Overview
Chapter 1 argued that the way in which bodies and body parts have been obtained for medical research and teaching creates three core forms of dispute. These have incrementally (and sometimes sharply, as for instance with the NHS Alder Hey organ retention controversy) shaped public understandings of the ethics and practices of medical science and thus the possibilities of, and constraints on, medical research. This chapter analyses the first of our categories: the implicit dispute. An implicit dispute is what happens when a person dies, their body enters a medical research and teaching culture, but informed consent is implied, never documented in full for the bereaved. A lot is therefore left unsaid, and deliberately so. It is normal for these sorts of bureaucratic processes to be very light touch, and to have audit procedures that look robust, but are the opposite. The aim being to make it a difficult logistical task to track at the time, or retrace later, exactly what is happening, or has happened, to human material once it enters a system of body supply. Even an insider might not know who exactly had shared a body and body parts, and what scientific studies these relate to. Those grieving thus never got an opportunity to make an informed choice. They are given the impression at the time of a loved one’s death that informed consent existed, when it did not. Instead, it was often implied, particularly by those staffing large teaching hospitals. In modern Britain, a proper system of consent was an aspiration, not a uniform working practice. As we shall see, implicit disputes thus constituted what modern research scientists would term ‘bio-commons’, and reconstructing their human stories is the central focus of this fourth chapter.
There are many ways in which such disputes can be analysed, but in this chapter we focus (detailing the 1950s and 1960s in particular) on disputes over bodies that became available because of bad weather. A first section explores the connection between foggy weather patterns, the deaths of the poorest members of society and the consequent supply of bodies and body parts for medical research and teaching.1 While everyone may have disliked fog, it was a boon for a medical community needing more research material.2 The chapter then moves on to develop this theme across a number of sections, focussing on the case study of a young boy who died in the ‘Great Fog’ of 1952 and was dissected for teaching and research purposes. Remapping the material journey of his brief life-story and body reveals the extra time of the dead created by the actor network of hospital staff, anatomists, coroners, and scientists. Subsequently, the chapter generalises this individual experience, reconstructing the body supply network for St Bartholomew’s Hospital in London from 1930 (when the New Poor Law ended) until 1965 (when a ‘mechanism of body donation’ was put in place that other medical schools in the capital subsequently copied). The next step in this critical analysis is to expand upon the new data, focussing on a number of representative stories of those taken for dissection and who did not consent to the ‘donation’ process. They ended up being dissected by virtue of being alone, friendless, socially isolated, or they died inside NHS premises where medical research was a priority. The penultimate section compares St Bartholomew’s data to national statistics on ‘body donation’ figures for the whole of England during the 1990s, arguing amongst other things that women come to be the mainstay of the body bequest process, and that current practices for encouraging organ and body donation do not reflect that material fact. The final section thus asks how the implicit disputes that arise out of the covert (if at the time perfectly legal) supply of bodies and body parts for medical research and teaching have shaped trust in medicine and the development of professional boundaries, a theme taken up again at length in Chapter 5. In this way, this fourth chapter builds on some of the core themes of this book, as outlined in Chapter 1, including: notions of expertise, the ambiguities of consent, the rise of the information state, deferential power relations and the particular authority of individual actors in the wider medical science and research community. We begin our engagement with these themes by exploring the medical hazard of fog; in a hidden history of disputed bodies, few could escape the old English weather lore –
Fog – Weather Warning!
In December 1952, The Times newspaper featured a severe weather warning about the harmful effects of a deepening winter fog across the capital:
A ‘LONDON PARTICULAR’
Of all the afflictions which visit the inhabitants of this temperate climate, fog is the most exasperating. There are some who think well of frost or snow, and rain is an undoubted necessity. It refreshes the earth and the air, and at one time was the only decent scavenging system London knew. But there is no decent use for fog. It cripples business and brings even winter sports to a standstill. Fog is a dirty and stifling cloud without any silver lining at all. We could do well without fog. … Fog is altogether too big a job for Science to handle.3
By the 1950s, air-pollution trapped in fog attracted considerable column inches in the British medical press.4 Smog from the constant burning of coal fires in houses, shops and factories across the capital was blighting Britain’s major cityscapes. Newspapers described the daily distress of commuting under a ‘green-yellow miasma’ lingering on London’s streets.5 The toxic haze eventually led to a concerted public health campaign around the time of this ‘Great Fog’, known as the ‘pea-souper’, of 1952.6 Scientists could not, as The Times observed, disperse fog, but it had boons for medical research and teaching. Weather crises such as that in 1952 increased emergency admissions to hospitals and more people died of heart and lung complaints, prompting a synchronicity of greater body supply on the one hand and calls for better medical research on the other hand. Moreover, there was also a deeper history.7 Trading dead bodies in fog, moving them under the cover of darkness, buying and selling at the back of Poor Law infirmaries and workhouses or on the streets of London had been commonplace for centuries. After the NHS was created in 1948, the old welfare institutions of the New Poor Law had become County Council care-homes, and they continued their supply-lines. Still the anatomical sciences waited in wintertime for the Grim Reaper to stalk British cities in the fog. Yet seldom did the scientific community speak openly about this fact of life because of public sensitivities surrounding dissection.
There is no doubt that the dense smog that hung over London at the start of December 1952 was an exceptional weather event, even for the damp British climate. A low, dank cloud covered the capital. It sat stubbornly on top of impenetrable smoke pollution. Out-of-doors everywhere was wet with a cold miasma. Foggy rain dripped from trees and formed a drizzly haze under lampposts. Along the packed streets, passers-by coughed, spluttered and wheezed, to and from work. The Times ran a daily health feature on how to combat colds, sneezes and asthma. They did so because of widespread concern about the high number of extra emergency admissions to large teaching hospitals that had stretched medical services to almost their breaking point. In North West London, Times journalists reported on how Harrow public school pupils experienced a cacophony of illness even though they lived on top of a steep hill, 406 feet above the rest of the capital. Most had contracted sore throats, chest cackles, and high temperatures. Cancelling sports in the foggy conditions meant that everyone stayed indoors in their boarding houses to manage the spread of infection. Tragically, however, the Headmaster of Harrow, Dr R. W. Moore, died aged just 46 during the foggy pall of 1952. His obituary explained that ‘early in 1951 he had an attack of bronchial pneumonia’ and despite being X-rayed and operated on to alleviate his condition, the symptoms returned with renewed vigour in the winter fog of 1952.8 All the pupils at Harrow ‘underwent X-ray examination’, but Moore died of the latest outbreak. The Times health correspondent highlighted that many London residents were experiencing the same severe symptoms of bronchial pneumonia. It was the worst outbreak since ‘the influenza pandemic of 1918’. Civil servants at the Ministry of Health meantime emphasised the virulence of the 1952 pneumonia strain. They warned central government that the peak in mortality rates from fatal lung diseases was akin to the sort of death statistics of ‘the last great cholera epidemic of 1866’.9 A public health report was thus urgently prepared for the London County Council. It revealed that some ‘2,484’ residents in the capital died from a ‘tenfold increase in bronchitis’ in the reporting period from 5 November to 5 December 1952.10 Within days, however, the foggy conditions worsened. Medical science was on hand to treat patients but also to benefit from higher fatalities in its dissection spaces.
During early to mid-December 1952, all of the daily newspapers devoted their front pages to the deepening winter fog that descended over London and would not shift.11 A combination of high pressure, near-freezing temperatures, light winds and thickening smog had intensified the hazardous public health crisis. The Automobile Association told The Times on 8 December 1952 that ‘it is the worst fog they had ever known’. The Daily Telegraph reported on how the dense smog had ‘blacked out central London and a band 40 miles across. … All buses had stopped by 10 p.m. Hundreds of cars were abandoned. … Thousands of people did not get milk.’12 Nightly there was a shutdown of all the capital’s transport systems because bus and train drivers could not see more than 100 yards ahead on the roads or railway networks. Only the underground stayed open, but even underneath London the fog seeped into the drainage system tunnels. Airport traffic-control staff took the unprecedented decision to divert ‘500 planes’ from London Heathrow to Hurn aerodrome in Bournemouth. Few planes could land safely in the capital because they did not have the radar capabilities to guide them blind onto the ground. The ambulance service faced a crisis it could not cope with as well: ‘It took five or six times as long as usual to get cases to hospital’, according to the Daily Telegraph; so bad was it that: ‘… women gave birth to babies in fog-bound ambulances’. Yet, it was the rising daily death toll, disproportionate amongst children and their grandparents, which caused the greatest public concern. In two weeks, ‘some 4,000 died’. The death toll then rose to ‘10,000’ in total by the close of the Christmas holidays of 1952.13 A single case-history from this tragic period – a young boy aged 7 living in the Harrow area and dying in December 1952 – symbolises the central themes of this chapter because we can trace what happened next to his human remains. Out of the medical miasma of fog emerges the material journey, reconstructed from detailed record linkage work on the mechanisms of body donation.
TAB – A Hidden History Remapped
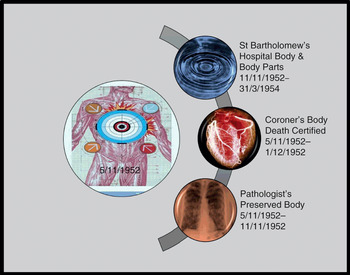
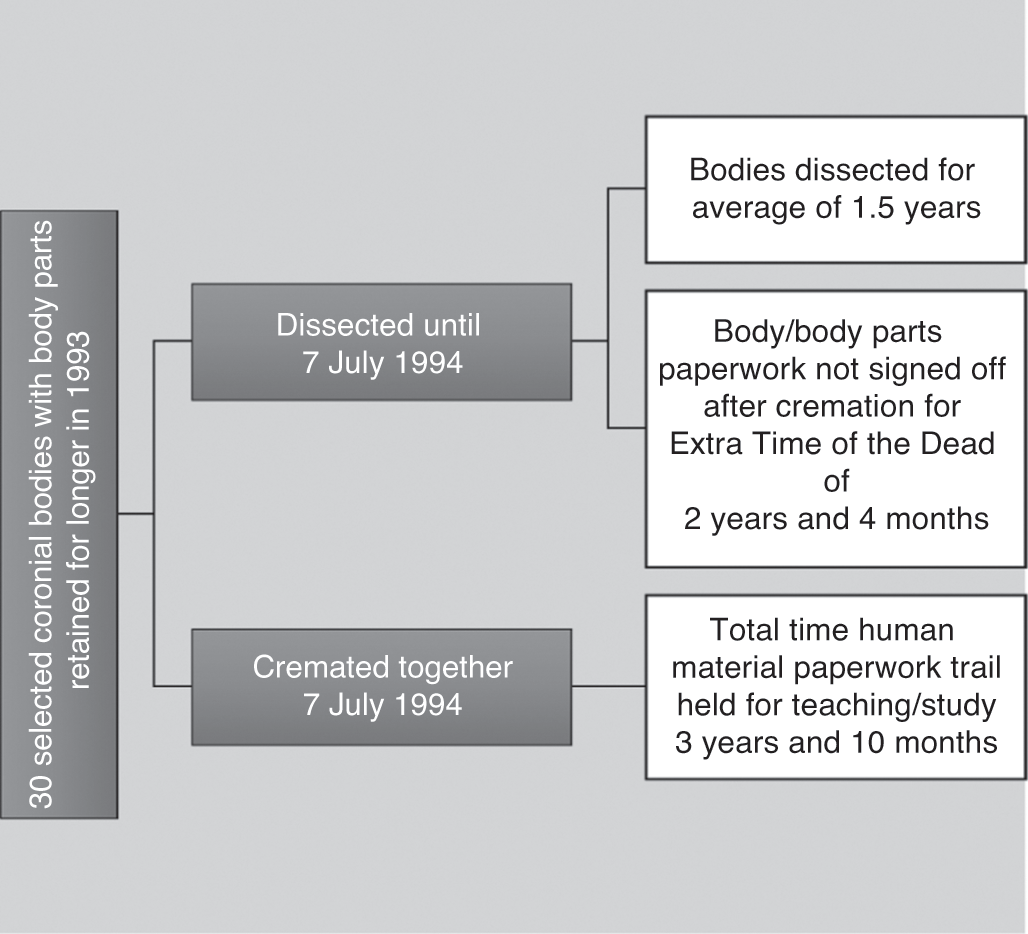
TAB was born in North London at the end of the WWII to parents (Mr WAB and Mrs HAB) who had married in their twenties sometime in 1938.14 They spent their savings on a small deposit to mortgage a three-bedroom house in Hendon. Having rented a property during the first year of their marriage, they wanted stability at home to start a family. Like many of their wartime generation, the ABs did not want to waste time. Their philosophical attitude was that if Mr WAB died at the front, then Mrs HAB would have the consolation of children. In Hendon during WWII, Mrs HAB gave birth to two boys – one in 1941, the other in 1945. She conceived each sibling during Mr WAB’s leave of absences from the armed forces. Detailed record linkage work reveals that whilst the eldest child (RAB) was to survive the ‘Great Fog’ of 1952, his younger sibling (TAB) did not. On 5 November 1952, TAB ‘died from pneumonia’ aged 7 in hospital. Under normal circumstances, once the funeral had been staged at a local church, his short life story would have ended but for the fact that he had died from prevalent pneumonia and his small body was thus a very valuable research and teaching tool for a medical profession facing a deepening epidemic of this deadly disease. Remapping its material journey from emergency admission to dissection and burial reveals the multilayered, hidden histories of a hospital coroner’s case. For the first time, we can trace a series of discrete research steps that were never officially recorded (Figure 4.1) but which go to the heart of attitudes towards body ethics in the immediate post-WWII era.

Figure 4.1 Remapping the threshold points of the dissected body and body parts of TAB, 5 November 1952–31 March 1954.
On the night TAB died, an ambulance transported him from Hendon to Harperbury Hospital near St Albans in Hertfordshire.15 Bonfire Night was a busy time for the emergency services in North London. Yet, this does not explain why a small boy breathing poorly went on a thirty-minute road journey about fifteen miles from home to hospital. There were four logistical issues shaping the local GPs decision-making. These helped to create research threshold points, stage-managed by an actor network of hospital staff, anatomists, a coroner and his pathologist. The first consideration was that out-of-doors most local people walked to and from work with a handkerchief over their face, often covered in a layer of coal dust from London’s dirty air. The ‘Great Fog’ of 1952 would culminate in politicians on all sides of the House of Commons passing the Clean Air Act (4 & 5 Eliz. 2 c. 52: 1956) as a national priority.16 The GP thus judged it prudent to move TAB out of the immediate area of the contagious pollution in Hendon. If air pollution was foul at the top of Harrow hill, 406 feet above London, then it was self-evidently best to remove the patient out of the capital altogether. Even so, a second practical factor shaped the decision-making too.
During WWII, St Bartholomew’s Hospital developed very close links with medical services at Hill End Hospital in St Albans.17 Once the site of an asylum and then re-designated a mental hospital in 1913, Hill End was requisitioned by the Ministry of Health during the Blitz to evacuate as many civilian casualties as was feasible out of central London. Hill End staff and those of St Bartholomew’s thus worked closely together. Medical personnel networked likewise with nearby Harperbury Hospital. In the 1950s, NHS staff continued to co-ordinate as they had done in wartime when the healthcare system was struggling to cope in the capital, as it was during the severe winter fog. Even so, a third logistical problem was a severe ambulance shortage in 1952.18 There was little point ordering a transfer into central London. Its inevitable delay meant TAB might never reach on time the critical medical help he needed at either Great Ormond Street in Bloomsbury or St Bartholomew’s Hospital in the City.19 He headed therefore for St Albans in the ambulance.
A fourth logistical factor was the fact that TAB’s family doctor faced a technical problem. His young patient had a bad attack of pneumonia, but there was a medical supply problem. The Chief Medical Officer (hereafter CMO) for England and Wales highlighted the key issue in the BMJ at the end of 1951:
There is a serious world shortage of x-ray films, due to increasing usage in all countries. In this country, usage during the first six months of 1951 was 16% greater than in the corresponding period of 1950 and was at a rate about 60% greater than in 1947. Production has been expanded and manufacturers have greatly improved their productivity. Nevertheless, it has not been possible recently to satisfy all hospital demands. New plant is shortly to be installed by manufacturers and should afford some measure of relief. Meanwhile, the present difficulties can be eased if all hospitals will exercise strict economy in the use of films and eliminate waste, particularly in processing.20
The CMO stressed that: ‘Economy in film production should not take precedence over the efficient examination of the patient’; nevertheless, it was necessary to ration X-ray films. An NHS directive stated that ‘only experienced clinicians’ were to be permitted to order X-rays in general hospitals. Nobody beneath the rank of a registrar could apportion precious film. In an emergency, the patient would be triaged and sent to hospital premises that had enough X-ray film to manage the critical condition. TAB thus had to journey out of central London to Harperbury Hospital at St Albans.
Once sent farther afield, another NHS stipulation complicated the accident and emergency protocols on 5 November 1952. On the night TAB died, the radiologist on duty was not authorised to X-ray a common condition like bronchial pneumonia just because they suspected its presence in the lungs of a young patient. A consultant on call was the only person who could make TAB’s case a clinical resource priority. The hospital management committee’s attitude was that there was little point in filming a fatal condition which medical intervention could do nothing to heal in a pre-antibiotic era. The BMJ had been critical of radiologists using what it called an ‘omnibus technique’: that is, doing radiology on all suspected cases as a matter of course regardless of the clinical prognosis. NHS resources were scarce and the subject of intense funding debates, straining central-local relations in 1952.21 In the case of TAB, there was an ambulance available to take him to St Albans where a supply of film was available. On arrival, there would be a specialist waiting for him with the authority to order a priority X-ray at Harperbury Hospital. Judged against these logistical criteria, moving TAB out of the Hendon area seemed to offer his best chance of survival. Even so, it is evident that the GP of the AB family had to work with a complex set of resource-allocation shortages on 5 November 1952. They explain why TAB’s body became available for dissection and medical research outside inner London.
On closer inspection of the case files, what cannot be determined from the surviving medical notes is whether (or not) TAB had an underlying medical condition from birth. This may have made him more vulnerable to pneumonia and might provide a further explanation as to why he was sent specifically to Harperbury Hospital rather than Hill End in St Albans with whom St Bartholomew’s had very close working relationships. Harperbury had a long history of treating those defined as suffering from mental incapacity in childhood according to the Mental Deficiency Act (3 & 4 Geo. 5 c. 28: 1913). The categories were:
a) Idiots – Those so deeply defective as to be unable to guard themselves against common physical dangers.
b) Imbeciles – Whose defectiveness does not amount to idiocy, but is so pronounced that they are incapable of managing themselves or their affairs, or, in the case of children, of being taught to do so.
c) Feeble-minded persons – Whose weakness does not amount to imbecility, yet who require care, supervision, or control, for their protection or for the protection of others, or, in the case of children, are incapable of receiving benefit from the instruction in ordinary schools.
d) Moral imbeciles – Displaying mental weakness coupled with strong vicious or criminal propensities, and on whom punishment has little or no deterrent effect.22
The hospital’s typical patient profile also included disabled children born with genetic conditions such Down’s syndrome or cystic fibrosis, impacting on their health profiles, learning needs and schooling proficiency. As one of the hospital’s first medical attendants, Dr H. E. Beasley, explained in Kelly’s Directory of 1937, Harperbury Hospital first opened as the Hangers Certified Institute in 1925. It was located on the site of an old WWI aircraft hangar, and the land was recycled to create a ‘colony for mental defectives’ in the 1930s:
The Middlesex Colony, begun in 1929, was opened on 20th May, 1936, by the Rt. Hon. Sir Kingsley Wood, M.P. Minister of Health. The Colony is intended for mental defectives who are socially inadaptable in the community, or who are neglected or without visible means of support. Male defectives who are capable of being employed are provided with suitable agricultural occupations on the land, or at various industrial occupations in the Colony’s workshops. Female defectives are suitably employed in the laundry, general kitchen or workrooms. Children who are capable of it are given various simple occupations. The patients live in separate ‘homes’ of the villa or pavilion type. The Administrative Centre, consisting of the main administrative offices, dental and surgical clinics, dispensary, central kitchen, reception hall, workshops, laundries, &c. has been built on an axial line running north and south, the Colony buildings for male and female being placed east and west around and overlooking playing fields. An isolated site on the south side is allocated for the children’s section.23
Nursing staff and a medical superintendent lived permanently on site. They supervised the medical cases using a wide variety of diagnostic and therapeutic interventions including art, drama, sport and daily farming activities for residents. The aim was to promote the benefits of occupational therapy for mental well-being. Under the NHS in 1948, the Middlesex Colony was renamed Harperbury Hospital in 1949.24 There was, however, more continuity than discontinuity in its healthcare provision. It often took in mental-health patients referred from the North London area during the 1950s. TAB thus entered a well-known facility for treating physical and mental disabilities in childhood on 5 November 1952, and one in St Alban’s with close wartime associations with St Bartholomew’s Hospital: again circumstances that materially influenced what happened next.
When TAB died on 5 November 1952, official jurisdiction over his material body started to change medico-legal hands. This was a child, the death was unexpected and his body passed from the emergency team to the pathology department but overseen by a hospital coroner. As there would need to be a hospital post-mortem, the cadaver was preserved in formaldehyde from 5 November to 11 November. In these six days, TAB had no official legal status in the public domain. No death certificate was issued. The body did not technically belong to his parents. In property law, it was ‘Res Nullius – Nobody’s Thing’, as we saw in Chapter 2. The coroner with the co-operation of the pathologist now had to establish the cause of death. Ideally, they would do so with the parent’s co-operation to reassure them that the hospital was not guilty of medical neglect. Even so, this was not strictly speaking a legal requirement, and such ambiguities could be misleading for the family involved. Indeed, on closer inspection it is apparent that standard procedures involving this seemingly routine post-mortem were not straightforward in 1952. As Figure 4.2 suggests, step by step TAB’s body and body-parts moved into the jurisdiction of medical science, creating an elongated and hidden afterlife of the body which was not ended until TAB was buried some fourteen months later.25 In his hidden history of the body, there are three noteworthy time gaps from detailed record linkage work. These provide important clues about the research threshold points of medical science’s work on TAB.
Extra Time of the Dead
In the early 1950s, GPs made a number of complaints to the British Medical Association that the NHS seldom informed them officially about the death of one their registered patients on a hospital ward. As a result, there was a lot of concern and considerable confusion about who should issue a death certificate to bereaved families and when exactly a family doctor should do it. In the interim, a bureaucratic space opened up for the medical research community to obtain jurisdiction over the dead for longer than it appeared. The General Medical Committee Conference thus informed the BMJ on 17 April 1954 that to resolve the confusion, from now on: ‘it has been agreed that a letter will be sent … drawing attention to the importance of ensuring that general practitioners are promptly notified of the death or discharge of hospital patients’.26 TAB’s dead body entered this extra time of the dead in its paperwork too, as Figure 4.2 illustrates.
Harperbury Hospital did not issue a death certificate for twenty-six days until their coroner eventually registered it officially on 1 December 1952. This happened at St Albans Registry Office, even though the child had resided prior to death with its parents in Hendon. In the meantime, TAB’s body became a site of negotiation and tension over the professional remit and standing of different groups of actors in the post-death process. We see such tensions clearly played out in early November 1952, just before TAB’s death. A concerned correspondent to the BMJ noted:
Pathologists’ Fees for Coroners’ Necropsies
SIR,-The salaries of the coroners in the County of London have again been increased. Everybody will approve, although the approval of the pathologists who serve them will be mixed with envy. Since the Coroners (Amendment) Act of 1926, the fees payable to pathologists for coroners’ necropsies have not been increased. Are not these pathologists the only group of the community who have had no increase of pay for more than a quarter of a century?
The Committee on Coroners, under the chairmanship of Mr. Justice Jones, has reported to the Home Secretary, but, as a matter of equity, the fees payable by coroners to pathologists should be increased without waiting for the report as a whole to be carried into effect. Cannot the B.M.A. exert some pressure on behalf of the admittedly small number of its members who carry out necropsies for H.M. coroners?27
A matter of days before TAB’s body entered Harperbury Hospital professional disputes were holding up supply-lines of bodies for potential dissection. Disagreements about fees and salaries created the context for generating implicit disputes. Liminal spaces opened up because of the delay in the official process of moving the dead whilst pathologists and coroners argued about the economic basis of their status. In TAB’s case, we can explicitly observe the timeline and time-travels. Slowed down, these created a twenty-six-day gap between death and official registration. This did not mean that the body did not physically move along the chain of command or supply; it did. The crucial point to appreciate is that it had no official status in law and hence did not technically exist for its relatives. If the parents had wanted to object to what was happening to TAB’s remains in the twenty-six-day gap, they would have had no official knowledge to react to. There was no record-keeping for this missing period of almost four weeks. This was commonplace and it created the potential for a series of discrete research thresholds without the full knowledge of the bereaved. Remapping what happened next brings these threshold circumstances into sharper focus.
On 11 November 1952, ‘further examination’ of TAB’s body began once chemical preservation was completed. The hospital coroner deliberately used this legal phrasing because it was permitted by AA1832 and the Coroners Amendment Act (16 & 17 Geo. 5 c. 59: 1926), even though critics like Pearl Craigie had objected to it (unsuccessfully) in 1906 (as we saw in Chapter 3). The same legal framework remained in force and therefore covered the removal of TAB’s body on the morning of 12 November 1952 to the dissection room of St Bartholomew’s Hospital in central London. Listing hospital transfers like this as a ‘B’ (bequest) in the dissection register (generally marked in pencil), was, however, misleading. There is no surviving evidence to suggest that this young body was the result of a written bequest. Paperwork detailing informed parental consent prior to dissection is missing, or it was never created in the first place; alternatively, the anatomist on duty may have been lazy about form-filling and did it verbally, or he was in a rush on the morning of TAB’s arrival and did not do his filing properly at the end of the day. This ambiguity in the bureaucracy is nonetheless informative since it reflects the common way that many bodies were supplied at the time through an implied consent process (as we shall see later in this chapter).
Whatever the paperwork discrepancies in TAB’s case, it is noteworthy that St Bartholomew’s Hospital had been keen to improve its ‘mechanisms of body donation’ after WWII. Records show conclusively that a new scheme of bequests did not get officially under way until 1954 (Figure 4.4). This made it very unlikely that TAB’s body supply involved a full bequest from Harperbury Hospital involving the parents. TAB thus appears to have been transported into central London to be dissected under an older system of supply that did not require explicit immediate family involvement, similar to what happened under the New Poor Law. There was, as we saw above, a close working partnership already established between medical staff working in the St Albans area. This made it feasible and normal for an existing network of suppliers to play a pivotal role in the presentation of TAB’s body to St Bartholomew’s anatomists, following long-established protocols stretching back to AA1832. A commercial transaction in TAB’s case can, however, be ruled out; supply-fees were not permitted by the 1950s. On 1 July 1947, James Cave, Professor of Anatomy at St Bartholomew’s Hospital, ordered that: ‘Payments for injecting subjects was to be stopped.’ Henceforth all such ‘petty cash [was] to be handed to Miss [Dorothy] Woolaway’, Cave’s departmental administrator.28 The old system of paying petty cash fees to Poor Law officials for dead bodies, supplied from infirmaries and workhouses, was phased out.29 At the same time, the wartime practice of compensating hospital staff in St Albans doing chemical preservation work was revised (although actual supply-lines from the same premises renamed under the NHS did continue to the close of the 1990s: a theme we return to below). In the transition, TAB’s body was not a crude commodity as it would have been under the Victorian system of supply. Rather, it was now symbolic of the changeover from the dead-end of the old business of anatomy to modern-day ‘mechanisms of body donation’ organised by hospital staff. The rest of this chapter examines this process in more detail.
Research Recycling
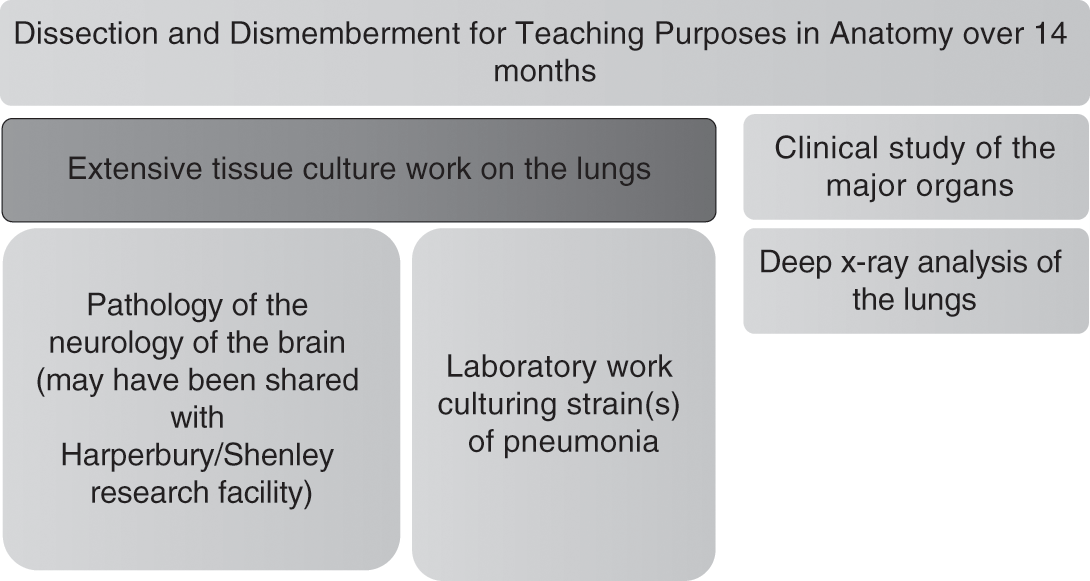
The fate of TAB’s body in terms of medical teaching and study highlights three key threshold points for the ethics of the body. The first is that TAB’s human remains were retained for 14 months in total before burial. That extended time frame effectively meant that the small corpse of a 7-year-old boy was dissected and dismembered extensively. In reality, there would not have been much material remains to bury at the end: less than one third at best. Seldom did doctors, coroners or pathologists explain this explicitly to grieving parents. Few could face such news on the night of a child’s death in hospital. Even if the family had been amenable to a body donation (and again, there is no evidence to confirm this in the record-keeping for TAB), in their initial bereavement their primary concern would have been for the dignity of their young offspring. This would have been a life-changing moment even for the most philosophical of family members. The very fact therefore of doing so much teaching and research on TAB’s human material created the potential for an implicit dispute to be generated. The process of consent was implied, not fully documented; even if it was done in some respect, it was at best ambiguous about all the research and teaching steps about to happen next. The extant evidence therefore points to the material fact that TAB’s parents were not given an opportunity to make informed decisions about their child’s potential to become bio-commons at this threshold point. Today, this is no longer permissible in the dissection rooms of medical schools, not simply because HTA2004 outlaws it but also because teaching facilities have now adopted a voluntary code-of-practice, which states that ‘no more than one third of a “human gift” to the medical sciences will be dissected’ for reasons of human dignity.30 While we must avoid judging past practice by standards which were not in force at the time, these new standard practices help to identify the liminal spaces and research threshold points that were routinely scheduled in case histories like TAB’s over the course of the second half of the twentieth century.
A second threshold for body ethics in the TAB case is the utility of the extensive dissection conducted as it became the focus of further work once teaching sessions on it had concluded. Figure 4.3 traces, through detailed record linkage work, the uses of body parts and tissue. The results are tangible. A 1961 study authored by clinicians working in the wards, pathology department and dissection room of St Bartholomew’s Hospital, and based upon research over the period 1949 to 1958, provided a new analysis of pneumonia. The research team reviewed the cases of ‘1,330 patients, 861 were males and 469 females; 303 were children under the age of 15’ who had all contracted persistent pneumonia. They concluded that typically: ‘some 634 (63 per cent) of the adults and 90 (30 per cent) of the children had a pre-existing disease. Respiratory disorders, particularly chronic bronchitis and emphysema, and cardiovascular diseases were by far the commonest concomitants.’31 Further clinical research led the research team to observe that: ‘In children, associated diseases and pulmonary complications were less common than in adults, but the mortality was high in infancy.’ Using deep X-ray equipment for which St Bartholomew’s was renowned at the time, medical evidence was found that: ‘The bacteriology of the sputum and the radiological appearances were similar to those seen in adults who did not have chronic respiratory diseases.’32 In other words, TAB was one of a number of cases whose lungs had been weakened by pneumonia straining his heart, making him ideal for further medical research study. He had thus been chosen by the hospital pathologist for ‘further Special Examination’ and in so doing he became a small but no less significant part of a medical mosaic that would eventually result in the drive for better precision medicine in the treatment of pneumonia. Yet against this benefit we must set the fact that the threshold points in Figure 4.3 were never mapped by medical science for his parents. Rather, they were kept behind the closed doors of private research facilities. This culture of secrecy was at the very least something that prevented the AB family from understanding the importance of their son for medical research, helping them to make some medical sense of their young son’s death.
A final threshold for body ethics is also highlighted by Figure 4.3. TAB’s brain was a valuable teaching and research tool even before it left Harperbury Hospital to travel to St Bartholomew’s on 12 November 1952. As we have seen, the Harperbury Hospital was at the forefront of occupational therapies to combat childhood learning disabilities and mental ill-health in the early 1950s. The hospital’s medical records are not sufficiently detailed to reconstruct whether parts of TAB’s brain may have been sliced and retained for research in-house, but nor can that possibility be ruled out either since it is noteworthy that clinical studies of brain matter happened regularly on site. It is conceivable in TAB’s case that his brain became a ‘control’, that is, retained but not sliced extensively. Equally, it is well documented in the extant records that childhood epilepsy was a feature of extensive brain research at Harperbury, with a particular focus on ‘hemispherectomy’. This method involved the removal of part of the brain, sometimes up to half in cases of severe epilepsy, on the basis that neurons in the young retain a neuro-plasticity to repair successfully after major invasive brain surgery.33 Known as ‘anatomical hemispherectomy’, it was carried out on both the living and the dead on site at Harperbury’s twin-research facility for brain studies called Shenley.34 It would be uncharacteristic of the research culture on site at that time if TAB had not been brought to the attention of the in-house team, either as a ‘control’ or a potential discrete brain-retention. Whatever the neurological circumstances, both at Harperbury and St Bartholomew’s, the actor networks existed since wartime to share in each other’s research priorities. TAB was thus a potential opportunity cost for the medical sciences. His cameo role in medical history illustrates the material fate of many others that entered similar premises, and highlights the process by which implicit body disputes might develop and the complex counter-currents of medical ethics, familial knowledge, openness and closed research processes that shaped the scale and meaning of body supply for research and teaching purposes in the recent past. In turn, we can generalise the lessons to be learned from the TAB case by switching our attention to material contained in St Bartholomew’s Hospital archives. This is where Richard Harrison (from Chapter 3) trained and, tellingly, what some medical students dubbed the Ministry of Offal in the press because it was one of the busiest teaching and research facilities in Britain. Here, we will hence bring to bear an ethnographic approach to the ‘mechanisms of body donation’ employed by the hospital and show how they operated both within the law and negotiated their way through it during the 1950s and 1960s. New data illustrates material afterlives, representative of the lost property of disputed bodies in modern British research.
St Bartholomew’s Bodies
St Bartholomew’s Hospital was a religious foundation first established at West Smithfield in 1123; thus, it is one of the oldest healthcare institutions in Britain.35 For almost nine hundred years, it has occupied a pivotal place in the heart of the City of London. On its flank stands the City Livery Companies near the Bank of England in Threadneedle Street along Lothbury, where many of the world’s leading finance houses are still located today. For centuries the hospital took in the dispossessed and sick poor, those often blighted by the hurly-burly of financial markets, sometimes bordering on the criminal that Punch exposed to ridicule in Victorian times. The courts of the Old Bailey were thus symbolically located just a short jaunt across the road from the hospital, which was within easy walking distance of St Paul’s Cathedral. Standing opposite the hospital gate was Smithfield meat market, too. Few missed the annual fair staged nearby. Strangers, passers-by and residents all came to enjoy the entertainments at the hospital’s King Henry VIII gate, erected in the Tudor period. After the dissolution of the monasteries, St Bartholomew’s survived the turmoil of the Counter-Reformation to emerge by the eighteenth century as a voluntary hospital with a long-term commitment to treat the sick poor from its endowments. This entailed embracing science and promoting a culture of teaching and research. That raison d’être spearheaded the expansion of medical education in the nineteenth century, so much so that St Bartholomew’s became the fourth-largest teaching facility in Britain by the close of Queen Victoria’s reign in 1901. Yet, for every new medical student recruited, there needed to be a constant supply of dead bodies to dissect. London’s destitute supplied the dissection table and thus helped to bring medical education at this famous hospital into the modern era.
