Simulation-based training (SBT) utilizes artificial representation of real-world processes to allow for learning with approximation of practice. It is an educational technique, not a technology, that facilitates learning through immersion, reflection, feedback, and practice in a controlled environment with minimal risk to patients. The Institute of Medicine’s “To err is human” highlighted medical errors and their consequences, emphasizing the need for patient safety through the design of a safer health system. 1 Common root causes of preventable medical errors were communication breakdowns, faulty systems of care, lack of standardization in practice, and insufficient knowledge. 1,Reference Makary and Daniel2 By allowing practice in a realistic and interactive setting with minimal risk to patients, SBT can help minimize medical errors by acquiring clinical skills through practice, improving communication skills, defining team structures, and refining protocols. Reference Dawson and Gould3,Reference Issenberg, McGaghie and Hart4
According to the Centers for Disease Control and Prevention (CDC), 1 in 31 hospitalized patients developed at least 1 healthcare-associated infection (HAI) in 2018. 5 Most HAIs are related to invasive devices or procedures: catheter-associated urinary tract infection (CAUTI), central-line–associated bloodstream infection (CLABSI), surgical site infection (SSI), and ventilator-associated pneumonia (VAP). Evidence-based prevention strategies can reduce HAIs but are insufficiently implemented. Education is a key component of infection prevention efforts and traditional methods of teaching include lectures, videos, and fact sheets with some opportunities for hands-on practice. Reference Safdar and Abad6 With growing recognition of SBT in healthcare education, SBT can also be used as an important adjunct to traditional teaching and assessment methods in infection prevention. In this study, we performed a focused literature review on the use of SBT in HAI prevention and highlight the importance of SBT as an educational tool in infection prevention.
