Book contents
- Field Hospitals
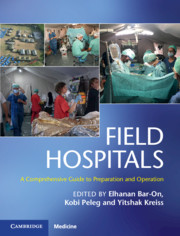
- Field Hospitals
- Copyright page
- Contents
- Contributors
- Preface
- Section 1 History
- Section 2 Scenarios
- Section 3 Operational Considerations
- Section 4 Clinical Considerations
- Chapter 13 Advanced Triage Management for Emergency Medical Teams
- Chapter 14 Medical Aspects in a Field Hospital
- Chapter 15 Pediatrics in a Field Hospital
- Chapter 16 Surgery in a Field Hospital
- Chapter 17 Wound Management in a Field Hospital Environment
- Chapter 18 Orthopedics in a Field Hospital
- Chapter 19 Burn Care in a Field Hospital Environment
- Chapter 20 Obstetrics and Gynecology in a Field Hospital
- Chapter 21 Otolaryngology and Maxillofacial Surgery in a Field Hospital
- Chapter 22 Ophthalmology in a Field Hospital
- Chapter 23 Anesthesia and Pain Management in Field Hospitals
- Chapter 24 Intensive Care Unit Buildup Within a Field Hospital Setting
- Chapter 25 Infectious Diseases and Public Health in a Field Hospital
- Chapter 26 Primary and Ambulatory Care in a Field Hospital in Disaster Areas
- Chapter 27 Mental Health in a Field Hospital
- Chapter 28 Nursing in a Field Hospital
- Section 5 Additional Contextual Considerations
- Index
- Plate Section (PDF Only)
- References
Chapter 22 - Ophthalmology in a Field Hospital
from Section 4 - Clinical Considerations
Published online by Cambridge University Press: 09 January 2020
- Field Hospitals
- Field Hospitals
- Copyright page
- Contents
- Contributors
- Preface
- Section 1 History
- Section 2 Scenarios
- Section 3 Operational Considerations
- Section 4 Clinical Considerations
- Chapter 13 Advanced Triage Management for Emergency Medical Teams
- Chapter 14 Medical Aspects in a Field Hospital
- Chapter 15 Pediatrics in a Field Hospital
- Chapter 16 Surgery in a Field Hospital
- Chapter 17 Wound Management in a Field Hospital Environment
- Chapter 18 Orthopedics in a Field Hospital
- Chapter 19 Burn Care in a Field Hospital Environment
- Chapter 20 Obstetrics and Gynecology in a Field Hospital
- Chapter 21 Otolaryngology and Maxillofacial Surgery in a Field Hospital
- Chapter 22 Ophthalmology in a Field Hospital
- Chapter 23 Anesthesia and Pain Management in Field Hospitals
- Chapter 24 Intensive Care Unit Buildup Within a Field Hospital Setting
- Chapter 25 Infectious Diseases and Public Health in a Field Hospital
- Chapter 26 Primary and Ambulatory Care in a Field Hospital in Disaster Areas
- Chapter 27 Mental Health in a Field Hospital
- Chapter 28 Nursing in a Field Hospital
- Section 5 Additional Contextual Considerations
- Index
- Plate Section (PDF Only)
- References
Summary
The role of the ophthalmologist in the field hospital is important and irreplaceable; ocular injuries during a disaster can result in considerable disability and often require the care of an ophthalmologic surgeon. The ophthalmology field is a high technology area with the need for expensive equipment that are not available in the field hospital. The working scenario for the ophthalmologist in the delegation is very different than the one existing in a hospital in developed countries; therefore, first and foremost, a change in mental attitude is needed.
Understanding the characteristics of ocular injuries during various types of disasters in different geographical areas is important to be able to prepare for them properly, both mentally and practically.
Another dominant factor is time: the nature of ophthalmology patient’s varies significantly as time passes.
While in the first days after the disaster most ocular injuries are related to disaster, as time passes most of the referral patients are nondisaster related injuries such as chronic ocular problems of the local population.
This chapter covers the preparation needed for treating ocular injuries during disasters and the ophthalmology layout in the field hospital scenario.
Keywords
- Type
- Chapter
- Information
- Field HospitalsA Comprehensive Guide to Preparation and Operation, pp. 217 - 224Publisher: Cambridge University PressPrint publication year: 2020