh, (3) Pakistan, (4) India. Each horizontal line of the forest plot represents an individual study and the box plotted as prevalence for that study. The horizontal points of the diamond represent the limit of 95 % CI.
A high degree of heterogeneity was observed in the prevalence of vitamin D insufficiency (I2 = 99·37 %; P = 0·00).
Country-wise result
Studies from four out of eight SA countries (Bangladesh, India, Pakistan and Nepal) matched our selection criteria, and hence were included in this study. No studies were found from Bhutan, Sri Lanka, Afghanistan and Maldives regarding serum vitamin D levels and prevalence of vitamin D insufficiency among pregnant women. The Forest plot shows the country-wise prevalence of vitamin D insufficiency (Fig. 2). Weighted mean level of vitamin D among SA pregnant women can be found in the Supplementary file Fig. S1.
India
We found twelve studies from India which consisted of 3182 participants(Reference Sahu, Bhatia and Aggarwal35–Reference Marwaha, Tandon and Chopra46). Study design was mostly cross sectional (nine out of twelve), with the others being either case controlled or randomised control trial studies. Out of twelve studies, half of these did not mention demographic areas for the study population, and the rest were either urban or rural or both. One-third of total studies did not mention socio-economic status for study participants, and rest of the studies include either both socio-economic groups (upper and lower) of populations or only lower economic groups of populations. The weighted mean level of vitamin D for study participants was 16·31 ng/ml (weighted sd 7·90 ng/ml), and random effect meta-analysis showed that the weighted pooled prevalence of vitamin D insufficiency was 67 % (95 % CI: 46 %, 85 %) with a significant heterogeneity (I2 = 99·30 %; P = 0·00).
Bangladesh
We could retrieve four studies from Bangladesh with a total of 3055 participants(Reference Ullah, Koch and Tamanna47–Reference Roth, Morris and Zlotkin50). The majority of the studies were randomised control trials, whereas there was only one case–control study. In case of demography, two studies were conducted among urban population, one in rural population and one study did not mention about demographic areas for study population. On the other hand, socio-economic status for study participants was not mentioned in two studies, and two studies include participants from both lower and upper socio-economic groups. The weighted mean vitamin D level for study participants was 15·55 ng/ml (weighted sd 5·29 ng/ml), and random effect meta-analysis revealed that the weighted pooled prevalence of vitamin D insufficiency was 64 % (95 % CI: 62 %, 66 %).
Pakistan
In Pakistan, we found three studies with a total of 404 participants(Reference Anwar, Iqbal and Azam51–Reference Karim, Nusrat and Aziz53). Study designs were either cross sectional or randomised control trials. Only one study mentioned about demographic area for study population that represented both rural and urban populations. On the contrary, socio-economic status for study participants was mentioned in two out of three studies. One study was conducted on a lower socio-economic group of population and another one included participant from both lower and upper socio-economic classes. The random effect meta-analysis demonstrated that the weighted pooled prevalence of vitamin D insufficiency was 76 % (95 % CI: 39 %, 99 %) among the study participants with weighted mean of 11·27 ng/ml (weighted sd 6·28 ng/ml).
Nepal
We found only one study in Nepal that was a randomised control trial and that study was conducted among 1163 rural pregnant women(Reference Jiang, Christian and Khatry54). The socio-economic status was not mentioned. Our study revealed that 14 % of the participants were vitamin D insufficient with an average of 20·44 ng/ml.
Study-Setting wise result
In case of study setting, more than half (11 out of 20) of the studies were hospital-based and the rest were community based.
Prevalence of vitamin D insufficiency was higher in the community-based studies (71 %; 95 % CI: 47 %, 90 %) compared with the hospital-based (60 %; 95 % CI: 40 %, 78 %) studies. High degree of heterogeneity was found in both studies setting (I2 = 99 %; P = 0·00) (Fig. 3).