The Medical Act (21 & 22 Vict. c. 90: 1858) stipulated that anatomical education was mandatory for every doctor. By the time those legal processes were extended in 1885, it was also a statutory requirement that each trainee should dissect a minimum of two cadavers (either whole bodies or enough body-parts to constitute two complete anatomies). This had to be done over a two-year anatomical teaching cycle at a designated teaching hospital like St Bartholomew’s, in order to qualify for general practice, surgery or midwifery. There remained, however, tensions over whether bedside training on the wards or research at the laboratory bench was the best way forward for a modern medical education. This tension was not resolved until after WWI when a redesigned curriculum tried to ensure that ‘medical education had a direct impact on clinical care’.36 As Keir Waddington explains, the ‘gap between science and the bedside had been bridged’ as a priority by WWII; nonetheless, ‘debate continued over the nature of academic medicine’. Waddington elaborates that by the early 1950s: ‘If science had been accepted as an integral part of a doctor’s training, old divisions between clinical and pre-clinical study were challenged as uncertainty grew about the location and content of training.’37 In many respects, dissection was at the centre of these ongoing debates because St Bartholomew’s had been extensively bombed in the war and its teaching facilities needed rebuilding to be world leading again. The NHS after 1948 tended to be slow about repairing this wartime damage, but committed staff pushed ahead to better integrate anatomical teaching with more specialised research facilities into the curriculum once more. Looking back, despite the problems of regeneration, many who worked on the premises in the 1950s recalled ‘golden years, with a sense of ever-expanding horizons’.38
Studying the dead in detail in this period is feasible because of the remarkable longevity of the accurate record-keeping at St Bartholomew’s Hospital. It has one of the best-documented archives in Britain and remains committed to sharing its past histories. Using such material, Figure 4.4 shows that 1,072 bodies were supplied for dissection from 1929, when the New Poor Law ended, until 1965. This reflected an organised network of suppliers. Four observations set in context the acquisition of these bodies and the implied system of consent that kept it functioning. The first observation is that the end of the New Poor Law had an immediate impact on the supply of the destitute for dissection from asylums, infirmaries and workhouses. As this author has documented elsewhere, on average St Bartholomew’s Hospital had been able to acquire at least 50 cadavers each teaching year from the time of the passing of the AA1832 until 1929. Indeed, in the early years of the new legislation, supply levels had peaked at 70 per year. A total of just over 6,000 bodies (from around 60,000 generated across the capital as a whole) were bought from the dead-houses of Poor Law institutions to the hospital in the period 1832 to 1929.39 In other words, St Bartholomew’s share was a minimum of 10 per cent of the entire system of body trafficking in the capital. Since these figures represent just whole bodies, another 10 per cent should be added for trades in body parts too. The latter were always more profitable because more money was made from the corpse broken up into piecemeal transactions. St Bartholomew’s trading figures were thus never less than 20 per cent of the dead of London until 1930. The system functioned because generous petty cash payments persuaded people in the employ of body dealers to co-operate. It became a well-organised business of anatomy and the dead were a commodity that medical education expansion relied on.
This deep history matters, both for the interpretation in Figure 4.4 and the subsequent issues around body ethics in the twentieth-century. St Bartholomew’s had a lot of go-betweens in its employ to make this trafficking in the dead operate efficiently each night. It was commonplace for a so-called ‘undertaker’, really a body dealer, to be employed by the dissection room. That disguise hid the fact that they were buying and selling corpses on the London streets. Once the New Poor Law ended, all of these trading arrangements had to be renegotiated, and this took time. Consequently, St Bartholomew’s trading position went down from 70 bodies in 1929–30 to 52 bodies by 1934–5, a loss of nearly 20 per cent. The dissection room staff then put a lot of effort in 1936–7 to try to improve supply-lines again, but they could not prevent them dropping by another 10 per cent to around 40 per year by 1937. By the start of WWII, these figures had stabilised to about 45 bodies each teaching cycle, but it was more difficult to maintain supply-lines in the Blitz once more people evacuated out of London. Putting this trading activity into its broader perspective, the 1939–40 supply-rate was just 64 per cent of the supply levels there had been in 1929–30. This was a crucial 36 per cent reduction overall at a time when medical student numbers were expanding. When Richard Harrison (see Chapter 3) signed up for a new medical career in 1939, he was unaware of this supply problem. It never featured in the recruitment literature sent out to prospective students. As the 1930s had been a very difficult economic decade after the Wall Street Crash, everyone inside the medical profession assumed that the dead of the destitute would be available in large numbers due to startling poverty levels (as they had been in late Victorian times), but this was not the case. Subscriptions to burial clubs run by trade unions and small co-operative societies provided the means to bury the dead and hence alleviated the stress of those subsisting on the threshold of relative to absolute poverty.40 This meant that St Bartholomew’s relied on a much narrower range of former Poor Law institutions, many of which became County Council care-homes for the aged, for its regular supply needs.
A second observation is that during WWII supply levels dropped sharply. This supply pattern matched that of WWI. Those medical students, like Richard Harrison, evacuated out of London to study at Queens’ College, Cambridge, together dissected no more than thirty bodies per year for the duration of 1939–45. It was thus much more common to dissect parts of bodies rather than whole cadavers over a two-year training cycle. This sets in context Harrison’s recollections of daily tensions in the dissection room about when to turn a body over to make sure everyone got a chance to do an anatomical procedure. In other words, dissection was piecemeal and this reflected the fact that men recruited into the armed forces died abroad in greater numbers, rather than at home in poorer parishes where they had traditionally been sold on in death. The majority of dissections during the war were therefore on the aged. Middle-aged women did not tend to feature in the dissection registers because they had vital war work in munitions factories, took on more childcare responsibilities and were generally nursed at home even when seriously ill because of their value to the makeshift economies of the labouring poor. In terms then of calculative reciprocity, women until their 60s continued to be cared for by their kinship networks. Only those worn out by a life of hard work, aged, friendless and lonely would eventually come into the purview of the ‘mechanisms of body donation’ supply-lines of St Bartholomew’s.
This situation did not improve in 1945. Until 1954 and the introduction of a new body bequest drive, supply-lines were under pressure, such that just thirteen bodies were acquired in the teaching year of 1953, and this despite the high death toll in the ‘Great Fog’ of 1952. At no time in the entire history of dissection had supply-lines been as difficult to sustain. Even under the Murder Act (25 Geo. 2 c. 37: 1752), supply-lines were relatively buoyant compared to this.41 Anatomists indeed often complained that the murder rate did not keep up with demand from medical students whose numbers increased sixfold; nonetheless, AA1832 resolved this situation. In the meantime, supply-lines nationally tended to be on average fifteen a year from 1752 to 1832. In the capital, however, by 1800 supply-lines were much worse than in provincial England: they peaked at seventeen a year in 1815 in the provinces compared to just three bodies per year in London. This meant that St Bartholomew’s in 1953 found itself with a very old supply problem more akin to that of the early nineteenth century than one normally associated with modern medical research in the standard historical literature. It meant that bodies like TAB took on a symbolic importance and a lot of use was made of them, as we have seen.
Finally, it is evident from Figure 4.4 that the introduction of a body bequest scheme from 1954 had an important effect, bringing supply to about 30 per cent of its early twentieth-century peak. During the 1960s, students at the hospital would have had access to around thirty corpses each teaching cycle. Yet, this is only a partial picture because there were also important changes to the composition and character of the bodies supplied, as further detailed record linkage on individual cases reveals. They illustrate epidemiological trends. In other words, we need to compare TAB’s material journey (from pneumonia death to dissection on into further research cultures) which was happening in parallel with other medical research activities at the time. It is important to examine these too because otherwise we will not gain a comprehensive enough historical picture about how a system of implied consent operated, the motivations driven by underlying disease trends, and thus nosology factors potentially shaping research priorities inside the actor network of anatomists, coroners and pathologists working together.
When each new body entered the dissection room, there was an important opportunity for the staff on duty to check the death certificate, which was often inaccurate. They stated the proximate cause of death, that is, the last ill-health episode the person died of. These were not reliable in terms of epidemiological trends in the general population because each GP would not have necessarily known the outcome of a detailed post-mortem. The poor were often signed off as ‘heart problems’, ‘diseased’ or ‘dying from neglect’, for instance. And, thus, expensive post-mortem costs were saved. Anatomists therefore as a matter of course always conducted their own autopsy before commencing teaching. They re-checked the pathology of death and arrived at a more accurate underlying morbidity result. This having been done, that then raised the possibility of doing further medical research on the body, its parts, organs and tissue in question. In Table 4.1 we thus see in the left-hand column the common certified causes of death before they underwent autopsy in the dissection room. In the right-hand column are listed the common ways that anatomists assessed the underlying potential for further medical research once they had arrived at more accurate morbidity results. In this way, staff on duty were able to identify a range of complications and to follow an enhanced set of research and teaching priorities. Thus, when the dead body of a male aged 70 named CD arrived on 25 March 1950, what appeared to be death due to a combination of mental and physical degeneration reflecting ‘decline in old age’, on closer examination proved to be caused by ‘tubercular enteritis’.42 CD had lived in abject poverty and died in the old St George’s Workhouse Infirmary on Mint Street in South East London. The medical premises, even in the 1950s, were still in use. The NHS occupied them to treat some of the most vulnerable residents of Southwark, a parish traditionally linked with high levels of death in Victorian times. Today, this association with typical disease patterns of endemic poverty continues, since ‘gastrointestinal and peritoneal tuberculosis remain common problems in impoverished areas’.43 Presentation of the disease TB in the abdomen has always been very difficult to diagnose. Even so, it is often present in the urban, elderly poor. Before the introduction of laparoscopy, it was hard for doctors to see the bacterium growing in the GI tract (in the ileocecal area, the ileum and the colon); in virulent cases, any area of the gut might be infected. Generally, it is still connected to poor immune levels (notably in HIV patients), but in the past tended to be a reflection of economic patterns of deep social deprivation and diseases associated with consumption.
| Death certification date(s) | Disease classification(s) | Potential for research |
|---|---|---|
| 1930–65 | Diarrhoea, Mental & Physical Degeneration | Old Age, Dementia & Decline |
| 1945–50 |
| Heart Attack Prevention |
| 1950–55 |
|
|
| 1955–60 |
|
|
| 1960–65 | Cerebral Haemorrhage |
|
CD was, therefore, typical of the sorts of bodies still generated for dissection at St Bartholomew’s from long-established links to the basic healthcare facilities of the New Poor Law. The dissection register states CD’s retention for teaching and research purposes lasted from 25 March 1950 until the start of 1951. In nine months, every opportunity was taken to culture the strain of ‘tubercular enteritis’ in the abdomen area, and to do further research on major organs including the heart and lungs. As with TAB, medical students cut up CD extensively. Eventually Robert Hogg (a so-called ‘undertaker’, really body dealer) buried what little remained. Hogg, according to the dissection accounts, also selected bodies from Guy’s Hospital too and took them to the Examination Hall if he thought they would be useful specimens for students’ oral tests. CD appears to have been one such case, and since the records confirm his destitution, this typical profile matches others in the sample size. It is likewise informative that the taking of his body from St George’s Infirmary was part of an implied process of consent from many other similar institutions because he was friendless in death. There was nobody to dispute what was happening except the infirmary staff, and it was not in their interests to upset a network that by the 1950s was deeply embedded into a chain of body supply that stretched as far back as 1834 when the New Poor Law was established. Nobody therefore searched for CD’s far relatives to check on his last wishes; although ethical standards at that time did not require this, the inaction does reveal a lot about questions of loneliness and autonomy in death, and the potential for implicit body disputes.
We often think that the current healthcare crisis in loneliness is a recent social phenomenon, but it occurred often in the early 1950s. In fact, the social anthropologist Geoffrey Gorer wrote in Exploring the English Character (1955 edition) about how ‘most English people are shy and afraid of strangers, and consequently very lonely … especially in old age’.44 Anatomists therefore deployed that social situation without fear of official censure. Indeed, the Lancet in one of its most forward-looking editorials in 1949 forewarned, ‘The plight of old people is one of the [sic] biggest and most embarrassing problems facing the National Health Service.’45 That fact of life was a boon for the medical sciences, as many similar entries to CD in the dissection books confirm. Indeed, it is feasible not only to retrace the three discrete thresholds in his case (teaching, heart-lung research, culturing tubercular enteritis) but also to reconstruct other ‘undertakers’ that were used to bury what little remained at the end of life because a tally of those who doubled up as body dealers was kept, as Table 4.2 shows. Many worked for New Poor Law institutions. Most stayed on the staff when premises were renamed, transferred to the NHS. The records facilitate therefore the opening of the door marked ‘KEEP OUT – Private!’ highlighted in Chapter 3.
Table 4.2 Undertakers that buried dissections from St Bartholomew’s Hospital, 1930–1965 (including those in the employ of Guy’s Hospital)
| Undertaker | Trading premises | Hospital supplier |
|---|---|---|
| Merett & Son | 519 Hackney Road, NE London | St Bartholomew’s |
| R. Hogg | 30 St George’s Road, Southwark London | St Bartholomew’s & Guy’s |
| • Burials at East London Cemetery Plaistow | ||
| J. Gaulborn | 61 Greyhound Road, Hammersmith London | St Bartholomew’s |
| J. Field | 183 Blackfriar’s Road, SE1 London | St Bartholomew’s & Guy’s |
| • Burials at East London Cemetery Plaistow | ||
| J. Kenyon | 45 Edgware Road, Paddington London W2 | St Bartholomew’s |
| • Burials of Roman Catholics | ||
| Askton Brothers | 252 Clapham Road, SW9 London | St Bartholomew’s & Guy’s |
| • Burials at East London Cemetery Plaistow | ||
| E. Napier and Sons | 157 Lancaster Road, Notting Hill W11 London | St Bartholomew’s |
The system of supply therefore afforded dignity and respect in death, and did so across religious denominations, but equally the network of body dealers disguised as ‘undertakers’ that facilitated a system of implied consent stretched across London, with some longevity. In the next section, we therefore explore this hidden history of the dead in further archive detail, because the historiography has tended to lose interest in the dead at burial – failing to appreciate that to get to burial could involve a complex medical research culture of pathways still to be mapped materially.
May-Die! Mayday! Mayday!
Disregarding such privacy notices personified by Table 4.2, it is notable how many healthcare institutions listed in the St Bartholomew’s dissection registers had close links with the New Poor Law. Often these premises were recycled under the NHS, continually hidden from public view. Some key examples stand in for many at the time and illustrate the sorts of network suppliers generated that made a complex system of implicit consent function over time inside the modern system of supply. The Mayday Hospital situated at Thornton Heath in Croydon did this on a regular basis.46 For appearance’s sake it was styled the Croydon Union Infirmary and then renamed the Mayday Road Hospital in 1923. This was because in an era of widening democracy, voting rights had to go hand in hand with better healthcare provision or else welfare facilities looked like an empty political promise to ordinary people. By the time that the Croydon Corporation took over the premises in 1930 and then the NHS absorbed the local healthcare infrastructure in 1948, it seemed that the Mayday Hospital had embraced the modern era of universal medical provision. Yet, many local people did not see it this way. For despite the careful rebranding of the hospital under the NHS, its popular name was the ‘May-Die Hospital!’ So sensitive were the local NHS health committee to this slur of medical negligence that eventually the premises were renamed the Croydon Hospital to sever all associations with social deprivation and poverty. Even so, this did not stop St Bartholomew’s lobbying for body supply there in the 1950s. Thus, when a 76-year-old female died in Mayday Hospital on 3 October 1956, her body went to St Bartholomew’s at 10 a.m. on Thursday 4 October 1956. The patient had died from a ‘cerebral haemorrhage’ and the body was retained over 20 months for teaching and brain research until 7 July 1958. It was again buried by Hogg, the ‘undertaker’ and body broker go-between.47
This case in many respects is intriguing because of its mundane conclusion, despite a number of curious features. It resulted in a dreary death and disposal, representative of many examples in the dissection registers. The female named EF had a Jewish birth name.48 Yet, it was a cultural taboo in the Jewish community to delay the burial or cremation of the dead for more than twenty-four hours. Ideally, the interred body would be intact. The woman lived, however, at the time of her death in a Church of England home for retired deaconesses located at Staines near Heathrow airport. The balance of the evidence suggests that this association with the Anglican faith made donation feasible. Even so, the body was not marked with a ‘B’ to indicate a written bequest in the dissection register. The female in question was respectable, but poor. It was common for care-homes of the elderly to offset funeral fees by agreeing to donate bodies in return for the medical school bearing the costs of burial or cremation. There seems therefore to have been an implied assumption in this case that handing over the body was conventional, given the deceased’s relative poverty. Besides, if EF’s orthodox faith had been strong, it is unlikely that she would have been retained for twenty months without her Jewish family’s consent. Perhaps she gave such consent herself verbally and willingly, with the paperwork not processed properly. Or her ‘donation’ was implied from her modest personal circumstances and carried out by the care-home to save money. Whatever the motivation, Hogg buried EF at East London Cemetery in Plaistow, which was some considerable distance across the capital from her last place of residence in West London and far from the Jewish cemetery at Kensal Green. There does not therefore seem to have been any further family involvement by her Jewish kin. Here we glimpse someone connected to an Anglican community, amendable perhaps to the ‘gift’ of the body, but for whom the end-of-life experience was not so far removed from the friendless dead-end of others less fortunate than herself such as CD. Death was not just a common denominator; it could be a social leveller too. Determining who entered the system of implied consent often involved something as simple as slipping beneath everyone’s social radar out of reach in old age, a situation that the Sutton and Croydon Guardian reported on even as recently as November 2013. Today, Croydon University Hospital (CUH) still faces insufficient staffing levels, substandard cleanliness and long waiting times in accident and emergency, affecting the elderly; for, according to a newspaper investigative journalist: ‘CUH is not officially stated as the worst hospital in London but it is the most complained about earning the misnomer The May-Die, referring back to its former name Mayday Hospital before it was renamed University College Hospital in 2010.’49 In hidden histories of the dead, such repeated scenarios are noteworthy. They suggest considerable longevity, little chance to dispute what was happening with regards to implied consent, and a system that was all about recovering a welfare debt in death. Others who equally were perceived as a burden to taxpayers entered the same supply chain too.
Perhaps one of the most interesting features of the body supply to St Bartholomew’s in this period is that many cases came from former asylums and prisons. They thus encapsulate a central dilemma in modern medical research – namely, the exploitation of the unfortunate for scientific gain. We saw this criticism in Chapters 2 and 3 during the 1950s when articles and letters published in the medical press expressed ethical concerns about how to protect with legislation those suffering from anxiety, depression, and more serious mental-health conditions like schizophrenia. Some patients consented to drugs trials they could not comprehend fully, since informed consent was very difficult to monitor in the mentally vulnerable. The standard approach in the historical literature to this sensitive issue is to tally up all of the premises of incarceration that were involved in body-supply schemes, mapping their geographical alignment to assess the business of anatomy on a regional basis. Yet in the modern era, that geo-approach could be misleading. What really mattered to modern medical research was not just the physical location of potential bodies, but the over-laying of hidden histories inside medical spaces of incarceration. It was possible for a patient to enter a mental health establishment for general treatment, for instance, and then get caught up in the dissection system by virtue of how research pathways had accumulated inside the premises over time. One representative case illustrates how this worked in detail.
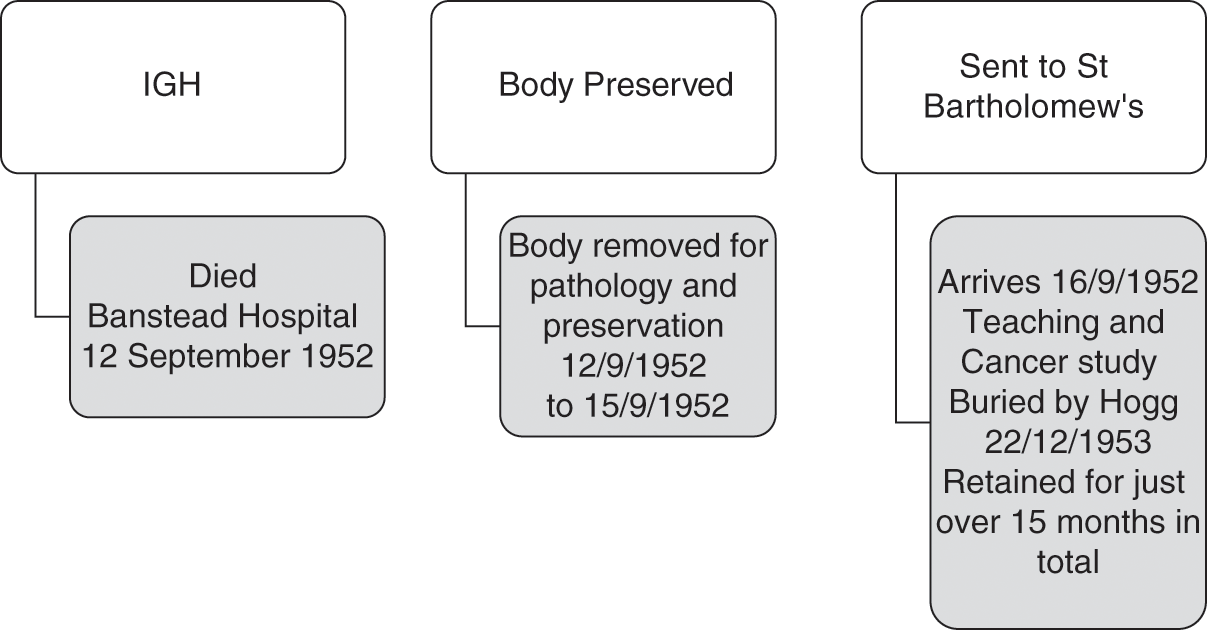
Thus, IGH was a 68-year-old female who died on 12 September 1952.50 She resided in a relatively affluent area of Notting Hill in London. Her home was grade-II listed and faced a garden square of some architectural merit. She was not therefore the sort of person that one would expect to end up on a dissection table unless she had agreed to a body bequest in her will, which does not seem to have been the case. So, how did she come into the medical purview of St Bartholomew’s? IGH had taken a decision to enter Banstead Hospital in Sutton towards the end of her life. She had contracted cancer and needed specialist nursing care.51 This institution, however, had a complicated healthcare history layered with meaning for the dissection system of supply. This IGH seems to have been unaware of in its entirety, but it did nevertheless have a bearing on her destination in death. Banstead Asylum first opened in 1877 with the capacity for 1,700 patients (615 males and 1,075 females).52 It was one of three asylums in Middlesex. The premises remained open to ‘mental defectives’ (broadly defined) under the New Poor Law until WWI. However, from 1889, Banstead came under the jurisdiction of London County Council. By 1912, it was a site covering 200 acres. On its 130-acre farm, patients did occupational therapy and learned self-sufficiency. After the war, however, with so many men returning from the trenches suffering from shell shock, institutional rebranding was commonplace. The premises became Banstead Mental Hospital. In 1937, it was restyled again as just Banstead Hospital, and it transferred to the South West Metropolitan Hospital Board under the new NHS by 1948. Various NHS reorganisation schemes from 1974 until the 1980s preceded its eventual closure in 1986. Often described as a ‘lost hospital of London’ its hidden history in the 1950s proved to be relevant for IGH’s body.
After being requisitioned during the war, by the start of 1950 the military had packed up and left Banstead Hospital.53 It once more became a civilian facility under the NHS. The bed capacity was now ‘2,599’, but in 1951 a decision was taken to designate the premises as a Regional TB Unit too.54 Here men that had contracted persistent TB, and were psychiatric patients, were treated. The female wards on the Unit also contained ‘21 typhoid carriers who were constant excretors’. Often standard treatments had failed to stem their contagious conditions. There were likewise a small number of ‘dysentery carriers’.55 A decision was taken to designate its 15 wards (each with a maximum of 60 patients) with special areas of clinical responsibility ranging from TB, epilepsy, typhoid, dysentery, VD, senility to surgical and psychiatric care. There were also ‘special rooms for disturbed patients’. An additional logistical issue was a ‘chromic shortage of nursing staff’ in the early 1950s. It took time to refurbish the wards to attract more specialist and general nurses, and, in the meantime, the plan was to open a new Clinical Psychology Unit from 1953. Once opened, art and social therapies were introduced. Treatments for persistent mental ill-health included: ‘leucotomy, deep insulin coma and ECT’. In 1951 the TB Unit for men was expanded to house 100 patients and surgical interventions were introduced such as ‘pneumo-peritoneum, pneumothorax and phrenic crush – or with chemotherapy, using a cocktail of streptomycin, PAS and INAH’. The antibiotic era had arrived at Banstead.
When IGH entered Banstead Hospital in the late summer of 1952, therefore, she came into premises deeply committed to the most modern research. Up to fifteen research pathways existed inside the hospital wards run on clinical research lines to facilitate better specialist medical work in-house. This also connected to external research facilities like those of St Bartholomew’s. IGH was not thus simply a lady suffering from terminal cancer; she had a patient profile that matched research pathways of some longevity and reflecting clinical priorities. Moreover, her cancer was clearly not ‘simple’. Even after extensive dissection her cause of death was described as ‘secondaries [sic] of carcinoma’. Evidently, the primary tumour was not found, and this, allied to the fact that she was in late middle age, but not elderly, seems to have made her an interesting subject for further cancer study. Indeed, St Bartholomew’s had an excellent reputation for cancer treatment in this period, and so she was an ideal body supply.56 In practice, IGH’s time travels were not dissimilar to TAB’s when we map her hidden history, as Figure 4.5 shows. In a period of low supply, the hospital was thus taking what it could get, but equally when it did have an opportunity to self-select the bodies chosen, these matched its research focus.
One final feature of the complex network of institutions that underpinned the St Bartholomew’s dissection registers is that there were increasingly very close links between this institution and the hospice movement in London. These started around 1948. One representative example involves IJ, aged 66, who died from ‘carcinoma of the stomack [sic] on 6 December 1948 in St Joseph’s Hospice in Hackney’.57 Located on Mare Street, it still treats the terminally ill today. It was established in 1905, and the Ministry of Health recognised the dedicated work of the nuns by 1923, officially designating St Josephs ‘a home for the reception of advanced cases of TB’. During wartime, the patients and nursing staff evacuated to Bath, and on their return in 1945 extensive bomb damage had to be repaired. Across Hackney, the nursing staff took in those needing end-of-life care, and they soon expanded by developing close links and clinical studies with Cicely Saunders, renowned for founding the St Christopher Hospice from 1958. The ethos of St Joseph’s Hospice has always been to help the poorest and dispossessed in society regardless of their religious belief, and this very much reflected its location in Hackney, the third-most-deprived area of London.58 Unsurprisingly perhaps it has always had close links to St Bartholomew’s, the main hospital for the sick poor in central London serving the East End. Thus, when IJ died on 6 December 1948, her body was retained by the hospice for an initial post-mortem and then chemical preservation until 19 December 1948, a time gap of thirteen days, before being sent to St Bartholomew’s for dissection. Once there, again teaching and cancer research were the features of the discrete research steps taken, with ultimate body burial some twelve months later. This was the same supply pattern occurring with KL, aged 82, who died in a hospice in Bournemouth on 14 December 1952, arriving at St Bartholomew’s to be dissected and diagnosed with ‘carcinoma of the colon’ by the anatomist on duty, some three days later.59 On this occasion, because KL had expressed a wish to the hospice to have a Roman Catholic burial, J. Kenyon, the ‘undertaker’, took charge of the internment after a total of some fifteen months of teaching and research on 7 July 1953.
Meanwhile, another major source of supply at this time was Salvation Army hostels. Thus, when MN, a male aged 56, died of ‘hypertension’ in a Salvation Army hostel on 20 May 1953, his last known address had a direct impact on his body going to St Bartholomew’s, where he arrived on 26 May 1953.60 It was studied until buried by Hogg in a multiple grave on 29 December 1954. The case was not dissimilar to OP, a male aged 85, ‘whose last place of abode was Whitechapel Infirmary’ when he died at Leavesdon Hospital on 1 December 1960.61 This was a deprived area of London where the Salvation Army were very active in rescuing the homeless found in dire straits on the streets and placing them in whatever former Poor Law premises where available close to death. Thus, OP was moved on to St Bartholomew’s within three days; his death from ‘myocardia degeneration’ was common but his body and body parts were still worth studying until 3 January 1962. Buried in a batch of six bodies in a common grave, there was little to inter at the end. This more extensive use of the human material reflected the much more detailed pathology from the 1960s in the dissection registers. At that time in 1963/4 when the scribe who wrote up the entries changed hands, the bodies became a surname in capital letters and just their initials. The clinical discourse of the medical sciences was being streamlined once more, and the ‘gift’ of the whole person disappeared into discrete research steps whose human identities were gradually downgraded to a summary in the record-keeping. The modern era of clinical research was now looking towards a more sophisticated biomedical future, and this extended the potential for an implied system of consent to be generated and re-generated, especially amongst the homeless of London. To engage with that context, it is essential now to track forward in the record-keeping to the 1990s and examine in our penultimate section the scale, scope and clinical reach of anatomical records on a national basis.
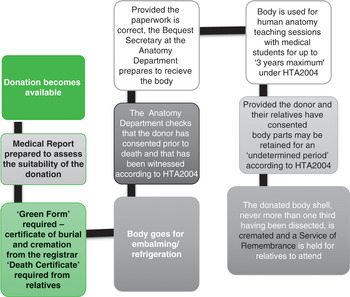
A National Picture – Remapping Donation and Dissection
The NHS public enquiries into organ retention that were the catalysts for HTA2004 established three things that are important for understanding the national scale of the implicit system of consent and its potential for body disputes by the 1990s. The first was that hospital coroners were crucial to the supply mechanisms of medical schools post-WWII. The second was that the need for high-tech pathologies on organs, body parts and tissue cultures complicated issues of consent by grieving relatives. The third was that even those amenable to donation had little material sense of what actually happened to each cadaver divided up in the name of medical science. One predominant issue was that detailed record-keeping had effectively lapsed during the 1980s because AA1984 did not reflect adequately the rapid pace of biotechnology. At the same time, the transplant era had begun and the scientific parameters of innovations, like drug-rejection therapies, were changing the course of research agendas inside the scientific community. In subsequent chapters, we will be engaging with this new biotech landscape in more detail, but before doing so, it is essential to try to understand the nature of dissection work in the recent past. The aim in this section is to examine the scale of the system of implied consent across England, and thus reflect historically on how many people could have been involved in disputing what was happening. Although some of the bereaved may have been in agreement, others might not have been; in fact, few got an opportunity to make that informed choice. Figure 4.6 thus provides an overview of rates of body donation around the country in the 1990s from figures made available by the Anatomy Office. This data is also displayed in Figure 4.7, with locations and rates of donation itemised for individual institutions in London. Then these figures are broken down again into annual rates of donation for all medical schools, and summarised in terms of regional versus metropolitan trends across Britain in Table 4.3.
| Medical school | 1992 | 1993 | 1994 | 1995 | 1996 | 1997 | 1998 | Total(s) |
|---|---|---|---|---|---|---|---|---|
| REGIONS | 100 | 465 | 435 | 352 | 343 | 471 | 339 | 2505 |
| Birmingham | 0 | 5 | 14 | 13 | 12 | 14 | 14 | 72 |
| Bristol | 3 | 17 | 22 | 22 | 17 | 20 | 19 | 120 |
| Cambridge | 7 | 65 | 33 | 50 | 36 | 45 | 39 | 275 |
| Cardiff | 11 | 47 | 55 | 20 | 29 | 46 | 38 | 246 |
| Leeds | 10 | 47 | 22 | 18 | 33 | 48 | 41 | 219 |
| Leicester | 6 | 35 | 35 | 25 | 22 | 42 | 21 | 186 |
| Liverpool | 20 | 52 | 44 | 42 | 45 | 41 | 19 | 263 |
| Manchester | 9 | 38 | 32 | 26 | 29 | 48 | 15 | 197 |
| Newcastle | 5 | 19 | 30 | 20 | 21 | 18 | 11 | 124 |
| Nottingham | 8 | 44 | 49 | 43 | 44 | 55 | 39 | 282 |
| Oxford | 4 | 24 | 31 | 18 | 13 | 21 | 2 | 113 |
| Sheffield | 8 | 40 | 47 | 26 | 26 | 50 | 52 | 249 |
| Southampton | 9 | 32 | 21 | 29 | 16 | 23 | 29 | 159 |
| LONDON | 77 | 212 | 208 | 225 | 210 | 311 | 225 | 1468 |
|---|---|---|---|---|---|---|---|---|
| Charing Cross Hospital | 10 | 19 | 21 | 16 | 40 | 46 | 29 | 181 |
| King’s College | 7 | 25 | 21 | 18 | 17 | 29 | 36 | 153 |
| QMWC* | 12 | 29 | 33 | 46 | 30 | 47 | 33 | 230 |
| Royal Free Hospital | 0 | 6 | 0 | 0 | 0 | 0 | 0 | 6 |
| St George’s Hospital | 13 | 37 | 35 | 33 | 13 | 33 | 23 | 187 |
| St Mary’s Hospital | 9 | 16 | 19 | 18 | 16 | 17 | 0 | 95 |
| UCL** | 9 | 27 | 27 | 24 | 22 | 41 | 33 | 183 |
| UMDS*** | 17 | 53 | 52 | 70 | 72 | 98 | 71 | 433 |
| Totals overall | 177 | 677 | 643 | 577 | 553 | 782 | 564 | 3973 |
* QMWC = Queen Mary and Westfield College London
** UCL = University College London
*** UMDS = United Medical & Dental Schools of Guy’s & St Thomas’ hospitals London including Royal Dental Hospital of London (all merged again into King’s College post-1998)
Considered in the round, we can see that although London dominated the dissection scene in terms of the economies of scale that an institutional collaboration, like UMDS, could acquire (involving the United Medical & Dental Schools of Guy’s & St Thomas’ hospitals, London including Royal Dental Hospital of London – all merged again into King’s College Hospital post-1998),62 the capital overall generated 1,468 bodies (42.4 per cent), but provincial institutions generated more cadavers (2,505; 58.6 per cent). Training in London was no longer the guarantee of a better-supplied anatomical education that it had been in the previous 200 years. We also, however, need to engage with the demography of this supply picture because younger bodies have always been prized by anatomists over older ones. Figure 4.8 analyses the age range of all ‘body donations’ in the 1990s and shows that the majority were in the 50- to 100-year range. This narrows again on closer inspection. For in the age range(s) 70–79, 1,067 bodies were donated; at 80–89 years-old it was 1,802 bequests; and even in the 90–99 age category there were 702 cadavers acquired. Perhaps the most surprising outcome is that 51 bodies were aged 100 or more, roughly equivalent to the 49 for those in the 50–59 age range and proof positive of the crisis of ageing affecting the modern NHS. Medical students today dissect the elderly just as much as, if not more than, their Victorian counterparts.