Methods
We reviewed English language publications from PubMed using combinations of keywords “simulation,” “infection prevention,” “healthcare-acquired infections,” and “disaster preparedness.” From this, we selected original articles that utilized SBT as the primary mode of education for infection prevention efforts in acute care hospitals. We defined simulation as the mode of training that utilized imitation or representation of one act or system by another. The references for each relevant paper were additionally reviewed.
Results
We retrieved 138 English language publications from PubMed, of which 111 were excluded because simulation was not utilized for infection prevention education in acute-care hospitals. We then performed a detailed review of 27 publications that utilized simulation as primary mode of education for HAI prevention in acute care hospitals (Table 1).
Table 1. Simulation in Healthcare-Acquired Infection Prevention: Review of Medical Literature
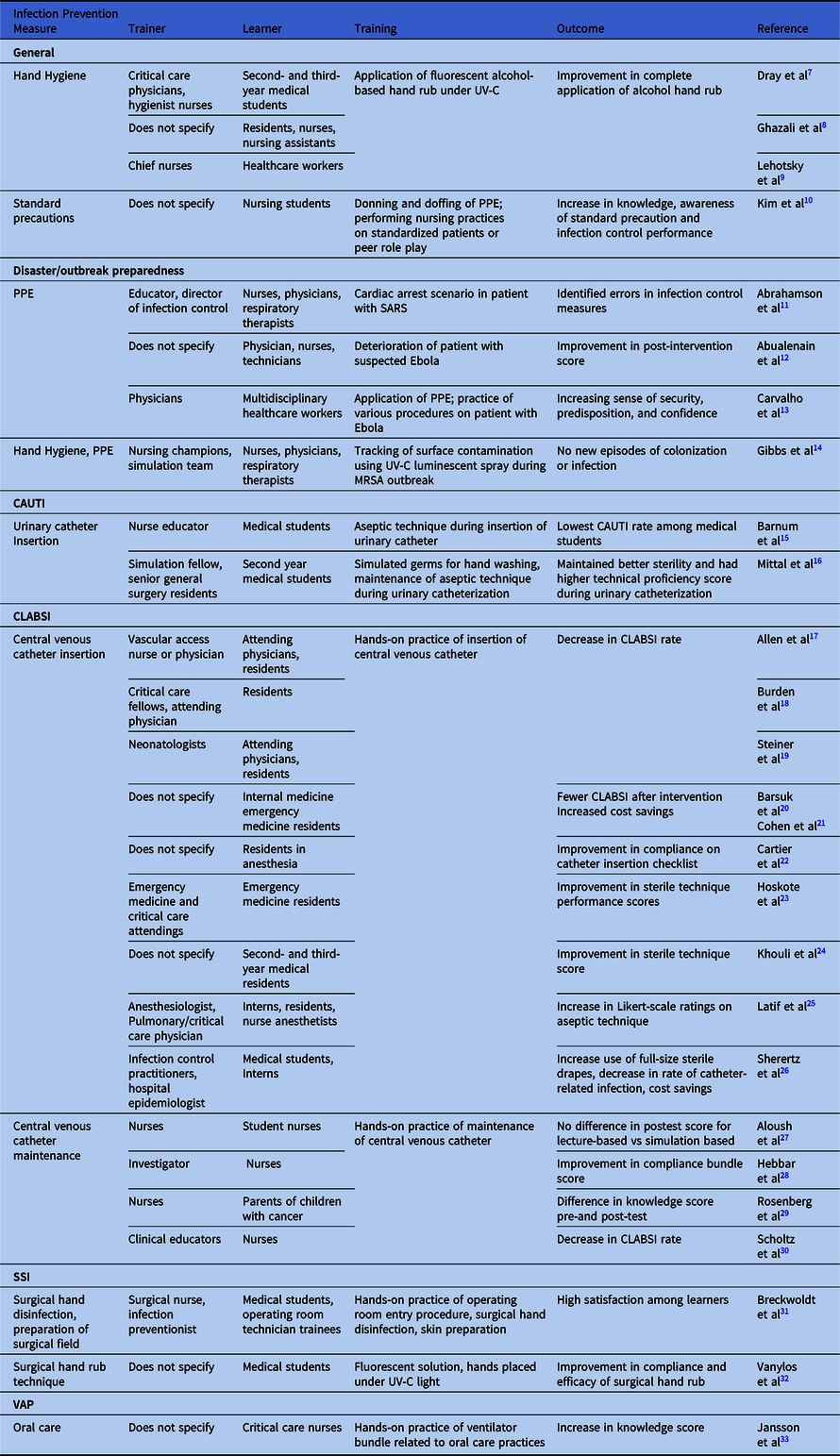
Note. UV-C, ultraviolet C; PPE, personal protective equipment; SARS, severe-acute respiratory syndrome; MRSA, methicillin-resistant Staphylococcus aureus; CAUTI, catheter-associated urinary tract infection; CLABSI, central-line–associated blossdstream infection; SSI, surgical site infection; VAP, ventilator acquired pneumonia.
Trainers included the following: physicians in 8 studies (30%), nurses in 7 studies (26%), infection preventionists in 3 studies (11%), and simulation center staff in 2 studies (7%). Learners included the following: residents in 10 studies (37%), nurses in 9 studies (33%), medical students in 7 studies (26%), and physicians in 5 studies (19%). Nursing students, technicians, and respiratory therapists made up a minority of learner types.