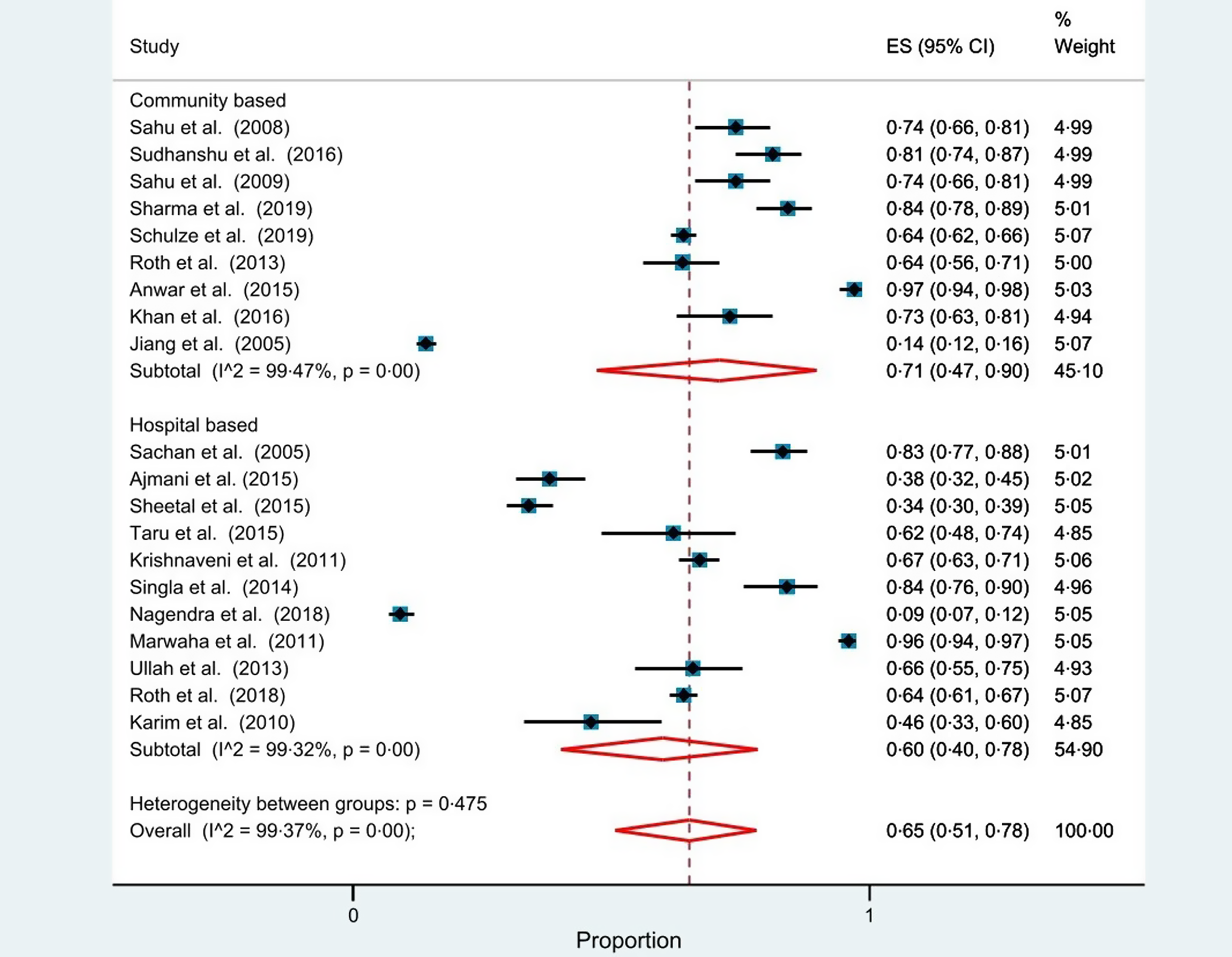
Fig. 3. Forest plot represents prevalence of vitamin D insufficiency in accordance with study settings (community-based v. hospital-based). In this forest plot, all the diamonds, except the last one, represents polled prevalence on the basis of study settings: (1) community-based and (2) hospital-based. Each horizontal line of the forest plot represents an individual study and the box plotted as prevalence for that study. The horizontal points of the diamond represent the limit of 95 % CI.
Quality assessment
Among these selected studies, no study was found with a high risk of bias, thirteen studies with moderate risk of bias and the reminder with low risk of bias. Risk of bias table available in supplementary file (online Supplementary Table S2).
Publication bias
The funnel plot indicated the existence of asymmetry and publication bias for the prevalence of vitamin D insufficiency (online Supplementary Fig. S2). Eggers’s test was found statistically insignificant, which means publication bias was small in case of this meta-analysis (P = 0·84).