Delving deeper into the demography of dissection is informative. If we break down the figures again by gender as well as age, as in Figure 4.9, there is evidently not a normal distribution. What becomes apparent is that 2,113 bodies (53 per cent) were generated from females dying between the ages of 50 and 84 years of age. Fewer women were dissected in the 85+ category. If, therefore, a medical student needed to dissect someone younger in the 1990s, that would have been a woman who had died in or near the standard retirement age in force in this decade. This was the exact reverse of historical trends over the previous 200 years when men, not women, dominated the dissection table.63 After age 84, men start to be dissected in much higher numbers than women during the 1990s, when the former generated 1,860 bodies (47 per cent) in the data-set, with the majority being in the 84 to 94 age range. The interesting point about this trend is that the medical students who recalled doing dissections from the 1940s up to the 1980s (see Chapter 3) remembered dissecting very old men, but not women. In the 1990s, therefore, a key cultural transition occurred with females supplying dissection. There appears to have been enough bodies to devise a screening process to select women over men, unless, that is, they were in the upper-age deciles. In other words, against the backdrop of general agreement at the various public enquiries into organ scandals in the NHS, which generated implicit disputes because so many of the general public were misinformed or uninformed about their Coronial remains, it is evident that it was a female voice that was lost in medical ethics during the 1990s. Medical science, which has been a male-dominated profession, relied on women for its teaching and research culture at that time, but then denied them full knowledge of the ‘gift relationship’ they had sustained.
This trend has had other important consequences too, especially for organ donation. Public health campaigns to increase organ donation have tended to target the mass media in a manner akin to shooting arrows at a target, the aim being to hit anywhere on the pool of public opinion regardless of its cultural impact. Had it, however, been better understood that women, rather than men, were more inclined to bequest by the 1990s, then public money spent on speaking to a female constituency with the most take-up rate in body-donations could have been more productively spent. Indeed, the latest NHS2020 strategy to improve donation rates admits that:
The problem is with family consent (or, in Scotland, ‘authorisation’) rates, which have remained unchanged at about 57% for many years. This means that every year, about 4,099 organs are ‘lost’ because, when a person dies, their families refuse to allow their organs to be removed. The target in the 2020 strategy is to increase family consent rates to 80% by 2020.64
In other words, there is little point in encouraging people to join the Organ Donation Register (ODR) alone. In death, what really matters at the point of bequest is talking beforehand about the need to give in families: ‘In order to achieve the 80% target it is necessary to also leverage the ODR so that new joiners go on to have conversations with their family about their wishes in the event of their death.’ As the ODR2020 strategy explains:
For the first time, NHSBT will thus attempt to achieve behaviour change among donor families as well donors themselves. This will require a major cultural shift throughout the UK. NHSBT will need to tackle common myths and misunderstandings around organ donation (particularly as it relates to burial or cremation). Moreover, it necessitates that families appreciate that this is a decision that they will be asked to take, discuss it in advance and come to view donation as a natural and positive step in the grieving process.65
Yet, the rediscovered evidence is clear and robust. First, it is women, and not men, who have been the chief source of communication about the need to be active donors in families. Second, that important observation is based on national dissection data, which confirms that from the 1990s females have been the active givers. The ODR2020 strategy therefore currently maintains (erroneously) that to target young people and get them to effect the most change is the way forward in families. Instead, the social reality is that mothers and grandmothers are key and this social policy finding arises out of the most recent ‘gift’ data available in modern Britain. ODR2020 is moreover concerned that: ‘Between April 2012 and March 2013, 2,918 families were asked for their consent to recover organs from their loved ones. Of these, about 43%, or 1,242 families, refused.’ It goes on to comment that ‘this figure is high, particularly when compared to other European countries, for example in Spain, fewer than 20% of families withheld their consent’.66 That being the case, it is vital to get women talking to shape family decisions, not men; and to do so in terms of ethnicity because up to 68 per cent of families still refuse to donate in communities of higher net-migration.
When we therefore neglect hidden histories involving implicit disputes, it can have very real consequences for a patient on a waiting-list for an organ transplant. Dissection and its discrete research steps have remapped all our medical futures in ways that we still need to engage with and talk about openly to improve the NHS of tomorrow. Under Prime Minister David Cameron, a Behavioural Insights Team was established and staffed by economists based in the Cabinet Office. Their behavioural economics policy promoted an agenda of: ‘If you want people to do something, make it easy.’ Easy that is, from the policy makers’ point of view. Their modus operandi was to ignore hidden histories of the body and instead create legal changes to ‘tax collection, organ donation, and energy efficiency – and most notably pensions … where participation … dramatically increases when people must explicitly opt out, if they are not be automatically enrolled’.67 This ‘psychological realism’, however, talks at people not with them; it lacks patience and creative imagination to find robust data to establish the appropriate historical course of action based on what we know, rather than on what we think we know. Political short-termism has failed to engage with the wider cultural meaning of death and dissection for everybody and, in particular, female voices in British society. If we do not properly model what was happening inside modern medical research cultures, then we can so easily define death in a way that is out of date – an issue that the final section turns to.
Defining Death – Out of Date?
There is one last and important aspect of these national figures that merits closer inspection, and it is disease classification. Before we begin that analysis, however, it is important to appreciate that the entire data-set for the 1990s has a number of curious features that are only discernible when tabulated. The first of these is that the medical terms used to describe the pathologies of death are rather old-fashioned and outdated. They resemble the sort of medical language used in the 1890s. Why this still occurred regularly by the 1990s is difficult to pinpoint with precision. It appears to reflect just how slow medical discourse is to change. Most anatomists and their pathologists doing dissections and post-mortem work in the 1990s trained just after WWII when an older nomenclature was in vogue in medical education. A Victorian vocabulary seems, therefore, to have survived much longer than one would expect in the record-keeping of anatomy departments. This also means that the pathologies of death were in themselves often a missed opportunity to learn more about the underlying causes of death from bequests in the 1990s, a theme we will be expanding on in Chapter 5 when we look at the work of the Coronial Office in more depth.
A second curiosity is that because these descriptions of death in the heart/lungs/brain are rather general when one analyses them from the vantage point of those used in emergency room medicine today, the older terminology looks confusing. Often one ‘mode of death’ seems to overlap with another. Hence, these descriptions of death in the anatomy records do not reflect how a doctor in general practice would certify death in the NHS. The system that they use is very different (as was briefly explained above). Doctors are required to certify ‘the cause of death’ (its pathology, if known) but not the ‘mode of death’ (the part of the body that actually failed). They do so by filling in a number of official categories on the death certificate, as follows:
1 (a) what finished the patient off?
1 (b) what was (a) due to or as a consequence of?
1 (c) what was (b) due to or a consequence of?
2 what other signs of pathology may be associated with the cause of death?68
Thus by way of example if a patient dies of
1 (a) Acute Left Ventricular Failure – in the heart as it became strained
1 (c) It was caused by bone cancer (primary cause)
2 The patient had type 2 diabetes complicating their pathology69
There is then a lot of potential disparity between doctors’ death certificates in the NHS and those of anatomy departments dissecting inside the same system. This common situation is further complicated by the fact that in London, coroners (who liaise with GPs, the police and bequests) tend to be doubly qualified – that is, medically and legally qualified – whereas in the regions, coroners still tend to be solicitors who hold a Diploma of Medical Jurisprudence. For this reason, the requirements of the Registrar in different Coronial areas will have subtle differences. Historically, therefore, there has been a tendency for descriptions on death certificates to be more lax in the regions compared to metropolitan areas, a trend that continues in the NHS. In other words, the system of death certification and disease classification ought to be streamlined, but it is not, and this has contributed to a system of presumed consent that was implied by insiders eager to get hold of bodies to know more about their real death causes. There are, in other words, many gaps, and a lack of uniformity in disease causation as determined in dissection spaces. So, although a lot of research was significant, anatomists co-operating with scientific studies, it could also have been much more streamlined if the system of death certification had not been convoluted and complex. This is a core theme we will be returning to throughout this book because there were lots of lost research opportunity costs caused by a system that functioned with so much ambiguity, and deliberately so, to keep up its supply chains.
Thus, for reasons of statistical significance, the disease classifications from the 1990s data-set have been grouped around the top ten big killers (as described in the record-keeping). These are detailed in Table 4.4. Each of the major categories comprises a mixture of proxy dates – that is, deaths in which pneumonia, for instance, was the final killer or a heart attack, but causation was actually a complex combination of underlying conditions and real causes of death. According to that data, almost 20 per cent of people died of bronchopneumonia, which indicates clinically people who were dying from multiple health complications. In other words, the various pathology categories if used today would have a lot of clinical overlap. In a typical heart attack patient, by way of further illustration, certified as dying of Ischemic Heart Disease (IHD), the individual would have also had three ‘modes of death’ that overlapped with IHD, including: Left Ventricular Failure (LVF), Congestive Heart failure (CCF) and Acute Myocardial Infection (AMI). The main underlying causes of the primary ‘mode of death’ and ‘secondary subset’ would have included little physical exercise, lack of mobility due to a sedentary lifestyle, poor nutrition, obesity, asthma and old age itself. Importantly, for the purposes of this book’s focus, these are patients who will have lived longer (often in extreme frailty) with a number of underlying health problems before death, and therefore had longer to consider organ donation and a body bequest as an option.
| Disease classification (biggest killers) | Numbers dissected in the 1990s |
|---|---|
| Bronchopneumonia | 773 cases out of 3973 in total (or 19.45%) |
| Acute Myocardial Infarction | 671 cases out of 3973 in total (or 16.88%) |
| CVA [Cerebral Vascular Accident] | 433 cases out of 3973 in total (or 10.89%) |
| CCF [Congestive Cardiac Failure] | 197 cases out of 3973 in total (or 4.95%) |
| Dementia -Extreme Old Age – Debility | 184 cases out of 3973 in total (or 4.63%) |
| COAD [Chronic Obstructive Pulmonary Disease] | 132 cases out of 3973 in total (or 3.32%) |
| IHD [Ischemic Heart Disease, known generally as Coronary Heart Disease] | 127 cases out of 3973 in total (or 3.19%) |
| Pneumonia – general | 93 cases out of 3973 in total (or 2.34%) |
| LVF [Left Ventricular Failure] | 89 cases out of 3973 in total (or 2.24%) |
| Cerebral Vascular Disease/Stroke | 76 cases out of 3973 in total (or 1.91%) |
| Top 10 killers in total | 2775 cases out of 3 973 in total (or 69.84%) |
Other major killers like cancer brought fewer into the ambit of dissection – less than one might expect given how many cases feature today in the media – 212 cases in total (or 2.26% of the total) in Table 4.5. Cancer broadly defined as carcinomatosis was the eleventh killer listed in the national sample as the ‘primary cause of death’. Again, it is noteworthy for this book’s focus that these patients had much less time to consider bequests, and therefore featured in fewer numbers in the data-set (even allowing for the fact that pneumonia could have been disguising cancer in individual cases). Overall, this would have mattered to teaching programmes and implied opportunities for further research. Whilst anatomists therefore were self-selecting women up to the age of 84, they could not control their disease classifications or background health conditions. This meant that it was difficult to predict bequests that matched research/teaching priorities. Any they did therefore acquire and shared with pathologists at the right time became exigent, a matter to which we return in Chapter 6. Thus, TAB (young body), EF, IGH and IJ (middle-aged bodies) and OP (elderly body) from St Bartholomew’s represent the spectrum of cases nationally sought and harvested for extensive and valuable further work.
| Cancer types | Area(s) of the body | Number(s) dissected |
|---|---|---|
| Carcinoma – general – carcinomatosis | Whole body | 72 |
| Carcinoma – specific areas of the body | Abdomen | 1 |
| Bladder | 9 | |
| Blood | 4 | |
| Bone | 2 | |
| Brain | 7 | |
| Breast | 13 | |
| Bronchioles | 17 | |
| Colon | 12 | |
| Endometrial | 2 | |
| Kidney | 8 | |
| Large bowel | 2 | |
| Larynx | 1 | |
| Lower Hip | 1 | |
| Liver | 1 | |
| Lung(s) | 65 | |
| Oesophagus | 17 | |
| Pancreas | 14 | |
| Prostrate | 23 | |
| Rectum | 2 | |
| Skin | 7 | |
| Stomach | 14 | |
| Thyroid | 1 | |
| Tongue | 1 | |
| Uterus | 5 | |
| Exhaustion following carcinoma | Whole body | 3 |
| Total cases of cancer | 212 |
Another important feature of this epidemiology is that historical longevity is a vital analytical tool when examining disease trends. So, for example, the foundations of lung conditions such as COAD (Chronic Obstructive Pulmonary Diseases) and heart conditions like IHD and LVF were in reality laid in the 1950s, but came to fruition in the 1990s. This was in terms of smoking, a general decline in exercise, the rise of blue-collar jobs, city pollution and the high salt content of diets, as well as brown fat in fast foodstuffs. In other words, when we try to measure the health of the nation from dissection cases, it is always a case of being Janus-like. St Bartholomew’s hence in the 1950s was really managing the remnants of New Poor Law health issues dating from the 1920s. Likewise, when looking at 1990s cases, what we are really seeing is a disease picture of the landscape of early NHS healthcare dating from the 1950s. Thus, by way of example, pollution levels, as we saw in the opening section of this chapter, were considerable in the 1950s for many people and the Clean Air Act (4 & 5 Eliz. 2 ch.: 1956) did not resolve these for some time. Consequently, lung complaints resurfaced in the 1990s. In fact, what complicates this epidemiology is the advent of car pollution that replaced coal fire smog, and has been a worse killer than, say, cigarette smoke or chimney pollution because one cannot always see car pollution to walk away from it.70 Most demographers faced with these sorts of everyday car pollutants would therefore ask a key question of the underlying statistics, namely: Are the rates and concentrations of the causes of death random in the population?
The answer is negative for both data-sets, either at St Bartholomew’s or in the national sample-set. It is a case of thinking very carefully about what the statistics are really saying, because they were the material basis of the system of implied consent and its research thresholds that we have been mapping for the first time. Examining the males in the sample base is instructive in this regard. At first glance, it looks like the anatomists were selecting by gender – this would explain why women up to the age of 84 appear so frequently in the dissection records but not their male equivalent. After 85 years of age, the number of men rises disproportionately (as we saw above). However, this was not simply about an aged-related screening programme. It reflects another social care explanation too. Men came from care-homes because they outnumbered women in social care provision during the 1990s. Historically, in fact, women have always been able to care for themselves for longer at home than have men. In poverty studies we see this continuity stretching back to the Old Poor Law of the eighteenth century.71 In other words, body bequests, donation rates and their gender profiling continue to rely on a basic understanding of life-cycle trends and their social care crisis points. Anatomists took what they could get, but equally they worked with what they had always known over the past 200 years. And, as they did so, what they began to do was to elongate how long they could keep hold of a body, a theme that we began to explore above and which is developed at length in Chapter 5. In this process, many questions were unasked or unanswered: Who decided what bodies and body-parts were worth keeping and what should be discarded? What got missed in this filtering process? Did access to certain research material shape medical breakthroughs and exclude other options? How did professional boundaries play out in matters of authority over the body and body-parts? And what role did financial budget setting play in remapping the ‘Human Atlas’? We will be continuing to ask these thought-provoking questions throughout the rest of this book, reflecting more broadly on them in the conclusion in particular.
Conclusion
Science and technology diminish the body’s mystery, employing a discourse of instrumentality and utility to which, from a practical standpoint, it is often difficult to object. And yet there is something disturbing in this emerging consequentialist strand in discourse about the body. Non-economic values are unlikely to enjoy prominence or protection in the law’s haste to take the body to market.72
One of the main scientific outcomes of the Enlightenment is that we have all become bodies of information in a global biotech age. This is the logic of medical proficiency and its flourishing research cultures around the world. Few would want to go back to the threats of famine, plague and war that blighted so much human endeavour for centuries.73 Even so, the medical threat of a worldwide pandemic has become a lived experience as this book goes into press, as things that people faced in the past are becoming very real in the present. We know to follow the science, but equally we have to keep checking on its working practices and ethical credentials as they evolve. When commodification is the primary mode of exchange in contemporary society, the law cannot always protect our physical vulnerabilities in a Genome era, whether alive or dead. There is a loophole in international law that fosters the breaking of medical boundaries, but it has seldom been discussed in relation to body disputes. In order to arrive at a consensus in, for example, the United Nations Security Council, all member states agree to comply with the principle of qui tacet consentire videtur [s/he who is silent, is taken to agree]. In diplomatic parlance it is known as the silence procedure of international law – speak up, and be heard; otherwise, it will be taken that silence means acquiescence and a tacit agreement.74 Although scholars have concentrated on the implications of property law for body disputes in case law, in reality the equivalent and precedence of a silence procedure of international law has been, often, deployed inside the ‘mechanisms of body donation’. The public never said anything about bodies being moved around and retained for up to thirty-six months, and that silence was assumed to have created a consensus in Britain. Added to which, we increasingly live in a social media world with a complex sense of community and belonging.75 At a time, therefore, of increased loneliness in modern society, there has been little detailed knowledge of just how much the medical sciences relied on our cultural disaggregation (however benignly) to foster a flourishing research culture from behind the dissection room door. Few got the opportunity to see the editing done in the name of medical progress, how the whole became piecemeal. As Halewood elaborates:
The conversion of the body into patentable information and the speed with which that information is processed and transferred effect a postmodern, technological transformation of the human body that undermines the stability of conventional, liberal legalist assumptions about rights and persons, and about self-ownership and the autonomy it is said to protect. Paul Rabinow … claims that the body is so fragmented by technology, so analysed into a ‘discrete, exploitable reservoir of molecular and biochemical products’, that really no conception of the person as a whole remains beneath.76
This is dangerous ethical territory, the equivalent of being back in the pea-soup of a London fog about to be despatched for dissection in the 1950s. For when we examine the potential for implicit body disputes in the post-WWII era in Britain, what is notable is the law of unintended consequences that follows on from the silence procedure of international law on the one hand and local research and professional practice on the other hand. The medical sciences effectively deployed their powers of acquisition to shape a clandestine culture of research thresholds that had time-gaps (between death and official registration), time delays (for post-mortem and chemical preservation to happen), and time stops (moved from one location to another), before doing morbid pathologies for up to three years before interment. It was easy to lose sight of the whole person divided up and hence bureaucracy literally left them behind, hidden inside the medical research community. TAB, CD, EF, IGH, IJ, KL, MN and OP – are now initials on the pages of this chapter, de-identified for ethical reasons, but also socially revived for medical posterity. They have been put back into research pathways that constituted their ‘gift’ to humanity – for, medical time was a thief that took ‘who that “me is”, or the “you understand” it to be, as the poet Marianne Boruch reminds us in her poem ‘Human Atlas’ that opened Part II of this book.77
Scientists hold that individual contributions and their hidden histories do not change the overall picture of medical progress. But how can we know this for certain about bio-commons, if we have never had the human information to look at properly in the first place? And what happens to us as human beings when we lose sight of each part of a whole story? Thus, Edward Thompson reminded us how the value of social history to science is a renewed sense of our ‘collective conscience’. It ensures we do not lose historical sight of life stories ‘of as many people as possible and as many ways of being in the world’ that represent ‘the complexity and content of human experiences in the past to the readership of the present’, so that medical ethics are the ‘engine of our collective maturity’ (refer, also Chapter 7).78 This again echoes Kwame Anthony Appiah’s recent lecture as part of the Reith Lecture series for the BBC in 2016: ‘Although our ancestors are powerful in shaping our attitudes to the past’ and we need to always be mindful of this, we equally ‘should always be in active dialogue with the past’ to stay engaged with what we have done and why.79 It is still very difficult to be engaged in, for instance, systems biology or the cultural impact of precision medicine in a meaningful way if its research processes are a disaggregated series of discrete research steps never mapped to maintain a sense of human connectedness.80 For when deadlines shift – as they do often with biotechnology – the ‘gift’ recedes, farther and farther from public view. Many insist bio-commons is the price we all pay for medical progress – but it has become one with negative aspects too that require regular historical scrutiny. In organ donation today, we can observe a convincing business case for not acting as we once did in the recent past. Medical science is still miscommunicating with donor families because in neglecting the female demography of dissection in the 1990s, we overlooked a gender bias in the underlying data. Consequently, we have lost sight of misperceptions and misunderstandings that HTA2004 tried to redress but did not necessarily resolve. In Chapter 5, we thus move on to rediscover the pivotal role that the Coronial Office has played in disputing deadlines.
On 6 December 1962, a Daily Mail headline announced: ‘12 People get notes from a Dead Man’. The newspaper article explained how a suicide victim had sent a letter outlining his decision to take his life ‘to his solicitors, his accountant, his bank manager, his next door neighbour, relatives and friends, a coroner and even the police’. Mr Herbert Jones, aged 77, resided in Southcliffe Road in Christchurch, Hampshire. He worked as a Borough engineer for his local council. Shortly after retirement, he was diagnosed with a terminal illness and his note explained that:
The necessity for hospital treatment is obviously becoming more and more imminent. I feel, however, unable to face the liability of causing so much inconvenience to a number of people, especially at this time of year, and so having the firm belief that my life is entirely my own responsibility, I have decided to end it by asphyxia. I am sorry to inflict this on you. … I wish to leave my body to Bristol University for research [sic].1
His neighbour Mr Reginald Wells explained to a Daily Mail reporter that the eloquence of the suicide note was typical of the deceased: ‘He was that sort of man, orderly, quiet and unselfish. He hated being a trouble to people.’ Further police enquiries established that Mr Jones had bought his family home, in which he committed suicide, for his only son. Sadly, the son had died a few months earlier, though the circumstances were not elaborated in the press. Jones had, according to neighbours, been bereft because he faced a double bereavement. His wife had died the year before in April 1961. Like Francis Partridge in Chapter 3, Herbert Jones was unable to cope with the pain of being both a widower and bereaved parent. Diagnosed as suffering from an incurable medical condition, he saw no reason to go on. Grief and memories did not outweigh his rationale that the quality of his life had been fundamentally diminished. An Inquest concluded that suicide was a measured decision. Jones wanted to cause the least disruption to medical staff at Christmas.2 Yet, ironically, the last request in his suicide note was to cause a lot of official consternation. As a Daily Mail reporter explained: ‘Mr. Jones’s last wish – to give his body to science – cannot be granted. The coroner has ordered a post-mortem.’ This simple statement published as a byline to the headline story exposed an explicit body dispute – on twelve prior occasions Jones had expressed in writing his explicit wishes to donate his body to medical research, which the coroner had the powers to countermand. As we shall see, this situation was in fact common because of the longevity of the powers, and ingrained procedural flaws, of the Coronial Office in the modern era: the central focus of this chapter.
Essentially, therefore, this fifth chapter is about these sorts of explicit disputes concerning the power and control over the dead body, body ethics and the boundaries and limits of professional practice, involving the official figure of the coroner. The chapter is thus split into two halves. In the first half we will encounter a brief history of the Coronial Office in England, before then engaging with a series of stories about explicit body disputes involving specific coroners. We will be focussing on the symbolic story of a dead girl called Carol Morris because the circumstances of her harvested human material proved to be very controversial. Her case exemplifies why tracking the material journeys of post-mortem bodies and their body parts matters in hidden histories of the dead. The details are lengthier than others presented so far in this book but that is because it was to be legally a very significant case. Thus, in the second half of the chapter, we explore why one human story is a historical prism for lots of others, and how micro-history can inform macro-trends of considerable longevity. In fact, as we shall see, the Carol Morris case made a significant contribution to establishing the legal precedent of anonymity for all donors in national and international law. Today, this remains in place, and we will be reflecting on the status quo of that standard of medical ethics, since the story behind its legal precedent is not known in the literature.
In other words, we will be asking: Does knowing the human circumstances of such cases change the way we view the ownership of the body once we know more about explicit body disputes, and what exactly were the long-term medico-legal ramifications of these stories that we have seldom thought about in the modern era of scientific achievement because they were neglected in the archives? In order not to dissect the storylines in the way that bodies were dissected and disassembled routinely inside the medical research community, with their human stories subsumed into a bio-commons, we will be looking in a little more detail this time at all the human factors and facets involved in the chosen representative cases. This means that the reader might wish to pause after the chapter’s first half, before discovering in the second half of this lengthier chapter the universal lessons that can be drawn from the newly discovered source material and the reasons for their historical longevity.
Our central analytical focus therefore is the palette and power exercised by coroners once a dead body was in their jurisdiction, despite explicit body disputes that were being generated between medico-legal officials and grieving relatives wanting to fulfil their loved ones’ dying wishes. It is also the case that in a transplant era the technical ability to harvest organs brought the Coronial Office into open conflict with the medical sciences. Historians of medicine have only very recently begun to examine these professional stand-offs through detailed case study, with most accounts still overly reliant on broad brush central government papers.3 Meanwhile, the lack of efficiency of the Coronial Office meant that important evidence about causes of death on coroners’ death certificates got lost inside the systems of forensic medicine and pathology, which should have been a ‘treasure trove of information’. Instead ‘real causes of death’ remained ‘hidden because of indifferent post-mortem examinations’ conducted hastily and which were often ‘obscured by deficient recording of data’.4 That common situation did not come to full public attention until the publication of the National Confidential Enquiry into Patient Outcome and Death in 2006 (hereafter NCEPOD). The National Patient Safety Agency commissioned the NCEPOD report into the professional conduct of the Coronial service because there were serious misgivings about its extensive powers of retention. It concluded that the system of certified autopsies had structural flaws throughout the twentieth century. Paradoxically, the history of explicit body disputes co-ordinated by the Coronial Office was one of many missed research opportunities for biomedicine too. We begin therefore with a short overview of the history of the Coronial Office in England.
Part I
The Coronial Office in Context
The history of the Coronial Office in England is one of slow expansion from the twelfth to early nineteenth centuries, during which the majority of coroners were legally, rather than medically, qualified.5 On average in England, they consistently dealt with about 5 per cent of all reported deaths from the early modern to modern period. Their main official responsibility was to investigate ‘unnatural deaths’ in the community. They did so by sifting gossip, and retrieving any relevant physical evidence at the scene of a death until foul play could be ruled out, or not. Coroners were under legal instruction, however, to wait until a suspicious death was reported to them. They had no official powers to investigate an unusual death. Legislation did not permit them to act just because they suspected that an unnatural or violent act of some description had occurred in their area of authority. Once, however, a suspicious death was reported officially to them and they had retrieved a dead body in their jurisdiction, they had a great deal of discretionary power. They could, for instance, decide how much to cut open the deceased or to leave the body intact. Each coroner could also waive the need for an Inquest if a cause of death in their opinion was obvious at a suicide or the scene of an accident at work or in the home. In this way, Coronial justice was often ‘remade from the margins’ because it involved a lot of discretionary powers of decision-making delegated to individual coroners.6
In suspicious circumstances, coroners have always been required to co-ordinate a ‘view of the body’.7 Normally from the thirteenth to the early twentieth century, this occurred within twelve hours of death. It involved calling a jury to service, composed of up to twelve local ratepayers respected for their social standing. The jury would congregate at a public house or another convenient place such as a gaol room or town hall. Here, a coroner’s assistant laid out the dead and jury members undertook a visual inspection of the deceased, looking for flesh wounds and suspicious bruising. This autopsy meant literally looking at the external appearances during the ‘view of the body’. At it, the coroner gave a verbal report that summarised for those assembled the physical evidence-gathering and general gossip garnered in the community. The jury under the coroner’s direction would then assess the circumstances surrounding the unexplained death and arrive at a verdict before releasing the body for burial. Disinterring bodies after Inquest was rare, even with new subsequent evidence. In the early Victorian era, formaldehyde replaced mummification and alcohol preservation of the body and tissues, respectively. Even so, it was hazardous to hold on to a corpse for long; contamination by contagious diseases, like cholera or diphtheria, was common. The smell of formaldehyde was also difficult to stomach and thus at the ‘view of the body’ chemicals tended to distort lingering synaesthesia impressions. The aim was thus to look quickly and get the body buried as soon as possible. By the 1880s, French morgues were introducing refrigeration techniques, and soon this was copied everywhere across Europe by the early twentieth century.8 Before then, it was vital for English coroners to conduct efficient enquiries in the thirty-six hours after death before the human material started to decompose. Putrefaction devalued human material from a forensic standpoint.
English coroners were under instructions to conduct themselves according to the legal principle of ‘the balance of probability’.9 In other words, provided the available evidence seemed to indicate that a death ‘probably’ looked ‘natural’, then the coroner had the discretion to pass a verdict without the need for an expensive Inquest. In the case of a drowning, this would be a suicide verdict, by way of example. Coroners were not required in law to prove that someone was guilty of causing that death. Nor did they need to abide by the legal stipulation that the accused was innocent until proven guilty in a court of law. Their role was to establish that neither manslaughter nor homicide was suspected, and, if it was, to refer on that serious matter to the local forces of law and order to investigate further and arrest the culprit. In which case, if it looked like a capital charge might go to the Quarter Sessions court, the coroner was duty-bound to ask a surgeon to perform a post-mortem on the dead body and report back to an Inquest jury.
From the 1830s, and following a concerted campaign in the Lancet, coroners slowly started to be medically qualified.10 They also tended to adopt standard post-mortem methods. Generally, this involved making a crucial incision from the neck to the naval, and across the chest cavity.11 An appointed surgeon would handle the heart and major organs, as well as closely examine the brain, for any suspected violent injuries. Coroners might also call additional medical witnesses who had the requisite expertise in, say, the forensics of poisoning to establish a death by misadventure.12 Likewise, an ‘unnatural’ cause of death could have been caused by a stabbing or a drunken brawl that got out of control. In which case, they could call on a medical man with a lot of experience in doing post-mortem examinations for high-profile cases tried at the Old Bailey in London. If subsequently at an Inquest a verdict of ‘murder’ was based on reliable medical evidence, the coroner would refer the matter to the appropriate legal authorities, and the dead person would be buried without further delay.13
The role of the coroner has always involved a very visual method of working. Looking at the surface of the body was important before medical science had X-ray technology, CT and MRI scans. There is therefore a long art history of the Coronial Office because such visual methods interested artists trained in life drawing who liked to sketch and paint dead bodies, and thus record coroners’ working-lives. For this reason, it is feasible to trace their broad development from the early nineteenth to early twentieth centuries through the medium of iconography. In Illustration 5.1, for instance, we see a typical satirical cartoon mocking the bumptious nature of the Coronial Office from the 1820s when arguments started to be made about the need to have medically, rather than just legally qualified coroners. The image thus lampoons an inept and legally qualified coroner who has little expertise in the metabolic mysteries of medical death. In this case, we can observe a blazing fire that may have warmed up a body, seemingly dead, but capable of resuscitation. To the disquiet of the surgeon on duty, it appears that the post-mortem he has been called in to perform in his clean pale apron might involve human vivisection. He wants to halt proceedings at the ‘view of the body’ because the so-called victim has in fact started to wake up. If the surgeon continues to cut the body in front of the assembled jury, he would be breaking the Hippocratic Oath ‘to do no harm’. Even so, the Coroner insists he carry on:
Surgeon [dressed in a yellow frock coat and apron] informs the Coroner: ‘The man’s alive. Sir, for he has opened one eye’.
Coroner [dressed in wig & dark coat and depicted as fat from his office fees] replies by deploying his discretionary justice: ‘Sir, the doctor declar’d him Dead two hours since & so he must remain Dead Sir’

Illustration 5.1 ©Wellcome Images, Reference Number V0010903, A Juror Protesting that the subject of the Coroner’s Inquest is alive; showing the dangers of blind faith in doctors when declaring medical death – Coloured aquatint by Thomas McLean, 26 The Haymarket, London, c. 1826, copyright cleared under creative commons Attribution Non-Commercial Share Alike 4.0 International, reproduced here under (CC BY-NC-SA, 4.0), authorised for open access, and non-profit making for academic purposes only.
By the late nineteenth century, the Coronial Inquest was held in private, away from prying eyes in a specially designed morgue. Seldom were the jury present by this time. Reporting the facts of forensic science at an Inquest court became accepted practice. Cutting the corpse involved hence a close working partnership behind closed doors between coroners, pathologists and anatomists working in tandem. We see this typical situation in Illustration 5.2. A coroner handed over a man to the St Bartholomew’s Hospital dissection room who died a ‘natural death’. The coroner had the discretion to rule that the death was obvious as the man died in the care of the Poor Law authorities and thus there was no need for an expensive Inquest. On 7 July 1894, when the corpse arrived, an artist skilled in pathology sketched the face and chest of the friendless man in order to study the nature of decomposition, represented here with the grey-scale area of shading, spreading down the right side of his torso, in reality a blue hue. The weather was hot at mid-summer and this accelerated putrefaction, despite the corpse being injected via the carotid artery with formaldehyde to replace bodily fluids over a forty-eight-hour period.
Further record linkage work from data previously collected by this author confirms that the corpse was that of William Smith, aged 64, who died in Islington Infirmary at Highgate Hill, North London.14 Supplied by a Poor Law dead house, he was dissected, then buried. Initially the coroner concluded from a visual examination of the body that William Smith the pauper had died from a common disease of poverty, namely ‘phthisis’ [tuberculosis]. This made his body ideal for study because it came into the dissection room without extensive post-mortem cuts. We can thus observe in Illustration 5.2 how the head supported by a brick has no lancet marks on the chest, where normally a crucial incision happened at autopsy. In other words, this is exactly the sort of supply mechanism that coroners were co-ordinating with medical schools on a regular basis and it placed the Coronial Office at the forefront of the expansion of medical education in the growing Victorian information state.15 In total, anatomists dissected William Smith for ‘250 days’ until 11 March 1895. His remaining body parts were interred into a shared pauper grave, next to six other bodies. This status quo was to remain largely intact for the poorest people in society at the behest of coroners even after WWII.

Illustration 5.2 ©Wellcome Images, Reference Number L0062513, Watercolour drawing done by Leonard Portal Mark on 7 July 1894, depicting the face and chest of a man (unnamed) to show the appearance caused by rapid post-mortem decomposition. It was made about twelve hours after death, during the hot weather of July 1894 at St Bartholomew’s Hospital dissection room, copyright cleared under creative commons Attribution Non-Commercial Share Alike 4.0 International, reproduced here under (CC BY-NC-SA, 4.0), authorised for open access, and non-profit making for academic purposes only.
In a third image, Illustration 5.3, we glimpse the modern situation during the late twentieth century. Instead of the coroner conducting a post-mortem in-tandem, the forensic examination has now been delegated entirely to a hospital pathologist. We can observe the cross-like pencil lines of the crucial incision down and across the torso. The equipment is sterile and resembles the design of an operating theatre, rather than an old late-Victorian morgue. There is a basin at the foot of the steel table to collect the major organs and any tissue samples retained for further pathological study or transplant surgery. Notice, too, the ridges on the steel table to scrub down the equipment after each post-mortem. The pathologist likewise wears surgical gloves and a disposable apron. To the rear are the large refrigeration units that keep the body fresh. Here there is little physical indication of putrefaction of the sort seen in Illustration 5.2. The coroner’s role is cleaned up, with the aid of biotechnology. The facial identities of both the pathologist and the body on the dissection table are indistinct: anonymity is an ethical choice here, but it also distances medical science from human stories and their hidden histories.

Illustration 5.3 ©Wellcome Images, Reference Number L0029414, ‘Royal Liverpool University Hospital: a pathologist cutting open a body in the mortuary’, original drawing on site by Julia Midgley, Liverpool, 1998, artwork dimensions 42 x 29.7cm, copyright cleared under creative commons Attribution Non-Commercial Share Alike 4.0 International, reproduced here under (CC BY-NC-SA, 4.0), authorised for open access, and non-profit making for academic purposes only.
Further record linkage work confirms that at the Royal Liverpool University Hospital in the 1990s this unnamed body in Illustration 5.3 was one of nineteen bequests (see Chapter 4, Table 4.3) that passed into the official ownership of the medical sciences. Its donation point was co-ordinated and delegated to a pathologist on duty via the Liverpool Coronial Office. This third image is hence the logical expression of a century of scientific co-operation – by coroners, the forensic sciences, pathologists and dissection rooms – in order to cement professional status. It represents what happened to Mr Herbert Jones in our opening story too. The coroner for south Hampshire examined his body; a hospital duty pathologist confirmed the cause of death; but there was no further dissection at Bristol medical school. The coroner had the discretionary justice to decide otherwise in an explicit dispute about the deadline and its dead-end of life: one of many cases we will be encountering in this chapter.
