COVID-19
SG-APSIC1026: COVID-19 vaccine acceptance and hesitancy among primary healthcare workers in Singapore
-
- Published online by Cambridge University Press:
- 16 March 2023, p. s3
-
- Article
-
- You have access
- Open access
- Export citation
Poster Presentation - Top Poster Award
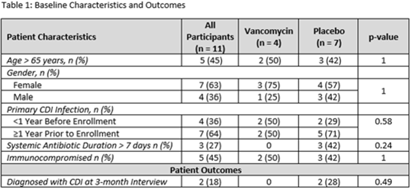
C. difficile
Utilizing vancomycin as secondary prophylaxis for the prevention of recurrent Clostridioides difficile infection
-
- Published online by Cambridge University Press:
- 29 September 2023, p. s5
-
- Article
-
- You have access
- Open access
- Export citation
Original Article
Costs of two vancomycin-resistant enterococci outbreaks in an academic hospital
-
- Published online by Cambridge University Press:
- 13 January 2023, e8
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
COVID-19
SG-APSIC1113: Descriptive study on COVID-19 exposures in Singapore General Hospital
-
- Published online by Cambridge University Press:
- 16 March 2023, p. s3
-
- Article
-
- You have access
- Open access
- Export citation
Poster Presentation - Top Poster Award
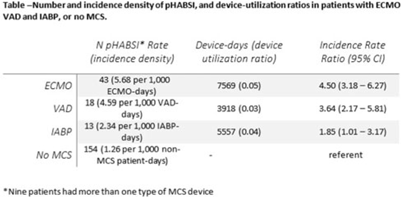
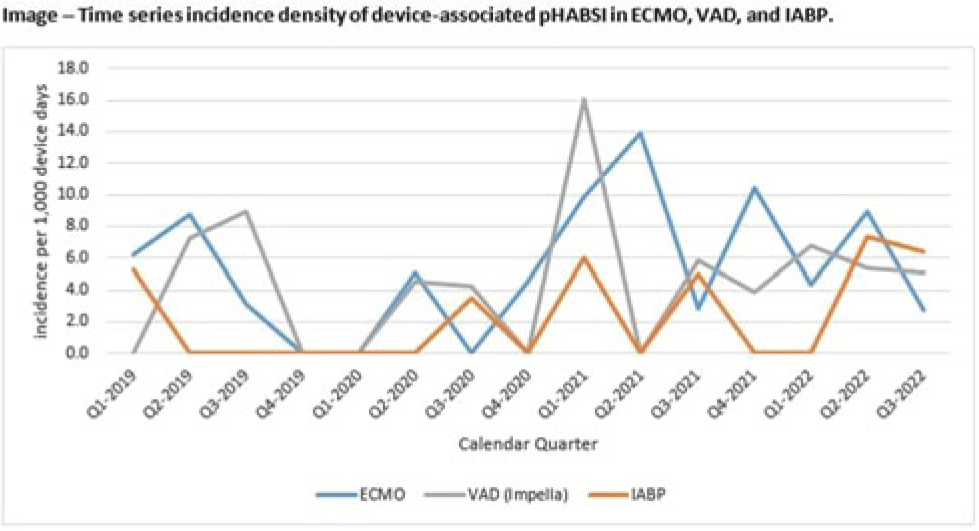
CLABSI
Relative risk of primary bloodstream infection in patients with mechanical circulatory support devices
-
- Published online by Cambridge University Press:
- 29 September 2023, p. s6
-
- Article
-
- You have access
- Open access
- Export citation
Original Article
Measuring clinical outcomes of highly multiplex molecular diagnostics for respiratory infections: A systematic review and conceptual framework
-
- Published online by Cambridge University Press:
- 09 January 2023, e9
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
