The majority of mental health problems first emerge during the adolescent years (Kessler et al., Reference Kessler, Berglund, Demler, Jin, Merikangas and Walters2005). Thus, adolescence is a critical developmental window for both mental health prevention and intervention. Despite improvements in our understanding and ability to detect and treat youth mental health problems, there remains a persistent need for mental health services among youth, with the majority of youth untreated (Cummings et al., Reference Cummings, Wen and Druss2013; Merikangas et al., Reference Merikangas, He and Burstein2011). Among youth who do get treatment, there is often a long gap between the onset of symptoms and when youth first receive treatment (de Girolamo et al., Reference de Girolamo, Dagani, Purcell, Cocchi and McGorry2012), as well as low treatment attendance and completion in this population. As rates of mental health problems such as depression and suicidality continue to rise during adolescence (Centers for Disease Control, 2018), the gap between those who need and receive mental health services will only continue to grow.
In this chapter, we review the potential for technology to advance our understanding and treatment of mental health problems among adolescents through digital mental health interventions (DMHIs). We first discuss existing barriers to mental health care among adolescents, followed by a discussion of how DMHIs can address these barriers to improve access to and quality of adolescent mental health services. We then review existing research on DMHIs and the digital frameworks that are used to collect and deliver psychoeducation, assessment, and interventions across different hardware (e.g., smartphones, computers) and modalities (e.g., online, text, apps). Finally, we conclude with a discussion of the current limitations of DMHIs and key directions for the field to improve adolescent mental health care using DMHIs.
Barriers to Existing Mental Health Services
Significant, and often systemic, barriers interfere with access and delivery of mental health services for adolescents, including barriers related to cost, geographic proximity, and time, among others. These barriers often result in long waitlists and travel times, as well as a shortage of professionals providing evidence-based care (Andrilla et al., Reference Andrilla, Patterson, Garberson, Coulthard and Larson2018), particularly those who are trained to work with youth (American Psychological Association, 2016). Access to treatment is especially challenging for youth in rural regions (Andrilla et al., Reference Andrilla, Patterson, Garberson, Coulthard and Larson2018) and for adolescents who are racial, ethnic, sexual, and/or gender minorities. These youth often face additional barriers to receive culturally sensitive care (Alegria et al., Reference Alegria, Vallas and Pumariega2010). Inadequate education about mental illness, distrust of medical providers, and stigma about help-seeking behaviors (i.e., internalizing stigma) and mental health care (i.e., treatment stigma) also prevent adolescents from seeking help (Clement et al., Reference Clement, Schauman and Graham2015; Gulliver et al., Reference Gulliver, Griffiths and Christensen2010). Teens also often lack awareness and understanding of their symptoms as clinically significant, are uneducated about their treatment options, or are hesitant to share their symptoms with parents or other adults (Gulliver et al., Reference Gulliver, Griffiths and Christensen2010). Even when youth do access mental health care, treatment completion and compliance are often low due to these persistent barriers (e.g., cost, time, transportation, stigma). Thus, there is a critical need for services that are scalable, accessible, and developmentally appropriate for the prevention and intervention of adolescent mental health problems.
Potential Benefits of Digital Mental Health Interventions for Adolescents
Advancing technologies offer novel opportunities to improve the detection, prevention, and treatment of mental health problems. DMHIs have the potential to revolutionize mental health care by providing effective, accessible, scalable, and low-cost interventions. While adolescents are at heightened risk for mental health problems, they also may be uniquely positioned to benefit from DMHIs and novel digital tools (Wong et al., Reference Wong, Madanay and Ozer2020).
DMHIs can overcome many of the aforementioned systemic and individual barriers for youth (e.g., availability, cost, transportation, stigma). There are several factors that suggest DMHIs may be promising for adolescent mental health care. First, certain technologies to deliver DMHIs are already widely in use. For example, smartphones have become nearly ubiquitous among youth, with over 95% of teens owning these regardless of gender, race/ethnicity, or sexual identity (Anderson & Jiang, Reference Anderson and Jiang2018). Second, adolescents are early adopters of many digital technologies. They report high levels of comfort with and preference for online communication, particularly when discussing mental health (Bradford & Rickwood, Reference Bradford and Rickwood2015). Thus, DMHIs also promote help-seeking behaviors and can serve as a “gateway” to initiating mental health care (Kauer et al., Reference Kauer, Mangan and Sanci2014). Third, adolescents also commonly use the Internet for mental health information (Leanza & Alani, Reference Leanza, Alani, Moreno and Hoopes2020; Park & Kwon, Reference Park and Kwon2018), which is especially the case for adolescents who identify as racial/ethnic minorities or have parents that are less health literate (Park & Kwon, Reference Park and Kwon2018). Finally, as the first point of entry for many adolescents, DMHIs can facilitate treatment by reducing uncertainty about interactions with providers and ambiguity about treatment options (Boydell et al., Reference Boydell, Hodgins, Pignatiello, Teshima, Edwards and Willis2014). Rather than being a passive participant, teens can gain a newfound understanding and agency over their mental health, which may promote treatment seeking and engagement.
Further, while stigma toward help-seeking and mental health care is prominent across age groups (Sharac et al., Reference Sharac, McCrone, Clement and Thornicroft2010), adolescents identify stigma as one of the greatest barriers to mental health care (Gulliver et al., Reference Gulliver, Griffiths and Christensen2010). DMHIs can be anonymous, private, and accessible to teens at any time of the day and in any location, thereby allowing teens to access and receive mental health care in the way that is most comfortable for them (Toscos et al., Reference Toscos, Coupe and Flanagan2019). In this sense, DMHIs can reach diverse groups of adolescents efficiently by connecting with teens where they are (online) and in the digital spaces where they feel most comfortable. DMHIs have the potential to not only reduce the gap in mental health services and delivery, but also reduce mental health disparities that exist across youth who are marginalized or undeserved (Schueller et al., Reference Chu, Wadham and Jiang2019). DMHIs can provide readily available, reliable, and accurate mental health information to adolescents, particularly youth who are traditionally underserved in mental health care. DMHIs may also be more readily adaptable or translated into other languages, which may help with the limited availability of multilingual mental health professionals. However, inequities in access to technology may actually create a digital divide in who has access to DMHIs (Odgers & Jensen, Reference Odgers and Jensen2020). By collecting and delivering content in real time and in real-world contexts, DMHIs have the potential to inform and deliver timely, flexible, and personalized mental health care, thereby improving detection and treatment of mental health problems across risk stages and demographics (Price et al., Reference Price, Yuen and Goetter2014).