Discussion
Results from this study reveal that as much as 65 % (95 % CI: 64 %, 72 %) of the SA pregnant women could be affected with vitamin D insufficiency (Fig. 2). Our findings parallel with a systematic review and meta-analysis conducted on Iranian pregnant women reporting approximately 68 % of the study participants being vitamin D insufficient (using < 20 ng/ml cut-off)(Reference Vatandost, Jahani and Afshari55). Comparison of this insufficiency to the other parts of the world implies that this problem might be worse in SA compared with Africa (around 34 %; using < 20 ng/ml cut-off)(Reference Mogire, Mutua and Kimita56). We speculate that such widespread insufficiency of vitamin D could be linked to the high prevalence of some of the health problems and pregnancy-related complications in this region. Indeed, this speculation is supported by high prevalence and the rising trend of pregnancy-related complications, communicable and non-communicable diseases in SA(23–Reference Siegel, Patel and Ali28).
For instance, like many other non-communicable diseases, the rate of cesarean section is increasing significantly in SA countries, especially in India, Pakistan, Bangladesh and Maldives. The overall cesarean rate has been found more than 15 % in these countries which have crossed the WHO recommended range (10–15 %)(Reference Verma, Vishwakarma and Nath25). In this regard, some studies reported the association between low serum level of vitamin D and the risk of cesarean section 26, 57. Besides this, some study reports also suggested that gestational diabetes, eclampsia and preeclampsia and various non-communicable diseases are increasing among different SA countries(Reference Soomro, Kumar and Lakhan24,Reference Mithal, Bansal and Kalra27,Reference Siegel, Patel and Ali28,Reference Begum, Begum and Quadir58,59) . Therefore, the causal association of high insufficiency of vitamin D and the rising trend of these diseases should be considered seriously for better health care delivery in SA.
While the highlight of this study was high vitamin D insufficiency, we also found a high degree of heterogeneity in overall results (I2 = 99·37 %). We hypothesise that geographical location could be a factor for such a large-scale heterogeneity.
Country-wise comparison showed that Pakistan had the highest prevalence (76 %; 95 % CI: 39 %, 99 %), followed by India (67 %; 95 % CI: 46 %, 85 %) and Bangladesh (64 %; 95 % CI: 62 %, 66 %) (Fig. 2). It is hypothesised that variability in the degree of sunlight exposure due to differences in geographical locations could be a probable reason for this. Throughout the year, people living in tropical areas get more sunlight exposure than those living in subtropical regions. Vitamin D synthesised naturally in our body when UVB from sunlight penetrates our skin and undergoes some physiological changes(Reference Holick1,Reference Nair and Maseeh2,Reference Maghbooli, Hossein-Nezhad and Shafaei13) . Pakistan is situated in a subtropical region where there is relatively low sunlight availability compared to tropical regions. The national boundaries of Bangladesh and India both share tropical and subtropical regions in their national map(Reference Mavridou, Pappa and Papatzitze60). Our hypothesis can be bolstered by the fact that a high prevalence of vitamin D insufficiency was also observed in countries like Iran (56 %) and China (70 %) (using < 20 ng/ml cut-off), which share similar geographical locations on their national map(Reference Vatandost, Jahani and Afshari55,Reference Wei, Zhu and Ji61) . Additionally, this hypothesis is also corroborated by intra-country study reports. For instance, geolocation hinted that northern part of India is placed in sub-tropical zone, whereas southern section is in tropical zone(Reference Mavridou, Pappa and Papatzitze60). Study reports suggested that prevalence of vitamin D insufficiency is higher amid north Indian pregnant women (93 %) in comparison with pregnant women (65 %) from south India(Reference Sharma, Kumar and Prasad38,Reference Navaneethan, Mani and Shrestha62) .
While a high degree of heterogeneity cannot be fully explained with variation in geography, several other factors such as skin colour, clothing practice, cultural aspects and diet may also influence variation among prevalence in this region(Reference Holick1,Reference Nair and Maseeh2,Reference Maghbooli, Hossein-Nezhad and Shafaei13) . For instance, in this review, we found only a single study from Nepalese pregnant women that reported pregnant women from Nepal had the lowest percentage (14 %) of prevalence than people in the Bangladesh, India and Pakistan (Indian subcontinent). In this regard, we hypothesise that this could be related to some of the cultural aspects and skin colour. According to the Fitzpatrick skin type, most Nepalese belong to lighter skin in comparison with Indian subcontinent women(Reference Afifi, Saeed and Pasch63). Despite Nepal being situated in a subtropical region(Reference Mavridou, Pappa and Papatzitze60), this lighter skin complexion could be an important factor behind the lowest observed prevalence of vitamin D insufficiency, in comparison to rest of the Indian sub-continent. Hence, we hypothesise that the disparity of skin complexion among SA population might be a potential confounding factor for the heterogeneity of serum vitamin D in SA.