COVID-19
SG-APSIC1158: COVID-19 vaccine booster hesitancy among healthcare workers: A retrospective observational study in Singapore
-
- Published online by Cambridge University Press:
- 16 March 2023, pp. s3-s4
-
- Article
-
- You have access
- Open access
- Export citation
Commentary
Antimicrobial Stewardship and Healthcare Epidemiology year in review, 2022: Celebrating successes while focusing on the future
-
- Published online by Cambridge University Press:
- 11 January 2023, e10
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Poster Presentation - Top Poster Award
COVID-19
Healthcare personnel at non–acute-care facilities are at risk of COVID-19 from workplace and community exposures
-
- Published online by Cambridge University Press:
- 29 September 2023, p. s6
-
- Article
-
- You have access
- Open access
- Export citation
COVID-19
SG-APSIC1054: Sputnik-V postvaccination immunologic responses in nasal mucosa: A prospective cohort study in Kazakhstan
-
- Published online by Cambridge University Press:
- 16 March 2023, p. s4
-
- Article
-
- You have access
- Open access
- Export citation
Original Article
Increasing cefazolin use for surgical prophylaxis in penicillin-allergy–labeled patients
-
- Published online by Cambridge University Press:
- 11 January 2023, e11
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
COVID-19
SG-APSIC1119: N95 mask concordance amongst female Muslim healthcare workers undergoing mask fitting with and without tudung
-
- Published online by Cambridge University Press:
- 16 March 2023, p. s4
-
- Article
-
- You have access
- Open access
- Export citation
Poster Presentation - Top Poster Award
COVID-19