Modes of Delivery for Digital Health Interventions
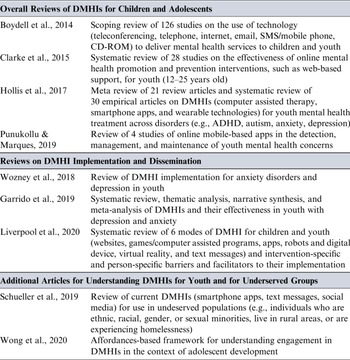
As technology evolves, an abundance of novel digital platforms and tools have been developed to improve mental health among youth and adults. DMHIs provide online services for interventions through various hardware (e.g., computer, phone, tablet, wearable) and modalities. These modalities include online/web-based interventions, video conferencing, text messaging, smartphone applications (“apps”), social media sites, game-based approaches (e.g., “serious games”) (Lister et al., Reference Li, Theng and Foo2014), virtual reality, as well as emerging technologies like passive sensing (e.g., wearables, digital phenotyping) and artificial intelligence (e.g., chatbots). Yet, technology has far outpaced research on DMHIs. Most work examining DMHIs is heavily skewed toward modalities that have existed longer (e.g., telehealth, online/web-based interventions). Newer modalities of delivering mental health services, such as mobile health (e.g., text messaging, apps), wearables, or games, are still in the earlier phases of testing for treatment effectiveness with youth. Nevertheless, given their promise for reducing the burden of mental health problems in adolescents, the field is rapidly expanding to empirically evaluate DMHIs for adolescent mental health problems. Below, we briefly discuss the potential benefits and effectiveness of a range of specific DMHI modes of delivery. Table 16.1 provides a review of suggested readings about DMHIs’ effectiveness and implementation. Later in this chapter, we will discuss potential challenges of these technologies for mental health interventions.
Table 16.1 Suggested readings for understanding DMHIs’ effectiveness, implementation, and future directions
| Overall Reviews of DMHIs for Children and Adolescents | |
|---|---|
| Boydell et al., Reference Boydell, Hodgins, Pignatiello, Teshima, Edwards and Willis2014 | Scoping review of 126 studies on the use of technology (teleconferencing, telephone, internet, email, SMS/mobile phone, CD-ROM) to deliver mental health services to children and youth |
| Clarke et al., Reference Clarke, Kuosmanen and Barry2015 | Systematic review of 28 studies on the effectiveness of online mental health promotion and prevention interventions, such as web-based support, for youth (12–25 years old) |
| Hollis et al., Reference Hollis, Falconer and Martin2017 | Meta review of 21 review articles and systematic review of 30 empirical articles on DMHIs (computer assisted therapy, smartphone apps, and wearable technologies) for youth mental health treatment across disorders (e.g., ADHD, autism, anxiety, depression) |
| Punukollu & Marques, Reference Punukollu and Marques2019 | Review of 4 studies of online mobile-based apps in the detection, management, and maintenance of youth mental health concerns |
| Reviews on DMHI Implementation and Dissemination | |
|---|---|
| Wozney et al., Reference Wozney, McGrath and Gehring2018 | Review of DMHI implementation for anxiety disorders and depression in youth |
| Garrido et al., Reference Garrido, Millington and Cheers2019 | Systematic review, thematic analysis, narrative synthesis, and meta-analysis of DMHIs and their effectiveness in youth with depression and anxiety |
| Liverpool et al., Reference Liverpool, Mota and Sales2020 | Systematic review of 6 modes of DMHI for children and youth (websites, games/computer assisted programs, apps, robots and digital device, virtual reality, and text messages) and intervention-specific and person-specific barriers and facilitators to their implementation |
| Additional Articles for Understanding DMHIs for Youth and for Underserved Groups | |
|---|---|
| Schueller et al., Reference Chu, Wadham and Jiang2019 | Review of current DMHIs (smartphone apps, text messages, social media) for use in undeserved populations (e.g., individuals who are ethnic, racial, gender, or sexual minorities, live in rural areas, or are experiencing homelessness) |
| Wong et al., Reference Wong, Madanay and Ozer2020 | Affordances-based framework for understanding engagement in DMHIs in the context of adolescent development |
Note: Full references are available in the References section.
Videoconferencing
Telehealth services (e.g., telephone and videoconferencing) most closely mirror traditional face-to-face assessment and treatment delivery, and also offer new opportunities. Videoconferencing provides synchronous communication between patients and providers, with the increased convenience for patients of eliminating travel. Being in one’s natural environment has the potential to improve ecological validity of both assessment and treatment for youth with certain mental health problems (e.g., depression, psychosis, anxiety) compared to traditional treatment in an office or hospital setting. Specifically, videoconferencing may allow the clinician to observe the home environment to better assess a teen’s home or provide opportunities to participate in more naturalistic exposures. Therapy conducted using videoconferencing has received empirical support to effectively treat a range of youth mental health problems (Myers et al., Reference Myers, Valentine and Melzer2007, Reference Myers, Valentine and Melzer2008; Nelson et al., Reference Nelson, Cain and Sharp2017). Videoconferencing is now relatively common and accepted in mental health care among professionals, youth, and their caregivers (Boydell et al., Reference Boydell, Hodgins, Pignatiello, Teshima, Edwards and Willis2014). Following the physical distancing practices of the COVID-19 pandemic (Gruber et al., Reference Gruber, Prinstein and Clark2021), videoconferencing will likely continue to increase in its use and acceptability as a means of providing mental health care to youth. Despite its more common use in mental health care compared to other DMHIs, empirical research is still underway to provide guidance for the use of videoconferencing (Nelson et al., Reference Nelson, Cain and Sharp2017), including how to ethically navigate patient boundaries in their homes, which will be critical for delivering care using this modality.