One of the main reasons the coroner did not send Mr Herbert Jones automatically for dissection was that at the time of his death old legislation outlawing suicide had recently been changed. To allow for suicide (no longer illegal) but prevent euthanasia (still illegal), the coroner was now legally obliged to make sure that nobody else was involved in the decision of the victim to take his life, even those patients facing an imminent fatal medical prognosis: a context from 1962 that still occupies policy-makers today. The Suicide Act (9 & 10 Eliz. 2 c. 60: 1961) had only recently legalised ‘self-murder’. There was thus extensive debate in the press and medical journals at the time whether ‘doctors should prolong dying or not’.16 Debates about what constituted medical euthanasia appeared often in the media. Against that liberalisation of suicide backdrop, it remained, however, still illegal to assist an individual dying from a fatal prognosis in making the decision to end their life, termed ‘complicity in suicide’. According to Section 2 of the Act, which still remains in force in Britain: ‘A person who aids, abets, counsels or procures the suicide of another, or attempt by another to commit suicide shall be liable on conviction on indictment to imprisonment for a term not exceeding fourteen years.’ Legally this can result in a charge of ‘conspiracy’ in ‘assisted dying’. The twelve letters that Mr Herbert Jones penned to his bank, legal representative, coroner, police and neighbours seem, therefore, to have been some sort of legal safeguard to make sure that this eventuality was ruled out at Inquest. The paper trail implied that he alone made the decision to commit suicide and donate his body to medical research. He was a careful and meticulous man, and thus his actions were in character. Even so, the coroner was sensitive to what amounted to his first case of this sort of suicide situation under the new legal guidelines. He acted conservatively, investigating the full circumstances of death and the ‘gift relationship’ attached to it. Using his discretionary powers, he ordered a post-mortem to clarify Coronial Office guidance, as to:
Whether the action which caused the death was done deliberately
Whether the intended consequence of the action was their death
If the individual did not intend to take the action, their death may have resulted from an ‘accident’ to be recorded by the coroner’s verdict
If the individual action was deliberate but the consequence was not intended to be fatal, then the coroner should record ‘a verdict of misadventure’
If the individual’s intention was unclear, the short-form conclusion by the coroner would be an ‘open’ verdict17
In other words, legally coroners could recommend verdicts according to the ‘balance of probability’; in practice, suicide and its assistance (or not) made it imperative for the coroner to dispute Herbert Jones’s explicit wishes.
Complicating this situation was the fact that the coroner was also working with another important context, and one of material significance to the eventual destination of the cadaver in this sad case. Herbert Jones self-evidently wanted to bequest his body to medical research. But whether it was suitable for donation or not could be disputed by those the coroner might decide to hand the corpse over to. If the cancer about to kill Herbert Jones riddled his dying body, then in death this made it of less material use for anatomical teaching. In which case, the body would be sent for cremation without delay once the coroner passed his verdict. If, however, the specific cancer was of research interest to medical science, then parts of the body and human tissue could still be used in part for further pathological study. Another alternative is that if the body did not have significant secondary tumours, but a key organ had deteriorated to such an extent that it threatened a patient’s life, then ‘parts of’ that dead body were still a very useful teaching and medical research resource. In other words, in hidden histories of the dead, the coroner had a very important role indeed to play in starting off the post-mortem after-life of human material that came into the Coronial Office jurisdiction: a factor seldom traced in the archives, and one which we will be elaborating on later when we encounter the detailed case of Carol Morris. In the meantime, the critical point to appreciate at this point in this chapter’s developing argument is that the type of Inquest ordered, given the diseased condition of the dead body, mattered a lot to its eventual destination for harvesting. Coroners typically faced two competing tensions in this situation – how much the pathologist should cut to complete death certification procedures and how a coroner could prioritise anatomists’ need for a clean corpse to dissect.
There is one final operational issue that many coroners had to work with. Most experienced moral pressure from grieving families to alter upsetting suicide rulings. Coroners thus typically recorded ‘accident’, ‘misadventure’ and ‘open’ verdicts on death certificates. In other words, disputed bodies were contested sites of multiple research agendas and reflected family sensitivities. That said, in Mr Jones’s case his wife and son had pre-deceased him. He died without family involvement. This case’s explicit body dispute was thus exclusively between the coroner and a dead person: the former over-ruled the latter because the dead, as we saw in Chapter 2, are Res Nullius – Nobody’s Thing. Herbert Jones’s post-mortem was thus akin to those of Keith Simpson, a leading pathologist who told the Listener magazine in 1977 that for all pathologists: ‘My patients never complain to me. If their illness is perplexing, I can put them in the refrigerator and come back later on.’18 Silent conversations in cold storage facilitated the medical sciences co-creating with the Coronial Office; yet these actor networks and their working arrangements remain opaque in the historical literature. Explicit body disputes involving those such as Herbert Jones sent for cremation rather than further study remain too often undisclosed in the paper trail of a bureaucracy that made these ‘mechanisms of body donation’ both function and malfunction. It is to this paper trail that we now turn. We begin by examining first some of the common systemic flaws in the system that processed and recycled the dead.
Auditing a System with Systemic Flaws
At the various public enquiries into the NHS organ retention scandals that led to HTA2004, a considerable weight of evidence was presented that the paper trail relating to dead bodies and co-ordinated by coroners, pathologists, anatomists or medical researchers was inadequate. At the time, the Chief Medical Officer Sir Liam Donaldson concluded that it was essential to carry out a full audit of all human material held in medical schools and Coronial facilities, as well as museums, to ascertain the extent of both historical and recent retentions. In a previous chapter we briefly discussed how the final report revealed that there were ‘105,000 organs, body parts and fetuses that had been retained in 210 English NHS trusts and medical schools’.19 Of these 210, ‘around 25 leading institutions accounted for nearly 90% of the body parts retained’. Michael Redfern QC, who conducted a separate public enquiry into organ retention involving the nuclear industry, likewise concluded there was: ‘a weak and poorly understood legal framework that had allowed bad practice to flourish’.20 It was difficult not to reach the conclusion that medical scientists of all descriptions had intentionally kept patients and their families in the dark. In response, the Royal College of Pathologists issued a statement defending their position and proposing to conduct an extensive internal investigation into working practices. Even so, a concerted press campaign reported on how some pathologists with the co-operation of coroners had conducted ‘their business by stealth’. This use of emotive language to describe medical research as a ‘business’ drew widespread criticism from inside the medical profession. Many were stung by the quoting of an old English proverb: ‘A thief is a thief, whether he steals a diamond, a purse, or a small part of you.’ There was soon a cultural stand-off. Yet it was established by a series of timely new historical studies that the term ‘business’ was an accurate depiction of dissection and its hidden histories, which were closely associated with the Coronial Office and its pathology partners.
The ‘business of anatomy’ flourished because AA1832 permitted it to do so until HTA2004 became law (see Chapters 1 and 2).21 However, because the medical sciences had very little historical sense of their own inner workings, the paper trail that was created to make this system of supply function was never retained by those in charge. As a result, when scandals about the retention of human material reached the press, there was a tendency to apportion blame to HTA1961 or HTA1984 without appreciating that AA1832 had stated transparently the need to keep records. The original legislation did have a tracking system for its mechanisms of body supply. Until at least the 1930s this monitored human material much better than any modern legislation, with up to twelve certificates issued each time a body or part moved from source to dissection table. The flaw in the system was that, once audited, usually every three months, destroying paperwork became the norm to avoid unwelcome publicity. Civil servants misunderstood therefore what happened inside the system by the 1950s. They assumed there had never been a system of accountability in the past because they could not find evidence of it when drafting new parliamentary bills. Their modus operandi was thus to tinker with statutes, instead of overhauling them. As a result, histories of anatomy often assume, incorrectly, that AA1832 had no paper trail and audit procedures. The opposite was the case. There was a complex system with detailed paperwork: a classic case of the medical sciences needing to look forward to the past.
The anatomy ‘business’ was also enterprising and inventive. Staff sought practical solutions to overcome any operational issues in the most pragmatic way; and, it was logical to do so. That status quo reflected the fact that, as Joanna Innes points out, parliamentary statutes for centuries were written with ‘a sufficient level of generality to cope with diverse local circumstances’.22 From the Georgian era onwards, successive governments drafted legislation in a cursory manner because what was proposed ‘often did not commend’ itself ‘to eighteenth-century Britons’. This meant that when it came to medical reforms, discretionary powers shaped procedures. There was a high degree of discretionary justice deliberately written into ‘orders’ and ‘guidelines’ accompanying any new legislation. Coroners soon used those powers to develop close working relationships with anatomists and pathologists. So much so, Coronial officials often made up procedures as they got on with the task in hand. Over time, this created a sense that medical paternalism mattered more than death’s customary rituals in Britain. A lack of public accountability had a ripple effect in other parts of the global community too, notably in Canada, Australia, New Zealand and other Commonwealth countries, where the British legislative framework continued to shape medico-legal standards until the 1990s.23 The odd thing about this backdrop is that AA1832 never intended this outcome.
When the NHS was created in 1948, new legislation gave the impression that teaching hospitals were now meticulous about the retention and disposal of human remains, but this was not always so. One example is illustrative of what could go wrong when procedures in morgues became disorganised. On Friday 14 December 2001, the Evening Standard reported on a case where procedures in a teaching hospital went awry. Paperwork was not properly attached to a dead fetus:
A baby has been found dead among hospital laundry in London. Scotland Yard were called just after 5am yesterday after reports of a ‘human foetus’ at the Laundry in Acre Lane, Brixton. Police are checking which hospitals provide the unit with laundry. One report said the body was that of a foetus of about seven month gestation. They are trying to establish whether the baby was born naturally or as a result of a miscarriage or abortion. A post-mortem will be carried out today.24
The Times some weeks later, on 13 January 2002, explained the events in more detail:
The body was that of a baby boy, J. K., who had died one hour after being born at Queen Mary’s Hospital, Sidcup. He had been born at 23 weeks gestation, some 17 weeks prematurely, his weight at birth having been 1lb 1oz. After death the child had been wrapped in a sheet and taken to the mortuary and placed in a refrigerated drawer. Next to the drawer was a bag for laundry from the mortuary and the wrapped body had accidentally been transferred to the laundry-bag. From there it had been taken to the Sunlight laundry, Brixton and had been put through a boil wash. The father, aged 36, and mother, aged 25, were both named, the latter being a Spanish national who had since returned to Spain to recover.25
In reviewing this case, and the circumstances that led to it, Robert Bruce-Chwatt MBBS, MFTM RCPS (Glasg.), Senior FME, Metropolitan Police, concluded that there had been ‘an error of omission’ in the paperwork process when the fetus was placed in the fridge next to the laundry basket. He did not find ‘an error of commission’ involving organ and tissue harvesting of the sort practiced at Liverpool Children’s Hospital at Alder Hey by Professor Dick van Velzen.26 The fetus had self-evidently come under the jurisdiction of HTA1984. When it was moved after being stillborn it should have thus been sent to the hospital morgue with the standard paperwork attached to it. But this had been ‘mislaid’ in ‘either theatre, the labour ward, or mortuary, with the soiled laundry’. It is thus a historical prism of the sorts of material anomalies that happened inside the system as soon as the dead were moved from one jurisdiction (hospital ward) to another (morgue, Coronial facility, pathologists’ lab). Along the way, parts of the person might be consigned as ‘clinical waste’ due to carelessness. For in the case under discussion, nobody could explain how exactly the stillbirth was taken out of the refrigerated drawer in the morgue and dropped into the laundry basket by mistake. Something had gone wrong, but who was involved remained undisclosed.
The fetus was found to be ‘5–6 months old’ when examined for forensic purposes, and it now had to be disposed of according to current regulations. But these were not necessarily what the general public would have expected either. There were three legal options. If the stillborn fetus was still intact (it was in fact in a poor state having been through a boil wash in the washing machine), then it came under the Burial Laws Amendment Act (43 & 44 Vict. c. 42: 1880). Where it was instead to be cremated (after its post-mortem), then this would be carried out in accordance with the Cremations Act (15 & 16 Geo. 6 & 1 Eliz. 2 c. 31: 1952).27 Even so, if the pathologists found the fetus to be incomplete in terms of its identity, and thus its body was, strictly speaking, in parts (again, having been through a double-spin cycle), it was then in law defined as ‘clinical waste’. In which case, it could only be disposed of according to the Control of Pollution Act (Eliz. 2 c. 40: 1974), or the Environment Protection Act (Eliz. 2 c. 43: 1990). In other words, there should have been a careful paperwork trail, but it was omitted. All those involved expected the Coronial Office to use its extensive discretionary powers to put things right after a dereliction of duty.
These overlapping agencies and statutes are illustrative of the sorts of misunderstandings that could occur about the bureaucracy attached to the movement of the dead and their disposal in England. It exemplifies how the paperwork attached to the deceased was often delegated by default to the coroner, especially when things went wrong in NHS hospitals. Indeed, as Chapters 1 and 2 pointed out, the central flaw in HTA1961 was that everyone assumed that each hospital owned human material that died on its premises. They thus had the authority to dispose of their mistakes with the help of any coroners and pathologists on duty. Even after HTA1984 tried to correct this, the situation was further complicated by clause 42 of the Coroners Rules (SI 1984 No. 552), which ‘expressly provided that no verdict’ should be framed in such a way as ‘to appear to determine any question of criminal liability on the part of the named person or civil liability’.28 In other words, even when things went wrong and hospital negligence was self-evident, Coronial rules meant that at a public Inquest there was no legal leeway to name either a negligent medical professional or an NHS facility as substandard. The facility staff might look morally culpable of contributing to a death, but it was not up to the Coronial Office to determine whether this constituted a criminal offence. The Times newspaper thus explained that if, for example, a man having a very bad asthma attack died as a result of a severe delay in the arrival of an ambulance, even when there was evidence of medical negligence and an ‘unnatural’ death, the coroner could not apportion blame.29 The pathologist doing the post-mortem was correct to state that the deceased had died from ‘status asthmaticus’ [a prolonged asthma attack], but whether the circumstances surrounding the death decreased the patient’s survival chances or not, and to what extent these constituted ‘a lack of care’, was open to legal interpretation. Technically in dispute was not ‘the cause of death’ in such a case, even if the circumstances surrounding the outcome were in doubt. This common situation recurred often during the 1990s in landmark cases like that of Regina v. the Coroner for North Humberside and Scunthorpe involving a prisoner put on a suicide-watch because he threatened to take his life.30 Due to a staff shortage, the man went unobserved for periods in his prison cell, and so died of asphyxia. Whether this was, strictly speaking, ‘self-neglect’ or due to ‘a lack of care’ was ‘blurred’. The question of how long the body should be retained and which parts of it should be taken for a criminal case (or not) remained contentious.
Coroners thus continued to act conservatively and often asked their designated pathologist to remove what ‘might possibly’ be required to determine ‘the balance of probability’: a judgement call based on their individual career experiences, as we saw in this chapter’s opening story of Mr Herbert Jones. To understand how this complicated medico-legal situation worked in practice, however, it is necessary to examine a broader selection of representative cases than the ones we have encountered so far in this chapter. In each, we can observe a coroner in conflict with those that claimed agency over the dead. The Coronial Office would nonetheless prove to have extensive powers of discretionary justice in the transplant era of the 1970s. The explicit disputes that occurred often exemplified the frustration that bereaved families felt to determine the material fate and resting place of their loved ones. Since this backdrop shaped a political consensus to pass HTA2004 and those new standards were adopted in many parts of the world, a detailed analysis of the role that coroners played in the circumstances that led to a system of informed consent to correct explicit disputes are of some relevance to this book’s central focus.
Coroner’s Explicit Disputes and Organ Donation Cards – The Alcock Case
In 1983, the Department of Health and Social Security (hereafter DHSS) had taken a strategic decision to re-launch a national organ donation campaign: outlined briefly in Chapter 2 and now elaborated with human stories here. The Conservative government of Margaret Thatcher was concerned that just 15 per cent of the population were carrying organ donation cards in Britain. As a result, the British Medical Association reported that transplant waiting lists were getting longer. The DHSS commissioned a number of social surveys to measure public opinion. These indicated that NHS patients were broadly in favour of donation, but this cultural trend did not translate into positive action. The DHSS therefore allocated a budget to raise the media profile of carrying organ donation cards, taking out expensive one-page advertisements in the national press. On the eve of the campaign, the actions of a coroner from North Staffordshire brought instead unwelcome publicity about explicit body disputes. The case was to highlight the extensive powers of coroners to requisition and hold on to human material without government or familial interference.
Thus, in December 1983, The Times reported on ‘a dispute over a Staffordshire coroner’s decision to stop the heart of a maintenance fitter being used in a heart transplant operation’. He had been ‘killed accidentally’ at work.31 The facts of the story were that:
Mr Graham Alcock, aged 28, a fitter at an excavator factory in Rocester [sic], had carried a donor card with him. Before he died last Tuesday, he told his relatives that he wanted his heart and kidneys to be used for transplants.
As a result of the request doctors at the Royal Infirmary in North Staffordshire kept him alive until suitable recipients could be found for the heart and kidneys. Tests were carried out on his organs to match those of patients waiting for a transplant.32
Several hours later a ‘suitable patient was found at Harefield Hospital in Uxbridge, West London’ and an air ambulance was ordered. A helicopter flight was the quickest way to get the donated heart from Staffordshire to London. At the last minute, however, the deputy coroner for Stoke-on-Trent, Mr John Wain, informed the head of the transplant team that he had ‘unexpectedly called a halt to the removal of Mr Alcock’s heart’. The Coronial Office issued an official statement that ‘the pre-existing condition of the deceased’s heart might be relevant to the Jury Inquest in due course’ and this necessitated halting the transplantation. If the man had an underlying heart complaint, then his employers might be guilty of a breach in health and safety standards at work where he had died from an accident. There could therefore be legal implications from the case and his human material needed to determine liability or not.
The widow of Graham Alcock was upset by this turn of events. She disputed the moral right of the coroner to prevent what her husband had explicitly requested in writing on his organ donation card. Interviewed by David Cross of The Times newspaper, she complained ‘that the dying wish of her husband had not been honoured’.33 As she stressed: ‘It seems he died in vain.’ The rest of her family were also critical of the decision. They thought it was counter-productive for the medical sciences. Mrs Dorothy Alcock (mother of the deceased) told the press: ‘Many people with organ donor cards could be dismayed that their wishes were not carried out. This has lost them hundreds of donor cards.’ Likewise, Mr Ray Alcock, father of the dead man, disputed the coroner’s actions, and in calling for a public enquiry declared: ‘It seems pointless to carry a donor card if the parents cannot carry out the wishes of their dead son.’ The transplant team supported their moral position. However, as a hospital spokesman explained, they had no choice. They had to ‘pay attention to what a coroner decided – We cannot argue about it.’34 The Coronial Office was all-powerful at the dead-end of life: a procedural fact that would be debated extensively in the 1980s, as we shall see later in this chapter when we examine similar representative cases.
The coroner in this case, Mr John Wain, did in fact have a very good reputation for representing people in his local community over his thirty-year career. On his death aged 77 in 2014, after ‘a long battle with cancer’, the Stoke Sentinel described him as ‘a much loved character’ whose ‘life touched many in Staffordshire’.35 He was regarded as fair-minded, and an advocate for the underdog, according to his colleagues. It was reported that he: ‘sprang from humble roots in the city’s neck-end [sic] and took his first fumbling steps into the legal profession as an articled clerk without even a law degree (back then)’. He obtained two A-levels, worked as journalist for a short time and eventually rose in the legal profession to run one of the busiest Coronial Offices in the country. In Stoke-on-Trent he was renowned for his human empathy, as a local obituary writer elaborated:
Because he came from the same humble origins, he had a deep affinity with ordinary families as he helped them to seek answers to how their loved ones died. As their champion he would fearlessly take on at times protected interests of the establishment to get to the truth. That could be anything from top surgeons messing up operations, and social workers ignoring alarm signs from the vulnerable, to deaths in police custody. At times he stretched coroner’s legal flexibility to its limit to announce verdicts which brought maximum benefit to those left behind.36
John Wain was also a keen advocate of opening up Coronial records if they could help further medical research into, for instance, the underlying causes of suicide in his district. In January 1999 he thus co-operated with a large-scale study covering North Staffordshire in which Wain had been the presiding coroner. Data was collected on ‘all cases of suicide’ and ‘undetermined injury’ between ‘1991 and 1995’ in which ‘212 cases and controls’ were identified.37 The study team concluded that ‘the risk of death due to suicide and undetermined death was associated with: recent separation, relationship difficulties, experience of financial difficulties, history of past criminal charges or contact with the police, a past history of deliberate self-harm, being on psychotropic medication at the time of death and a diagnosis of bipolar affective disorder’. In a similar refrain, Wain had assisted with an NHS study into whether ‘pre-hospital deaths from accidental injury were preventable’.38 Again he released Coronial records covering the period ‘1 January 1987 to 31 December 1990’ in which there were ‘152 pre-hospital deaths from accidental injury (110 males and 42 females)’. The important conclusion of this study was that: ‘Death was potentially preventable in at least 39% of those who died from accidental injury before they reached hospital. Training in first aid should be available more widely, and particularly to motorists as many pre-hospital deaths that could be prevented are due to road accidents.’ Wain was thus not the sort of coroner who would routinely hold up a heart transplant unless he believed it was necessary.
Nevertheless, the Alcock family thought he was guilty of having ‘stretched coroner’s legal flexibility’ (to use his obituary writer’s precise phrasing). Even so, whether the bereaved family had legal grounds to challenge what happened or not, what really mattered in the end to them was that Wain had the discretionary justice to act as he did and he brought about a dispute at a key discrete research threshold point in a donation process. Generating explicit disputes in a transplant era was, seemingly, often part and parcel of a coroner’s normal working-life. Since cases like this raise the issue of representativeness, it is important to explore general trends regarding the retention of human remains involving the Coronial Office covering elsewhere in England. As we shall see, other coroners also took a similar view of their extensive powers to be advocates for the bereaved but also to query organ donations and hold them up if necessary. An important case of Carol Morris outlined next is illustrative of general trends in the Midlands. It is, moreover, a significant story because it was to make medico-legal history by changing the law on the anonymity of organ donation in Britain and around the world (as we shall see in Part II of this chapter, where we discuss the case’s ingrained lessons and their historical longevity involving coroners).
The Carol Morris Case
On 6 August 1977, the BMJ carried a detailed report on the modus operandi of the coroner for Leicester City and South Leicestershire.39 Since what he wrote was to have far-reaching consequences just three years later in another explicit body dispute, it is important to pause and consider the coroner’s detailed letter to the BMJ to set the scene in what became known as the Carol Morris Case. Mr Michael Charman explained in 1977 that he was legally qualified. On average, he oversaw about ‘1400 unexplained deaths’ every year in a busy area of the Midlands. He paid careful attention to the bereaved and tried where possible to relieve their stressful situation, as he explained:
Of necessity the reports issued to me by my pathologists are all couched in medical terms and when I first became a coroner I had to unravel this terminology to discover the cause of death. I also determined that to be efficient I would need to obtain explanations from my pathologists. I therefore not only view the body but also, in cases in which there is some difficulty or peculiarity, will view the body while the necropsy is taking place and my pathologists are kind enough to demonstrate to me the actual cause of death. In cases of death from a cause other than a natural one, I find this very helpful indeed when taking the inquest. Since usually the only medically qualified person at an inquest is my pathologist he is also careful to give an explanation in non-medical terms of the cause of death so that those present, including the jury, understand precisely what has happened.40
Charman told the BMJ that he worked with one of four pathologists, and he carried on the tradition at Leicester of allowing the duty-pathologist to pass on a copy of his report to the bereaved family’s general practitioner once an Inquest had been finished. He was not legally obliged to do this, but he felt that it did alleviate grief. Often the GP was in a better position to reassure a family that the deceased had not suffered or been in a painful condition. In terms of the grey areas of these legalities, he elaborated that:
It must be remembered that in England the post-mortem report on any sudden death is prepared by a pathologist appointed by the coroner and that the report is the coroner’s and belongs to no one else; furthermore it is not a public document until after the inquest or the issue of the coroner’s certificate that the death was by natural causes. It therefore follows that it would be very difficult indeed for the pathologist conducting the examination to give any explanation to a relative except in the vaguest of terms until the legal formalities have been completed. Once this has happened I personally, as coroner, would be very happy indeed to permit any of my pathologists to alleviate distress by giving simple explanations, but at the same time I know they are very busy people. …41
It would be precisely this medico-legal situation – a coroner having extensive powers to withhold information if he judged it to be in the public interest – and with the co-operation of his pathologist often pushed for time – which was to cause an explicit dispute that made national headlines. Events at Leicester by 1980 would prove contentious and ultimately change the terms of reference of working coroners everywhere in England. We begin with a tragic accident in the Carol Morris case files.
On 25 January 1980, Carol Morris, a young woman aged 16, was driving a moped in the early rush hour at Houghton-on-the-Hill village about 6 miles from Leicester city-centre.42 It was a cold and icy winter’s day. Near a crossroads in the centre of the village close to a garage, Carol Morris tried to join the oncoming traffic down the lane from her home. The location was notorious for car accidents where the B3129 crossed the A47. Tragically, in the inclement conditions a 40-foot lorry collided with the moped as it exited from a side road into the main arterial route into the city. Carol lay on the ground seriously injured. She was soon taken unconscious by ambulance to Leicester Royal Infirmary, where three days after the accident she died from her injuries. Carol Morris was carrying a donor card. Dr David Riley, a surgical registrar on duty, thus began the formal medico-legal process of checking on whether the accident victim was a suitable transplant donor. He needed to liaise with a transplant team at Papworth Hospital in Cambridgeshire to carry out a tissue match with patients on the organ donation waiting list covering East Anglia and the Midlands NHS regions. Because Carol Morris was aged 16, there were two lifestyle factors to assess. An evaluation of her general health condition prior to the accident was undertaken. The doctor found in her case-notes that it had been generally very good before the fatality. She was a fit and healthy young woman. There was every chance therefore that her kidneys (specifically ticked by Carol Morris on her organ donation card) would be healthy and ideal for transplant. The medical team also needed to assess the wishes of her bereaved parents and their familial relationship with Carol. She was aged 16 and so over the legal age of adult consent, but she was not yet 18 years old; therefore, her parents had guardianship of their daughter as next of kin. They wanted to respect Carol’s wishes to donate, and so the transplant team prepared the body without further delay. What happened next nevertheless was to cause considerable controversy – so much so that it generated a national debate in Parliament about the need for a change in the law to enshrine the principle of anonymity into organ donation programmes across Britain. The catalyst was the actions of the coroner for Leicester City, Mr Michael Charman, and the involvement of some journalists working for a number of popular daily newspapers who acted unscrupulously to get a news scoop.
Carol Morris remained on a ventilator until ‘her heart, kidneys and eyes were all removed for transplant’.43 The heart was despatched by plane and car to Papworth Hospital in Cambridgeshire on the night of 28 January. The transplant team were waiting on it. The pathologist on duty did a careful tissue crossmatch. Then the leading surgical consultant, Mr David English, and his colleagues completed a successful operation on ‘Mr Nigel Olney a 35 year old man’ from Bedfordshire, a patient desperately in need of a new heart. He was in due course to be the fourth heart transplant patient at Papworth after the relaunch of its surgical programme in 1979. Olney lived for almost nine years before he needed a second (unsuccessful) heart transplant in December 1988.44 He was thus one of the longest survivors at that time.45 Meanwhile, the Papworth team had recalibrated their working practices with some success from 1973, as recent histories of the hospital explain:
During 1973, 162 open heart operations were undertaken with a mortality rate of 5%. However, surgical activity increased rapidly and, after visiting Stanford [University], Terence [English] decided Britain needed a heart transplant programme. A major problem was lack of support from the cardiologists. However, after research at Huntingdon Research Centre where techniques for preserving the donor heart prior to its implantation in the recipient were developed, the first heart transplant was performed in January 1979. This was not successful, but four of the next five cases lived between three and eight years. Funding was also a problem in the early years, but help from the National Heart Research Fund and the Robinson Charitable Trust helped until Papworth Hospital was designated a national centre for transplantation.46
In addition, in 1980, around the time of Carol Morris’s death, a British Heart Foundation Research Group established itself at Papworth. This initiative funded the additional staff needed to expand innovative heart transplant work. Indeed, from 1981, they were able to undertake heart-lung transplants on site for the first time. In no small measure then the heart of Carol Morris was to contribute to Papworth’s becoming the preeminent heart and lung transplant unit in the UK. Even so, although the staff that led the unit feature as ‘Papworth’s heroes’ today on the hospital’s public engagement website, and the fund-raising efforts of Mr Nigel Olney after his first heart transplant are detailed (with Christopher Hubbard), no mention is made of Carol Morris. She never became an official Papworth heroine. Evidently, once removed, a body part became a discrete research step – ‘Nobody’s Thing’. That remapped the whole person into a series of hidden histories of the body, the equivalent of a consignment in the cul-de-sac of history, omitted from the success story of biomedicine.
Once Carol Morris’s heart was transplanted, the rest of her body was still technically under the official jurisdiction of the Leicester City coroner. He was required to commission a post-mortem from his duty-pathologist since the road accident might later result in the police charging the lorry driver with death by dangerous driving. There would need to be material evidence of sudden death, made available at any subsequent prosecution. An Inquest was thus scheduled. Before it convened, however, the coroner noticed that there was a discrepancy in his pathologist’s paperwork. Dr David Riley, the surgical registrar on duty at Leicester Royal Infirmary the night that Carol Morris died, asked the coroner to authorise the removal of her kidneys. Carol stated this option explicitly on her organ donation card and so her parents decided to comply with their dead daughter’s wishes, as we have seen. However, the deceased did not tick any other organs for donation. There were separate cards for each organ at the time. The bereaved parents searched their dead daughter’s belongings in her bedroom but found nothing. Carol’s intention seems to have been to donate her kidneys, probably because (her parents thought) there had been a number of media campaigns to improve their donation in the national press over the previous three years or so under the auspices of the DHSS (as described above). The coroner, Mr Michael Charman, was very mindful of being sensitive to the parents’ shocking bereavement. Indeed, he had a long history of sharing pathologists’ reports with grieving families shocked by the sudden death of their relatives in tragic circumstances, as he had previously explained to the BMJ. He felt he was now in a very difficult medico-legal and ethical situation. He had been officially asked for the kidneys of Carol Morris but not her heart and eyes which, it seemed to him, had been harvested as ‘extras’ for organ transplant and grafting purposes, respectively. The parents told the hospital staff in Leicester that they were ‘keen’ for ‘all the organs to be donated’; they interpreted the fact of their dead daughter’s having a donor card as confirmation that she was a supporter of transplant surgery per se. The coroner nevertheless believed that in case of the need for a subsequent prosecution involving the lorry driver and the question of his legal culpability on the morning of the fatal collision, the dead body had to remain solely in a Coronial officer’s medico-legal jurisdiction. He felt the transplant team at Papworth Hospital was deliberately ignoring this legal consideration, with the support of their surgical liaison at Leicester Royal Infirmary. Together they had harvested more than he had authorised. There would soon prove to be a very difficult professional stand-off between all the interested parties at the Inquest.
The Inquest opened on the Thursday after the death of Carol Morris. Charman was mindful of the stressful situation for the bereaved family, but there were a number of pathology discrepancies that in his opinion required action. He stated that he felt very uneasy about what had happened and how much was harvested from the body of Carol Morris, having ordered that: ‘no organs could be removed in his area without his written consent, countersigned by the surgeon carrying out the removal’. This claim by Charman that the ‘body of anyone who had died suddenly was his to decide upon’ was, however, ‘contested at the Inquest’. Carol Morris’s father stated categorically that as far as his family was concerned his daughter wanted to be an organ donor, stated so explicitly on a donor card, and they needed to comply with her wishes under the tragic circumstances. To do otherwise would mean she had died in vain (echoing the sentiments of the Alcock case outlined earlier in this chapter). Even so, Michael Charman replied:
His contention is that coroners should have the ultimate power of decision over how the bodies of potential organ donors are to be handled. The law, which is based on the Human Tissue Act of 1961, is at best open to interpretations, and at worst confused, say medico-legal experts.47
As the atmosphere at the Inquest was adversarial, Charman took the unusual step of calling a press conference afterwards. This upset the bereaved family, and with good reason, for since the death of Carol Morris they had been the focus of considerable unwelcome media attention. Before examining in more detail what the coroner said to the media, we first need to factor in what had been happening to the Morris family since the night of the fatality.
The Morris family had been under a media siege at Houghton-on-the-Hill since the death of their daughter on the night of 28 January 1980. So intense was the media intrusion that George Morris made an official complaint to the Press Council (hereafter PC) in London.48 He told them that: ‘on the 1 o’clock news on 29 January it was reported that a heart transplant operation had taken place at Papworth hospital and that the family of the donor particularly wished to remain anonymous’.49 He elaborated that ‘a [news] leak occurred and within three or four hours’ from someone working at Leicester Infirmary, Papworth Hospital or a PC news agency. The Evening News was the first media outlet to telephone the family for further information about the heart transplant that had taken place. Then the phone started to ring and ring. George Morris described how the phone ‘rang continuously’ from 1 p.m. to 5 p.m. when the family finally decided to ‘take it off the hook’. Events were, however, to get worse, as he explained:
However, that did not alleviate the position. The newspapers that had been told by telephone that the family were not prepared to comment sent reporters to the door. To add insult to injury, most reporters attempted to obtain additional information and a photograph of the dead girl from the villagers, despite the family’s request for anonymity.50
The family felt that ‘particular newspapers, such as the Daily Mail … behaved especially badly’. They even contacted their ‘next-door neighbour, Mr. Stephen Turnbull, giving the impression that they were friends of the family requesting information’. George Morris explained that the way that the reporters worked was to inquire ‘about the donor card’ and only later admit that they were journalists seeking a news scoop. In the family’s opinion at such a sensitive time, they all felt understandably: ‘That is a despicable way of obtaining information.’ Yet, worse was to come.
George Morris alleged that one determined reporter for the Daily Mail (Sally Brompton) waited outside the Morris family home ‘from 10 am on 30 January until 6 pm’.51 She then ‘canvassed the village from door to door in an attempt to buy a photograph of Mr. Morris’ daughter Carol’. George Morris subsequently relayed to his member of Parliament how ‘Miss Brompton even attempted to persuade a 14-year-old girl to go into her elder sister’s bedroom to remove a photograph of Carol’. She finally toned down her actions when ‘at about 6 pm Miss Brompton left a card with Mr Morris requesting an interview at a later date’. The family had taken enough. They requested and were granted police protection by the Leicestershire constabulary. A police officer, posted outside the family home at Weir Lane in Houghton-on-the-Hill, also arranged for British Telecom to make the home telephone number ex-directory until further notice. Mr Morris did acknowledge to the PC that although the Guardian newspaper and the Leicester Mercury had obtained photographs of his dead daughter, they decided not to print them once it came to light that they had been obtained by unscrupulous means. Their editors had acted, in his opinion, with common decency, unlike all the other newspaper tabloids which had ‘not acted in a professional manner’ at such a tragic time. The family now found themselves in the middle of a media storm not of their making and one which the coroner for Leicester city centre was about to exacerbate by calling a press conference after the Inquest about an explicit body dispute.
Michael Charman explained to the media that he felt obliged to call a press conference about the circumstances surrounding the death and harvesting of the organs (heart, kidneys and eyes) from Carol Morris because he believed procedures were unethical and technically illegal. He clashed with Mr Bernard Hargrove, head of a legal team who appeared for the three transplant surgeons involved: one at Leicester and two at Papworth Hospital. The Medical Defence Union funded Hargrove. He insisted that since 1977 the Home Secretary had taken the view that ‘no coroner could refuse for the removal of an organ unless it was needed for criminal proceedings or had been faulty’.52 In the case of a fatal road accident arising from careless driving causing brain-stem death, the retention of the brain in question would suffice as material evidence of medical death at a criminal prosecution. Hargrove also insisted that in the opinion of most doctors it was their medico-scientific duty to facilitate ‘all organ donation’. Yet, as a newspaper reporter for the Guardian who was present at the Inquest press conference explained, it really came down to one key question in this controversial case: ‘Who has the ultimate right to decide’ on organ donation in a Coronial case – ‘the coroner or the family?’ Moreover, this raised an important procedural point too – ‘Could a coroner refuse permission for the removal of organs, even if the deceased carried a donor card?’ Charman defended that he was very concerned that the surgeons who removed the heart had effectively ‘disregarded the law of the land which says that my consent must be obtained’. He clarified that he was not accusing the transplant team of deliberately flouting the law – ‘What they did was make assumptions which didn’t exist and thought that they had got consent when it wasn’t there at all.’ Soon, the storm created encouraged other medical bodies to get involved in the widening debate about this and other explicit body disputes involving the Coronial Office in England.