Furthermore, 3 studies focused on SBT for hand hygiene using the application of fluorescent alcohol-based hand rub under ultraviolet C light with all studies demonstrating improvement in complete application of alcohol hand rub. Reference Dray, Lehingue and Valera7–Reference Lehotsky, Szilagyi and Ferenci9 In addition, 3 studies used SBT to recreate clinical scenarios pertaining to suspected Ebola and severe acute respiratory syndrome (SARS) cases Reference Abrahamson, Canzian and Brunet11–Reference Carvalho, Castro and Leon13 with identification of errors in infection control measures, Reference Abrahamson, Canzian and Brunet11 and improvement in both postintervention scores Reference Abualenain and Al-Alawai12 and learners’ sense of confidence. Reference Carvalho, Castro and Leon13 Also, 13 studies utilized SBT for CLABSI prevention, and 10 studies focused on aseptic technique pertaining to central venous catheter (CVC) insertion Reference Allen, MIller and Nicholas17–Reference Sherertz, Ely and Westbrook26 with improvement in sterile technique Reference Barsuk, Cohen and Feinglass20–Reference Aloush27 and CLABSI rate. Reference Allen, MIller and Nicholas17–Reference Steiner, Langgartner and Cardona19 We identified 4 studies that focused on CVC maintenance Reference Aloush27–Reference Scholtz, Manoachino and Nishisaki30 with improvements in compliance in bundle usage Reference Hebbar, Cunningham and McCracken28 and decrease in CLABSI rates. Reference Scholtz, Manoachino and Nishisaki30 We identified 2 studies that utilized SBT for Foley catheter insertion Reference Barnum, Tatebe and Halverson15,Reference Mittal, Morris and Kelz16 with improvement in sterile technique Reference Mittal, Morris and Kelz16 and decreased CAUTI rates. Reference Barnum, Tatebe and Halverson15 Finally, 2 studies focused on SSI prevention with surgical hand washing technique and preparation of the surgical field. Reference Breckwoldt, Knecht and Massee31,Reference Vanylos, Peto and Viszlai32
Discussion
SBT is underutilized in infection prevention, but it can serve as an important adjunct to traditional educational tools. It can target learners ranging from students to nurses, physicians, and other ancillary staff. SBT programs in infection prevention can vary widely from disaster preparedness of high acuity to low-frequency clinical scenarios to day-to-day infection prevention measures. SBT can improve learner’s sense of competence and confidence, Reference Abrahamson, Canzian and Brunet11–Reference Carvalho, Castro and Leon13 increase patient safety through improved compliance in infection prevention measures Reference Mittal, Morris and Kelz16,Reference Cartier, Inan and Zingg22–Reference Sherertz, Ely and Westbrook26,Reference Hebbar, Cunningham and McCracken28,Reference Vanylos, Peto and Viszlai32 and increase in knowledge, Reference Rosenberg, Terhaar and Ascenzi29,Reference Jansson, Syrjala and Ohtonen33 improve HAI rates, Reference Barnum, Tatebe and Halverson15,Reference Allen, MIller and Nicholas17–Reference Barsuk, Cohen and Feinglass20 and reduce healthcare costs.Reference Cohen, Feinglass and Barsuk 21
Simulation modalities can offer a realistic imitation under test conditions. Different simulation modalities and environments are classified as low fidelity, medium fidelity, and high fidelity, with the highest fidelity modality or environment most accurately representing the real environment. Various simulation modalities have been integrated into infection prevention efforts, each with its own advantages and disadvantages (Table 2). Task trainers (low-fidelity simulators) have been predominantly utilized to help learners practice specific psychomotor skills such as aseptic technique in the insertion of central venous catheters Reference Allen, MIller and Nicholas17–Reference Sherertz, Ely and Westbrook26 and indwelling urinary catheters. Reference Barnum, Tatebe and Halverson15,Reference Mittal, Morris and Kelz16 Standardized patients, which are real people portraying the role of patients, have been utilized to practice standard precautions and interpersonal skills. Reference Kim, Kim and Kim10 Virtual reality (high fidelity) has also taught healthcare personnel to safely don and doff PPE, Reference Ragazzoni, Ingrassia and Echeverri34 as virtual reality help learners to gain knowledge on the proper process of a procedure in a scalable fashion. In prior outbreaks, mid- and high-fidelity manikins, which are full-body manikins, were utilized to mimic patient encounters with rare communicable diseases like Ebola and SARS, aiding in the identification of errors in infection control measures. Reference Abrahamson, Canzian and Brunet11–Reference Carvalho, Castro and Leon13 These simulators can replicate a patient’s physiology modeling through the programming of vitals, breathing, or other patient presentations. They enable a team to work collectively to deliver care (eg, intensive care unit setting with in full hazmat suit) while performing a certain set of procedural tasks (eg, intubation) in a physical environment. This enables teams to practice not only individual skills, but also critical teamwork and communication skills.