Online/Web-Based Interventions
Online or web-based platforms can provide a myriad of services. This includes: access to comprehensive mental health information (e.g., blogs, websites); scalable, affordable, and effective interventions to youth and their families for mental health problems; and translation of existing evidence-based treatments into computerized or online lessons, modules, or sessions accompanied by homework or tasks, among others. Systematic and meta-analytic reviews of randomized control trials (RCTs) support the effectiveness of online/web-based services for treating adolescent mental health problems (Clarke et al., Reference Clarke, Kuosmanen and Barry2015; Hollis et al., Reference Hollis, Falconer and Martin2017). Most studies have been conducted with youth with subclinical or clinical levels of depression and anxiety (Grist et al., Reference Grist, Croker, Denne and Stallard2019; Khanna et al., Reference Khanna, Carper, Harris and Kendall2017). To date, online interventions for these clinical problems have garnered the most support. Most online or web-based interventions are based on cognitive behavioral therapy (CBT) (Ebert et al., Reference Ebert, Zarski and Christensen2015). The majority of computerized and internet-based CBT programs were found to be of moderate to high quality (Clarke et al., Reference Clarke, Kuosmanen and Barry2015; Wozney et al., Reference Wozney, McGrath and Gehring2018). These programs included components of self-monitoring, interactive content (e.g., videos, characters storytelling, games), and both online and offline support. However, online programs now include other treatment modalities and approaches for targeting youth mental health problems (Garrido et al., Reference Garrido, Millington and Cheers2019), such as positive psychology, mindfulness (Ritvo et al., Reference Ritvo, Daskalakis and Tomlinson2019), and problem-solving (Hoek et al., Reference Hoek, Schuurmans, Koot and Cuijpers2012).
Importantly, there is a need to better understand the level of human interaction (if any) needed for online or web-based interventions to be effective with youth mental health treatment, especially to counter low rates of engagement and adherence. Most online or web-based interventions are therapist-assisted, including a virtual or online therapist or to supplement in-person and face-to-face clinician visits. Meta-analytic reviews suggest online interventions that included therapists or clinicians performed better in reducing depression and anxiety symptoms than interventions that were self-guided (Clarke et al., Reference Clarke, Kuosmanen and Barry2015; Hollis et al., Reference Hollis, Falconer and Martin2017). Indeed, some research suggests that self-guided online or web-based interventions were not effective for youth depression (Garrido et al., Reference Garrido, Millington and Cheers2019). Alternatively, some studies indicate that minimal therapist involvement was better for youth anxiety than significant or more extensive therapist involvement (Podina et al., Reference Podina, Mogoase, David, Szentagotai and Dobrean2016).
Some of the largest barriers for self-guided online treatments for adolescents are low rates of treatment completion and adherence (Clarke et al., Reference Clarke, Kuosmanen and Barry2015; Garrido et al., Reference Garrido, Millington and Cheers2019). To address these concerns, low-intensity web-based interventions have been developed to deliver skill-based interventions in single sessions (Schleider & Weisz, Reference Schleider and Weisz2018). Self-administered online single-session interventions have demonstrated effectiveness in reducing adolescent depressive symptoms, as well as other core characteristics of depression (e.g., low perceived agency, self-worth, and hopelessness; Schleider & Weisz, Reference Schleider and Weisz2018; Schleider, Dobias, Sung, & Mullarkey, Reference Schleider, Dobias, Sung and Mullarkey2020). One recent trial found that online single-session interventions demonstrate effectiveness in natural settings and also reach a large number of adolescents with one or more marginalized identities (Schleider, Dobias, Sung, Mumper, & Mullarkey, Reference Schleider, Dobias, Sung and Mullarkey2020). Thus, online single-session interventions may offer brief, low-intensity, accessible, and scalable mental health interventions for youth who may otherwise not engage in care, possibly serving as tools for universal or indicated prevention or during transitional periods of more intensive care. More research and diversification of these online brief interventions (e.g., length, type) is needed to evaluate the setting and context in which they are most effective (Schleider, Dobias, Sung, Mumper, & Mullarkey, Reference Schleider, Dobias, Sung and Mullarkey2020). Further, a recent RCT tested the effectiveness of a web-based decision aid to support young people in help-seeking for their self-harm (Rowe et al., Reference Rowe, Patel and French2018). Youth generally reported the online decision aid to be acceptable, easy to use, and informative for seeking help, which suggests another way in which online or web-based interventions can promote adolescent mental health.
Text Messaging
Text messaging can also be an affordable and effective way of providing interventions, monitoring symptoms, or prompting adolescents to engage in behaviors to promote mental health, such as coping skills during crisis. This type of platform can prompt adolescents to employ skills, as well as provide automated reminders for appointments and medication to improve treatment attendance (Branson et al., Reference Branson, Clemmey and Mukherjee2013). Texts can be personalized and tailored to the adolescent based on their needs and preferences by altering the message frequency, content, and customized interactions. Text-based services may be an especially accessible DMHI. Nearly all youth have mobile phones and smartphones and text messaging does not require internet for delivery. Further, text messaging interventions are not at risk for deletion, which is common for smartphone apps (Baumel et al., Reference Baumel, Muench, Edan and Kane2019), as text capabilities are embedded in phones. Text messaging interventions also may have lower upfront costs for development compared to apps that need to be adapted and delivered for both iOS and Android platforms. Importantly, there is some support for the effectiveness of text interventions for treating youth health problems (Loescher et al., Reference Loescher, Rains, Kramer, Akers and Moussa2018), including substance use and depression (Mason et al., Reference Mason, Ola, Zaharakis and Zhang2015; Whitton et al., Reference Whitton, Proudfoot and Clarke2015). Further, a recent text messaging intervention also improved the mental health literacy of parents of adolescents (Chu et al., Reference Chu, Wadham and Jiang2019), which may subsequently improve mental health care for teens by reducing one potential barrier to treatment.
Smartphone Apps
The widespread ownership of mobile phones, particularly smartphones, provides unparalleled and unobtrusive access to adolescents in real time and in the “real world” to deliver scalable and low-cost mental health interventions. Current mental health apps can serve multiple purposes, including for psychoeducation, monitoring symptoms or behaviors, providing “just in time” or ecological momentary interventions, and as adjunctive or stand-alone treatments. There are many potential benefits to using apps to engage youth in mental health services, including heightened sense of privacy, accessibility, convenience, and integration in daily life. Importantly, apps can be more personalized and tailored to the individual, and can provide more developmentally appropriate and interactive material that engages adolescents (Bakker et al., Reference Bakker, Kazantzis, Rickwood and Rickard2016). For some youth, the very act of mental health monitoring may be beneficial in improving symptoms (Kauer et al., Reference Kauer, Reid and Crooke2012), which can be delivered in a user-friendly manner and can be used as a preventive measure or adjunct to treatment. Monitoring apps that serve as an adjunct to treatment may increase engagement among youth, allowing adolescents to have an increased awareness and sense of agency over their own behavior and mental health symptoms. However, most monitoring apps available for download have received limited empirical support. In general, relatively few apps have been empirically tested to determine their effectiveness in treating youth mental health problems (Melbye et al., Reference Melbye, Kessing, Bardram and Faurholt-Jepsen2020; Punukollu & Marques, Reference Punukollu and Marques2019).