The British Medical Association (hereafter BMA) was quick to respond, issuing a press statement that they were worried that the adverse publicity could dissuade other organ donors from coming forward in the future. If all coroners requested a written rather than a verbal consent (the latter was standard practice in some transplant units), then that might also delay the removal of a heart and render it unsuitable to transplant in time. But Charman pointed out that this was nonsense, since written permission from the coroner delayed matters for no more than ‘an hour at the most’.53 Besides, he pointed out, in practical terms most donor patients were kept ‘on a heart-lung machine and time is not so vital, except at the moment of removal’. The Coroners’ Society for England and Wales (hereafter CSE&W) nevertheless joined in with the BMA’s concerns since both professional bodies were pro-transplantation. Dr Burton, a spokesman for the CSE&W, told the press that he had been a member of the Transplant Panel which had been convened to monitor the progress of transplantation, and in his experience: ‘For years we have been slowly moving towards the general public’s general acceptance of transplants as a routine matter of course. Every time this sort of thing happens’, where there is a stand-off between a coroner and the bereaved involving an explicit body dispute, ‘it sets the progress back years’. The assembled reporters thus asked Charman how he felt about contravening the family’s wishes. Did he consider whether he was going against the wishes of the bereaved and making things much more difficult for them? In reply, Charman defended: ‘No, I don’t. They must of course consent before my consent is asked for. I don’t think that in any way asking them for written permission affects it’ (that is, the decision to donate or not by the bereaved). He told the packed Inquest that the police had found that ‘there was not sufficient evidence to prosecute anyone for contravening the Human Tissue Act 1961’. Moreover, after hearing all the evidence collected from the roadside scene, there was no evidence that the lorry driver was guilty of dangerous driving. It was a tragic case; in the end, the coroner recorded a verdict of ‘accidental death’.
At the close of the public controversy, the BMA issued a further statement. They did so to clarify that each Coronial official should have sole jurisdiction of bodies in unexplained circumstances. And yet, they went on to state that HTA1961 gave ‘the next of kin ownership of their loved one’ when they were a whole person, whereas ‘the removal of parts of it must be up to a coroner’.54 This meant that as far as all the medico-legal officials involved were concerned Carol Morris had been a person with a family history that gave her a sense of community and belonging – until, that is, in death, she had become a cause célèbre because she wanted to ‘gift’ part of her body as a bequest. Consequently, her lack of agency in death and dwindling material integrity because of becoming a transplant target meant that she became recycled for public consumption: an outcome that her family found painful to come to terms with. They now had a very difficult decision to make about whether they should retreat into private grief or seek public redress from the press for being hounded. Given how much their privacy was breached, few onlookers would have blamed them for closing ranks and never speaking again about the dreadful circumstances of Carol Morris’s donation. Yet, with emotional fortitude, they decided to contact their local member of Parliament and asked him on their behalf to highlight the dreadful experience they had been through as an organ donation family. For, they did not want others to be in the same position of exposure to such intense public censure. And thus, we see how an explicit dispute came to national attention.
Donor Anonymity – A National Issue
On 5 March 1980, the Right Hon. Mr John Farr, MP for Market Harborough in Leicestershire, tabled an early day motion in the House of Commons. He did so on behalf of his constituents the Morris family:
I beg to move, that leave be given to bring in a Bill to provide for protection of the identity of donors of human organs. My reason for rising to present this Bill to the House is to respond to a request from one of my constituents whose daughter was recently tragically killed. After her death my constituent and his family underwent what can only be described as persecution by the media in a most improper way during their time of sorrow.55
Farr explained that he had ‘cross-party support’ for an amendment to the new Health Services Bill about to come before Parliament. The proposal was to attach to it a revised Code of Practice introduced in 1979, with the support of the BMA, to better regulate the transplant surgery of hearts by making all donations anonymous. There were thus two ways forward, as Farr explained: ‘First, again in order to assist anonymity, could not all the cards of those who wish to remain anonymous have the word “anonymous” printed diagonally in large type across the top? Secondly, in these days when organs of all types are so pressingly needed, could not we have a single donor card for all organs, which would greatly simplify the system?’ Farr had consulted the Secretary of State for Health, who was supportive. There was general agreement that the new procedures would protect families like the Morris’s from such public exposure for an altruistic act at a time of tragedy.
During the early day motion debate, Farr explained to his fellow MPs that the pace of transplant surgery in terms of its new techniques was moving faster than the law in Britain.56 So, whilst a Code of Practice for the Organ Donation(s) of kidneys was well known and had been operating efficiently for some time, the surgical ability to do spare-part surgery with hearts had exposed explicit body disputes that would become more contentious. The heart seemed to rouse public sensibilities because of its important cultural symbolism in Western society. It meant that any lack of clarity in the Code of Practice left heart transplant surgeons exposed to media harassment. Families that donated faced a maelstrom of press intrusion too. Yet, the Code’s language was loose when transplant techniques were influx. The press were thus quick to quote any lack of clarity in the wording. It was now important, in Farr’s opinion, to alter the discourse to reflect the changing realities of biotechnology by 1980. This would then ensure that compliance was transparent. He gave an example of how ‘paragraph 37 of the Code’ states that: ‘The staff of hospitals and organ exchange organisations should always try to maintain the anonymity of the donor and of the recipient.’ He reiterated: ‘I do not believe that that goes far enough today. I should like to see a fresh code drawn up.’ If the Code was redrafted in ‘plainer language’ – replacing should with must – this would guarantee anonymity for all involved on both sides of the donation exchange. The time had come to no longer fudge the pressing ‘question of anonymity’. It ought not to be dealt with ‘in a cavalier manner’ of the sort that the Morris family had experienced. In a final gesture that acknowledged the stressful situation his constituents found themselves in, Farr closed his speech by clarifying the current law according to HTA1961: ‘That Act clearly lays down that coroners have the right to require consultation before organs are secured. However, I understand that most organs are obtained after telephone consultation with the coroner, which I believe is a proper and correct procedure, which does not take up very much time.’ This reiterated that although the Leicester coroner was correct in medico-legal terms, others were working their way around the law in practical ways to facilitate transplant surgery. Reforms to working practices would thus ensure the Coronial Office avoided generating explicit body and body parts disputes.
In due course, as Hansard confirms, ‘Mr. John Farr accordingly presented a Bill to provide for protection of the identity of donors of human organs: And the same was read the First time; and ordered to be read a Second time upon Friday 14 March and to be printed. [Bill 160].’57 He did so successfully because he had widespread support in the Commons, including amongst the ranks of an influential lobby of leading exponents of transplant surgery:
Mr. Greville Janner Labour MP for Leicester West (1974–1997), Mr. Tony Marlow Conservative MP for Northampton North (1979–1997), Mr. Jack Ashley Labour MP for Stoke-on-Trent (1966–1992), Mr. R. A. McCrindle Conservative MP for Brentwood and Ongar (1974–1992), Mr. Tam Dalyell Scottish Labour Party MP for West Lothian (1962–82) and then Linlithgow (1983–2005), and Mr. Michael Hamilton Conservative MP for Wellingborough (1959–64) and then Salisbury (1965–1993).58
Of these, Tam Dayell had been one of the most high-profile spokespersons in Britain. He wrote a regular column for the New Scientist in which he often featured the need for more transplants and the lobbying on this issue that he was undertaking in Parliament.59 Likewise, Jack Ashley was a lifelong exponent of disability health issues and he promoted the re-enablement of those who could benefit from new medical treatments. All the others had strong local political connections to the East Anglian and Midlands regional areas of the NHS where many of the explicit Coronial disputes were being generated during the 1970s and early 1980s.60 Together they thus constituted a powerful faction that could substantiate the unpalatable position of donor families from across the social and political spectrum. As John Farr emphasised, the issue of anonymity was an emotive one because it had real consequences:
Mr. Morris alleges that the behaviour of the media caused more pain and anguish to my wife and daughter. The newspaper reporters even had the nerve to challenge Mr. Morris when he wished to leave his house, as if he were a criminal on the run. Mr. Morris said if transplants are to continue donor organs are essential. Families will not consent to the use of deceased relatives’ organs if the media continue to act in such a disgraceful and unsympathetic way. If families are to be badgered in this disgraceful and unsympathetic way by the media even when requests for anonymity have been made, the source of organs for transplant will dry up. I agree with Mr. Morris, and though I am in the van of those who believe in the need for a free press, I believe that the conduct that I have described is evil. We must therefore make it as difficult as possible for such ghouls to gain any clue as to the identity of sorrowing families.61
‘Evil’ was a strong term to use – too strong for some newspapers editors – and so soon events would prove that anonymity was not necessarily as straightforward as was implied in Parliament; for, there was another side to the Carol Morris controversy that came to light too.
The Controversial Nigel Olney Case
The PC and its media outlets were somewhat stung by the criticism being levelled at them in the Carol Morris case. Indeed, it was clear that the disputed actions of some journalists could lead to a change in the law. This would give donors, and their recipients, anonymity in transplant surgery on a permanent legal basis. If the press were to make a case for more public accountability, then they needed to take a new tack. They soon found a news angle. Reporters were despatched to investigate the personal circumstances of Mr Nigel Olney who had received the ‘gift’ of Carol Morris’s heart. The Guardian newspaper was one of a number of the broad sheets and popular dailies that opened with a report that was positive in its tone. It informed readers that Nigel Olney had been sitting up in his hospital bed at Papworth, and he was recovering well from the heart transplant operation, which took ‘five hours and seven minutes and was led by the South African-born surgeon Mr Terence English’. Then lead articles turned into an exposé:
Mr Olney, a Leighton Buzzard, Bedfordshire, chiropodist, had separated from his wife and two young children and lives with his parents. His severe heart complaint was amongst the factors that had saved him from being sent to prison last year after he was found guilty of obtaining £5, 553 from two local health authorities by deception. At Bedford Crown Court he admitted claiming money for patients who had died or moved. Suspending an 18-month sentence for two years Judge David Lowe said: You are a man of no previous convictions and we take into account your medical condition [sic].62
The unwitting testimony implied in this editorial line was that this was a man with questionable morals by virtue of his pending divorce (allegations of adultery and child custody rights for men were still a sensitive social issue in the 1980s). He was also a convicted fraudster that had benefitted from being in an NHS facility paid for by the same taxpayers he had defrauded in his chiropody work in the community. The Guardian newspaper was nevertheless careful to balance its editorial slant. Interviews were obtained from Mr Olney’s soon-to-be ex-wife, his near-relations, and a Papworth Hospital spokesman about the costs of his operation and aftercare. All stressed that he was a suitable donor recipient. A neighbour of the Olney family in Leighton Buzzard, Mary Campbell, described Nigel: ‘He is a hell of a nice guy. Nobody deserves to live more than he does. He’s been so weak recently he’s had to be carried when he goes out.’ In mitigation, she alleged: ‘I think his illness and his marriage problems would account for some of his other troubles.’ Likewise, Nigel Olney’s separated spouse who had moved to a Hertfordshire village with ‘her two children Jason and Nicole’ told a reporter on her doorstep: ‘I am extremely concerned and hope Nigel makes a steady recovery.’ It was a dignified response from his separated wife in the face of full public exposure. Nigel Olney’s parents similarly ignored the accusations of his unworthiness and stressed instead in a statement to the press: ‘We are most grateful to the hospital for accepting our son and taking such good care of him.’ A Papworth Hospital spokesperson meanwhile explained that recently the transplant team received a charitable grant of £50,000 from the National Heart Research Fund and this money, not NHS resources, was funding the transplant and aftercare required. When pressed, the transplant team estimated that ‘the operation and a year’s aftercare would cost about £15,000’ in each case. In other words, the Carol Morris explicit dispute with a coroner was now being recycled into a much wider set of other body part disputes about the future medical ethics of transplant surgery in a modern world.
It was well known at that time that the NHS had refused to fund such risky surgical procedures as heart transplant. On the one hand, then, the newspaper coverage was being duplicitous in connecting Mr Olney’s fraudulent behaviour to his alleged exploitation of public healthcare funds. On the other hand, the NHS had built Papworth Hospital in the first place from central taxation and so Nigel Olney was technically receiving a benefit in kind by being cared for in that facility. Evidently, the assessment of the case on financial, medical and moral grounds rested entirely with the transplant team and the charity in question. Indeed, the medical team stressed that they examined the best surgical chance for a tissue match and, provided the pathologist on the transplant team found that the immunology looked favourable, it was judged prudent to go ahead. There would have been a sound medical case for the transplant to proceed. It was not, moreover, for transplant surgeons to investigate the moral grounds for proceeding in individual cases. However, this question of the morality of transplant work did not abate, either at the time of the Olney case or subsequently once liver transplants became feasible. Often the media would ask: Should an alcoholic (for instance) receive a liver transplant? It was an ethical question that featured in many high-profile cases such as the ex-footballer George Best, famous for his hedonistic lifestyle and family history of alcoholism.63 Yet, Nigel Olney’s brother in response to the considerable media storm, and the very personal criticisms being levied, reiterated to the Guardian: ‘the family are very distressed that Nigel’s past has been “raked up” when he was still in intensive care’.64 In many respects then Nigel Olney was a test case for what would prove to be ongoing ‘moral’ debates surrounding transplants and the anonymity for recipients in Britain and Europe. What Carol Morris’s bereaved family felt when they discovered the personal circumstances and criminal record of Mr Nigel Olney was not recorded publicly at the time in the newspapers; yet, it cannot have been palatable to be part of an ongoing press exposé, even by association, during the first stages of grief.
The balance of the evidence in this symbolic case makes it clear that heart transplant surgery was an emotive issue in the British media – journalists tapped into a long history of the heart being a central and enduring symbol of humanity in histories of the body for many cultures.65 Yet, it was also a litmus test for many of the procedures put in place when the Victorian Information State established working arrangements, aspects often neglected in standard historical studies.66 Coroners had extensive powers of discretionary justice, and they had worked hard to promote their image as protectors of law and order in the community. As they moved from being legally to medically qualified, and worked alongside pathologists more regularly, it enhanced their professional status. Their individual sense of personal agency increased too. So much so, that by the modern era they had become the fulcrum of advances in forensic medicine and pathology. In an era when medico-legal jurisdiction over the body was to become contentious as researchers inside the medical sciences competed for better access to cadavers and ‘live’ donors (in kidney transplants, for instance), coroners began to clash with those they had co-operated with in the first place to raise their professional status. The Carol Morris case exemplified that trend and soon led to international scrutiny too. In this way, explicit disputes had a global impact.
International Impact
There had been an initial ‘transplant fever’ across the world from 1968. As the Observer reflected there were ‘more than 100 heart transplants by 64 teams in 22 countries. But most of the patients died, succumbed to infection or rejection, the biochemistry of which was not clearly understood, and the fever never faded’.67 In the mid-1970s, many thought that the transplant era ‘was over’ because the new technology had ‘left in its wake considerable distaste for the eagerness with which some surgeons had joined the transplant rush’.68 An added logistical issue was that governments saw such risky operations as an electoral liability. Few wanted to divert their healthcare budgets to fund the research and development of transplant units, even though survival rates and immunosuppressive drugs had improved by the end of the 1970s. Papworth had raised the profile of heart transplants in Britain, but whether they could sustain their success depended on more funding by medical charities and better management of the attendant media publicity. This is what made the Carol Morris case noteworthy. For, it exemplified that public relations were an intrinsic aspect of the transplantation era whether the medical community liked it or not.
It was in many respects ironic then that those involved in the Carol Morris/Nigel Olney heart swap expressed surprise about the negative coverage after the coroner’s explicit dispute exposed the details of the case to media scrutiny. For, in an interview with Christian Bernard (who carried out the first heart transplant in the world) for Tomorrow’s World televised on the BBC in 1968, the audience of medical experts and church leaders assembled from across Britain kept making repeated criticisms of his team’s ‘mishandling of the media publicity’.69 He was asked ‘why he had made available pictures of the donor and his relatives’, and ‘why had he made the personal details of the donor made known to the recipient’ when this was unnecessary? It could be interpreted as a breach of the Hippocratic Oath’s commitment, to maintain patient confidentiality at all times. Bernard defended:
‘If you could do that you’re a better man than I am. … It was just impossible’. He elaborated on how: ‘We tried to stop all publicity to start with but you will well remember that when you heard the first reports of this no names were mentioned. But after this it was completely impossible, it just snow-balled, we had no control over the matter. It’s just something that you can’t control’.70
Bernard then threw down a challenge to whoever did become the first heart transplant surgeon in Britain. If they and their team succeeded in controlling, limiting or stopping the publicity of the inevitable media frenzy, then he would, he said, ‘Take my hat off to them!’ The transplant team at Papworth Hospital soon found themselves in an equivalent situation in the early 1980s. Yet, they could have designed a better and more confidential transfer handover process. Precedents in kidney transplants were established, and the controversial South African heart transplant situation meant professional lessons had been publicised. Equally, the Coronial Office could, and sometimes did, countermand new procedures that were put in place because they had the individual discretionary justice to do so in England. Explicit disputes were thus literally ‘the heart of the matter’ in many localities outside of London.
The change in the law that the Carol Morris case created to protect the anonymity of donor families, and by extension their recipients, was to have far-reaching sociocultural consequences, but not necessarily ones that were anticipated at the time. There did appear to be strong ethical grounds for checking media intrusion, especially in Britain where the tabloid press were persistent in pursuit of a newsworthy medical breakthrough. There was also a reasoned medical case put forward that some recipients who knew their donor’s identity did experience psychological pressures, which included feeling guilty about being the beneficiary of someone’s death. Recipients likewise expressed concern about not having the physical energy for any emotional involvement in another family’s trauma. Yet, it is equally apparent that around the world as countries adopted British standards, the sociocultural distance between donor ‘gift’ and recipient got wider and wider as transplant techniques improved. So much so that eventually ‘Red Markets’ have been created in countries like India, as Scott Cairney points out (see Chapter 1), which have facilitated organ ‘vendors’.71 It is a disturbing irony that anonymity, which was introduced to protect the Morris family and many others like them, also shields unscrupulous body brokers operating as spare-parts traders via the Internet in many of the poorest parts of the world today. This socio-medico reality has recently been the subject of renewed debates in transplant surgery circles about whether to rescind or keep anonymity. Briefly, we consider this outcome of the human stories we have been examining in this first half of the chapter, and which reflects the importance of their wider historical lessons.
In Belgium, politicians debated in 2009 whether better communication should be facilitated between ‘live’ donors (and/or grieving families in cases of sudden death) and their living recipients.72 They commissioned studies to test public sentiments. In one leading example, a representative sample was identified of 249 transplant patients, and, of these, 176 people took part in an opinion survey. Some 70 per cent of those participants (n=123) wanted to maintain the status quo for the psychological reasons stated above, namely, the recipient would find it very difficult to cope with any emotional engagement with the donor family. Around 19 per cent (n=11) were keen, however, ‘to obtain some information about their donor’ and would at some point wish to ‘express their gratitude’. Meanwhile about 42 per cent (n=72) of the sample ‘would worry about the donor having a different background to them’, and what differences would mean (there was no suggestion of racism but rather concerns about socio-economic status, class and educational differences) in terms of relating to each other. Nonetheless, 36 per cent (n=55), having considered the survey carefully, thought there probably should be a change in the law to connect people in the ‘gift’ relationship and make it more ethically transparent. Eventually, it was concluded that: ‘Prudence to change the law is warranted, as only a minority of patients are in favour of rescinding the anonymity.’ The matter was tested again in the Netherlands in 2015, and a survey of about the same size and scope (again involving liver donations) came to the conclusion that: ‘There is no need to change the current legislation on anonymity of organ donation.’ However, it also found ‘that most liver transplant recipients would like to receive some general [author’s emphasis] information about their donor’. Therefore, ‘clear guidelines on the sharing of donor data with recipients needs to be established’.73 Moreover, in countries like Israel and the USA, studies have recently been delivering similar messages. Provided transplant co-ordinators take the initiative and facilitate appropriate contact between donor families and recipients in all types of surgical interventions (heart, lungs, kidneys, eyes and liver), then there is a public appetite for promoting more personal interactions, paced properly and sensitively handled.74 The Carol Morris case continues hence to be the focus of global ethical debates, even by those who are unaware of how the powers of an explicit body parts dispute by her Leicester City coroner were to change the terms of reference in transplant history for everybody in Europe and beyond. Having therefore engaged with these human stories we now need in Part II of this chapter to evaluate their ingrained historical lessons to reconsider how and with what outcomes the power and palette of the Coronial Office endured for so long. To do this, we need to look in more detail at the systemic flaws in the Coronial system of handling the dead – picking up on themes we have encountered in Chapters 2 and 4 and now expanding on them – namely, the extra time coroners spent with human material, how it was harvested, and in what ways the flawed system of death certification potentially undermined the precious information that could be generated from ‘causes of death’ pathologies to further medical research in the modern era. In other words, the next section is concerned with how micro-stories, reassembled from their dissected remains, have macro-lessons of significant longevity in hidden histories of the dead.
Part II
More Extra Time of the Dead
Adverse publicity generated by the Coronial Office was placing anatomists too in a very uncomfortable professional position by the 1980s. In the media, they had been busy promoting body bequests as the ethical way forward since 1954. Few relished being tarnished by the sorts of explicit body disputes happening routinely in organ donation. Practically speaking, however, anatomists had to find a way to continue to work with coroners involved in sensitive explicit disputes to keep up their supply-lines. As a result, most anatomists became evasive and publicity shy when asked about the specifics of their workload, fearful that being honest could undermine their campaign for more body bequests. This atmosphere of public engagement on the one hand and public retreat on the other hand, sometimes created the misimpression that all cadaver work was suspect, when, in fact, anatomists were just being cautious to protect essential supply-lines for better medical education. An added operational difficulty was that in the Thatcher era, all NHS facilities were under intense financial pressures to cut budgets. Staff were being made redundant or leaving voluntarily to train in another career. Hence, the medical research sector started to contract. Often administrators were hit by the first rounds of budget squeezes. As a result, the bureaucratic time it took to process dead body bequests inside the medical school system was elongated. By 1993, it could take up to an extra thirty-one months in some training facilities to get human material signed off officially by the Anatomy Inspectorate at the DHSS. These bureaucratic inefficiencies not only created the potential for discrepancies to occur from time to time but also started to alert the public to paperwork slippages. Those covered in the media created a climate of mistrust by the end of the 1990s when the tide of public opinion turned against the medical research community. To appreciate that context, and how it was to shape debates surrounding HTA2004, it is important to engage with how much extra time with the dead was first created inside the system (as we did in Chapter 4) and then extended (as we will do here).
The way that the system of supply worked was that when a death occurred on the wards of a teaching hospital, it was reported to a coroner. S/he then asked a pathologist to do a post-mortem to rule out medical negligence, as we saw above. If the cause of death was obvious, then the body could be passed on as a bequest, or a body part such as the heart could be retained for future research. This was entirely in the ‘gift’ of the coroner, provided the donor family had been consulted beforehand. That then opened up the possibility for dissection. Provided there was no reason not to go ahead, a medical school would receive a bequest body in the usual way. For up to two years, medical students would train on the corpse. Once this had finished, the human remains went for ‘disposal’, generally by cremation authorised by the anatomist on duty (see Chapter 2). All of the paperwork so far inside this system of supply looked straightforward, until, that is, one examines the official returns to the Anatomy Inspectorate for the 1990s. These reveal minor but important paperwork discrepancies.
In a significant number of cases, the signing-off certificate that should have been issued at the time of cremation was delayed – sometimes for up to another three years post-cremation. Grieving families generally assumed that at cremation, ‘disposal’ was certified and then the case closed as signed off by the dissection team, but this was not always the case. The coroner, for example, could delay issuing a final sign-off certificate if body parts, human tissue or cell-lines had been retained for ‘further consideration’. Hence, these were not cremated with the residual corpse after dissection, a situation exposed during the NHS organ retention scandals in 1999. The absence of a final signing-off notification was in fact ample proof that parts and pieces of the corpse might be used to push past a deadline. The anatomy auditors either did not notice this discrepancy on the part of pathologists (who kept the retentions), or by convention chose to ignore what was not their business. Either way, the system of supply did not operate in such a way that officials could easily take an overview of all the discrete research steps involved, reiterating the autonomy and discretionary power that has often featured in this book. The power and palette of the coroner was pivotal to this system of retention and recycling.
A further complication is that even though most anatomists worked within the law according to HTA1984 (keeping detailed records and ensuring that bodies were signed off locally before cremation to complete paper trails), the DHSS centrally was not necessarily following suit. Serious underfunding of the Anatomy Inspectorate during the Thatcher era meant that if for any reason paperwork related to a dead body that then went for cremation got held up inside the reporting system (the local sending in returns to central control that got delayed), it could remain in an overworked official’s in-tray (now that staffing had shrunk) and not signed off centrally, sometimes for as long as three years. Under normal circumstances, this would not have mattered. After all, it was an internal procedure. The body in question had finished being dissected and was cremated properly with an appropriate ceremony. Yet, it also left open the opportunity for future criticism of anatomists that they were not in full control of their internal audit mechanisms: facets of their working-life that would be closely scrutinised in the run-up to the HTA2004. Anatomists also kept little track of Coronial material designated for ‘further consideration’ that might involve more research study for an extended time period. Several cases are illustrative of this sort of routine gap in the record-keeping.
An elderly man aged 85 died of a stroke on 22 March 1993. His body went to King’s College medical school. This was done with the co-operation of the Coronial Office on 25 March 1993.75 The original cadaver was then sent for ‘disposal by cremation on 23 May 1994 to the South London Crematorium’. Thus, it underwent dissection study for 14 months in total. The final signing-off certificate was not, however, issued by the Anatomy Inspectorate, centrally (having been originally countersigned locally by King’s College anatomy department) until 12 December 1996, another 2 years and 5 months post-cremation. Whether this involved the ‘further consideration’ of any human material taken from the Coronial supply-chain was not disclosed or recorded. Similarly, when a female aged 75 died of ‘MI [myocardial infraction, a heart attack due to lack of blood flow] on 3 January 1993’, with the co-operation of a hospital coroner, she was passed over to St George’s Hospital medical school for dissection on 7 January 1993. That is, once the pathology had been done on her defective heart over 5 days, the original body shell was then dissected until 6 October 1993 before being ‘disposed of by cremation’, again at South London Crematorium. Once more, however, the signing-off certificate was delayed, not issued in this case until 12 November 1996, another 3 years and 1 month post-cremation. In terms of the complete paperwork trail, this body looked like it had been retained for a total of 3 years and 11 months, whole and in part(s). Again, whether this covered human bio-commons taken for ‘extra consideration’ is not clear.
The anatomical sciences, without anticipating how public perceptions might view this bureaucratic slippage, were leaving themselves wide open to future criticism that they had lost sight of a series of all their discrete research steps, when in fact it was the central authority that was letting them down. It was unfortunate that systemic flaws in the bureaucratic system for signing off the dead (the result of understaffing problems) made it look like what was happening was that hidden histories of the body were designed to deliberately flout HTA1984. Generally, they were not, but the gap between the public rhetoric denying systemic problems (everything is fine and functioning well – the official DHSS line) and the reality of financial constraints (constant financial cuts, and corners cut in paperwork by exhausted personnel) was never properly explained to the general public to protect the supply-lines of anatomists from coroners. As a result, when we look at the official figures from this time period, they look odd. It appears that anatomists were spending more extra time with the dead than may always in fact have been the case. Figure 5.1 illustrates this common situation by using the example of UMDS medical school (one of the biggest in London, combining anatomical, medical teaching and dentistry training) which first featured in Chapter 4. A sample year of 1993 has been chosen to illustrate trends in the time lag of signing-off procedures. However, although these figures show that the creation of this extra time of the dead was not the fault of those working in individual medical schools, it does raise the question: Did these time lapses created by the central authority become something that later those that wanted to keep hold of more human material for ‘extra consideration’ took advantage of? In other words, did the systemic flaws in the system of processing the dead, after Coronial, pathological and anatomical work, create the canvas on which explicit body disputes were to be played out? To answer this question, we need to delve deeper into the archive material.
Returning to the large anatomy data-set of national trends that underpinned Chapter 4 (data displayed in Figures 4.6 and 4.7, and Table 4.3), it would appear that from 1993 onwards it became normal to delay the sign-off of human material post-dissection.76 This happened as a matter of course not just at leading London medical schools, like King’s College, St. George’s and UMDS, but also at Bristol, Manchester and Liverpool medical schools too. Consequently, in the record-keeping one can observe the broad contours of what would become the prime locations of NHS organ, heart and human tissue scandals, some seven years before they came to public attention. Thus (by way of example), there were 55 bodies in the 1993 teaching cycle in which ‘extra time’ was created after initial cremation. Again Figure 5.1 focusses on 30 of those 55 bodies donated to UMDS, since it illustrates the typical time frames of retentions that may have involved more recycling of material. Altogether the human material was not officially signed off for 3 years and 10 months, even though the corpses supplied from Coronial officers were cremated after 1.5 years. In other words, in cases that were potentially already explicit disputes inside the system of processing for teaching and research purposes, there is an extra time of the dead of 2 years and 4 months which is unaccounted for. It might be a bureaucratic slippage as a result of financial factors constraining less staff to sign off the paperwork centrally, or we could be viewing a process of ‘extra consideration’. We will probably never know which because the archival record is so patchy, but nonetheless we are glimpsing a hidden history of the dead arising out of explicit disputes, and one of some longevity. Today this is no longer legal, as Figure 5.2 explains.
Any attempt (intended or by default) to elongate the authorised paperwork trail that processes the donated dead is no longer permissible under HTA2004. As Figure 5.2 shows, the maximum retention period is three years for the body, though generally most are cremated after two. Significantly, no more than one third of the donation bequest is used for ‘teaching and/or further examination’. This code of practice is to guarantee human dignity in the dissection room. Provided, however, that the donor and their relatives have agreed to it, body parts can be subject to a bequest for ‘an undetermined’ period. This must nonetheless have been the result of fully informed consent. In other words, there is still an ‘extra time of the dead’ inside the system, but it is now a transparent process rather than a covert one. Altogether the old system of ‘extra consideration’ that we saw in Figure 5.1 has now been outlawed by the new system of ‘an undetermined period’ with fully informed consent in Figure 5.2. This means that the explicit disputes of the past have now been redressed, but before we leave behind that context we need to pause and appreciate what all this extra time with the dead (intended and unintended) meant. Thomas Laqueur writes: ‘Death in culture takes time because it takes time for the rent in the social fabric to be rewoven and for the dead to do their work in creating, recreating, representing, or disrupting the social order of which they had been a part.’77 We can only know this, however, in terms of how medical research recycles the dead by first finding and mapping material fates found in the death certification processes of dissection, its pathologies and the performance of actor networks. If we are to follow explicit disputes from human story to advancement in medical science, then we need to also ask two related research questions in the final stages of this fifth chapter. If Coronial remains were pivotal for anatomical teaching and practice, the expansion of pathology and forensic medicine, as well as more wider research cultures, what role did their death certification process play in improving public health in Britain after WWII? In this way, were body disputes the bedrock of better medicine for everybody, and did this justify their bio-commons?
Coronial Necropsies – Missed Opportunities and Their Public Health Costs
In the early 1980s, the National Patient Safety Agency (hereafter NPSA) commissioned a series of annual reports paid for by medical charity funding under the auspices of the National Confidential Enquiry into Patient Outcome and Death (referred to from now on as the NCEPOD), which we touched on in the introduction to this chapter.78 The aim of the initiative was threefold: first, to better understand why patients died in large medical facilities, such as NHS teaching hospitals. Second, to ascertain what Coronial reports indicated about ‘real’ causes of death on a national, regional and local basis in order to improve healthcare standards. Third, to identify whether pathologists could help improve autopsy reports and assist with auditing perioperative deaths. Professional bodies like the Association of Anaesthetists and Surgeons and the Royal College of Pathologists and the Coroners’ Society agreed to co-operate with the NCEPOD to try to improve best practice. It was, however, the NCEPOD report for 1990 that would cause the most controversy by identifying that with respect to autopsy reports, ‘communications between pathologists’ (whether working in hospitals or with coroners) ‘and clinicians is so poor that useful lessons cannot often be learnt’. As a result, a Joint Working Party of the Royal Colleges convened in 1991. It recommended that there should be a more ‘systematic monitoring of the discrepancy rates between ante-mortem [patients’ health profiles] and post-mortem diagnoses’, with this vital clinical information being made ‘more widely available to consultants’.79 In other words, there was a recognition that explicit body disputes existed, they were generated by Coronial cases, and yet, not enough was being done to learn from them. Cases that attracted a lot of adverse publicity had therefore no balancing mechanism of a public gain for the medical scientific community. Bio-commons was not necessarily beneficial for everybody.
Further complicating this common situation was that central government defended its position about a lack of public health gains by pointing to better clinical audit procedures that were enshrined into the National Health Service and Community Care Act (Eliz. 2 c. 19: 1990). That new legislation had created self-governing NHS trusts, as well as GP fund-holding practices. They were now responsible for managing healthcare and welfare services in the community, including their financing.80 This was creating serious resource issues for the Coronial Office, with central government finance re-diverted to NHS frontline need. With less in local budgets for coroners and pathologists to spend, fewer healthcare lessons were passed on. The situation was a missed opportunity cost. It was becoming unaffordable for the dead to improve medical outcomes for the living. There thus remained uncertainty inside the reorganised NHS system as to whether autopsy results were in reality informing clinical practice or not, with many practitioners sceptical that they did so.81 Against this backdrop, the fact that autopsy rates declined significantly between the 1990s and the passing of HTA2004 appeared to be a worrying trend. Consequently, the NCEPOD in 2006 undertook a new investigation styled: ‘The Coroner’s Autopsy: Do we deserve better?’ Its ramifications were to be far-reaching.
The NCEPOD 2006 audit highlighted that the Broderick Report (1971)82 and the Lucre Report (2003)83 had both indicated that there were persistent problems with autopsy reporting procedures across the United Kingdom. It remained the case that as late as 2006 there was ‘no single body or department that oversees death certification and coroners’. Exacerbating this situation was the fact that ‘the service is part local and part national’. Although most pathologists worked for the NHS, ‘coroners are appointed by the Lord Chief Justice and come under the Department of Constitutional Affairs’. So even when a coroner and pathologist worked side by side, each had a different reporting mechanism, as well as different systems of audit and accountability. In addition, the Registrars of Death responsible for monitoring the accuracy of death certificates remained the responsibility of ‘the Office for National Statistics … under the aegis of Her Majesty’s Treasury’. The NCEPOD thus concluded: ‘There is no centralisation or unification of responsibility and accountability’ involving the Coronial Office. As a result, potentially many sorts of body disputes were being generated by a lack of communication, sporadic co-ordination, and ad hoc customary practices in Coronial autopsies, even post-HTA2004. They hence asked a pressing question: ‘What level of quality in the Coronial autopsy service does the public want?’ Answering this conundrum proved to be provocative because there was a mismatch between public perceptions and actual Coronial working practices of some longevity.