Low infectivity among asymptomatic patients with a positive SARS-CoV-2 admission test at a tertiary-care center, 2020–2022
-
- Published online by Cambridge University Press:
- 29 September 2023, p. s7
-
- Article
-
- You have access
- Open access
- Export citation
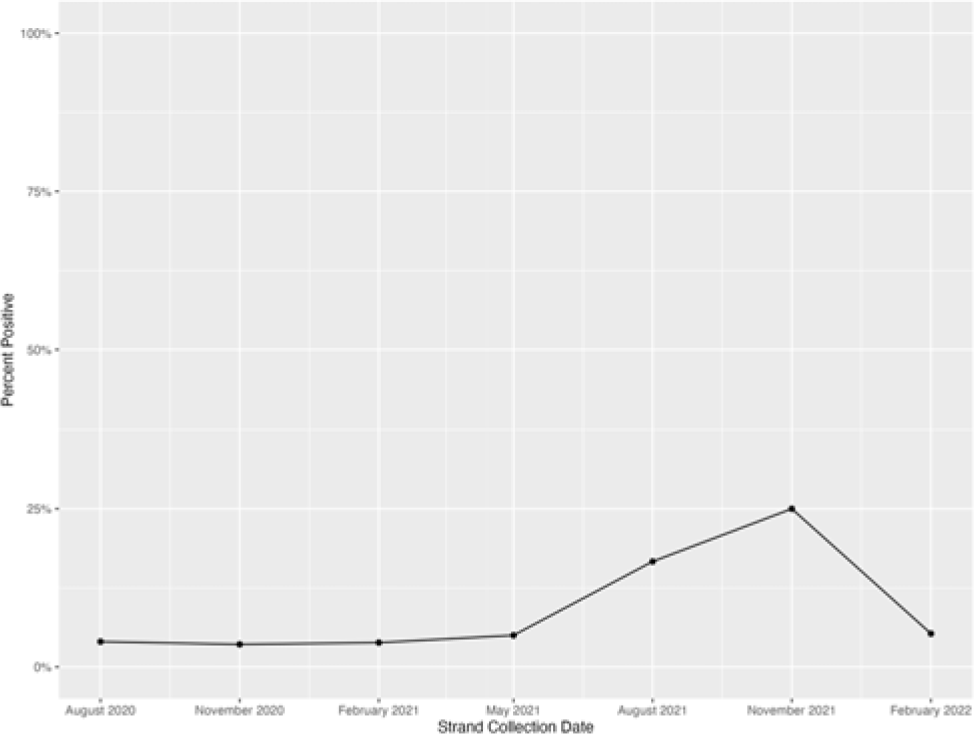
Concise Communication
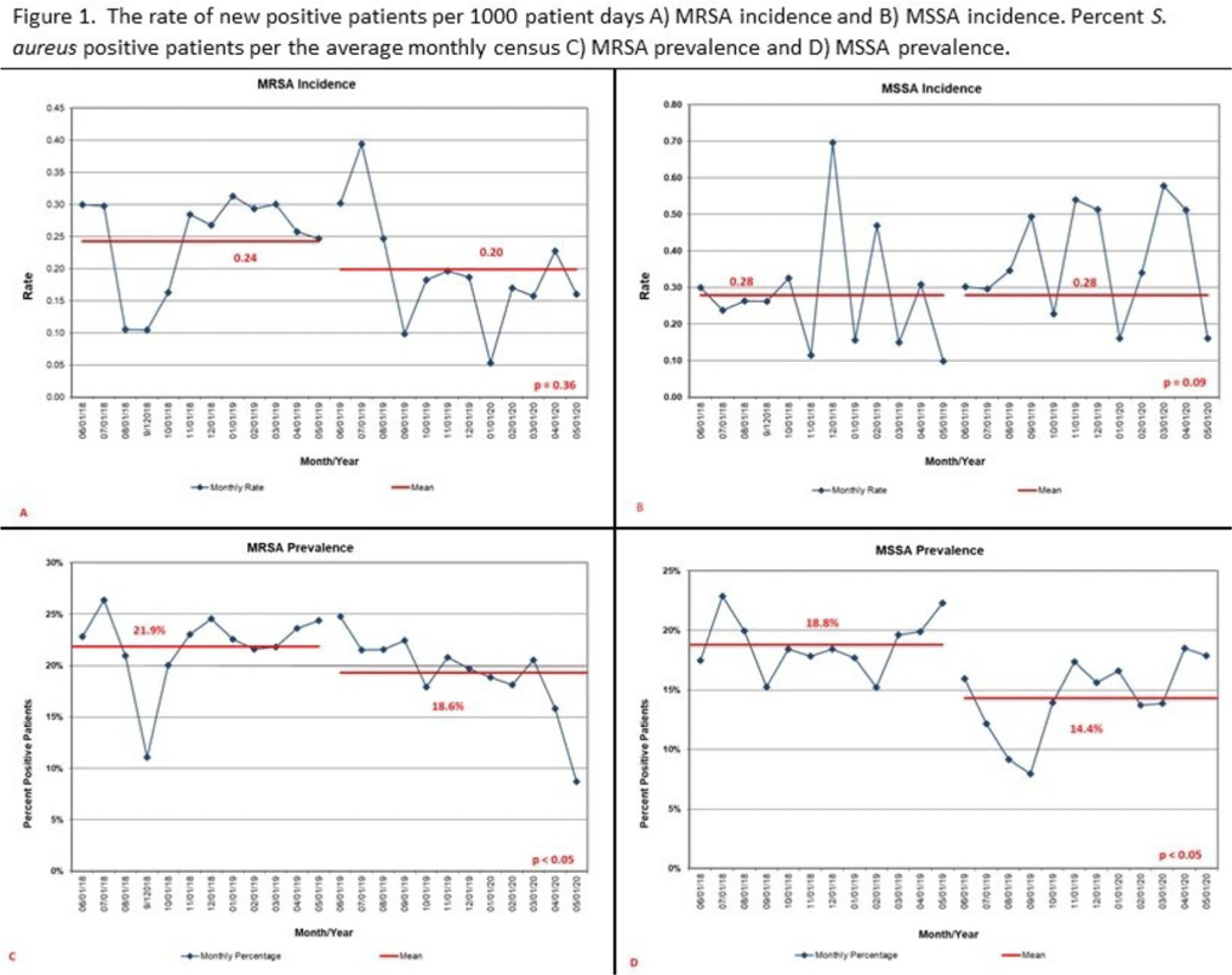
Trends in pediatric community-onset Staphylococcus aureus antibiotic susceptibilities over a five-year period in a multihospital health system
-
- Published online by Cambridge University Press:
- 17 January 2023, e12
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
COVID-19
SG-APSIC1049: Immunogenicity of Gam-COVID-Vac and Sinopharm BBIBP-CorV vaccines in seropositive and seronegative adults
-
- Published online by Cambridge University Press:
- 16 March 2023, pp. s4-s5
-
- Article
-
- You have access