Although research is limited, apps designed to supplement other mental health treatment and aid care between sessions have demonstrated effectiveness, particularly for youth anxiety (Carper, Reference Carper2017; Pramana et al., Reference Pramana, Parmanto, Kendall and Silk2014; Silk et al., Reference Silk, Pramana and Sequeira2020). These apps enhance treatment exposures and skills-based practice, homework compliance, and symptom tracking between sessions. Apps also have the potential to provide adolescents with “just in time” adaptive interventions that are low-intensity and high-impact and when they most need it most, such as times of crisis. Indeed, specific suicide prevention apps have been developed (Martinengo et al., Reference Martinengo, Van Galen, Lum, Kowalski, Subramaniam and Car2019), with preliminary evidence of positive treatment effects (Arshad et al., Reference Arshad, Farhat Ul, Gauntlett, Husain, Chaudhry and Taylor2020). While not encouraged to be stand-alone treatments, digital safety planning and tools (Kennard et al., Reference Kennard, Biernesser and Wolfe2015, Reference Kennard, Goldstein and Foxwell2018) may help adolescents at risk for suicide while youth are in crisis or during high-risk periods by addressing the gap between hospital discharge and outpatient treatment.
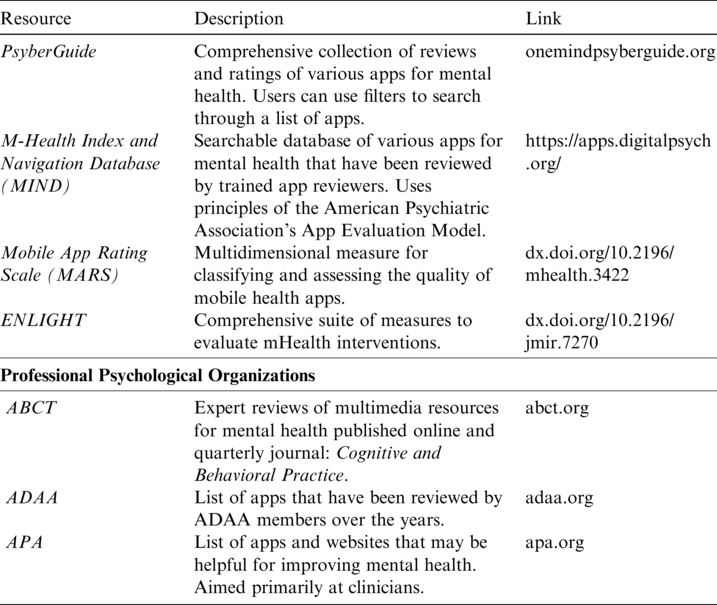
Most evidence-based apps developed by researchers are not yet commercially available (Punukollu & Marques, Reference Punukollu and Marques2019). In contrast, there are tens of thousands of commercially available apps for mental health, highlighting the large divide between apps developed for commercial use compared to those developed by researchers. Few of these available apps have been tested for effectiveness and most popular apps do not include therapeutic elements (Wasil et al., Reference Wasil, Venturo-Conerly, Shingleton and Weisz2019), though empirical evaluation is currently underway for some commercial apps (Bry et al., Reference Bry, Chou, Miguel and Comer2018). There is also very little regulatory oversight of apps and limited available high-quality information on the effectiveness of commercially available apps (Boudreaux et al., Reference Boudreaux, Waring, Hayes, Sadasivam, Mullen and Pagoto2014). This can leave adolescents vulnerable to mental health misinformation or using DMHIs that offer little therapeutic benefits (and some that could be harmful). Given that adolescents report difficulty distinguishing accurate from inaccurate information sources (Park & Kwon, Reference Park and Kwon2018), user guidance is needed to inform teens, parents, and providers (Palmer & Burrows, Reference Palmer and Burrows2021). There are several resources available that provide quantitative feedback, rubrics, and recommendations about mobile apps (Table 16.2). However, teens would likely benefit from a readily available tool, available in app stores, to provide information to them on which apps are research-based (Lagan et al., Reference Lagan, Aquino, Emerson, Fortuna, Walker and Torous2020) in a developmentally appropriate manner.
Table 16.2 Resources for evaluating mental health apps
| Resource | Description | Link |
|---|---|---|
| PsyberGuide | Comprehensive collection of reviews and ratings of various apps for mental health. Users can use filters to search through a list of apps. | onemindpsyberguide.org |
| M-Health Index and Navigation Database (MIND) | Searchable database of various apps for mental health that have been reviewed by trained app reviewers. Uses principles of the American Psychiatric Association’s App Evaluation Model. | https://apps.digitalpsych.org/ |
| Mobile App Rating Scale (MARS) | Multidimensional measure for classifying and assessing the quality of mobile health apps. | dx.doi.org/10.2196/mhealth.3422 |
| ENLIGHT | Comprehensive suite of measures to evaluate mHealth interventions. | dx.doi.org/10.2196/jmir.7270 |
| Professional Psychological Organizations | ||
|---|---|---|
| ABCT | Expert reviews of multimedia resources for mental health published online and quarterly journal: Cognitive and Behavioral Practice. | abct.org |
| ADAA | List of apps that have been reviewed by ADAA members over the years. | adaa.org |
| APA | List of apps and websites that may be helpful for improving mental health. Aimed primarily at clinicians. | apa.org |
Game-Based Interventions
Another promising domain of DMHIs is video games, which includes those that are entirely focused on mental health (e.g., “serious games” or “mental health games”) and components of video games added to DMHIs for “gamification” of mental health (Fleming et al., Reference Fleming, Bavin and Stasiak2016). With the components inherent in video games (e.g., levels, challenges, rewards), video games facilitate intrinsic motivation to incentivize adolescent engagement and adherence. Games have the potential to facilitate specific skills that also promote mental health and even improve treatment uptake, such as learning, memory, and coping skills. Games are also highly popular among adolescents (Rideout & Robb, Reference Rideout and Robb2019), which may encourage adolescent engagement. Video games can be played on familiar, low-cost platforms that are already integrated into the lives of youth (e.g., smartphones, web browsers, game systems, computers, etc). This may make these DMHIs more easily accessible compared to other cutting-edge platforms (e.g., virtual reality). Many research-based video games are still only available on computers, but gamification of mobile apps or other DMHIs offer promise (Lister et al., Reference Li, Theng and Foo2014).