NCEPOD 2006 set out that there was a historical problem with the basic cost of autopsies to the taxpayer – a controversy stretching back to the 1830s – which had never been resolved.84 It had continually undermined the official reach of the Coronial Office in England and Wales. The public expected a high standard of service and coroners to be accountable, but such aspirations did not match adequate funding allocations. As NCEPOD pointed out, ‘when considering the variable quality of the current autopsy process, several pathologists and coroners commented: What do you expect for £87.70 [the current fee for a standard autopsy without further investigations]?’ Low fees meant spending no more than thirty minutes on an autopsy. Coroners paid pathologists to do their pathology work but had to factor in the opportunity costs associated with budget shortfalls. This had given rise to what this book calls a system of presumptions. That is, over time the public made assumptions about coroner/pathologist working relationships that did not match realities. For instance, most coroners on cost grounds continued to tolerate a certain level of amateurish procedures due to underfunding. Many autopsies had the official appearance of a forensic examination, but they are nothing of the sort, as the standard modus operandi of a detailed ‘post-mortem’ remained undefined in law. Consequently, the NCEPOD found that there were significant levels of misinformation inside the autopsy system, exacerbating a lack of clinical clarity. Very basic and routine mistakes happened a lot because of poor or illegible handwriting on rushed reports written hastily by coroners and pathologists. It was impossible to engage with autopsy outcomes because they were often indecipherable. In a digital age, this was unquestionably outdated and represented an opportunity cost for researchers to better engage with both the demographic and geographical subtleties of mortality rates in community medicine. Against this backdrop, the NCEPOD report in 2006 became the focus of a national debate about the future of the Coronial Office.
In 2005–6, the NCEPOD audited 114,600 autopsies (some 22 per cent of a total of 513,000 deaths that year) in which the Coronial Office was involved in England and Wales. In terms of those demographics, one headline announcement that was to shape media reaction was that ‘the advisors had concerns over the quality of autopsy examinations in the very elderly’. They concluded that ‘these were done less carefully than those on younger patients’. In an ageing population, this was a noteworthy trend, especially since anatomy teaching and research were reliant on the gerontology of necropsy bequests. There was little joined-up thinking between coroners/pathologists/anatomists of the sort that had characterised the Victorian era. A summary of the audit study also observed how:
One in four autopsy reports was judged as poor or unacceptable
In one third of mortuaries, the pathologist failed to inspect the body before the anatomical pathology technologist commenced opening it and removed the organs
In one in sixteen cases, it was deemed that histology should have been taken in order to determine the cause of death
In nearly one in five cases, the cause of death as stated was questionable
The extent of the examination of the heart, in those with abnormalities that might be due to cardiomyopathy (some of which are inherited), was poor
The extent of the examination of patients with known epilepsy who died unexpectedly was poor
There was poor recording of the presence of external injuries
The examination of decomposed bodies was of poor quality
There was poor communication between coroners and pathologists
There were significant gaps in the information provided to the pathologists by the coroner85
Since WWII, it ought to have been the case that Coronial necropsies were a potential ‘treasure trove of information’ (as this chapter argued earlier). Instead, ‘real causes of death’ remained ‘hidden because of indifferent post-mortem examinations’. Done hastily, they were often ‘obscured by deficient recording of data’. Such basic flaws had not been resolved for over fifty years.86 It was thus self-evident to many inside the profession why disputed bodies came about from the 1960s to the 1990s. As one coroner described it: ‘The system is confused chaos [run] more by default than by design.’ Hidden histories of the dead thus mattered and still matter for the living. For every explicit dispute, there needed to be a much better public health gain. Central government’s solution was to launch an inquiry into the power and palette of the Coronial Office, but this soon proved to be controversial too.
Around 2006, after the NCEPOD report was published, the media turned their attention to a central government proposal to create a new Chief Coroner for England and Wales. Extensive newspaper coverage debated whether this was justified on costs grounds or not. Central government proposed that the person appointed to the new role must get rid of a lot of wasteful bureaucracy and instigate a reformed system. Only this approach, it was argued, would begin to counteract explicit body disputes and the lack of public health gains: the latter was occurring on a regular basis. Everyone agreed with the NCEPOD main findings. Public health schemes should be better informed by Coronial statistics in a biomedical era. Yet, how this was to be counterbalanced with the desire to strengthen the impact of the Inquest process was unclear. What complicated the contemporary debates was that a global recession occurred in 2007. It would require a large budget to set up a new Chief Coroner’s Office at a time of severe government cutbacks. Exacerbating this budget issue was that after the Coroners and Justice Act (Eliz. 2 c. 25: 2009), there was an expectation that the new legislation would overhaul a Coronial system with three inherent structural problems. First, there needed to be unambiguous leadership at the top of the Coronial service to direct future policy making. This strategic focus should be in line with central government thinking and reflect the range of stakeholders that coroners had to work with on a regular basis, including the public, pathologists and the police. Second, there had to be a better system of public accountability that would involve streamlining diverse local working practices so that these were co-ordinated around strategic priorities to improve the Coronial service overall. Third, the devolution of funding and its historical discrepancies had to be rectified. What then complicated this tripartite juggling act was a political commitment in the new Bill. It promised to uphold a new Charter for the Bereaved, which ‘set out a range of service standards and consumer rights’.87 The general public wanted more medical information, better consultation and improved communication channels, with the option to appeal against a coroner’s verdict when, for example, ‘viewing a body’ or attending an Inquest.
In considering this insider/outsider set of stakeholders and their different perspectives, Alexander Pitman was one of a number of expert commentators who highlighted the inherent flaw with central government’s public engagement aspirations. He told the press, ‘The possibility remained that the Charter might raise expectations beyond the capabilities of the service, offering bereaved people a list of laudable but unenforceable empty promises [sic].’ The latter was discussed at length during the second reading of the Bill.88 In other words, the question of how to bridge rhetoric (legislation) versus reality (working styles) was a significant Coronial hurdle. As a result, a three-year consultation process began against the backdrop of the global financial crisis.89 The Coalition government (2010–15) threatened to cancel the new office of Chief Coroner to help meet the budget deficit, but then did another volte-face when confronted with concerted opposition by Parliaments’ Public Administration Select Committee, influential pressure groups such as INQUEST and the House of Lords. After much political wrangling, the new Chief Coroner, appointed from the judicial circuit, was told to prioritise cost analysis right from the start of taking up office in July 2013. Reviewing the subsequent annual returns of the reformed Coronial Office is instructive about how exactly the new changes would redress explicit body disputes, improve public health gains from Inquest information and streamline procedures that were still ad hoc in the regions. The simple answer is that this was an impossible task. Findings explain the longevity of ingrained problems with the power and palette of Coronial Office responsibilities, as we approach the conclusion to this chapter.
The Coroners’ Statistics Annual Report for England and Wales is issued in May each year as a Ministry of Justice bulletin. It is the main legal instrument by which leadership, accountability and devolved budgets of the Chief Coroner are measured. These three facets of the working portfolios of all Coronial offices also feed into the Office for National Statistics mortality figures. In 2015 some
234,406 deaths were reported to coroners … an increase of 12,565 (6%) from 2014 … [with] just under half (45%) of all registered deaths [being] reported to coroners … [in] the last ten years, this proportion has been generally consistent within the range of 45% to 47%.90
In terms of post-mortems, some ‘89,206’ were ordered by coroners, or ‘38% of all cases reported to them’. That said, not all post-mortems required that an Inquest come to court. Some are now ‘a paper inquest’ – a process that used to be known as a ‘non-Jury’ inquest in the past. In fact, since ‘1995, the proportion of post-mortem inquests has decreased by 23 percentage points, from 61% to 38%’. Examining those statistics in Figure 5.3, it is evident that there had been a decline in post-mortem work (broadly defined) after the mid-1990s, from 126,398 cases in 1995 to 119,610 by 2003. Yet after the passing of HTA2004, there was a further falling off of post-mortem work, with a downward trend of about 5,000 Coronial cases in every biennial accounting cycle. Chapter 6 will be exploring the impact of these trends on the work of pathologists, too. Meantime, the overall picture of post-mortems from 2011 to 2015 now has stabilised, with 95 per cent of all coroners’ cases requiring a standard post-mortem.91 Generally, 20 per cent required histology and 14 per cent toxicology (to ascertain class A drug or alcohol abuse, as well as poison from a drug overdose in cases of suicide). These are therefore the remaining potential explicit body disputes still in the system, though many have now been modified by the HTA2004’s fully informed consent provisions. It remains, however, to be seen whether public health measures will improve because the system is still not uniform, remains underfunded and still operates by a considerable amount of discretionary justice: we conclude by reflecting on these historical observations of some longevity from Part I (human stories of explicit disputes) and Part II (their creation by the Coronial Office) of this chapter.

Conclusion
Delays have been a very big problem, and they continue to be a big problem. If there is one thing that comes across my desk on a regular basis, which is more distressing than anything else, it is families writing, saying: Why has there been three years’ delay? Why has there been five years’ delay? Why has there been seven years’ delay? Why has there been no date? Why don’t I have a date for anything? When is my inquest going to be? What about my family? We are all distressed. One case came in my direction recently where the High Court had ordered a coroner to resume an inquest. He had decided that there was no need to resume the inquest, and was going to leave it at that. But the High Court decided otherwise. So they ordered the coroner to resume the inquest. Unfortunately that case got forgotten about. The papers got put on a shelf in the back of the office for six and a half years. When it was brought back, the family not surprisingly wanted a new coroner to conduct their inquest. I helped them, and they got one. So delays are really poor, and they need to be reduced.92
In a history of explicit disputes, it was the sense of more ‘extra time of the dead’ inside the Coronial system that created the context for families to become frustrated by the amount of bureaucracy involved. Many expressed cultural reservations about losing control of a loved one’s body, especially once the transplantation era opened. And, as the above quotation by the Chief Coroner for England and Wales confirms from 2013, this historical problem of procedural delays has not necessarily been resolved in the intervening years. Hence, in 2015 the Criminal Law and Justice Weekly reported that: ‘The most recent report of the Judicial Conduct Investigations Office showed 556 complaints were made about coroners in 2015–2016, up from 262 in 2014–2015 and 51 in 2013–2014.’ By way of example, they cited the following case:
Mary Hassell, senior coroner for Camden, Islington, Hackney and Tower Hamlets, in a letter to Camden Council, extracts from which were quoted by the Mail on Sunday last year, alleged bullying and intimidation by the Orthodox Jewish Community in the wake of her decisions to order autopsies against the wishes of some members of devout religions. Following investigation of a complaint against her, to the Judicial Conduct Investigations Office, the Lord Chancellor and the Lord Chief Justice concluded that Ms Hassell had not misrepresented or distorted the position in her letter, as had been alleged, and dismissed this aspect of the complaint. However, they found that her decision to disclose the ‘private letter’ to the media demonstrated a serious lack of judgment, amounting to misconduct, and issued a reprimand.93
This question of tense relationships with the media and what public statements an individual coroner could make has remained one of the most challenging for the Coronial service in its long history. Indeed, at the heart of the all the representative cases cited in this chapter involving organ donation cards was the problem of how to manage the bereaved wanting agency over their dead loved one, transplant stakeholders in NHS facilities and media interest in new biotechnologies, which was often intrusive at the most tragic moment in family life. It was no easy task for coroners to be public advocates and protect the privacy of the grieving. An added difficulty has been the way that coroners were appointed, and then authorised to work on an ad hoc basis. Again, as the Chief Coroner explained in 2013:
There are also signs of a lack of a modern approach amongst some coroners’ offices. I went to one coroner’s office in the north, I won’t say where, where there had been problems with delays, and they were using typewriters. That was a symbol, it seemed to me, of a problem of lack of organisation, and of efficiency. If you don’t have efficiency, you will have delays. You will put that case at the back of the shelf and forget about it because it is a bit troublesome. So there are procedural reforms which have a rather more modern look to them. They involve opening inquests in public, recording all the hearings, setting a date for the next hearing, hopefully the final hearing, at an early stage, and giving directions to experts to provide reports and statements within a short period of time. One coroner said to me: ‘I have a pathologist who’s a bit slow. Usually it takes her a year to produce a report.’ I said ‘That’s not a report. That’s a guess about what her notes mean’ [sic].94
The only way to resolve this situation is to acknowledge that coroners have, for far too long, relied on underfunded post-mortems, often scribbled down, frequently illegible, and these have represented missed opportunities for biomedicine to learn from the dead for the living with fully informed consent. Inside the system, any legal loopholes created by inefficient bureaucracy also shaped public misperceptions in the run-up to HTA2004 that medico-legal staff acted duplicitously with taxpayers that paid their salaries in the NHS. Most did not do so deliberately, but it was nonetheless the impression fashioned in the public imagination. Anatomists suffered from this situation too when their final certificates after cremation were not signed off efficiently or officially by the Anatomy Inspectorate during the 1990s, in some cases by as much as three years at the DHSS. It looked like they were as guilty as pathologists of working their way around the law, when in fact most had been meticulous. Anywhere inside the system in fact, where too many overlapping agencies had been created, gave rise to a potential pathway for a future body dispute – a trend that medico-legal officials lost public sight of. Some medico-legal staff took advantage of this situation to conduct ‘extra considerations’ – a slippery medical research term – that we can only glimpse happening in an imperfect historical record filled with gaps and paperwork consigned for shredding.
The case of Carol Morris (and many others like it) is hence symbolic of heightened disputes about when to ‘call death’ and who could officially vie for disputed body parts from the 1960s through to the end of the 1990s. Herbert Jones (who opened this chapter), for instance, expressed in writing to numerous officials, close friends and remaining relatives in his life his wish to donate post-mortem and give the ‘gift’ of new ways of seeing his body. Yet, once peri-mortem (at or near the point of death), he was frustrated by the Coronial Office involved. This was because he was (strictly speaking) one of the first legal suicide cases in Britain once any foul play and assisted suicide was ruled out: and the ramifications of that Coronial dilemma are still unresolved in Britain today. As we shall see in Chapter 7, the ethical boundaries between suicide and assisted dying remain very controversial – even more so than in Herbert Jones’s day. A painful prognosis like fatal cancer continues on many occasions to confound caring and understandably cautious medico-legal staff. Nonetheless, his explicit dispute is informative about the number of officials that had an official opinion in processes of decision-making. These actor networks could be very extensive indeed. Yet, it has always been vital for coroners to work collaboratively whatever the circumstances of their working-lives. Indeed, this is a commonplace situation that the Chief Coroner acknowledged in 2013, when he commented: ‘It is no good for the coroner to sit back in his office, with the typewriters clicking away in the next room. He has got to work with that rather peculiar triangle within which he has to operate.’95 Unquestionably, he elaborated, one of the main procedural difficulties is that:
A senior coroner is appointed by the local authority but not employed by them, so their line manager is the Chief Coroner, or possibly the Lord Chief Justice. Then you have coroners’ officers, employed by the police. Their line manager is a detective sergeant, or some other officer. Then you have administrative staff, who are employed by the local authority, and line managed by someone there.
In other words, there was, and has continued to be, a: ‘peculiar triangle and it only works if everybody is working together.’ The solution, the Chief Coroner believes, especially when dealing with disputed bodies and complaints about coroners on the rise, is: ‘talking about problems, making sure where there is a disciplinary problem in the office and getting that sorted out, keeping a review of cases on a monthly basis, discussing, collaborating’. The ‘balance of probability’ has always been decided by public engagement, and it thus remains one of the most important communication tools in explicit body disputes involving the Coronial Office.
In the next chapter, we thus explore in more detail why it was that pathologists got that balance wrong in their working-lives and protocols of medical research. We turn next to consider brain retention work because it is even more emblematic to families in body disputes than organs and tissues taken from those involved in tragic accidents like that of Carol Morris that were to make national and international headlines in transplantation with far-reaching consequences for medical law and bioethics. Our final substantive chapter is going to focus on missed disputes that involved research on the brain and its controversial nature in the modern era. For as professionals, pathologists looked very guilty of working their way around the law because the time constraints they operated with proved to be very different from those of everyone else in hidden histories of the body.
Introduction
On 15 March 2017, the BBC reported the controversial case of John Culshaw deceased. Greater Manchester Police (hereafter GMP) had retained his organs for over twenty years.1 An investigation found that there had been no official audit of his retained human material by the Home Office, despite HTA2004. The facts were that after Mr Culshaw was stabbed to death in Wigan on 23 October in 1993, Manchester Coronial Office appointed a senior forensic pathologist from Birmingham to his case. The bereaved family were not informed of the extent of the subsequent histopathology; effectively John Culshaw’s ‘stomach, liver and other organs and tissues had been retained after two post-mortem examinations’ – one to establish the cause of death and the other to gather evidence for a criminal prosecution of homicide. Contemporaneous and subsequent harvesting meant that around 50 per cent of his entire body mass had been taken, much more than was required to satisfy legal evidence standards in court at the time. The victim’s family meanwhile thought they had buried him mostly intact. The GMP thus told the press that they had ‘agonised over a number of months’ whether to tell the family or not that ‘a significant amount of extra human material of John Culshaw’ had been stored in a police laboratory ever since his death. On balance their ethics committee concluded that they had a moral duty to do so. The retentions had been before HTA2004 came into force, and were not therefore, strictly speaking, illegal. Nevertheless, GMP wanted to be transparent about the pathology error in keeping the body parts for so long without doing anything with them.
This chapter’s central focus is therefore a third type of body dispute compared to those we have encountered in Part II of this book so far. In Chapter 4 we examined disputes that arose because consent was implied but never done properly with incomplete post-mortem paperwork inside the system of bequest or donation that supplied anatomical schools and medical research facilities. In Chapter 5 we examined two further types of explicit body dispute involving the Coronial Office: cases in which loved ones wanted to donate a dead relative’s organs but were stopped by the coroner who owned the dead body in law if there was an outstanding legal case to be decided as a result of an unnatural death such as a fatal road accident. And another type involving cases where someone carried a kidney donor card but then after they died their body was harvested for the heart, lungs, brain, and other associated human tissue too. Taking these extra donations resulted in explicit body disputes between grieving relatives, coroners, their pathologists and transplantation teams needing more human material to save lives. In this sixth chapter we now explore missed disputes. A typical missed dispute, as we shall see, arose because of delayed, missing or withheld information about the extent of the harvesting of human material and its long retention period that relatives of each dead person expected to be kept informed about, but were not. Instead, pathologists involved in checking on causes of death for coroners often took the opportunity to harvest brains to do further research. Although families knew that some human material had been retained for legal purposes to secure a court conviction in cases of dangerous driving, homicide and manslaughter charges, not everything about the extent of human harvesting was disclosed. The Culshaw case that opened this sixth chapter is emblematic of that commonplace situation.
Like, therefore, our longer Chapter 5, which contained human stories to illustrate common dilemmas, this chapter is likewise divided into two parts. Part I sets in context the liminal space of medical death and how biotechnology made calling the time of death much more complex in the modern era. It was not an exact science as the ability to monitor even the smallest traces of life-signs in the brain-stem became feasible, complicating the medical ethics of death’s door. This discovery reflected the rise of neuroscience and its brain banking activities that became the new frontier of medical science in the late twentieth century. To appreciate how this new medical landscape gave rise to missed body disputes, Part II of the chapter investigates the controversial case of the Isaacs family, which created a national outcry in 2000 after it was found that Mr Isaac’s brain had been retained with 23,900 other brain material deposits for ten years or more without fully informed consent (themes first introduced in Chapter 2). Families missed an opportunity to know what was happening to the brains of their loved ones because of a controversial and covert system of brain supply by pathologists. For whereas brain banking usually was done with the consent of families, generally what was described by pathologists as brain accumulation and brain collection was not. It was thought that after HTA2004 those missed body disputes had been resolved, but by the time GMP in 2017 got in contact with bereaved families about human material they had held in forensic pathology facilities around the UK for a decade or more, the time gap between the rhetoric and reality of informed consent was obvious for all to see. We return, therefore, briefly here to the story of John Culshaw deceased that opened this chapter and the reaction of his grieving family to a missed body dispute since it is a historical prism of many of the themes and human situations which we will be exploring together in this sixth chapter.
Jenny Culshaw, mother of John Culshaw deceased, told the BBC that she was shocked to learn that so much of her dead son, who had been murdered in 1993, was still in closed storage in 2017, supposedly supervised by a senior Home Office pathologist for almost a quarter of a century. Had she known, she would have asked questions about what was happening and why. Instead, she now found herself involved in a missed body dispute. It was evident she had not been told the full material facts relating to her son’s fatality and subsequent criminal investigation in 1993. Being kept in ignorance for twenty-four years had prevented her from asking the right sort of questions and querying the ongoing situation. She knew that some human material had been taken because it was very necessary for a court case (and thus this was not an implied process of consent that she was objecting to); instead, it was the extent of human harvesting she was querying and the length of time such information was withheld from her, which she would have objected to had she known. As she put it:
He’s my son. And he’s been left – half of him – If he’d have died and they’d asked me if they could use his parts to help somebody, then yes. But just to be sat in a lab for 23 years doing nothing, that’s just horrendous – Somebody has made a big mistake. Not just me but a lot of other families are suffering as well – I don’t want anyone else going through this. It’s devastating.2
Further inquiries by a journalist working for the Manchester Evening News revealed that ‘180 dead victims of crime in Greater Manchester had been discovered during a recent audit of organ retentions’ under the official jurisdiction of GMP.3 Again, Jenny Culshaw questioned the reason that her son’s body had been harvested for so many organs that did not relate to how he had been murdered and could not therefore have informed the victims’ court case in 1994:
I thought I had buried the son that I gave birth to. In fact I buried a shell. Why? He was stabbed through the heart. Why would they need to retain other parts? We don’t know we’ve got everything back. That’s what we are panicking about. Are they going to come back and say they have found some more? The officer who visited us apologised to us. But there are other people out there suffering like I am. We have been visiting him at the cemetery every two weeks. But he’s not there. He’s not at rest.4
Jenny Culshaw was not alone. An audit of all human tissue stored on behalf of police forces around the country, carried out in 2012: ‘revealed 492 whole organs or significant body parts [like brains] were kept at police stations, labs and hospitals mortuaries on behalf of the police in murder or suspicious death cases’. These related to cases across England, Wales and Northern Ireland (Scotland has a different legal system). When pressed by angry families about missed body disputes (and their human parts), the Home Office took the view that: ‘this is an operational matter for the police’. In the case of GMP, its former Forensic Science Service came under the audit spotlight in 2014, leading to the rediscovery of John Culshaw’s potential missed body dispute. The description of his human material in clinical terms (‘one of 180 samples’) is noteworthy given our discussion in previous chapters about the need for the human life to be put back front and centre to the body ‘gift’ process. In this case, GMP appointed a dedicated team of detectives familiar with the original case files. They worked methodically to identify the retained human remains of all of their ‘police cases’ and to contact their respective families. A spokesperson for the GMP review confirmed to the Manchester Evening News:
In this case we have been to visit John Culshaw’s family twice and had several open and honest conversations with them. Every family we visited has reacted differently to this difficult conversation and in this case they were clearly upset by the news. As with all cases we have offered them specialist support and will continue to do so. We have now spoken to dozens of families and in many cases they have thanked us for the personal visit, but we accept that everyone reacts differently.5
In response, Jenny Culshaw told the press that there needed to be more human understanding of the impact that such delayed news would have on the majority of families. She refuted the accusation that her emotional response was either exceptional or excessive. Mrs Culshaw conceded that she was perhaps more outspoken than others about feeling pained, but all those she now knew in similar circumstances were equally shocked. Indeed, she and the other families resented the corporate-speak used to describe how the GMP press office was engaging with them in ‘open and honest conversations’. Repeating that phrase several times made it feel like the opposite was happening and the GMP staff were out of touch. The Culshaw family’s expectation was that HTA2004 had sorted out ‘all’ potential missed body and body parts disputes, not just in the NHS. Now they learned that John Culshaw’s human material was located at a forensic science laboratory in Birmingham:
Honestly, this has put 10 years on my life. We’ve kept this quiet because the detective who visited us said ‘don’t say anything until the other people have been told’. And we have kept it quiet until now. But I can’t cope with this all on my own. There’s somebody else out there suffering like I am. Somebody should be standing up and saying they have done this. We were never ever told anything had been kept from John. In fact, after the Alder Hey scandal my daughter wrote to the authorities to find out if anything from his body had been kept and she was told no. She did that for me. I don’t believe in cremation [Mrs Culshaw is a Roman Catholic]. We’re now going to have another burial on Thursday and put those remains in his grave.6
The Culshaw family went back to the original grave plot at Westwood Cemetery, Ince, in Wigan and held a second burial service, some twenty-four years after they had interred John Culshaw.
This story is emotive because it has a history of emotions and oral history context. For that reason, it gets to the heart of many of the core themes of this book. First, it alerts us to the multilayered material pathways, networks and thresholds that dead bodies once broken up did not simply travel along – from supplier to medical research facility – but also occupied for some considerable period, often forgotten time, in cold storage. Second, because this pathology system had to be confidential to secure convictions in court, it could also be secretive about everything that was being done and retained out of interest by pathologists. Third, this meant that spaces were created in which time stood still as harvested human material was held in refrigerated suspension for far longer than the general public expected to happen, notwithstanding the legal imperative of a pending prosecution. Fourth, the personalised history of each body (organs, parts, tissues and brain) may have faded from public view, but the identify of each did not dissolve altogether. That which was dissected and disaggregated could be – with a great deal of detailed detective work by the police – reassembled and re-identified when public tastes changed. Fifth, that outcome shows that bio-commons could have been documented by post-mortem passports in the first instance; if it was possible to reactivate human identities, it was equally possible to keep track of them inside forensic pathology facilities. It was therefore not impossible (as historically many inside the system claimed) to monitor working methods and paperwork protocols. Sixth, this finding represented a major public relations challenge for pathologists trained clinically to conduct their expertise because the feelings of families were a human checking mechanism that had never been a direct part of their standard workload allocations. As a result, the challenge for a historian of the body when assessing what was done and why is to rebalance hidden histories of the dead in these clinical settings with experiential perspectives after public exposure. Our approach is therefore that introduced in the conclusion of Chapter 3, namely, to build on Paul Thompson’s seminal book about the value of oral history, The Voice of the Past (2000).
Thompson argues that there needs to be a reconstruction of the written and spoken historical record because it ‘can give back to the people who made and experienced history, through their own words, a central place’.7 To do so, we must keep in mind Julianne Nyhan and Andrew Flinn’s important observation that it is essential to keep asking of oral histories whether or not they were or are ‘fatally compromised by the biases and uncertainties introduced by the interview process’.8 In other words, what we are going to do in this chapter is to subject the evidence base that came to light since 2000 to a ‘rigorous cross-checking with other sources, arguing for the general accuracy of memory and its suitability as a source of historical evidence’. For as Alessandro Portelli reminds us, oral histories when combined with histories of emotion can provide new perspectives often hidden from public view. Indeed, he is praiseworthy of what he called ‘the peculiarities of oral history’ and their subjectivity precisely because they are ‘not just about what people did, but [what] they wanted to do, what they believed they were doing, and what they now think they did’.9 This conceptual approach is pivotal to this chapter’s method of listening to both sides – the clinical (by pathologists) and emotional (by the families) – to arrive at a consensus about what the balance of the evidence is telling us. For as William Reddy points out, the advantage of exploring the navigation of feelings is that historians of emotions can appraise the extent to which giving voice to a set of difficult experiences gives those involved a greater awareness of their fragility in trauma, or an ability to cope in a difficult personal crisis. Often it provides the chance to reconcile difficult circumstances which can produce a more philosophical outlook and thus a positive set of outcomes from something that was imposed but can be accommodated by the person or people involved.10 In other words, we can assess did people feel worse, about the same, or much better than they thought they might once hidden histories of the dead and their missed body disputes about brain harvesting were revealed for the first time. And what do those discoveries tell us about the changing shape of cultural attitudes to the body and its material afterlives in a Genome era? It is exactly this set of human scenarios that we will encounter as we appraise the Culshaw story with others like it, and encounter those spoken by pathologists at the time, too. For the Culshaws’ position (as was inferred in the oral history evidence) was not unique.
It soon came to light in the national press that: ‘the Police Service of Northern Ireland kept the most samples with 71 items, West Midlands kept 30, Metropolitan Police 39, Merseyside 37, Cambridgeshire 35 and West Yorkshire 31’.11 These had been located after an investigation was ordered following the discovery that ‘many criminal investigations failed to record accurately why human material had been kept’. In response to the public furore in the media about this finding in 2017, all the families involved stated they would have wanted to have been kept informed about material retentions, whether in the past, present or future. The majority spoke to journalists about the emotional ‘bolt out of the blue’, ‘the shock of not knowing’, and ‘the knock at the door telling us we did not know what had really happened’ after so many years.12 Those who learned their dead child was part of the ‘sample size’ were understandably very upset indeed. In the cases of body parts retained from ‘90 children’ often involving their brains, it was being misinformed that bereaved parents objected to the most. Hannah Cheevers was one bereaved parent. She told BBC Radio 4’s Today Programme how after her baby son died of heart failure, she and her husband assumed they had buried him. Then one day a police officer came and told them: ‘totally out of the blue. … We had his funeral, we got on with our lives as you have to and 13 years later we have a knock on the door from the Dorset police to inform us that his brain has been retained at Southampton hospital.’13 There were no suspicious circumstances surrounding their child’s death and therefore his brain retention had no legal justification or the family’s consent for over thirteen years. Hannah, like Jenny Culshaw, was not against donation. It was the lack of consultation which was objectionable. Now she too was involved in a missed dispute. She felt this outcome was very sad, since: ‘We had absolutely no idea that they had kept his brain.’ Indeed, the Cheevers family, despite the controversy, ‘decided to donate his brain to hospital research, rather than have it destroyed or reburied after another funeral’. Hannah told BBC News that the family decided they ‘did not want to disturb his human remains again’, even though they were very heartbroken by the hidden history of what had happened.
These symbolic but not unrepresentative cases attest both to the emotive nature of not being informed and to the almost universal feelings of revulsion felt by most people when missed disputes were exposed to public enquiry. Since these missed disputes often involved brain retentions, we need to engage with two practical factors before we encounter more human stories and engage with their historical lessons in hidden histories of the dead. First, why was medical death so confusing after WWII, and how did that context shaped brain banking and brain collecting that led to so many missed disputes? Part I now outlines that pivotal medical landscape, before Part II takes up their human stories again.
Part I
Medical Death’s Dead-End?
Contrary to perception, death is not a specific moment but a potentially reversible process that occurs after any severe illness or accident causes the heart, lungs and brain to cease functioning. If attempts are made to reverse this process, it is referred to as ‘cardiac arrest’; however, if these attempts do not succeed it is called ‘death’ [Sam Parnia, Professor of Critical Care Medicine and Director of Resuscitation Research at the State University of New York at Stony Brook, USA, 2014].14
In April 2016, National Geographic opened with a lead article that posed a thought-provoking medical question: ‘Is Science Redefining the Boundaries of Life and Death?’.15 The answer was a resounding yes, thanks to new, sophisticated technology. An investigative journalist explained that once society accepted that death was a physical set of processes (based on a growing body of empirical evidence in emergency room medicine), the boundaries of when that occurred in medico-scientific parlance were always going to shift. This new status quo had prompted a Harvard University panel of experts in 1968 to look at the two ways death had been defined since the eighteenth century: ‘the traditional way, by cardiopulmonary criteria, and a new way, by neurological ones’.16 Their conclusions led to a new recognition that death in the brain mattered just as much as death in the heart and lungs. Evidence showed how, unaided and without extra oxygen, the brain could still survive for about three minutes even after the heart had stopped and the lungs had ceased to inflate. Consequently, ‘brain death’ in medico-legal circles now had ‘three cardinal benchmarks’. These included: ‘coma or unresponsiveness, apnea or the inability to breath without a ventilator, and the absence of brainstem reflexes’; these have tended to be ‘measured by bedside exams such as flushing the ears with cold water to see if the eyes move, poking the nail bed to see if the face grimaces, or swabbing the throat and suctioning the bronchia to try to stimulate a cough’. Therefore, death acts like a dimmer switch in the body; it can be turned down in trauma, but that does not mean that the light of life has expired in the brain or vital organs. Quoting Dr Sam Parnia (who opened this section), the article observed:
Death is ‘a process, not a moment’, writes critical-care physician Sam Parnia in his book Erasing Death. It’s a whole-body stroke, in which the heart stops beating but the organs don’t die immediately. In fact, he writes, they might hang on intact for quite a while, which means that ‘for a significant period of time after death, death is in fact fully reversible’. … He says ‘CPR works better than people realize and that under proper conditions – when the body temperature is lowered, chest compression is regulated for depth and tempo, and oxygen is reintroduced slowly to avoid injuring tissue – some patients can be brought back from the dead after hours without a heartbeat, often with no long-term consequences’. Now he’s investigating one of the most mysterious aspects of crossing over: why so many people in cardiac arrest report out-of-body or near-death experiences, and what those sensations might reveal about the nature of this limbo zone and about death itself.17
Yet, the interesting thing about this storyline was the reaction to the online newsfeed by regular readers of National Geographic. Some subscribers blogged that they thought the evidence presented of a number of cases in which patients had been brought back from the dead many hours after they seemed to expire in the emergency room was disturbing. Others dismissed the notion of a Near-Death Experience (hereafter NDE) calling it pseudo-science. Many more believed that this NDE grey zone proved life after death existed in some form and thus validated how many people had a spiritual faith in the global community. Few, however, expressed an opinion about the reporting of the history of resuscitation and whether ‘the facts’ as presented in the article were reliable or not. Although the reportage did not intend to mislead, it did not cover just what a long and disruptive issue medical death has been in the history of anatomy: an important context for this chapter’s central focus on the role that medical death and brain research would play in creating missed disputes by the turn of the twenty-first century.
Recently, historical scholarship has established that English penal surgeons had been very troubled by when to call medical death since at least the mid-eighteenth century. As this author has argued extensively elsewhere, those medical men who were given the task of dissecting criminals convicted and hanged for murder on the gallows under the Murder Act (25 Geo. 2. c. 37: 1752) found that in the winter, cold corpses that should have been dead could be revived when cut down from the hangman’s rope.18 Hypothermia in the body protected the brain, heart and lungs from expiring, and when warmed up the deceased began to wake up in the dissection theatre. Since they were socially dead (having committed homicide), legally dead (being condemned in court and hanged in public) but not medically dead (still having life signs in the body), the only solution was to transport the convict for life to the Americas or Australia. Somewhere today there are the ancestors of condemned criminals who are living proof that the boundaries of life and death have always been fluid. This unforeseen outcome seldom features in standard historical accounts, so it is perhaps unsurprising that such findings have not informed modern debates concerning when death really occurs. In other words, from the eighteenth to the twentieth century medicine behind closed doors knew about the complexities of ‘calling the time of death’. Indeed, one physical factor that eighteenth-century surgeons encountered regularly, which twenty-first-century consultants in emergency medicine know to be a physical fact, is that to keep the brain-stem alive, effective oxygenation of the bloodstream must be sustained in trauma. It is best to start oxygenating the blood at the point of injury, even before ambulance transfer. This is because biomedicine really does work best when it is as easy as breathing. That discovery has complicated today when exactly to call the time of death. For traditionally doctors used to call the time of death at twenty minutes in emergency rooms around the world. That was when they accepted the flatline of the heart as proof of medical death. There seemed little point in continuing to do compressions or jolt the heart with an electrical stimulus beyond the twenty-minute marker if the brain was beyond repair. The person in trauma would be in a vegetative state, functioning on a heart-lung machine but not capable of an independent quality of life. This customary practice, however, started to run counter to the new capabilities of medical technology. From the 1980s, it was feasible to monitor even the very faintest traces of life in the brain-stem. Sophisticated equipment began therefore to elongate the timing of medical death. In resuscitation medicine, the twenty-minute marker looked outdated. Thus, in the recent past, saving a life involved oxygenating the brain-stem and reviving patients thought dead. This discovery has redrawn the fine line we all will cross one day into our individual deadlines. In other words, by the 1960s research facilities around the world reliant on brain material to advance neuroscience now faced new practicalities, and medical ethics had to respond in kind.