Table 2. Simulation Modalities
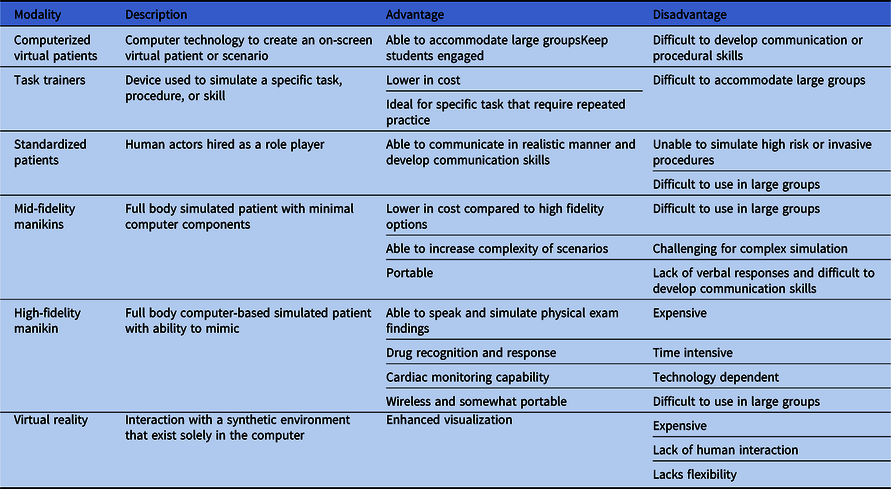
Ultimately, simulation experts match the learning objectives to the most effective modality. For effective learning, SBT should be offered as part of a curriculum to supplement and complement other educational methods with clearly defined objectives and benchmarks for learners to achieve. The program should provide individualized and team learning and should allow for repetitive practice with clinical variation such as varying levels of difficulty if feasible. Expert trained facilitators should provide feedback during or after a learning experience through rapid cycle deliberate practice or debriefing, based on learning objectives. Reference Al-Elq35
SBT in infection prevention has predominantly focused on central venous catheter insertion and maintenance with various studies reporting significant improvement in compliance with sterile techniques and decrease in CLABSI rate. Reference Allen, MIller and Nicholas17–Reference Scholtz, Manoachino and Nishisaki30 However, despite its proven effectiveness in CLABSI prevention, SBT has remained underutilized in other realms of infection prevention. Through repetitive and deliberate practice to develop procedural competence and immediate constructive debriefing by an expertly trained debriefer, SBT can allow for standardization of routine infection prevention measures and proper implementation of evidence-based prevention strategies to reduce HAI rates. In addition, SBT can play a role in understanding and optimizing workflows and bottlenecks in high-acuity, low-frequency encounters for disaster preparedness. Centralized SBT that promotes competency-based education can yield a large return on investment by reducing overall healthcare costs through improved quality of care, reduced HAI penalties, mitigation of readmissions, and decreased lengths of stay. Reference Cohen, Feinglass and Barsuk21 This study demonstrates the benefits of SBT in an expanded role in infection prevention teaching and argues for continued innovation.
In summary, SBT is underutilized in infection prevention but can serve as a crucial educational tool. The coronavirus disease 2019 (COVID-19) pandemic has exposed our inadequacy in infection prevention training as healthcare personnel train on the job in high-risk clinical environments. SBT can bridge this gap and improve compliance with infection prevention measures through repeated education in standardized teaching sessions in a safe environment by reinforcing best practices and personal accountability.
Acknowledgments
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.