The majority of research on video games has been conducted on internalizing disorders and demonstrated some effectiveness (Lau et al., Reference Lau, Smit, Fleming and Riper2016; Li et al., Reference Li, Theng and Foo2014), especially in conjunction with other treatments (Merry et al., Reference Merry, Stasiak, Shepherd, Frampton, Fleming and Lucassen2012; Schoneveld et al., Reference Schoneveld, Lichtwarck-Aschoff and Granic2018). Studies indicate that video games may be especially effective at increasing motivation, teaching cognitive restructuring, imparting relaxation techniques, and providing psychoeducation to ameliorate these types of disorders (Knox et al., Reference Knox, Lentini, Cummings, McGrady, Whearty and Sancrant2011; Pramana et al., Reference Pramana, Parmanto, Kendall and Silk2014). These rewarding elements (e.g., levels, positive feedback) also draw on adolescents’ cognitive and motivational development (Somerville & Casey, Reference Somerville and Casey2010), which may motivate adolescents to participate and engage in treatment. Some recent programs also integrate biofeedback techniques to teach breathing, meditation, and relaxation exercises (Pramana et al., Reference Pramana, Parmanto, Kendall and Silk2014). The use of avatars in gaming also provide a higher level of personalization and engagement, as well as reduce stigma toward mental health (Ferchaud et al., Reference Ferchaud, Seibert, Sellers and Escobar Salazar2020). Personalization may also have the potential to aid youth in identity development, as teens can experiment with different ways of presenting themselves. This may be particularly important for youth who identify as sexual and/or gender minorities, providing safe spaces to anonymously explore and discuss difficult topics related to their identities and mental health (DeHaan et al., Reference DeHaan, Kuper, Magee, Bigelow and Mustanski2013). Video games and gamification may be particularly compelling for adolescents with autism spectrum disorder (ASD) or those with attention deficit-hyperactivity disorder (ADHD) due to the existing popularity of video games in these populations (Yerys et al., Reference Yerys, Bertollo and Kenworthy2019). Future RCTs and reviews are needed to fully capture the benefits and evaluate the effectiveness of gaming for adolescent mental health.
Virtual and Augmented Realities
Virtual and augmented realities create new opportunities for delivering and enhancing treatments. Virtual reality provides an immersive experience that virtually transports individuals into a real or imaged physical environment. In contrast, augmented realities overlay image and video content on top of reality, enhancing a person’s in-person physical environment. Virtual and augmented realities can deliver services in an interactive manner while still remaining under the control of the adolescent and provider (Li et al., Reference Li, Yu and Shi2017). Virtual and augmented reality may be promising for youth with ASD (Berenguer et al., Reference Berenguer, Baixauli, Gomez, Andres and De Stasio2020; Vahabzadeh et al., Reference Vahabzadeh, Keshav, Abdus-Sabur, Huey, Liu and Sahin2018) and for youth with anxiety disorders (Barnes & Prescott, Reference Barnes and Prescott2018), where sensory input can be tailored to the individual need. For example, virtual realities can simulate experiences found in everyday life or expose youth to fears or situations that may not otherwise be possible in daily life (e.g., fear of flying) or the clinical setting (e.g., public speaking in large crowds). Augmented realities can further extend youth’s natural environment to simulate real-world experiences, such as specific phobias (e.g., spiders) and social interactions with peers. To date, virtual reality is more regularly used and examined with adults (Cieslik et al., Reference Cieslik, Mazurek, Rutkowski, Kiper, Turolla and Szczepanska-Gieracha2020); there is still limited empirical support on the effectiveness of virtual and augmented realities for youth mental health treatment (Grist et al., Reference Grist, Croker, Denne and Stallard2019). Despite its initial development nearly two decades ago, there continues to be a lag in the adoption of virtual reality for clinical interventions or in clinical practice, potentially due to its high cost and complex development. However, research may surge in virtual and augmented reality systems as they become more mobile and available on smartphones, commercially available, and as design becomes more centered on its potential clinical utility (Bell et al., Reference Bell, Nicholas, Alvarez-Jimenez, Thompson and Valmaggia2020).
Social Media
Given the increasing presence of social media in the daily lives of adolescents, researchers have sought to employ social media as novel tools for mental illness detection, prevention, and intervention. Adolescence is a unique developmental period during which individuals are more sensitive to social feedback, peer relationships, and peer influence (Prinstein & Dodge, Reference Prinstein and Dodge2008). Social media provides adolescents with a range of social affordances, including social support, sense of belonging, and access to a network of known and unknown peers (Nesi et al., Reference Nesi, Choukas-Bradley and Prinstein2018). Thus, social media-based DMHIs have the power to reduce stigma, increase help-seeking behaviors, connect peers, and provide support and psychoeducation about the benefits of mental health problems (Betton et al., Reference Betton, Borschmann, Docherty, Coleman, Brown and Henderson2015). Social media can also connect adolescents with needed support and information that aids in treatment engagement, symptom reduction, and even as a form of suicide prevention (Robinson et al., Reference Robinson, Cox and Bailey2016). Indeed, social media campaigns targeting mental health awareness and stigma reduction have demonstrated effectiveness in reducing stigma and increasing adolescent treatment engagement (Booth et al., Reference Booth, Allen, Bray Jenkyn, Li and Shariff2018).