Furthermore, we hypothesise that clothing practice may also act as a factor behind such a high prevalence of insufficiency in the Indian subcontinent. The use of burqas (traditional full-body covering), hijab (Muslim wearing that covers the upper part of the body), similar to other non-religious body coverings (traditional clothes) block direct sunlight exposure event in the outdoor setting. These types of clothing practices are very common in many states of India, Pakistan and Bangladesh. A recent media report also suggests that these practices have increased exponentially in this region over the past three decades(64). We argue that this could be linked to the high prevalence of vitamin D in this region and also the high heterogeneity observed in this study.
Our argument is bolstered by the fact that people from the European countries have quite opposite skin colour and dressing practices from the Indian sub-continent(Reference Afifi, Saeed and Pasch63). A study report from a large observational data suggested that insufficiency rate is lower among Europeans in comparison with SA (using < 20 ng/ml cut-off – 40 % of Europeans are vitamin D insufficient)(Reference Cashman, Dowling and Škrabáková65). Therefore, clothing practice might be a confounding factor for such a high prevalence of insufficiency in this region.
Besides this, we also hypothesise that the cultural aspect of this region may also act as a factor for such a high prevalence of insufficiency. A lesser number of SA women spend their time in outdoor environment for work purpose (meaning the majority stay in the households), which effectively limits their exposure to direct sunlight for the majority. In the year 2020, World Bank reported that the participation rate of female labour is close to 24 %, whereas the participation rate of male labor is 80 % in SA(66). Similar trends have been found in Middle East women. The World Bank stated in 2020 that female labor participation in Middle East countries is close to 20 % only(67). As a majority of SA women spend more time in household jobs, they are more likely to receive lesser exposure to sunlight. Perhaps, this partially explains 60 % of Saudi Arabian women residing in Riyadh city being vitamin D insufficient(Reference AlFaris, AlKehayez and AlMushawah68).
Additionally, in our study, we also found that studies that are designed on community-based setting (71 %; 95 % CI: 47 %, 90 %) showed a high prevalence of insufficiency in comparison with hospital-based setting (60 %; 95 % CI: 40 %, 78 %) (Fig. 3). According to the iceberg phenomenon(Reference Magombedze, Ngonghala and Lanzas69), our findings suggest that a substantial number of pregnant women who lived in SA countries are affected with vitamin D insufficiency that is either subclinical, unreported or concealed from view. Therefore, community-based study settings demonstrated such a high prevalence of insufficiency in SA pregnant women.
Furthermore, a high percentage of early marriage (meaning likely early pregnancy) which has been implicated with insufficiency of essential nutrients for the young adults could be another factor behind high-level vitamin D insufficiency in SA. During pregnancy, women require more vitamin D than usual for fetus development(Reference Pilz, Zittermann and Obeid3–Reference Leere and Vestergaard5). UNICEF reported that more than half (56 %) of the SA women get married before the age of 18. The child marriage rate is higher in Bangladesh (74 %), then followed by India (58 %) and then Nepal (52 %)(70). Consequently, this early pregnancy and lack of nutrition(71) might be also acting as a factor for such a high prevalence of vitamin D insufficiency with high degree of heterogeneity among the pregnant women in SA.
While all of the hypotheses proposed above could be contributing to the observed heterogeneity, slightly different cut-off values (other than < 20 ng/ml) used by some of studies that were included in this systematic review(Reference Sachan, Gupta and Das36,Reference Sharma, Kumar and Prasad38,Reference Gupta, Wahi and Gupta40,Reference Ullah, Koch and Tamanna47,Reference Roth, Al Mahmud and Raqib49,Reference Roth, Morris and Zlotkin50,Reference Jiang, Christian and Khatry54) might have influenced the degree of heterogeneity in our analysis. However, such heterogeneity may not be uncommon as we have demonstrated in one of the similar studies on SA adult population(Reference Siddiqee, Bhattacharjee and Siddiqi72). However, it is clear that further study is required to reveal the true source and extent of heterogeneity.