- Open access
- Export citation
Poster Presentation - Top Poster Award
COVID-19
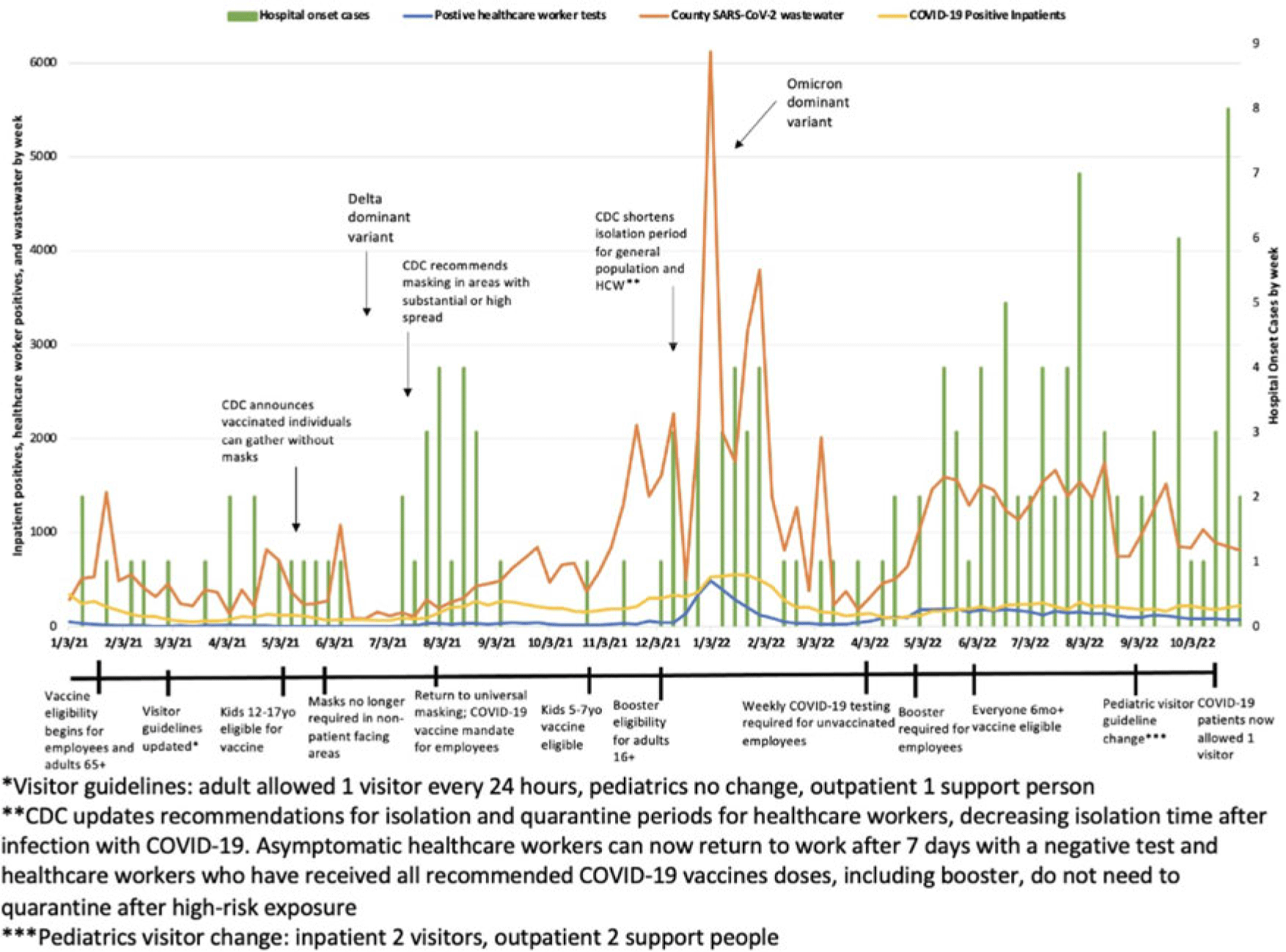
Hospital-onset COVID-19: Associations with population- and hospital-level measures to guide infection prevention efforts
-
- Published online by Cambridge University Press:
- 29 September 2023, p. s7
-
- Article
-
- You have access
- Open access
- Export citation
COVID-19
SG-APSIC1176: Laboratory-acquired COVID-19 during the SARS-CoV-2 ο (omicron) pandemic wave at a tertiary-care hospital in Korea
-
- Published online by Cambridge University Press:
- 16 March 2023, p. s5
-
- Article
-
- You have access
- Open access
- Export citation
Poster Presentation - Top Poster Award
Decolonization Strategies
Effectiveness of a Staphylococcus aureus mupirocin decolonization protocol in a neonatal intensive care unit
-