Research is still in its nascency for employing existing social media platforms to deliver interventions, with most systematic reviews identifying a need for high-quality studies examining online peer-to-peer support (Ali et al., Reference Ali, Farrer, Gulliver and Griffiths2015) or social networking sites (Ridout & Campbell, Reference Ridout and Campbell2018). Thus far, social media-based interventions that include social networking or peer support components have been found to be acceptable, feasible, and safe for youth across a range of mental health problems (Ridout & Campbell, Reference Ridout and Campbell2018), including depression (Radovic et al., Reference Radovic, Gmelin, Hua, Long, Stein and Miller2018; Rice et al., Reference Rice, Goodall and Hetrick2014) and first-episode psychosis (Alvarez-Jimenez et al., Reference Alvarez-Jimenez, Bendall and Lederman2013; McEnery et al., Reference McEnery, Lim and Knowles2021). These interventions are professionally mediated to ensure networks remain supportive and informational, while also training some youth to be leaders in these peer networks.
Emerging Digital Tools
There are several new and emerging digital tools, such as passive sensing and artificial intelligence, that may further revolutionize how and in what ways DMHIs promote adolescent mental health. One exciting avenue for DMHIs is the use of passive sensing from wearables or digital phenotyping of individuals’ online or mobile footprints. With the integration of passive sensors from smartphones or wearables, ecological momentary interventions can be developed that provide just-in-time and adaptive treatments (Russell & Gajos, Reference Russell and Gajos2020). As smartphones are nearly always with adolescents (Anderson & Jiang, Reference Anderson and Jiang2018), the rich data collected by smartphone sensors can yield information about location, activity levels, light exposure, social networking activity, and social connection (e.g., calls/messages). This information can be synthesized into clinically meaningful metrics of sleep, physical activity, emotional distress, and upstream clinical presentations (Huckvale et al., Reference Huckvale, Venkatesh and Christensen2019; Vaidyam et al., Reference Vaidyam, Halamka and Torous2019). This field is rapidly evolving for youth (Russell & Gajos, Reference Russell and Gajos2020), particularly to address the rising mental health concerns and suicide crisis in this population (Allen et al., Reference Allen, Nelson, Brent and Auerbach2019; Torous, Larsen, et al., Reference Torous, Larsen and Depp2018). To date, few apps have been developed that operationalize digital phenotyping data in actual interventions (Wong et al., Reference Wong, Madanay and Ozer2020), though some are currently being developed and tested.
Artificial intelligence has also progressed in recent years, including the development of fully automated conversational agents (e.g., chatbots). Chatbots are able to process text and emojis entered by a participant and provide personalized responses that aim to mimic human conversation. Unlike other DMHIs that are fully automated, chatbots offer a level of direct and synchronous interaction that may motivate users to continue participation and even provide empathic support (Morris et al., Reference Morris, Kouddous, Kshirsagar and Schueller2018). Chatbots can provide daily check-ins for participants’ symptoms and behaviors. They can also be readily integrated with other passive sensing metrics to increase awareness and individualization. Since some individuals are more willing to disclose to a machine than other individuals (Lucas et al., Reference Lucas, Gratch, King and Morency2014), chatbots can serve as moderators or agents when real human interactions are not available. While preliminary studies indicate symptom reduction for adults with the use of chatbots (Fitzpatrick et al., Reference Fitzpatrick, Darcy and Vierhile2017), particularly for psychoeducation and self-guided treatment, there is still much work needed to understand the risks and benefits of using this mode of delivery for DMHIs (Vaidyam et al., Reference Vaidyam, Halamka and Torous2019). Nevertheless, integrating components of artificial intelligence like chatbots into other DMHIs may enhance connectedness and engagement in care for adolescents.
Challenges and Future Directions to Digital Mental Health Research and Treatment
Although DMHIs demonstrate great potential for delivering scalable and low-cost mental health services to adolescents, many obstacles remain. Simply stated, there is a significant divide between research and technology development. Commercially available technology is far outpacing research on the effectiveness and implementation of DMHIs for youth, as well as the enforcement of data privacy and security measures. The scalability of DMHIs also remains in question to determine whether these tools are actually as cost-effective, accessible, and effective in reaching underserved youth as initially promised. This section outlines the current challenges of the field and critical directions for growth to improve our understanding and use of DMHIs for adolescent mental health care.
Effectiveness of DMHIs: For Whom and in What Contexts?
There is a dearth of research investigating the effectiveness of DMHIs across modalities in adolescents, particularly newer and currently popular modes of delivery (e.g., smartphone apps). While most research has been conducted on web-based/online interventions, more rigorous research is needed to examine the effectiveness of DMHIs delivered via mobile applications, social media, and gaming platforms. These DMHI modalities represent areas of potential high engagement for teens. To date, most research also has focused on DMHIs for youth depression and anxiety. High-quality research is needed to examine DMHIs for specific mental health conditions beyond internalizing disorders (Hollis et al., Reference Hollis, Falconer and Martin2017), such as youth with ASD (Yerys et al., Reference Yerys, Bertollo and Kenworthy2019), psychosis (Reilly et al., Reference Reilly, Mechelli, McGuire, Fusar-Poli and Uhlhaas2019), and eating disorders (Loucas et al., Reference Loucas, Fairburn, Whittington, Pennant, Stockton and Kendall2014). Most research is also limited to short-term outcomes, and research on the long-term effects of DMHIs is needed. It also is critical to understand which youth may benefit from DMHIs and in what contexts, such as different stages of clinical severity or treatment progression. For instance, certain modalities may be most appropriate as a gateway to care, during waitlist or transitions to care, or “booster” sessions to supplement prior treatment and prevent relapse. Certain DMHI modalities also may pair better with certain conditions, such as using virtual or augmented realities with youth who have ASD and ADHD (Yerys et al., Reference Yerys, Bertollo and Kenworthy2019). While there are concerns noted about using DMHIs clinically with high-risk adolescents (Palmer & Burrows, Reference Palmer and Burrows2021), recent research suggests DMHIs may be effective in reducing suicidality (Hetrick et al., Reference Hetrick, Yuen and Bailey2017) and for use in screening, prevention, and intervention with psychosis (Reilly et al., Reference Reilly, Mechelli, McGuire, Fusar-Poli and Uhlhaas2019). This research points to the potential utility of DMHIs for higher-risk adolescents as well. However, research would benefit from more systematic examination of how the effectiveness of DMHIs varies across clinical presentations, symptoms, and severity. Research is also needed to evaluate effectiveness of DMHIs by intervention stage (e.g., prevention, intervention) and type (e.g., skill building, CBT, exposure). Further, the active ingredients of DMHIs and fidelity to evidence-based approaches remain to be specified (Hollis et al., Reference Hollis, Falconer and Martin2017). More details about DMHI design and implementation would help isolate the most effective elements, such as short motivational messages, gamification features, or symptom monitoring (Whitton et al., Reference Whitton, Proudfoot and Clarke2015). Research on the dose of clinical/human interaction needed (if at all) to engage and treat adolescents also is imperative, particularly since level of clinician involvement affects both cost-effectiveness and scalability.