In 1968 (as we have seen) invited scientists, anaesthesiologists and experts working at the forefront of emergency medicine, as well as leading ethicists and a medical historian, convened at Harvard University. They styled themselves the Ad-Hoc Committee on Brain Death (hereafter AHCBD) and assembled at Harvard Medical School. Their remit was to review and make new policy recommendations concerning the changing ethics of ‘irreversible coma’ and shifting medico-legal definitions in a biotech world.19 The AHCBD concluded that in a non-functioning brain, permanent death needed a clinical description of ‘brain death’, re-defined in three diagnostic ways:
1. Unreceptivity and unresponsitivity – patient shows total unawareness to external stimuli and unresponsiveness to painful stimuli
2. No movements or breathing – all spontaneous muscular movement, spontaneous respiration and response to stimuli are absent
3. No reflexes – fixed, dilated pupils; lack of eye movement even when hit or turned, or ice water is placed in the ear; lack of response to noxious stimuli; unelicitable tendon reflexes20
However, because there was also a considerable weight of medical evidence that some bodies in hypothermia or after drug intoxication could sometimes be revived in the brain-stem and still had a beating heart, a fourth checking mechanism was required, too. Each patient had to have an electroencephalogram (EEG) and two experts in resuscitation medicine to check the reading. They had to agree that the person was deceased and could potentially be part of an organ donation scheme, provided, that is, they met the new medico-legal protocol steps 1–3 plus EEG. A patient was only then essentially ‘brain dead’ and this diagnosis defined their end of life, rather than a non-beating heart. The hope was that this new diagnostic tool would separate out ‘brain dead’ patients from those in a ‘persistent vegetative state’: the latter can still physically experience cycles of sleep and wakefulness despite being in a deep unconscious state.21 A priority was to protect transplant surgeons against accusations of killing patients during technical procedures when the heart had to be stopped to be transferred to a donor or a kidney was taken from a so-called ‘living cadaver’ on life support until the transplant was complete. In medico-legal circles ever since, the AHCBD meeting became renowned as a landmark ethical event.22 It also stimulated considerable controversy.23
From the outset, critics observed the close links between the AHCBD report and organ donation schemes in Intensive Care Units (hereafter ICUs). Collected evidence from around the medical world seemed to indicate that the majority of ‘brain dead’ patients became ‘solid organ’ donors (heart, lungs, kidneys and liver). Harvesting of on average four donations per dead donor soon became the norm. Other ‘donors’ became ‘tissue transplants’ (eyes, bone grafts and general human material). Sceptics questioned therefore the degree to which ‘the dead donor rule’ was ethical. Did it effectively drive up donation rates? It looked like those involved in transplantation actor networks could have been motivated to improve biotechnology, rather than promoting medical altruism (in that order of priority). For this reason, the AHCBD report, whilst influential, did not create a global medical consensus about an agreed precise timing of ‘brain death’. Consequently, the US government convened a President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioural Research in 1981. The aim was to look again at patients who seemed to be ‘beyond coma’. This diagnostic emphasis stressed that it was ethical to explore when the ‘whole of life’ appeared to have ended in a patient in deep trauma. As Margaret Hayden, bioethicist, explains: ‘The report’s other reason for this new definition was equally pragmatic, stating that patients in irreversible comas (with beating hearts but irreversible brain damage) could place an undue burden on families and hospitals.’24 The review group hence concluded that the holistic essence of life is in the brain. Hayden elaborates that in 1981 the President’s Commission drew ‘on both biological and philosophical premises’ concluding that:
death is the moment at which the body’s physiological system ceases to constitute an integrated whole. Even if life continues in individual cells or organs, life of the organism as a whole requires complex integration, and without the latter, a person cannot properly be regarded as alive.25
In other words, brain research and advances in emergency medicine were dealing with a new reality – death’s door stayed open for longer than many skilled medics cared to admit in public – and on its threshold were the living-dead which required new protocols. Soon, the 1981 President’s Commission findings were being enacted across America.
Forty-five US states adopted a definition of ‘total brain failure’ under new legislation known as the Uniform Determination of Death Act (1981) (hereafter UDDA). Again, however, critics like Hayden point out: ‘Much of the clinical guidance is designed to mitigate and mask the ambiguity between what a brain dead individual looks like (well-perfused, warm skin, with a beating heart) and how we expect a dead body to appear (grey, “lifeless,” with no heartbeat or pulse).’26 Often ICU staff reported on families feeling upset and confused about being informed their relative was ‘technically alive’ and not knowing what exactly this meant clinically. Thus, the UDDA had provided a useful working-protocol, but families trusted their instincts too and this led to a cultural stand-off, sometimes culminating in body disputes. What further complicated the separation of life from death by the Millennium were new clinical findings highlighted by Dr Caroline M. Quill, the lead author of a disquieting study into ICU practices across the USA. These were co-ordinated by the Pearlman School of Medicine at the University of Pennsylvania. As NBC News explained in May 2013: ‘If you land in an intensive care unit sick enough for doctors to consider withdrawing life support, be warned – Whether and when to pull the plug may depend in large part on the practices and culture of the ICU itself …’
Quill and her team analysed records of more than 269,000 patients treated in 153 ICUs in the United States between 2001 and 2009. Overall, nearly 12 percent of patients had a decision made to go from a ‘full code’ – an all-out effort to save lives – to some kind of limit on care. That could have included: a DNR or do-not-resuscitate order; an order to withhold CPR or cardio-pulmonary resuscitation plus removing mechanical ventilation; dialysis or other life-saving treatments; or simply an order to provide only comfort measures or hospice care. About 59 percent of the patients died in the ICU and another 41 percent survived to discharge, the study found. Particular patient characteristics accounted for most of the variability in decisions to withdraw life support, Quill acknowledged. But even after age, illness, functional status and other factors were analysed the variation among ICUs to authorize a DFLST – decision to forgo life-sustaining therapy – was striking.27
Dr Douglas White, an Associate Professor of Critical Care Medicine and Director of the Ethics of Critical Illness at the University of Pittsburgh, likewise pointed out that often ‘decisions about whether and when to withdraw support are not scientific ones’. Hence, patients should be encouraged to talk much more openly about what they would want to happen in a critical situation at the end of life and leave a legal will stating their healthcare wishes. Yet, many in the recent past felt unable to do so; others put off the inevitable, or hoped their families would take over, often with mixed results, as an anonymous nurse working in ICU explained to NBC News:
Speaking as a registered nurse in a hospital myself, the choice to withdraw life support is one of the hardest decisions to make during the crisis. Often times what I see is not so much that the person in crisis isn’t ready to go, it’s usually the family isn’t ready to let go. I once had a patient wheeled up to floor who looked me in the eye and said: ‘I want to die’. He had stage 4 cancer with no chance of treatment, his body was starting to shut down little by little, he was confused but not THAT [sic] confused. So, because of the ‘confusion’ he had to depend on his family to withdraw life support. They didn’t want to. So, instead of letting the man go with some dignity, he ended up tied to a bed for trying to pull his lines out, he ended up with an infection as his body had stopped fighting off invaders, his kidneys had stopped working properly so he gained water weight from all the IV antibiotics we gave him. A few days later he did eventually pass. I just remember thinking, instead of being able to die peacefully in his right mind, he had to beg every day to die, live through the torture of feeling his body shut down piece by piece, and what was accomplished? Nothing. People deserve to die with dignity and honour, and sometimes life support is a curse.28
Even so, a further complicating factor was advances in emergency medicine during the same period.
In April 2013, Sam Parnia expanded on his hands-on experiences of medical death. In The Lazarus Effect, he wrote about how after training in resuscitation medicine at Guy’s and St. Thomas’ hospitals in London and then becoming head of ICU at Stony Brook University Hospital in New York, he observed that:
The one thing that is certain about all of our lives … is that we will all eventually experience a cardiac arrest. All our hearts will stop beating. What happens in the minutes and hours after that will potentially be the most significant moments of our biography. At present, the likelihood is, however, that in those crucial moments we will find ourselves in the medical environment of the 1960s or 1970s. The kind of CPR (cardiopulmonary resuscitation) that we are familiar with from medical dramas – the frenzied pumping of the chest – remains rooted … in its serendipitous discovery in 1960. It remains a haphazard kind of procedure, often performed more in hope than anticipation. Partly, this is a question of personnel. Most doctors will do CPR for 20 minutes and then stop. … The decision to stop is completely arbitrary but it is based on an instinct that after that time brain damage is very likely and you don’t want to bring people back into a persistent vegetative state. But if you understand all the things that are going on in the brain in those minutes – as we now can – then you can minimise that possibility There are numerous studies that show that if you implement all the various resuscitation steps together you not only get a doubling of your survival rates but the people who come back are not brain damaged.29
In other words, the culture of ICU functioned with an out-of-date historical concept of life and death: as Parnia explained at the start of this chapter’s Part I. Such basic findings reflect how much medicine has been about looking forward, not back: criticisms which echo those of George Steiner discussed in the Introduction. He highlighted that science’s methodologies have a fundamental flaw. Discarding ‘old knowledge’ happens routinely with each new medical breakthrough. By contrast, the medical humanities seldom casts off accumulated human experiences or their arts forms, recognising instead that the potential remains for the revival of old ways of thinking in a future context.30 Kwame Anthony Appiah (philosopher, cultural theorist and novelist) said the same thing during the recent Reith Lectures for the BBC. He observed once more: ‘Although our ancestors are powerful in shaping our attitudes to the past’ and we need to always be mindful of this, we equally ‘should always be in active dialogue with the past’ to stay engaged with what we have done and why.31 In many respects, mapping hidden histories of the body is an important way to reveal the flaws in medico-scientific methodologies, as this book and others by this author have done for the first time.32 They reiterate that an eighteenth-century surgeon and his twenty-first-century equivalent in ICU face the same ethical dilemmas. It is not therefore the case that ICU has been too respectful of historical concepts of life/death, as many claim today in resuscitation medicine and standard historical studies.33 What has really happened is that ICU never engaged with its own past practices. They thus lost sight of the working protocols of their surgical predecessors dissecting in the Georgian period. Eighteenth-century criminal surgeons first discovered the extraordinary capacity for resuscitation in the brain, even after it sounded like the heart had stopped beating in the chest cavity of a hanged criminal. Sam Parnia has therefore returned to old medical questions with renewed biomedical capabilities. In so doing, he alerts us to two important factors on missed body disputes of the modern period – that the brain was the frontier of medical research and that we know less than we should have done of its harvesting networks. To appreciate the importance of this context for our human stories later, it is important to reflect briefly on the dominance of neuroscience in our biomedical world.
Brainstorming Neuroscience
We have a brain, and people without brains don’t have thoughts. So the brain must do it. It’s a huge problem to discover how it does it, but that will come. There’s no alternative.34 [Professor Colin Blakemore, Chair in Neuroscience, University of Oxford, quoted in ‘Brain research’s golden age’, BBC News Magazine, 22 June 2011]
Few scientists would disagree with Professor Colin Blakemore that brain research has become the medical frontier in a biomedical age across the global community, and a timely one. As the Brain Research Trust highlighted in 2016, ‘over 12.5 million are affected by neurological conditions in the UK (that’s one in five)’.35 The medical charity’s online promotional video explains that: ‘the brain is the most complex organ in our body – it weighs just 3 pounds – yet it controls our emotions, senses, and actions – it’s how we process the world around us – so when it breaks down, we break down’. In a similar refrain, Carl Zimmer explained how in 2014 he surveyed the most innovative brain research for National Geographic across America:
Some neuroscientists are zooming in on the fine structure of individual nerve cells, or neurons. Others are charting the biochemistry of the brain, surveying how our billions of neurons produce and employ thousands of different kinds of proteins. Still others … are creating in unprecedented detail representations of the brain’s wiring: the network of some 100,000 miles of nerve fibres, called white matter that connects the various components of the mind, giving rise to everything we think, feel, and perceive. The U.S. government is throwing its weight behind this research through the Brain Research Advancing Innovative Neuro-technologies (BRAIN) Initiative. In an announcement last spring, President Barack Obama said that the large-scale project aimed to speed up the mapping of our neural circuitry, ‘giving scientists the tools they need to get a dynamic picture of the brain in action.’36
In many respects, new digital technology entrepreneurs and their personal computer revolution have also been leading the way globally, too. One such is the late Paul G. Allen, co-founder of Microsoft with Bill Gates. He created the Allen Institute for Brain Research in 2003 with a philanthropic donation of $100 million. Subsequently, Allen donated another $400 million to ensure that brain research remains an ‘Open Science’. His window-on-the-world legacy is a data portal known as the Allen Brain Atlas – ‘part of a 10-year plan launched in March 2012 to understand the neural code—how activity in the brain’s cortex leads to perception, decision making, and ultimately action’. His foundation thus promises: ‘We will be focusing our understanding through simultaneous study of the brain’s components, computation and cognition.’37 Allen, before his untimely death (he died of septic shock related to a terminal cancer diagnosis), was the personification of an Idea Man (the fitting title of his 2012 memoir), for he has taken up the anatomical legacy of the past and pushed it forward into a neurological future he often described in his public speeches as ‘What if’. It is a motto penal surgeons working on the dark science of the brain were once very familiar with in the past, too. They punished the ‘dangerous dead’ in popular culture and found that around 25 per cent of criminals hanged came back to life on the dissection table across England between 1752 and 1832.38 Continually, the boundaries of life and death shifted in the anatomy theatre. They proved to be more fluid than conventional European science traditionally thought over the next two centuries. So much so, that with the advent of biotechnology and the rise of neuroscience, the boundaries of life and death came into even sharper clinical and research focus, revealing differential power relations depending on claims of scientific expertise. And even though this remarkable work on the brain looked like it was robust, this was not necessarily the case. One example stands in for many at the time, and it explains why the general public started to become more sceptical about missed body disputes involving brain retentions once they came to public attention in modern Britain.
On 6 July 2016, Forbes magazine asked its readers to think the unthinkable – ‘Could Brain Research from the Past 15 years Really Be Wrong?’ The lead article, penned by Bruce Lee (Assistant Professor of International Health at Johns Hopkins University Bloomberg School of Public Health) highlighted how three researchers from Linköping University in Sweden had published a startling neurological study in the Journal of the Proceedings of the National Academy of Sciences of the United States of America.39 It explored the use of Functional Magnetic Resonance Imaging (fMRI) in brain research. This was a twenty-five-year old piece of technology and surprisingly few researchers have ever asked: Does it actually work properly, and have its research results been reliable? Essentially, the Swedish research team found a flaw in the operation of software used to detect brain activity, tracked under fMRI scans. As Lee explained:
Anders Eklund, Thomas E. Nichols and Hans Knutsson examined fMRI data from 499 healthy patients and found that the software (i.e., SPM, FSL and AFNI) used to generate the fMRI images often showed parts of the brain lighting up when it shouldn’t have, in some cases up to 70% of the time (i.e., a false positive rate of up to 70%). These software packages had bugs or glitches in them that were leading to faulty images and may have existed for 15 years until they were recently found and corrected. This means that up to around 40,000 fMRI studies published in the scientific literature over this period could have shown incorrect results.40
Soon Lee’s article made medical news around the world because as he asked: ‘Why wasn’t this software glitch caught earlier?’ There were ‘Several Reasons’, he explained –
First, there is not enough research being done on the software used for medical research and how to improve or develop new software. Secondly, scientific journals often will not publish studies that try to recreate already-published studies. At the same time, funders may not support research that tries to recreate other people’s research. This means that once a study is published, others may have no incentive to check or re-do the study. Instead, we need to change the system to encourage people to test and re-test scientific hypotheses and findings. Like a new fashion, scientific ideas are sexiest when they are first demonstrated, and then the scientific community quickly loses interest afterwards. But the first person to find or study something is not always right.41
In other words, in brain studies leading researchers had taken their own working histories for granted. Science Alert likewise highlighted that although scientists thought they were measuring brain function using fMRI, what they had really been doing was interpreting data produced by a machine, not the actual human brain. In other words, ‘Software, rather than humans … scans the voxels looking for clusters [of brain activity]. …When you see a claim that “Scientists know when you’re about to move an arm: these images prove it,” they’re interpreting what they’re told by the statistical software’ – an important data distinction.42
The particular computer software bug that the Swedish study identified was located and repaired in May 2015. Even so, it had skewed the results in some 40,000 published papers since the 1970s. As the Swedish team explained: ‘One of the biggest obstacles has been the astronomical cost of using these [fMRI] machines – around US$600 per hour’. Thus, ‘studies have been limited to very small sample sizes of up to 30 or so participants, and very few organisations have the funds to run repeat experiments to see if they can replicate the results.’43 An added problem had been ‘that because software is the thing that’s actually interpreting the data from the fMRI scans, your results are only as good as your computer, and programs used to validate the results have been prohibitively slow’. Debates and disputes should have been happening on a more regular basis inside the medical research community about the status of the science involved in brain work, and what this might have meant for public relations in terms of brain bequests. But this was not the case. To appreciate that context, and why it would later give rise to missed disputes, it is necessary to focus on the advent of brain banking because this provided the backdrop for future NHS scandals over retentions.
Cambridge University in the 1970s was the centre of new directions in neurosciences. In particular, it started to attract talented researchers interested in neurodegenerative disorders such as Huntington’s disease. By 1975, a consortium of these researchers had come together to form what became known as the Cambridge Brain Bank. Not only was this one of the first research facilities in the UK, but one of only four in the world at that time. Its nearest geographic rival was an early brain collection set up by Professor John (Nick) Corsellis (1915–1994) at Runwell Hospital in Essex during the 1950s which contained over 6,000 specimens from patients suffering from psychiatric illnesses, as well as neuro-degenerative diseases. However, although Corsellis shared brains with other leading researchers from time to time, his main research focus was brain collecting for his own use, rather than brain banking (in the latter, brain tissue is shared routinely for distribution amongst the research community). What made brain banking a new trend at Cambridge, and elsewhere, from the 1970s was the discovery that enzymes in brain tissue could be studied chemically post-mortem. So, for instance, in the case of dementia it was feasible after death to still study the enzymes active in brain tissue and reach meaningful results to potentially make better drug treatments. At a recent Witness Seminar run by the Wellcome Trust in London, Professor Gavin Reynolds described what it was like to be a young researcher and to acquire brain material at Cambridge in the 1970s:
… we were often seen, I think, as sort of eccentric scavengers. In Cambridge I, or my technician, used to go downstairs to the mortuary and negotiate over brains. This was, of course, in the days when this sort of thing was rather more possible. We could discuss the opportunity that we might be able to provide some pathological feedback in exchange for having these brains that we could then bank and formally provide for those who in the future wished to withdraw. But it was very much a sort of negotiated process, wasn’t it?44
Likewise, Professor David Mann elaborated on how a brain bank was set up in Manchester too and for what research reasons. Although lengthy, his explanation is worthwhile quoting in full, as it sets the scene for the Isaacs Report that we will be encountering later in this chapter. This was the typical sort of research pathway and actor network in pathology and new neuroscience that we have been rediscovering throughout this book:
We wanted really to follow this up in a large number of cases, and getting cell biopsies and the right amount of material from cell biopsy was really not easy to achieve. So we looked and said: ‘How can we use post mortem material to answer that question?’ In Manchester we set up a system whereby we obtained pre-mortem consent to brain recovery with the relatives fully involved when the whole situation was explained to them. They gave their agreement that we could obtain the brain tissues as soon as the patient died, so we weren’t hidebound by this ‘green form’ paraphernalia that so besets us nowadays. And the net effect of that was that I would make journeys across Manchester at 2 o’clock in the morning to Prestwich Hospital, a big psychiatric hospital at the time, where many of the patients were resident. There, I would meet the local mortician and we would extract the contents of the head from these individuals who had kindly agreed to donate the tissues for research, and I would hot foot, literally, across Manchester back to the University of Manchester laboratories, where we would dissect the brain and put it into these wonderful containers that David and Paul had devised, which contained preservative fluids. The next day the brain would find its way, courtesy of British Rail, down to Queen Square, and Paul will love to tell the tale that I would ring him up at some unearthly time in the day or night and say in my best Yorkshire voice: ‘Hello Paul. There’s a brain on a train for you.’ [Laughter] And really, as Paul says, it was the chemistry that drove the need not only to collect brains, but to collect brains of better quality than those you could simply get hold of from pathological archives, where everything had just been stuck willy-nilly into preservative. It was a rather surreal experience carrying really warm brains across a city at 2 o’clock in the morning.45
Mann was pressed for his views on what he believed the general public thought about this sort of brain research at the time. He replied: ‘I think actually it was not in the public perception until the Alder Hey story broke and then the stuff really did hit the fan at that time. That really did impact upon brain collections and brain donations.’ It was his perspective as a young researcher that: ‘I think, by and large, people had an understanding of why it was necessary to collect brains and were happy to participate in that process, but with the Alder Hey scandal, the whole notion of pathologists became people who kept things in cellars and dark rooms. We were tarnished badly by the whole business.’46
Other participants at the same oral history event spoke up for the first time concerning their personal feelings about Alder Hey. As Professor Margaret Esiri explained: ‘I felt very, very undermined by it. I felt the media portrayed it in the wrong way.’47 She elaborated that:
I felt we were the victims of a system that involved particularly coroners’ post mortems, which had nothing to do with the hospital system, where we had what we called medical interest post mortems and that often contributed to the brain banking as well. That was completely different to the coroner system where the problem was, I think, that the coroners never really explicitly said what you should do with an organ after you’d examined it for their purposes, which was to find the cause of death.48
These ethical issues were exacerbated, she explained, by a lack of communication. There were too many overlapping agencies involved. As a consequence, missed disputes occurred routinely in what was a fundamentally flawed coroner/pathologists’ set of procedures: ‘So [hospital] departments ended up with a lot of organs that they’d taken from coroners’ cases, and they didn’t know what to do with those organs afterwards.’ This was the complex cultural context that the Culshaw family experienced, too, in this chapter’s opening story. In order, however, to assess the historical value of these oral histories taken from a pathology perspective, and engage with the navigation of their feelings too, to balance the evidence of clinical and family lived experiences, it is necessary to understand a little bit more about the history of brain banking. In particular, we are going to focus in on the detailed activities of the Cambridge Brain Bank because it was pivotal to the actor networks of pathologists across the country and set new research standards that came in for significant public criticism involving many potential missed disputes after WWII.
Brain Banking
In 2003, the Department of Health (DofH) decided to investigate the controversial issue of brain retention in the post-war era. The research focus soon fell on the Cambridge Brain Bank because it was of national importance. Civil servants examined its paperwork processes and pathology records. The results of their findings are summarised in Table 6.1. In total, ‘2,547 … whole brains’ were banked for research purposes between 1980 and 2001, something that can be confirmed by cross-matching to Addenbrooke’s Hospital pathology records. The DofH report concluded that: ‘The Cambridge brain bank evolved from research undertaken by Dr. Bird in the Neurochemical Pharmacology Unit in the early 1970s. The first research was into Huntington’s Chorea (now referred to as Huntington’s disease).’ Having explained that context briefly, the report went on to state its broad findings from the DofH audit in 2003 (Tables 6.1 and 6.2). There were several important observations that would create a growing climate of mistrust in medical research, culminating in HTA2004. The first was that pathologists did not maintain proper post-mortem records. The DofH had a great deal of difficulty locating the incomplete paperwork trail. This meant that the figures they were able to ascertain were probably very conservative about the extent of unauthorised retentions. Anatomists, as we saw in Chapter 5, faced the same audit trail problem. They had been understaffed, had not done their paperwork efficiently in the 1980s and 1990s and thus had failed to get all their cremation work signed off officially by the DHSS once they had completed their teaching and research work on the dead. They looked guilty of holding on to human material for much longer than they actually did. In the case of pathologists, there was so little paperwork that it was difficult to assess for audit purposes whether the system was at fault because of similar low staffing issues or whether everyone preferred to operate with a lack of efficiency and transparency. One outcome, though, was certain. The DofH report concluded that a significant amount of paperwork involving the Cambridge Brain Back was destroyed, misfiled or never created in the first place from the 1970s onwards.
| Category | Number of brains received | Earliest date | Most recent date |
|---|---|---|---|
| Prader-Willi syndrome (B) | 3 | 21.01.1997 | 24.02.2001 |
| Normal control (C) | 557 | 05.01.1980 | 08.10.2001 |
| Dementia: long PM delay (D) | 172 | 10.01.1980 | 02.03.1993 |
| Epilepsy (E) | 39 | 10.05.1983 | 28.12.1988 |
| Dementia: short PM delay (FD) | 272 | 21.11.1985 | 23.04.2001 |
| CC75C (L) | 206 | 22.06.1989 | 29.11.2001 |
| Huntington’s disease (H) | 707 | 17.02.1980 | 10.12.2001 |
| Fronto-temporal dementia (JH) | 102 | 20.01.1992 | 16.01.2002 |
| Down’s syndrome (M) | 16 | 04.03.1981 | 19.10.1998 |
| Multiple sclerosis (MS) | 2 | 12.03.1995 | 22.05.1997 |
| Parkinson’s disease (P) | 62 | 01.02.1980 | 02.09.1992 |
| CFAS (RH) | 86 | 14.05.1993 | 21.12.2001 |
| Schizophrenia (S) | 182 | 04.01.1980 | 22.09.1994 |
| Spinal cord (SC) | 2 | Unknown | Unknown |
| Progressive supranuclear palsy (SR) | 1 | 07.09.1979 | - |
| Depression (X) | 66 | 01.02.1983 | 23.12.1992 |
| Suicide (Y) | 43 | 18.02.1983 | 13.03.1989 |
| Tissue held for Oxford CFAS | 29 | In one batch, sometime mid 90s | |
| TOTALS | 2547 | ||
| I. | The Huntington’s disease study had the active support of relatives and of COMBAT (the voluntary organization formed to support families of those with Huntington’s disease). Consent was obtained for brain removal in these cases. |
| II. | Further programmes developed and in 1985 the MRC received a proposal to support the brain bank as a service facility to support research teams undertaking neurochemical and other investigations that required brain tissue. |
| III. | ‘Control’ brains from ‘normal’ subjects were collected. Consent from the relatives was not sought or obtained. |
| IV. | The Department of Pathology of the University provided diseased brains and ‘control’ brains. |
| V. | No distinction was made between hospital and Coroners’ cases when brains were obtained. |
| VI. | There is no record that the collection of ‘control’ brains was ever considered by an Ethical Committee before 1985. |
| VII. | The 1985 application to the MRC was ambiguous on the question of consent. One section, referring to collection of index cases, underlined the need for consent by the relatives. Elsewhere the requirement for ‘control’ brains is set out with no linkage to consent of the relatives. |
| VIII. | During the 1980s the brain bank technician would review the list of post mortems scheduled each day and identify brains that would be of interest to the brain bank. |
| IX. | In 1987 the funding basis of the bank changed. From that date it was to focus on individual projects rather than provide a ‘banking’ facility. |
| X. | In 1988 the bank became involved in a multi-centre prospective epidemiological study of dementing diseases of the elderly (the CFAS programme). This study received Ethical Committee approval. |
| XI. | For the CFAS programme, full consent for brain retention had been routinely obtained from the relatives. |
| XII. | Collection of brains from Coroners’ cases as ‘controls’ and for the suicides study continued in parallel with the large prospective dementia study. |
| XIII. | The post mortem reports to the Coroners failed to record when brains were retained for use by the brain bank. |
| XIV. | In 1991 Mr Smith, the Coroner for Cambridge City, discovered that brains were being removed from Coroners’ cases. He ordered that no brains or other organs from Coroners’ cases were to be retained for research without the consent of the relatives. Organ retention was permitted only for diagnostic purposes. |
| XV. | The brain bank continues to collect brains, with consent, from hospital cases. |
| XVI. | As earlier chapters have indicated, the Cambridge brain bank was regarded as a model for other brain research routes to follow, and the methods of obtaining ‘controls’ from Coroners’ cases appear to have been copied. |
The auditors concluded that although they lacked accurate figures for the 1970s–1980s period, the surviving but scattered figures they had located for the 1990s probably reflected general working protocols. The DofH auditor thus explained that:
The post mortem reports sent to the Coroner listed any tissue samples or other investigations made by the pathologist that could have a bearing on the cause of death. The reports did not mention that brains had been retained for the brain bank. All the post mortem reports on the 43 suicide victims whose brains had been obtained for the bank were examined. The records of the brain bank confirm that these brains were retained but none of the post mortem reports mentions brain retention. These reports were made to the Coroners for Cambridge City, South Cambridgeshire and Huntingdon Districts. A number of post mortem reports on cases where the brain had been retained as a control were also cross checked against the brain bank records. Again, the post mortem reports were silent about brain retention for the bank. In this respect these post mortem reports were deficient as they did not alert the Coroners to what was going on.49
There was therefore a sustained culture of a lack of informed consent for families. In other words, although the figures available were incomplete, it was reasonable to conclude that there had been many different sorts of missed disputes generated inside the brain research community. Leading brain researchers did not necessarily know everything on the supply side about the activities of coroners and their pathologists or morticians. However, they also did not choose to look in any greater detail. As a result, it is only the recent oral histories (introduced above and elaborated below) which confirm that there was a lack of persistent questioning, notably from the pathologists on duty. The system was peopled by caring staff, but it was equally careless in its working practices, and this was the chief cause of different sorts of missed disputes by the late 1990s. It seemed thus that many people felt tarnished by a lack of others’ transparency. To better understand that wider context, we need now to turn our attention to the controversial Isaacs Report (2003), first introduced briefly in Chapter 2. It is a historical prism of what was happening on a regular basis inside hidden histories of the brain dead and outlines how paperwork was disguised, and crucial information withheld, to create missed disputes. Part II of this chapter is thus all about engaging with the human stories that people medical death and its neuroscience context.
Part II
The Isaacs Controversy
In April 2000, Mrs Elaine Isaacs discovered the retention of the brain of her deceased husband for post-mortem and further research purposes in Manchester.50 She was very upset by this because the revelation came 13 years into widowhood under traumatic circumstances. On 26 February 1987, Mr Cyril Isaacs committed suicide. Aged 54 years, he had been suffering from episodes of mental ill health and had tried to take his own life on several occasions. His detailed medical case notes explain that during 1986–1987: ‘In the five months before his untimely death, Mr Isaacs had experienced depressive mental illness and had been under the care of both private and NHS doctors.’ In this state of mind: ‘He had taken three overdoses, two of these in the same weekend within one month of his death.’ Subsequently, it also reported that: ‘Mr Isaacs had received in-patient psychiatric care as a voluntary patient. He had been prescribed medication at the time of his death and was due to see his general practitioner Dr Rosenburg’ on the day he took his own life. In the evening, Mrs Isaacs and a relative named Mr Clive Lingard discovered Mr Isaacs dead at home. They made an emergency call to the police on Thursday evening, 26 February 1987. Mr Isaacs had hanged himself from a hatch in the loft. A duty police surgeon attended the suicide scene and pronounced death at 7.50 p.m. As the circumstances surrounding the unnatural death were unclear, it was essential to involve the coroner. This was when Mrs Isaacs lost control of the material fate of her dead husband, as Chapter 2 introduced, and a missed body dispute occurred that will be elaborated in detail here.
The Isaacs family were devout Jews. Their traditional faith required them to bury Mr Isaacs’s body within twenty-four hours of death. It must be ‘whole’: according to religious rites, it must not be cut extensively, and the organs must not be removed. They argued that as the cause of death was obvious, there were witnesses to verify its sad circumstances, and medical notes would confirm a recent case-history of depression, no post-mortem should take place. The coroner had the option to do just an autopsy. In this way, the family could adhere to their deeply felt culture of laying out the body at home, saying prayers for the dead over it and burying it according to orthodox Jewish rites. It was therefore very distressing for Mrs Isaacs and her son to discover that Mr Isaacs’s body was taken from the family home in preparation for a full post-mortem scheduled for Monday, 2 March 1987. An undertaker transported the body by arrangement with the local police. They issued instructions to deliver it to the mortuary at Prestwich Hospital, where the local coroner according to standard practice commissioned a full pathology report. The dead body arrived at 20.45 p.m. on 26 February 1987, just 55 minutes after the police surgeon on duty pronounced death. In material terms, it was a very fresh cadaver. The body, refrigerated overnight, would be in a good condition for pathology. It was also potentially ready for further medical research.
There were, according to the official records, two people present at the subsequent post-mortem – Dr R J Farrand (pathologist) and Mr Dennis Walkden (mortician) – both were acting for the coroner. They did bring forward the date of the post-mortem in recognition of the Jewish family’s burial rites. A written record confirms the removal of Mr Isaacs’s brain at 11.15 a.m. on Friday, 27 February 1987 by the conclusion of the post-mortem. In accordance with standard practice, those on duty telephoned the coroner, confirming that the cause of death was suicide. There was no evidence of foul play. The North Manchester’s Coronial Office released the body for burial to the family’s Jewish undertakers. Nobody informed them of the brain retention. Nor did it form part of the evidence presented at a reconvened Inquest conducted by Mr Bryan North, coroner for the area in which Mr Isaacs had died. As the verdict of suicide was unopposed, the coroner had the official capacity to declare it a ‘paper inquest’ (like the ‘non-jury’ cases of the past). This meant that various written documents (police report, GP statement, post-mortem evidence and so on) were enough to pass a verdict and establish there were no suspicious circumstances. Crime scene photographs were taken, but it was never officially explained why they did not form part of the Inquest evidence reviewed by the coroner (forensic teams in the event of an unexplained suicide take digital images as a matter of course). Mrs Isaacs did have an opportunity to attend the Inquest. She was supported by a solicitor and barrister arranged by the elders in the Jewish community. What upset the family the most was the final verdict of ‘Suicide … Hanging … Cyril Mark Isaacs died of the aforesaid at his home. He was found hanging from the loft by an electric flex’ [sic].51 In the Jewish community, the taking of life is taboo and there had been no official reference to Mr Isaacs’s accumulated history of mental ill health at the Inquest. The family felt that as it stood, the verdict could bring them cultural shame in their community since the exonerating circumstances did not form part of the official reporting.
Mrs Isaacs remained very troubled about her husband’s death and the removal of his body from their home for a post-mortem without her consent. She wrote many letters to the coroner, Mr Brian North, between 1987 and 1991 to query the verdict because it seemed to her to reflect a lack of cultural and human understanding. Each time, the coroner informed her that it was his duty to base his verdict on the written evidence presented by the police, witnesses and pathologist assigned to the case; their medico-legal verdict was prescribed in regulations and could not be adjusted retrospectively. Eventually, Mrs Isaacs managed to get official access to Mr Isaacs’s medical records still held by his general practitioner in April 2000. She was anxious to read these to see if they would exonerate in any way the stark verdict of suicide. What she found amongst her dead husband’s medical papers was surprising and upsetting. A letter to Mr Isaacs’s general practitioner, Dr Rosenburg, explained that the Department of Psychiatry at Manchester University ‘had collected samples from Mr Isaacs’ brain’ and the research team were anxious to frame their research study by reference to his history of mental ill-health and medication for depression administered prior to death. The coroner permitted this hidden history to be used for research purposes, but he did not reconsider the humanity of the suicide verdict. A dead husband’s brain was fresh, a research opportunity, and thus formed part of a large mental ill-health project. At the time of death, Mrs Isaacs had explained her religious convictions to the police, a coroner and her husband’s general practitioner. It was self-evident she had been ignored. There was a clear breach of medical ethics, resulting in a missed body parts dispute. Mrs Isaacs’s son thus wrote to the Secretary for Health, Hon. Alan Milburn MP, demanding a full investigation into the original circumstances surrounding the death, post-mortem, retention and disposal of Mr Cyril Isaacs’s brain. Events revealed a pathology and medical research cover-up.
On 29 July 2001, Her Majesties Inspector of Anatomy, Mr Jeremy Metters, conducted a formal investigation on behalf of the government into the controversial Isaacs Case. Over the next two years, his enquiries were extensive and exhaustive. He found that there was a ‘joint research team’ involved in brain study comprising members of the physiology and psychiatry departments at Manchester University. Their main research focus was neuropathology and in particular mental ill-health conditions (broadly defined). North Manchester Coronial service from 1985 to 1997 had routinely permitted the retention of brains for further research purposes at Manchester University without the knowledge of the families involved: a common practice amongst many pathologists employed by coroners across the country. In addition, GMP were criticised for their officious conduct in relation to Mrs Elaine Isaacs (a theme we will be returning to later in this chapter since such criticisms have re-emerged with renewed force recently, as we saw in our opening story of the Culshaws in this chapter). Essentially, the Isaacs Report (2003) highlighted:
7. The report shows, among other things, that relatives were not aware that:
➢ Organs would be removed as part of a coroner’s post mortem examination;
➢ Organs removed might not be returned to the body after the post mortem examination;
➢ Organs could be retained legally by the coroner without their permission in connection with establishing the cause of death; and
➢ Organs might be retained for other purposes, such as research, without their consent and thus without legal authority.