- Published online by Cambridge University Press:
- 29 September 2023, p. s8
-
- Article
-
- You have access
- Open access
- Export citation
Original Article
Developing a quality measure to assess use of antibiotic medications for respiratory conditions
-
- Published online by Cambridge University Press:
- 17 January 2023, e13
-
- Article
-
- You have access
- Open access
- HTML
- Export citation
Poster Presentation - Top Poster Award
Diagnostic/Microbiology
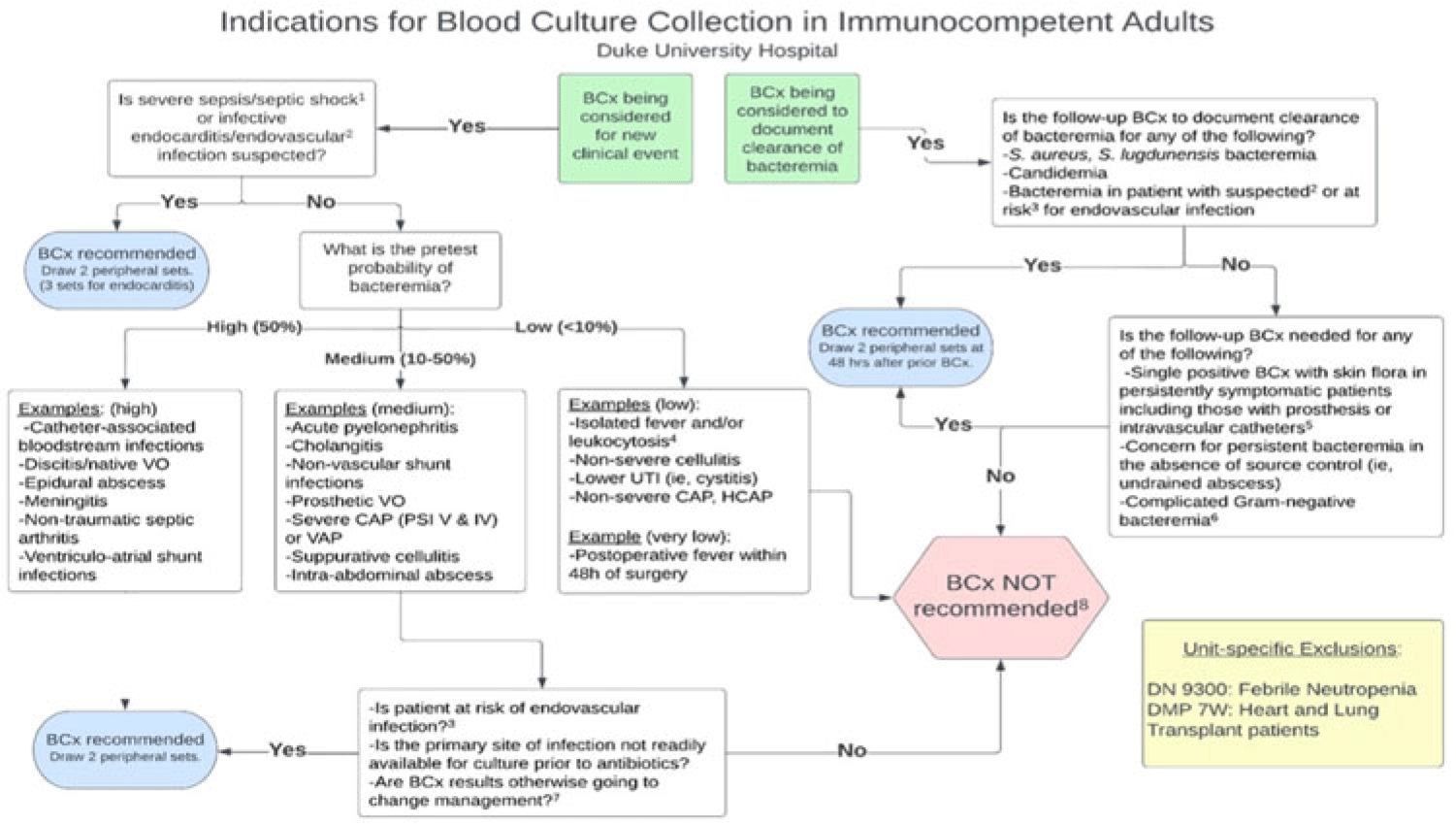
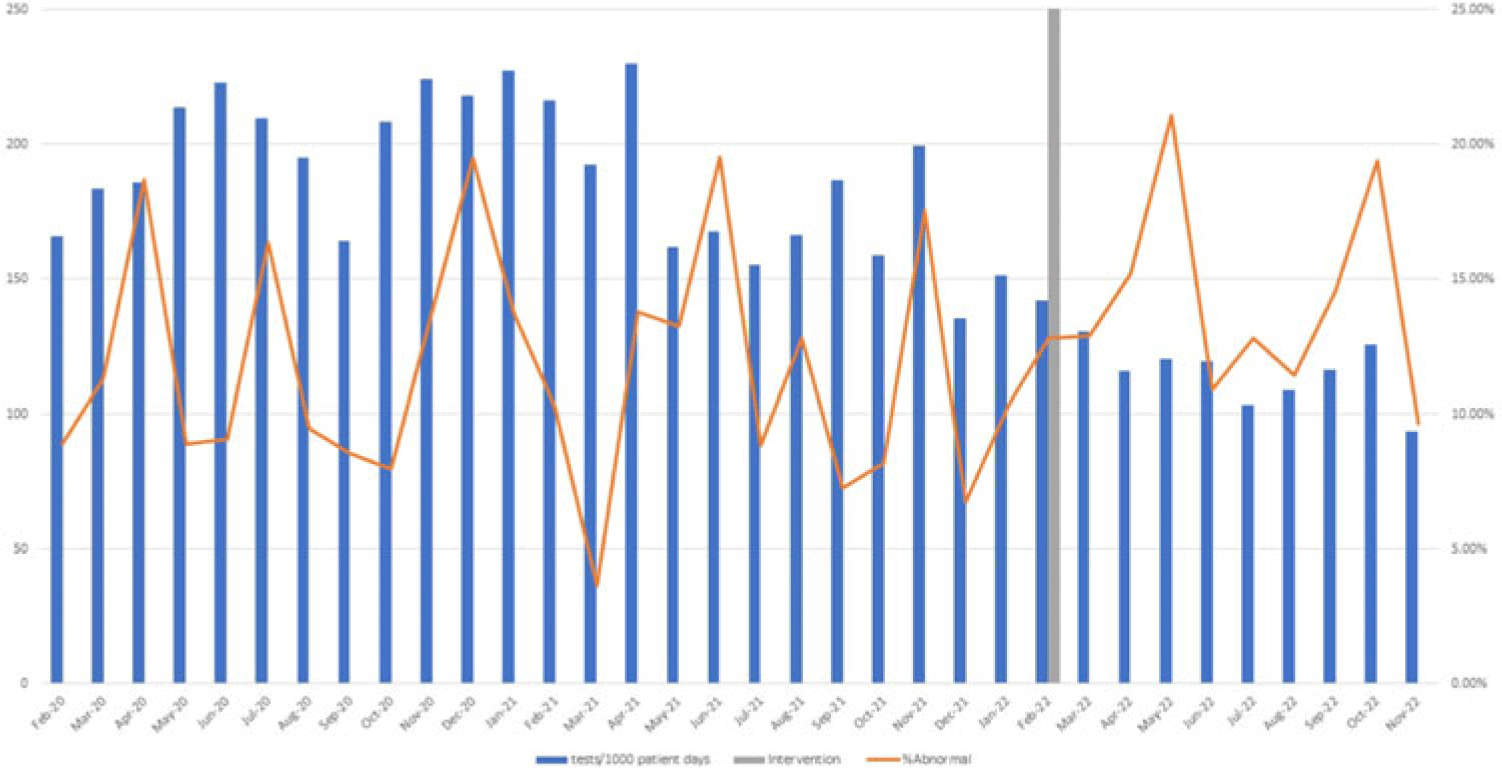
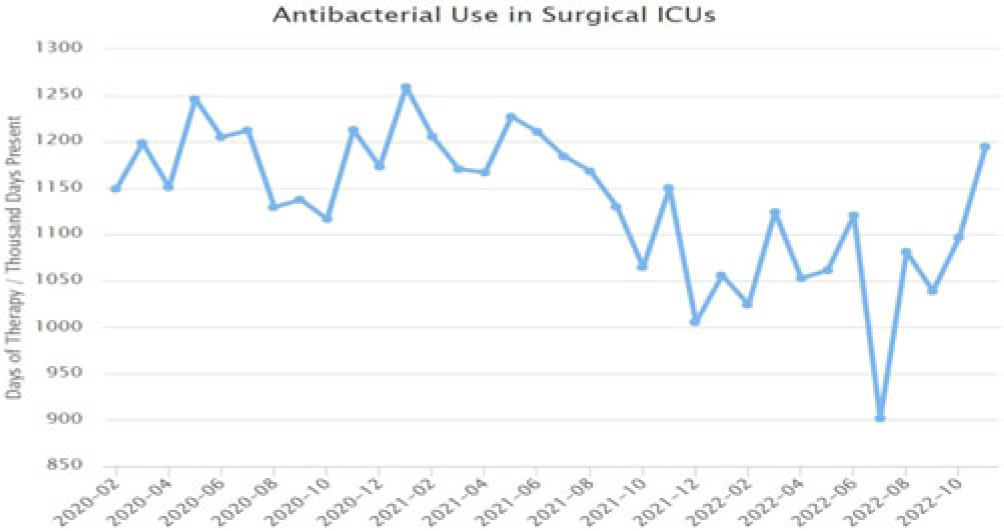
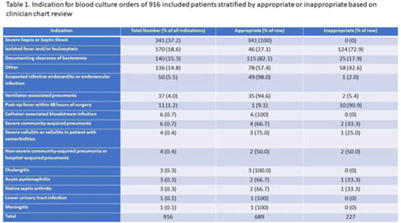
Implementation of diagnostic stewardship in two surgical ICUs: Time for a blood-culture change
-
- Published online by Cambridge University Press:
- 29 September 2023, pp. s9-s10
-
- Article
-
- You have access
- Open access
- Export citation