Gap between Research and Commercial Technology
The fast pace at which technology is developed presents a major obstacle for the academic and research community. In contrast to commercial technology, research is typically produced at a much slower pace. RCTs are the “gold-standard” approach for determining efficacy and effectiveness. However, RCTs can take 5–7 years from initiation to dissemination (Hollis et al., Reference Hollis, Falconer and Martin2017), and even longer for broader implementation. This length of time may render a DMHI modality irrelevant by the time it is deemed effective. Timing may be particularly important to consider in the context of DMHI research for adolescents, who rapidly adopt new platforms and technology. DMHIs that are specific to a single platform or modality may quickly become obsolete or outgrow their functionality. For instance, text-based interventions may be effective, but it remains unclear to what extent teens will use texting platforms as social media messaging continues to become more common. Thus, revised or alternate approaches to developing and testing DMHIs are needed that balance the need for rigorous testing with the need for evaluations that are timely and relevant (Murray et al., Reference Murray, Hekler and Andersson2016; Pham et al., Reference Pham, Wiljer and Cafazzo2016). One such approach may be reducing the need for reevaluation for revised iterations of DMHIs that do not alter the core therapeutic principles (Torous et al., Reference Torous2019). Another option to bridge the research-commercial gap is to partner with existing apps that are already popular with teens and test their effectiveness or incorporate evidence-based approaches as needed. This may be a particularly effective method given that teens report that brand familiarity helps with app engagement (Liverpool et al., Reference Liverpool, Mota and Sales2020). Furthermore, systematic and consensus guidelines on DMHIs are needed (Torous et al., Reference Torous2019), which may help close the gap between commercial and research digital tools and ensure high-quality mental health services for adolescents.
Privacy and Security
One major challenge at the forefront of DMHI research is the privacy and safety of digital spaces (Wong et al., Reference Wong, Madanay and Ozer2020). Indeed, most teens are unaware of who has access to their data or how it is being used. Teen privacy and data security present concerns for providers with recommending or implementing DMHIs with adolescents. While privacy policies may exist for some apps, a recent review of apps targeting teens found that most data privacy statements were written at or above a 12th-grade reading level (Das et al., Reference Das, Cheung, Nebeker, Bietz and Bloss2018), which is problematic for adolescents and their parents. Without knowing how their data will be used, adolescents may agree to have their private information sold and marketed to third-party companies. Violations of teens’ privacy directly conflict with adolescents’ strong preference for mental health privacy in engagement with DMHIs (Park & Kwon, Reference Park and Kwon2018). Uncertainty regarding teens’ data privacy also presents ethical concerns for clinicians in recommending or using commercially available digital tools with patients (Kerst et al., Reference Kerst, Zielasek and Gaebel2020; Palmer & Burrows, Reference Palmer and Burrows2021). Thus, it is critical that researchers take special consideration in ensuring that adolescents are aware of how their digital data will be stored and secured (Torous, Reference Torous2019). One potential avenue for addressing these concerns could be increasing digital health literacy among adolescents, such as through school-based curricula in childhood and throughout adolescence (see Chapter 15 of this volume). Directly addressing digital mental health literacy with teens may help them navigate the overabundance of digital tools and select DMHIs that are private, safe, and from reliable sources (Park & Kwon, Reference Park and Kwon2018). However, it is also important for researchers to take a more active role in disseminating tools (Lagan et al., Reference Lagan, Aquino, Emerson, Fortuna, Walker and Torous2020) or advocating for policies that will aid teens, providers, and parents in understanding and identifying evidence-based DMHIs as they develop. Research on whether these approaches improve teens’ perceived and actual privacy, as well as the reach and engagement of DMHIs, would further inform future directions in this area.
Youth-Centered DMHIs
Most DMHIs are plagued by low rates of adherence from participants (Fleming et al., Reference Fleming, Bavin, Lucassen, Stasiak, Hopkins and Merry2018; Hollis et al., Reference Hollis, Falconer and Martin2017). Programs that are self-guided or that include minimal human (especially clinician) contact suffer the most from low engagement across modalities compared to interventions that include more human and clinician contact. Indeed, most teens stop using mental health apps within days to weeks (Baumel et al., Reference Baumel, Muench, Edan and Kane2019), do not complete all modules of online interventions (Christensen et al., Reference Christensen, Griffiths and Farrer2009), and do not use video games created by researchers in their daily lives (Fleming et al., Reference Fleming, Bavin, Lucassen, Stasiak, Hopkins and Merry2018). This suggests a large difference between clinical trials in which adolescents are incentivized, which still struggle from lower adherence rates (Clarke et al., Reference Clarke, Kuosmanen and Barry2015), and real-world application.
While there are many factors that contribute to adolescents’ poor engagement in DMHIs (Torous, Nicholas, et al., Reference Torous, Larsen and Depp2018), poor usability and the absence of adolescent-specific design may be key components. Collaborating with experts across disciplines (e.g., design, engineering) is critical in designing DMHIs that are more user-friendly and that integrate components well-received by adolescents, such as the inclusion of graphics, video, personalization, and elements that facilitate social connection (Liverpool et al., Reference Liverpool, Mota and Sales2020). Adolescents’ input and preferences, particularly from those with lived experience of mental illness, are especially important in the development of DMHIs (Scholten & Granic, Reference Scholten and Granic2019). Furthermore, leveraging developmental science to inform the development, design, and implementation of DMHIs may be particularly effective for adolescents (Giovanelli et al., Reference Giovanelli, Ozer and Dahl2020). For instance, adolescents are highly sensitive to social contexts and, perhaps unsurprisingly, DMHIs that are conducted without any provider interaction are less effective (Hollis et al., Reference Hollis, Falconer and Martin2017). Though social media interventions hold particular promise, there are major challenges for developing DMHIs via social media (Pagoto et al., Reference Pagoto, Waring and May2016). For instance there is a need to adapt content to fit specific social media platforms and to stay abreast of evolving norms of the targeted population (Pagoto et al., Reference Pagoto, Waring and May2016). This is particularly challenging for teens given the relatively quick adoption and extinction of platforms and norms, which suggests that DMHIs using social media may be best developed across platforms rather than relying on a single medium. However, researchers should also consider the unique affordances of social media, including its social, cognitive, identity, and emotional affordances, in designing mental health interventions for social media that best fit the needs and goals of targeted youth (Moreno & D’Angelo, Reference Moreno and D’Angelo2019). However, research is needed to examine the affordances of DMHIs that are most important to adolescents (Wong et al., Reference Wong, Madanay and Ozer2020).