Limitations
While this study highlights critical health issues, it also has a few limitations. First, most of the studies that match with our selection criteria (15 out of 20) did not mention socio-economic conditions (income status, urban v. rural differences). Therefore, because of inadequate data, we could not test the effect of these factors in our study. Furthermore, we did not find any study from Sri Lanka, Bhutan, Maldives and Afghanistan. About 95 % (19 out of 20) of our selected studies were conducted among pregnant women from the Indian sub-continent. We only got a single study from Nepal. As such, because of insufficient data, we could not find the weighted mean level of vitamin D status for that country. Moreover, studies included in this review used various methods to assay the status of vitamin D in serum. While this might have introduced assay bias to our findings, this limitation is present in similar studies and was indeed inescapable. Another limitation is that, in this study, we used cut-off < 20 ng/ml to define vitamin D insufficiency. However, due to lack of studies among SA pregnant women, a few of studies were also included in our analysis that used different cut-offs(Reference Sachan, Gupta and Das36,Reference Sharma, Kumar and Prasad38,Reference Gupta, Wahi and Gupta40,Reference Ullah, Koch and Tamanna47,Reference Roth, Al Mahmud and Raqib49,Reference Roth, Morris and Zlotkin50,Reference Jiang, Christian and Khatry54) . Furthermore, due to poor economic condition, vitamin D assessments are often expensive for SA pregnant women. Therefore, only pregnant women with suspected deficiency or who participated in a study or a trial that included assessment of vitamin D may be assessed. This is an inherent limitation of any such study on secondary data, and, therefore exercise of caution is recommended before generalising the results of this study.
Recommendations
Our study revealed high rise of vitamin D insufficiency among SA pregnant women. We recommend that further study is needed to see if our findings apply to a wider group of the general population. While some researchers argue that deficiency of vitamin D should be treated similar to an ongoing pandemic(Reference Holick7,Reference Cashman, Dowling and Škrabáková65) . However, our search did not unveil any policies or national-level nutritional guidelines for vitamin D except in India(73). While the existing guidelines as such supplementation and food fortification program from other countries(73,Reference Bouillon74,Reference Cavelaars, Kadvan and Doets75,Reference Aguiar, Andronis and Pallan76) can be helpful for SA, we argue that the socio-cultural scenario of the individual countries (e.g. clothing practice, skin complexion and economic status) needs to be taken into consideration. Women, who wear heavy clothes and spend more time in indoor activities, can be advised to check their serum level of vitamin D regularly and take proper supplements. It has been suggested that an adult without adequate sunlight exposure should take 800–1000 IU of vitamin D per day(Reference Holick1). In addition, women can be encouraged to spend time in direct sunlight exposure to prevent themselves from vitamin D insufficiency. Moreover, some other challenges need to be addressed in SA. A negative attitude towards sunlight exposure can be a big challenge. It has been reported that Indian and Pakistani students had a lack of knowledge about vitamin D and a negative attitude towards sunlight exposure(Reference Arora, Dixit and Srivastava77,Reference Tariq, Khan and Basharat78) . This lack of knowledge and a negative attitude could be a major factor behind staying away from sunlight that can lead to vitamin D insufficiency. While further research is necessary to understand this. However, launching mass campaigns about the relationship between sunlight exposure and vitamin D insufficiency can be effective for SA governments.
Apart from the policies focusing on supplementation and encouraging natural synthesis, necessary measures should be taken to increase the number of diagnostic tests for detecting the serum level of vitamin D status. For achieving this, increasing the number of diagnostic centres and reducing the price for testing by offering subsidies can also be considered by the governments in the SA region.
Conclusions
Our findings reveal that more than six out of ten SA pregnant women could be suffering from vitamin D insufficiency. To our knowledge, this is the first systematic review and meta-analysis that discusses the prevalence of vitamin D insufficiency among SA pregnant women. While this study focused solely on a small group of SA pregnant women, further research is needed to check if our findings represent a wider group of general population in SA. Furthermore, strategies for prevention, diagnosis and treatment of vitamin D deficiency need to be integrated into public health policy by SA policymakers.
Acknowledgements
We are thankful to Mohammed Tanveer Hussain for his efforts in checking the grammatical aspects of the manuscript.
Our research received no grant from any funding agency in the public, commercial or not-for-profit sectors.
M. H. S., PhD: Conceptualisation, study design, reviewing method, supervision, checking literature, data analysis, drafting and reviewing manuscript. B. B., MS: Study design, reviewing method, searching literature, data compilation and writing manuscript. U. R. S., PhD: Conceptualisation, study design, supervision and reviewing manuscript. M. M. R., M. H. S: Reviewing method, supervision, checking literature and data analysis.
The authors declare that they have no competing interest.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114521004360