8. Relatives were not given:
➢ Information about the coroners’ post mortem process;
➢ Information about the options for the ultimate disposal of any organs removed;
➢ Support, advice or counselling; or
➢ Suitable consideration of religious or cultural beliefs.52
Jeremy Metters provided a national census of all brain material held in research repositories across England and Wales (see Table 6.3). Mr Cyril Isaacs’s brain was one of 23,900 deposits that had been stored since the 1970s for further research purposes. Pathologists generated these on behalf of coroners across the UK. In Manchester, several morticians co-operated at Prestwich Hospital with this ‘supply mechanism of donation’ for a reported fee of ‘£10 per brain’. Although one particular coroner denied he knew the specifics of what was taking place, Metters concluded that this was ‘hardly credible’ under the circumstances. It appeared that ‘brain collections’ rather than ‘brain banking’ had constituted the majority of ‘retentions-without-consent’; it was difficult to retrace the individual research thresholds inside the supply system because the paperwork trail was either never created in the first place, had been destroyed subsequently or was ambiguous at best. The media and patients’ groups who took this as confirmation of a culture of duplicity queried the extent to which the official figures were a true picture of pathologists’ covert working practices and their corporate culture of denial.
Table 6.3 Nature of retentions in pathology stores, which had been accumulated since 1970, and were present at the National Census Point, c. 2001–2003
| Organ | Number of organs | Percentage of total retentions |
|---|---|---|
| Brains | 23 900 | 44% |
| Hearts | 9 400 | 17% |
| Lungs | 6 900 | 13% |
| Other Organs | 6 100 | 11% |
| Body Parts | 3 700 | 7% |
| Stillbirths/Fetuses | 2 900 | 5% |
| Not Specified | 1 400 | 3% |
| Total(s) | 54 300 | 100% |
Metters concluded that his figures were the best indication of the scale of brain retentions, and he distributed them into three research categories: Brain Accumulation (generally created by coroners’ cases via hospital mortuaries and commissioning pathology reports for post-mortem purposes); Brain Collection (held by pathology departments initially for diagnosis, but also for further teaching and research use); and Brain Banking (linked to pathology departments and university research centres), often working with relatives who have given consent to further specialised research into specific conditions like Creutzfeldt–Jakob Disease (hereafter CJD), Huntington’s or Alzheimer’s neuro-degenerative diseases. Metter decided that it was Brain Accumulations and Brain Collections that were ethically questionable. Pathologists had been working their way around the law to facilitate brain research.53 Effectively, they colluded in a system of supply that ignored codes of practice on informed consent. In turn, these should have been defined properly under HTA1961 and Coroners Rules (see Chapters 2 and 5), but were not. The paternalism of the past had been exposed to public scrutiny and found wanting in a biomedical era. It was this culture of concealment which would result in HTA2004. Yet, like all new legislation, it would take time for ingrained attitudes to change. In other words, the medical research community that had relied on hidden histories of the dead for so long neglected to appreciate the range of disputes they had generated for the future. They did operate within the legal requirements of their time, but this also meant that medical ethics remain fixed in an era when biotechnology was fast changing. As a result, only by blending the numerous historical and hidden ethical issues created can we begin to appreciate their cultural ramifications, including, importantly, notions of trust and expertise, the problem of piecemeal legislation and the ambiguities of consent, which went undetected from the 1960s to 2000. This proved to be a public relations mistake, exposing differential power relations in an era of full democratic representation when everyone had a taxpayer stake in the NHS. There were many gains from the new era of medical research for the general public in this historical process, but equally the bereaved expressed how excluded they felt in terms of the role of memory, the changing boundaries of life and death and the scale of the Information State’s lack of accountability in their medical lives. To better appreciate how pathologists defended their position in response, we need to trace a representative sample of oral histories that document typical reactions to the public outcry for HTA2004 because of the scale of the missed disputes being rediscovered.
Once HTA2004 became law, many pathologists in the UK resented the position they were placed in. Most felt hounded by the media, made a scapegoat for the degree to which the Coronial service relied on their expertise. The Pathological Society of Great Britain and Ireland hence took the decision in 2008 to commission a new book by Sue Armstrong called A Matter of Life and Death: Conversations with Pathologists,54 based on extensive interviews with practicing pathologists. An important theme of the oral histories assembled was the Alder Hey scandal in the NHS and its aftermath. There was uniform agreement amongst participants that it was ‘a dark hour for pathology’ across the British Isles and Ireland. As Professor James Ironside – an expert on the neuropathology of CJD and member of the new Human Tissue Authority set up in 2005 – explained:
What happened in Alder Hey was terrible. It opened up the whole question of autopsies – retention of tissues and organs, how much relatives knew, how much relatives had been consulted – and had some terrible messages for all concerned. It was a dark hour for pathology, no doubt about it. Not helped, I must say, by the media. You were made to feel that not only had you examined a baby that had died from cot death or something, you’d actually gone out and killed it beforehand. Just terrible! And also I think that we were not best supported by the Minister of Health at the time, Alan Milburn. He just opted to go ‘belly up’ and do anything to satisfy the various pressure groups that had emerged from the media, and I think a more measured response would have been better. Some of the first attempts at the legislation were just completely unworkable. And through pressure from a whole range of groups, the legislation was changed in the UK. It’s still not perfect, but it’s better than it was.55
Professor David Levison (now retired), former Chair in Pathology at Dundee University, reflected with a slightly different emphasis:
I don’t think that Alder Hey and Bristol were scandals. They’re only scandals because the media say they were scandals. … I know of quite a few people who have given up being paediatric pathologists because of this – because they couldn’t stand the kind of pressures they were being put under, the phone calls, and the abuse they were getting as they walked home, and this sort of thing. It has done a lot of harm to some people, and I mean it has really kicked paediatric pathology in the teeth. … I know of studies that have not been done because it’s just not worth the effort of going through the ethical hoops. … It really does slow things up.56
Others such as Professor Sebastian Lucas, Chair in Clinical Histopathology at Guy’s, King’s and St Thomas’ hospitals, pointed out that from a pathology point of view by 2008:
In a way things haven’t got all that much better [since Alder Hey]. They’ve got more bureaucratic, but there’s still a huge grey area in tissue retention across the consented to coronial autopsy spectrum, and it’s not very clear. Or it’s very clear what to do if you want to stay absolutely within the letter of the law, be squeaky clean. You do nothing! But the point is, to be good and to be useful for public health you need to do a bit more than that, and that’s where the grey areas come in.57
Most argued that it was poor communication that was at the heart of recent biomedical debates and the public exposure of pathology’s inner working practices. Irene Scheimberg, Consultant Paediatric and Perinatal Pathologist at the London Hospital, thus took the view that:
At one point during the Alder Hey crisis I said, ‘I am going to go and talk to the Liverpool parents so that they realise that not all pathologists have horns and are horrible’. At the beginning they were all very confrontational – there were lots of them – and I said, ‘I do understand what it is to lose people, to experience the untimely death of people’ [as someone from the Jewish community who needed political asylum, she lost many friends and family to war and conflict]. And I told them my story – because they were so immersed in their grief that they didn’t realise other people might have had a traumatic history as well. They were surprised because I was crying. One of them came up and hugged me afterwards, and said: ‘I never thought I’d ever hug a pathologist.’58
Scheimberg suggested that it was better for people when grieving to keep looking forward, an attitude of mind she had learned from the long history of being political refugees in her Jewish family of Russian extraction. Her personal motto was: ‘Memory is very wise – you don’t remember what you cannot live with.’ She did respect the fact that learning later that information had been withheld about human harvesting could be shocking for families. Consequently she explained how:
In coroners’ cases I write a personal letter to the families. I use the name of the child, and I explain to families why I’m asking them if we can keep blocks and slides. In the first place because it’s important for their sakes in case there is a problem or something later. Then, so that we can use them for teaching and training. Because someone has to carry on with the work when I’m no longer here; the knowledge has to be passed on. And then I explain why we need them for research, and what type of research we’re talking about – because it’s important for them to know that it’s research that will benefit them personally, but we can’t do it unless we have specific consent.59
In this selection of oral history material we have therefore an important opportunity to elaborate on the conceptual approach of Alessandro Portelli, who reminded us at the start of this chapter about the importance of ‘the peculiarities of oral history’ and their subjectivity precisely because they are ‘not just about what people did, but [what] they wanted to do, what they believed they were doing, and what they now think they did’.60 Thus, it is apparent that some pathologists operated on a need-to-know basis because they felt it was better to keep pressing ahead with their research agendas, and unkind to tell the general public everything about brain research when they were grieving. Others did not accept that the organ donation and pathology retentions in the NHS around 2000 were a scandal but a media-generated medical outrage designed to sell newspapers. Most had been as open and engaging in their working-lives as they could be under difficult circumstances, committed to communicating the importance of their work and legacy of human material retentions. Pathologists were thus complex actors, shaped by social, cultural, political, economic and administrative circumstances. Like all human beings, they could fail, and some did so in terms of public relations; for there was a general recognition by HTA2004 that pathology’s paternalism and patriarchy were past their clinical sell-by-date. Its actor network had to leave behind the ethics of conviction of the past and embrace the ethics of responsibility for tomorrow. Against this backdrop, the Royal College of Pathologists (hereafter RCP) have been working extensively to try to resolve these experiential issues, and they recognise the need for consensual medical ethics: a trend that has increased in the past ten years or so. There has been an official recognition that pathologists had taken a ‘proprietorial’ view of the body rather than a ‘custodial’ one: a theme that has run throughout all the chapters of this book.61 At the same time, in the intervening years since HTA2004, common themes have emerged in conversations with pathologists: as we saw above and touch on below, too.62 Ingrained attitudes have been of long duration, and some pathologists have refused to make the clinical adjustments, retiring early. There has continued to be ambivalence felt by many RCP members about the extent of public accountability required by new statutes, mushrooming bureaucracy and the media.
Today the RCP publishes widely its latest research and innovations, engaging the public with stories of how pathology into common cancers, for instance, saves lives every day in the NHS. It has also been keen to promote new solutions for old pathology problems. One innovation it has been eager to publicise is digital autopsies in cases where the probable causes of death are known in Coronial cases in England and Wales. RCP now recognises that CT scanning techniques could provide a cultural and practical solution for families like the Isaacs who would not consent to the cutting of the body and the removal of human material on religious grounds but would be amenable to a CT scan instead because it is non-invasive, replacing a post-mortem. The way it works is that the deceased can undergo a CT scan to confirm ‘unnatural death’ with a minimal amount of interference with the dead body. A new study published in the Lancet, co-ordinated by Professors Guy Rutty and Bruno Morgan at the University of Leicester, thus showed recently that in a sample size of 241 cases in which an adult had died of unexpected outcomes that were not necessarily suspicious, some 92 per cent of these coroners’ cases (where n=222) could be established from digital CT solutions.63 Currently, the cost is £500 per case, paid for by the family in question, raising ethical issues about fair access to the technology for everyone, especially in communities of high-density ethnicity and poverty patterns. Nevertheless, as the RCP press office told the Guardian newspaper in May 2017: ‘The College fully supports further research in this area while reinforcing the need for thorough and robust governance in this emerging field.’64 Evidently, the Isaacs Report was an important catalyst for cultural change in medical research around the Millennium in Britain. It has resulted in an emphasis on informed consent in brain research and finding new solutions to complex human dilemmas over the ownership and use of bodies and body parts. Even so, in interviews given off the record for this book, many pathologists have made it clear why they left the profession in the past five years or so. Most felt their job description ‘was now too restrictive’, ‘there’s just too much bureaucracy’ and ‘it’s taken away my sense of professional standing … I mean who wants to deal with all the hassle’.65 So rather than reform from within, what has tended to happen since HTA2004 is that the numbers of qualified RCP members have thinned out. There is unquestionably a lot less hands-on experience than there once was inside the Coronial system. To balance this sense of a loss of professional expertise, the final section of this chapter thus returns to the human impact of pathologists’ workload, particularly involving those who have just retired or resigned from office. In this way, we can engage with a wider cross section of lived experiences of missed disputes, similar to the storyline of the Culshaw family which opened this chapter. For the events described test public trust in pathology work since HTA2004, which was supposed to have been changed fundamentally the national conversation about harvesting brains and human tissue retentions.
‘Hospital Stored Dead Children’s Brains in Jars’: Southampton Hospital under Public Scrutiny66
In 2012, the Association of Chief Police Officers (hereafter ACPO) faced an ethical dilemma. They had to inform the Human Tissue Authority that a large number of organ and tissue retentions had gone unnoticed at the time of HTA2004. This was because the police had special powers concerning human material retention up until 2006. They were exempt under Section 39 of the HTA2004, as follows:
Section 39 of Human Tissue Act
(1) Subject to subsection (2), nothing in section 14(1) or 16(2) applies to anything done for purposes related to—
(a) the prevention or detection of crime, or
(b) the conduct of a prosecution.
(2) Subsection (1) does not except from section 14(1) or 16(2) the carrying-out of a post-mortem examination for purposes of functions of a coroner.
Forensic PM examinations
If a person dies in circumstances considered to be ‘suspicious’ or where homicide is suspected, HM Coroner after consultation with the police can authorise a Home Office Registered Forensic Pathologist to perform a forensic PM examination to—
• Ascertain the identity of the deceased
• The cause/surrounding circumstances of death
• To allow collection of evidence from the body67
The Human Tissue Authority also issued a public statement clarifying that there were three statutes that authorised the police to hold human material. These were: the Coroners and Criminal Justice Act (Eliz. 2 c. 25: 2009), the Police and Criminal Evidence Act (Eliz. 2 c. 60: 1984, especially sections 19 & 22) and the Criminal Procedure and Investigation Act (Eliz. 2 c. 25: 1996). Together they permitted an investigating officer to be present at a post-mortem, which they had authorised by virtue of asking forensic scientists and Home Office pathologists to lawfully enter premises and seize whatever material evidence was necessary to bring a criminal act to justice. They also had extra powers under English Common Law of seizure for physical items or human material found elsewhere that were not on the premises of a specific crime in the locality where it was committed. Since these procedures had overlapping regulations, there was not a coherent national policy in the police force of how to seize, record, evaluate evidence, present in court and return human material after a conviction or court hearing. The Murder Manual (2006, especially Section 11) did try to give clear pathology guidelines, but this too resulted in disparity amongst actual police forces in England and Wales, with individual senior officers taking a pragmatic view of their particular medico-legal position. The ACPO thus conceded in 2012 that many police forces did not actually know what their responsibilities were in respect of human material retentions. Most thought this problem of a lack of uniformity was delegated to coroners and their pathologists to monitor and resolve, given the former’s historic powers of discretionary justice (a theme we encountered in Chapter 5).
In 2012 a central government commissioned ACPO audit grew out of the National Gold Group established alongside the National Police Improvement Agency (later to be renamed the Home Office Pathology Unit). These policing bodies were granted permission to take proper legal advice from suitably qualified barristers during the national audit process, which was concerned with three categories of material infringement:
Category 1 – Material taken at PM examination which would not generally be considered part of the body e.g. scrapings, fingernails, hair, stomach contents
Category 2 – Samples of human tissue which are not a significant part of the body e.g. small tissue samples, blocks, slides & so on
Category 3 – Samples of human tissue that incorporate a significant part of the body e.g. organs, limbs & so on68
Category 3 formed the central focus of the ACPO audit, in liaison with the Human Tissue Authority. Together they found that ‘492 organs’ or what was described as ‘significant [sic] body parts [brains] were held on police premises or other establishments. These related to historical cases going back to the 1960s.’ To try to reassure the public that this did not repeat Alder Hey, the Human Tissue Authority issued a press release confirming that ‘between 1960 and 2010 there had been 6.2 million PM [post-mortem] examinations’ conducted in England and Wales. Of these 6.2 million, just 2.45 per cent, or 151,900, resulted in the need for a forensic examination in which the police became involved. Of the 151,900 cases, only 0.33 per cent, or 50,633, related to potential organ retentions or significant body parts kept by the police and their Home Office pathologists.69 Yet, this statistical statement still did not provide enough reassurance to the families involved, because even a basic calculation underscored that in a 50-year period, on average there were not less than 1,000 cases a year that could potentially have resulted in missed body disputes. It was (again) media testimony of those who were misled that would prove to be a powerful reminder of the need to remain vigilant in a biomedical era.
At first, ACPO tried to counter any negative publicity by stressing the expertise of those that retained the human material and the important legal reasons for doing so. Thus, it was explained that under police powers, a selection of NHS hospital premises were designated as regional autopsy units. Here coroners and their pathologists on behalf of the Home Office had stored human material pending a court case. The Home Office expressed regret that human material had been kept without informing families, but the police tried to reassure the media that it was done in the best interests of criminal justice. One such location was Southampton Hospital in Dorset, a regional autopsy unit for the West Country. The families involved were told on a case-by-case basis that their loved one’s remains were still in cold storage. It did not help that as this slow process was just getting under way, a civil servant at the Home Office was despatched to tell the press that: ‘It is down to individual forces to decide … whether the material is needed or not. In some cases the retention period may have been longer than necessary.’ This was a classic case of official understatement, as events subsequently proved in the press.
On 14 August 2012, the Sun newspaper led with a headline – ‘They took brains from our boys too … WHY?’ Their investigative journalist, John Coles, spoke to Hannah Cheevers, whose baby son had died of a heart defect aged 2 days old in 1998, and Melanie Galton, whose infant son died aged 1 of sudden infant death syndrome in 1997. Each was told that there would be a post-mortem, but neither was informed that their offspring’s brain had been retained and kept for 15 years by pathologists on behalf of the police. Melanie explained:
They turned up just before Christmas and told me, ‘We’ve found Ricky’s brain at the hospital’. I was stunned, I couldn’t believe what I was hearing. … I asked them ‘Why have you kept it so long?’ and all they could say was something like it had ‘got lost in the system’ and they were now chasing everything up. … They gave me a letter and leaflet explaining the situation – but instead of ‘son’ the letter refers to him in one place as ‘mother’ and ‘father’ in another. … I’m disgusted and angry as well as upset. I’m not going to let this drop. … They had a post mortem which found the cause of death as sudden infant death syndrome, so why did they need to keep his brain? I imagine it’s been forgotten about on the back of a shelf somewhere. I want to have another funeral – it will probably be just me by his grave – because I want it returned to his body where it should be. I don’t want it to go missing [author’s emphasis] for another 15 years.70
In a similar refrain, Hannah Cheevers and her partner, Martin Lovell, from Wimborne Dorset were shocked to be in an equivalent missed body part dispute. Hannah recounted:
They told us tissues from Rhys had been retained – I thought they meant a sliver of tissue on a slide. Then they said it was his whole brain. I was shocked. I was never told about this and if they’d asked my permission I would have said ‘no’. They wouldn’t tell me why it had been kept and they said that nothing had been done to it. It was dreadful – I had a new baby in my arms and it brought it all back. … If they’d kept Rhys’s heart I might have understood, but there was no reason to keep his brain. When he died they offered us a post mortem to find out what had happened and we agreed because we wanted to know. So he was taken from Poole Hospital to Southampton Hospital, but we had no idea they would keep his brain. It’s absolutely disgusting what has happened. I remember the Alder Hey scandal, and I said to my mum at the time that I was glad it wasn’t Southampton. There really needs to be an inquiry into this.71
Each mother recalled having to go through a harrowing series of police enquiries at the time of their child’s death to make sure that it was not suspicious – it felt as though old and very painful memories were being re-opened again. Indeed, one of the most poignant press stories to appear was that of Ryan Franklin who ‘was killed by his dad, aged two in 2002’. A case of manslaughter was secured in court based on medical evidence that the child had been battered to death. His mother then explained what happened a decade later. She was told by Southampton Hospital that her dead baby’s brain, eyes and spinal cord had been retained. Like the other mothers affected, she had known it was necessary to have a post-mortem but she claimed that she had said ‘no to donating his organs’, telling doctors in 2002: ‘He came into this world full and I want him to go out full – don’t touch him.’72 Around the time of the Alder Hey scandal, she began to suspect that she may have been misinformed. This uneasy sense of a missed dispute re-emerged in 2012: ‘When I heard about this review police are carrying out I hoped they would have got in touch with me. I would like someone to come forward and tell me what’s happened to his organs so I can have closure.’ Catherine Franklin ‘discovered that some of Ryan’s organs had been taken. His eyes went to a hospital in Sheffield for research – but no one knew what happened to the rest.’ The newspaper reporter explained how she had gone on to have ‘another son, Benjamin, eight’. Nonetheless Catherine stressed: ‘Every time I try to find out what happened I hit a brick wall. I hope now police are doing their audit I’ll finally get the truth’ about what really happened. In fact, it soon emerged that there were forty cases in Southampton all relating to young dead children whose brains had been removed and stored.73 In the majority of cases, it appeared that any fears of suspicious deaths were cleared up quickly and no physical evidence for the criminal court was necessary to secure a conviction. Each was a tragic tale of child bereavement. The mothers, according to their own testimony, all found the pain of loss almost unbearable to experience again after ten years had elapsed.
Personal spoken and reported histories like these representative cases provide thought-provoking testimony concerning the conduct of the medical research community in a biomedical era. Their discourse reiterates Alessandro Portelli’s inciteful comments (encountered earlier in this chapter’s introduction) about the value of the ‘the peculiarities of oral history’ in the medical humanities. Their subjectivity again reveals ‘not just about what people did, but [what] they wanted to do, what they believed they were doing, and what they now think they did’.74 To many pathologists, it had seemed that the press has been responsible for stirring up emotive stories and putting the spin of scandal on the editorial byline to sell more newspapers about the recent ACPO audit findings. Yet, it is undeniable that the same sorts of experiential histories were often repeated, and verbatim by those families involved. Indeed, as Philip Cheung has recently pointed out, it is impossible to deny how much the twice-bereaved have needed each other for support when missed body parts disputes recur, exemplified by the number of support groups that have been set up and continue to flourish today. There is:
NACOR (The National Committee Relating to Organ Donation), and PITY II (Parents who have Interred their Young Twice) … Respect for Leicester, Stolen Hearts in Birmingham, Bristol Heart Children’s Action Group, Cambridge Area Support Network, Derbyshire Organ Retention Support Group, South Yorkshire/North Derbyshire Support Group for Post-Mortems Retention Parents and Relatives, NERO North East Organ Retentions Group), Storm in Manchester, Our Children, REGAIN groups in Nottingham, Legacy Faborio, PORSH in Plymouth, and so on.75
Cheung points out that there is ‘a danger that’ such support groups will ‘be seen by scientists and medical researchers as anti-science and anti-research’.76 Many scientists do not believe in an afterlife or appreciate that the physical remains can have a powerful meaning in the grieving process of the bereaved, even though there is ample evidence that the GMP failed not only the Isaacs family in 2002, but the Culshaws and others more recently. Too often, points out Cheung, such families who express strong natural emotions are ‘perceived in the same light as animal research campaigners’. He thus argues that the medical research community need to accept ‘the challenge of shaping ideas and attitudes’ to their work and its importance by meeting those bereaved with genuine humanity to bridge the recent past to a better biomedical future for everybody. It is therefore informative and important how the journal Science reported on 7 April 2017 that: ‘the Rules of Memory are being beautifully rewritten’.77 Because such perspectives have the potential to reshape how historians evaluate oral histories on the sensitive topic of missed disputes too.
It is often said in the global media that the British have a character trait that is admired around the world. They are renowned for being stoic, exemplifying the stiff upper lip in times of adversity. It was a national trait that was said to have brought the country through two world wars, associated food rationing and many millions of deaths. As, however, public tastes changed during the 1960s with the liberalisation of British society, the old values of a wartime generation were refashioned. It became culturally less acceptable to button-up emotions, and instead many more people began to speak about issues of mental health and well-being. Today, it is a popular topic of national conversation in Britain. At the same time as this process of promoting more compassion and understanding of mental and physical well-being was happening, neuroscience was also contributing to debates about the relationship between the brain and emotions. Recently, evidence has come to light that the way we thought the brain absorbed and accommodated trauma has been misleading. In the past, a medical assumption was made that the best way to help people to get over a very traumatic episode in their life was never to talk about it again – the stoic approach. Then this changed from the 1960s with qualified therapists encouraging those suffering from mental ill-health to come to terms with a dramatic experience by talking it through – the compartmentalising approach. Each medical intervention was about reviewing negative experiences and helping the patient to move on in a more positive direction. However, new scientific studies in Japan and the USA have challenged the neuroscience of this type of trauma management, and the results of these recent scientific findings are very important for assessing the emotional reactions of families to the missed disputes of the ACPO audit in 2017. The key to understanding what the bereaved were going through has been to better appreciate that the way we thought we handled and remembered trauma has been scientifically incorrect.
The brain is clever. It seeks to protect us in trauma. To do this, it does not ask us to be exclusively stoic or to compartmentalise what is happening when confronted by extreme stress. Instead, new scientific studies in Japan and the USA have found ground-breaking evidence that all painful memories are absorbed in two ways. First, the brain will store short-term recollections when we are in shock. Then, at the same time, it begins a neurological process of transferring the memories of that initial trauma from the hippocampus of the brain. Slowly, the brain has a neurological mechanism that converts short-term experiences into long-term memories in the cerebral cortex where they are ‘banked’ for life. In this way, the brain ‘doubles up’ its memory system. It creates two simultaneous memories that mirror each other every time we experience something out of the ordinary as human beings.78 This neurological balancing act is unconscious in the mind. The function of this doubling up is to help us as human beings to live with what has happened. We cope by assimilating together physical reactions (short-term shock, hippocampus) and their emotional impact (long-term feelings, cerebral cortex) of trauma. This works well neurologically, provided that the balancing mechanism is not disturbed. If, many years after a shocking event, it revived in an unexpected manner, then that would have the effect of unbalancing the brain’s trauma survival mechanism. So, we can be stoic and we can compartmentalise, precisely because of the amazing balancing mechanism in our brains, and this is what scientists mean when they say that ‘the Rules of Memory are being beautifully rewritten’.79 In 2017, the families involved in the findings of the ACPO audit experienced what happens when this newly discovered neurological balancing system was disturbed by reviving painful memories.
When we encounter oral histories and the navigation of their feelings in a history of emotions, it is important in the medical humanities not simply to dismiss their testimony of trauma as too subjective. In fact, what people recount is telling us that we need to fully consider the latest neurological perspectives of what is happening in the brains of the bereaved. The ACPO families experienced what it was like to go through a missed dispute about withheld information. This destabilised the short-term and long-term neurological centres of memory formation and unbalanced the maintenance of their well-being. Those involved thus found it mentally very hard to cope, and this is verifiable by the neuroscience of memory formation and maintenance. Effectively, some experienced a neurological U-turn that triggered a very stressful episode in the mind’s emotional centres. Importantly, the implications for this book’s study into missed disputes and how people emotionally react (hippocampus, short-term shock) and learn to live with the unpalatable facts (cortex assimilation, very painful emotions) are profound. If medically correct, Mrs Jean Culshaw and others like her were not being duplicitous or exaggerating when they said they were ‘suffering’ mental upheaval in March 2017. In neurological terms, their minds were, literally, disturbed, as they had to again go through very painful memories from 1993. Thus, in a history of emotions, scholars, such as William Reddy, are correct to emphasise how talking about feelings is essentially the only way that a person can then rebalance if forced to revisit something so painful.80 Ironically, science, which has long stressed its dispassionate and secular purpose (laudable aims), has itself discovered that the brain has a ‘beautiful’ medical function that is all about re-balancing the rational and the instinctive when missed disputes occur. It works with human nature holistically, and this is a significant finding for the medical humanities, echoing what George Steiner the moral philosopher suggested in this book’s Part I. The brain does not discard ‘old’ information for ‘new’ memories – instead, it runs these lived experiences ‘in parallel’ because life is like that, and this is what keeps us creative as human beings. In other words, those involved in missed disputes could cope well, provided communication was very good and trust existed between all those involved in the network of actors when a crisis point involving the death of a loved one had to be revisited. To illustrate that there could be more positive outcomes in this more transparent process for pathologists too, we end with the sort of brain story that seldom features in oral histories or the press on this sensitive topic.
In 2000, Sean and Sarah Luff became new parents. Tragically, soon after birth, their 3-day-old baby died because of medical negligence in Southampton Hospital. Mistakenly, staff on duty gave him a morphine overdose – ‘100 times the proper dose of painkillers’ – in an attempt to save his young life.81 At a subsequent Inquest, the medical evidence established that their son would have died in any case, such were the fatal complications in this sad case. This did not excuse the medical errors, but the hope was that the forensic findings would alleviate the Luffs’ concerns that their baby was not in pain when he died. However, the family was shocked when Dorset police informed them in 2012 that Southampton Hospital had retained their baby son’s brain in a jar without their consent in 2000. Sean Luff asked: ‘How many times can one family, and one little baby, be betrayed by the authorities?’ He questioned in the press: ‘How much more heartache can they inflict on us?’ There was, even so, to be a twist to this news story, and one that exemplifies the Janus-like nature of pathology expertise today. In February 2012, Sean Luff received a diagnosis of myeloid leukaemia. This happened just several months after Dorset police informed him about his dead son’s brain retention. Sean became very ill and had to endure ‘three gruelling sessions of chemotherapy and a bone marrow transplant’.82 Unfortunately, this series of life-saving treatments compromised his immune system, and he caught pneumonia just before the Christmas holidays in 2013. Because Sean was unable to fight the serious infection in his lungs, doctors judged it best to place him in a medically induced coma. It would take eight months of intensive care before Sean was stabilised and able to go home. Yet, the medical team that had saved his life three times in those eight months was based at Southampton Hospital, where his baby son had died under exceptionally stressful and medically culpable circumstances, twelve years earlier. Even so, the Luff extended family were grateful for Sean’s recent medical interventions. They hence decided to raise money for more medical research at Southampton Hospital in August 2013. The Luffs were happy to publicise the good work of medical staff in the local press. There was self-evidently a pathology paradox in this case, and a poignant one. Sean Ruff was kept alive by the same expertise that had once retained his baby son’s brain without his consent. The latter’s successful outcome did not justify the lack of medical ethics in the former case-history. Yet, it did make for a thought-provoking parallel in what have too often been hidden histories of the brain. For it left open the unanswered question: How much more could have been achieved if brain research and retentions had been a more open and engaging research partnership with the bereaved across Britain after WWII?
Conclusion
In 2010, a consortium of scholars convened at the University of Manchester to explore ‘forensic cultures’ in contemporary society prompted by the fact that coroners, pathologists and DNA specialists ‘now have an unprecedented level of visibility’ across the UK, not least because of ‘true crime’ drama on television.83 The conference concluded that ‘forensics is best understood as a historically-shifting material and social entity but also as mediated through a cultural grid of forms, languages and resources, through which credibility is built up, negotiated and contested’. Simon Cole, one thoughtful contributor, ‘questioned the idealised image of a scientific culture as a unified entity governed by a clear and stable set of rules which produce and guarantee a single form of knowledge’. This was essentially the case in many types of missed disputes in brain research, too, of the modern era. Recently, Paul Roberts has hence helpfully pointed out that histories of forensic science and pathology cannot simply be pieced together to produce a harmonious picture that does not reflect local realities or public sensibilities. Indeed, he has been critical of a strong confirmation bias in histories of science covering laboratory studies that elevate the positive and ignore the negative aspects of secretive working cultures (themes the Introduction and Chapter 1 highlighted). Thus, the Manchester conference concluded that there is more
value of attending to the complex interrelationships, cultural specificities, and diverse and shifting identities of forensic practitioners, the institutions within which they work, the techniques they deploy to produce and display forensic truths, and how these truths are transformed in public as forensic cultures engage the worlds in and for which they act.84
One of the main difficulties with researching the nature of pathology and neuroscience in the modern era has been the culture of the closed door. Not only was recording of brain retentions insubstantial but those records that survive in archive collections are often sealed under the 100-year rule. General statistics are obtainable under special written request according to the provisions of the Freedom of Information Act (Eliz. 2 c. 26: 2000) in the UK. Even so, there are many legal barriers erected to complicate better open and transparent research in the medical humanities. In protecting the past, pathology has often looked guilty of maintaining a culture of denial and subterfuge, and this has unquestionably damaged its reputation. When, moreover, new evidence emerges of past failings, like the GMP revelations recently after the ACPO audit, those conducting the conversations with relatives came across as insincere. Occasionally, named pathologists were revealed, but most remained hidden behind an anonymous title or official jurisdiction disclosed in the most general terms to families left confused and upset – angry about the faceless mandarins of a Home Office firewall. The corporate-speak which was often repeated by the police force about holding ‘open and honest conversations’ with relatives informed of brain retentions, sounded more like a publicity campaign for the press than a genuine attempt to engage with how the twice-bereaved felt. Jenny Culshaw and others felt understandably that their emotional well-being was being devalued and undermined. Indeed, it is noteworthy just how many shocked parents in the same situation repeated their shared understandings, using the same phrases and words to describe common predicaments and feelings of distress. In tragic circumstances, they had to re-open painful memories to gain concrete information. That neuroscience itself has discovered the ‘Rules of Memory are being beautifully rewritten’ in order to explain the double memory and its careful balancing mechanism we all create in the brain to deal with traumatic events in our lives is informative.85 The Culshaw and Isaacs families were not, it turns out, being excessive, overdramatic or unreasonable in their reactions, but rather their neurological response was functioning in a normal manner. In a history of emotions, it has always been essential to talk about such feelings to rebalance traumatic experiences reopened by time delays, misinformation, and half-truths.86 As all good historians know, careful attention should, likewise, be paid to what is not said, just as much as to what is. For the history of these missed disputes is like a dry-stone wall – in its research gaps are the future human solutions to consensual medical ethics. First we have to locate them, and then we must look that past honestly in the face to ensure we provide better access for professional researchers to evaluate those gaps in a measured manner.
In an ageing population around the world, brain research has a powerful role to play wherever we live in our community settings. With approximately one in five people in Britain now suffering from neuro-degenerative disorders, healthcare practitioners need the co-operation and co-creation of the public to make new medical breakthroughs. This cannot, though, be achieved in cultural isolation – the consent of the silent majority being taken for granted is no longer the modus operandi of pathologists, post–Alder Hey. Most recognise this and are working together to promote the sort of expertise in histopathology that we all need. Others resent the levels of bureaucracy and have retired or resigned from the profession, bruised by the public criticisms, which they still believe is excessive. That this will be a lost research opportunity in some respect, curtailing individual career paths in the short term, is undeniable. Yet, it is equally irrefutable that such a status quo had been created by closing ranks and not engaging with the public enough in the recent past. The responsibility, therefore, first and foremost, for this cultural stand-off, rests with pathologists and not society as a whole. The history of missed body disputes and disputed body ethics brought together in this chapter shows clearly that some pathologists acted as though they owned the human body, its parts, organs and tissue. In the 1950s, those entering the medical profession spoke of a vocation, a calling, a sense of purpose that this was the job they were meant to do. Some were arrogant about their expertise; others genuinely thought that they were working hard for the greater good. Medical science too has become an endeavour concerned with career progression, enhancing one’s scientific reputation and making headlines promoting the latest drug therapy. Those with a vocation did and do still people the system, yet the consensual and custodial only very slowly – too slowly, in many cases of missed disputes – gained ascendancy over proprietorial approaches to bodies and body ethics. Thus, missed disputes in brain research are a function of, and embody, slow and partial processes of cultural change in the post-war era. Yet even as medicine and the medical sciences have learned to talk with, rather than at, their patients, the expanding frontiers of the possible in terms of the cure and the extension of life made possible through precision medicine introduce a new potential for body disputes and a much more complex landscape of body ethics. It is to this matter that we turn, finally, in Chapter 7, the conclusion to this book, when we reflect on the question of scientific eternities of material afterlives in a Genome era.