Scalability of DMHIs
Relatedly, research on the scalability and implementation of DMHIs in real-world contexts is sorely needed (Liverpool et al., Reference Liverpool, Mota and Sales2020). Most research has focused on acceptability, adoption, and appropriateness, but the cost and sustainability of DMHIs remain understudied (Wozney et al., Reference Wozney, McGrath and Gehring2018). Although there is potential for improving mental health outcomes for adolescents, DMHIs are still not widely employed in clinical practice or within health systems. Thus, research efforts should assess both provider and patient acceptability and intention to use DMHIs. It is also critical to address potential barriers to their implementation, such as comfort level, privacy, and safety concerns (Kerst et al., Reference Kerst, Zielasek and Gaebel2020). Further, the costs of development and maintenance for DMHIs, including long-term maintenance (Hollis et al., Reference Hollis, Falconer and Martin2017), is important for scalability and integration in clinical care (Liverpool et al., Reference Liverpool, Mota and Sales2020). One approach to overcoming barriers in long-term maintenance DMHIs is to increase the use of open-access methods and resource-sharing to ensure DMHIs are accessible and free. Using open-access methods might also increase the reach of DMHIs to underserved populations. Interdisciplinary research teams that include various stakeholders may be most effective in troubleshooting these barriers and improving the implementation and scalability of DMHIs (Torous et al., Reference Torous2019; Torous, Wisniewski, et al., Reference Torous, Larsen and Depp2018). Thus, research and development of DMHIs should collaborate across disciplines, including medicine, computer science, engineering, public health, schools, education, policy-makers, and clinical care. Most, importantly, adolescents and their families should play an integral part in improving the scalability of DMHIs.
Culturally Sensitive and Equitable DMHIs
While DMHIs may be able to reduce health disparities through their reach and accessibility, it is important to develop and implement interventions that are equitable and inclusive, and that engage diverse communities in DMHI design and implementation. For instance, most research with DMHIs in youth has been done in developed countries, and consequently, there is much less access to DMHIs in lower- and middle-income countries (Liverpool et al., Reference Liverpool, Mota and Sales2020). Even within developed countries, disparities exist both in access to high-quality mental health services and for adolescents who are racial, ethnic, sexual, or gender minorities. There is a dire need to customize interventions to these minority and historically underserved populations (Schueller et al., Reference Schueller, Hunter, Figueroa and Aguilera2019). Yet, it is critical that DMHIs engage in participatory designs that reflect the diverse and evolving needs of these populations (Schueller et al., Reference Schueller, Hunter, Figueroa and Aguilera2019), as some online resources may inadvertently increase feelings of marginalization and misinformation (Steinke et al., Reference Steinke, Root-Bowman, Estabrook, Levine and Kantor2017). For instance, DMHIs that “group together” all sexual and gender minority youth or all Latinx/Hispanic youth may further alienate individuals from mental health services given the large heterogeneity that exists within these populations (Schueller et al., Reference Schueller, Hunter, Figueroa and Aguilera2019; Steinke et al., Reference Steinke, Root-Bowman, Estabrook, Levine and Kantor2017). Further, few to no DMHIs have been specifically designed or implemented that target the unique needs of youth with marginalized and intersecting identities. Thus, DMHIs may have the potential to increase access and delivery of equitable and effective mental health services to youth across demographics; however, research on culturally sensitive DMHIs remains a high-priority area.
Double-Edged Sword of Digital Media
There is a potential irony in using DMHIs with adolescents amid general concerns about adolescents’ use of and reliance on digital technology. Using DMHIs for mental health may be especially concerning for youth who may use or experience digital media in ways that further exacerbate their symptoms (Radovic et al., Reference Radovic, Gmelin, Stein and Miller2017). Thus, a critical future direction will be the development and tailoring of interventions or programs that help youth, particularly those with mental illness, use digital media in a way that promotes mental health. One such example is #chatsafe, which is an international program that helps teens communicate safely online with others about suicide (Robinson et al., Reference Robinson, Hill and Thorn2018). Preliminary results suggest that individuals who participated in #chatsafe felt better equipped to communicate safely about suicide online, as well as to identify and support others who may be at risk for suicide (Robinson et al., Reference Robinson, Teh, Lamblin, Hill, La Sala and Thorn2020; Thorn et al., Reference Thorn, Hill and Lamblin2020). To date, there is still limited research on interventions that target media use and behaviors among youth with mental health problems. However, there are several emerging interventions that use mindfulness (Weaver & Swank, Reference Weaver and Swank2019) and daily reflection (Hou et al., Reference Hou, Xiong, Jiang, Song and Wang2019) as a means to improve mindless scrolling and reduce unwanted use. Further, a recent values-alignment intervention focused on adolescents’ own motivations to self-regulate their social media use (Galla et al., Reference Galla, Choukas-Bradley, Fiore and Esposito2021), finding that adolescents who participated in the intervention experienced more motivation to self-regulate and independently changed their social media behaviors to be consistent with their values. Thus, it is important to consider the potential for conflicting messages regarding the risks and benefits of digital media when using DMHIs with adolescents. Further, it will be critical to continue designing and implementing interventions, offered both digitally and in other formats, that help adolescents use media in a way that promotes their mental health.
Conclusion
Given the large gap between the need and delivery of mental health services for adolescents, DMHIs have received considerable attention among researchers and providers. The current state of research with youth suggests only preliminary effectiveness of most DMHIs, with the most support for online/web-based interventions for depression and anxiety (Hollis et al., Reference Hollis, Falconer and Martin2017). However, the field is rapidly expanding to evaluate DMHIs and to address the current challenges in research on DMHIs’ effectiveness and implementation. Thus, DMHIs continue to hold great promise in delivering accessible, developmentally informed, and scalable interventions for the detection, monitoring, prevention, and treatment of adolescent mental health problems.