 Advancing Women's Health Through Medical Education
Advancing Women's Health Through Medical Education Book contents
- Advancing Women’s Health Through Medical Education
- Reviews
- Advancing Women’s Health Through Medical Education
- Copyright page
- Dedication
- Contents
- Contributors
- Preface
- Acknowledgments
- Introduction
- Section I Abortion Training: Workforce, Leadership, Social & Political Impact
- Section II Integration of Abortion into Graduate Medical Education
- Section III Family Planning Curricular Design & Implementation
- Section IV Reproductive Health Services & Abortion Training: Global Examples
- Index
- References
Section III - Family Planning Curricular Design & Implementation
Published online by Cambridge University Press: 30 July 2021
- Advancing Women’s Health Through Medical Education
- Reviews
- Advancing Women’s Health Through Medical Education
- Copyright page
- Dedication
- Contents
- Contributors
- Preface
- Acknowledgments
- Introduction
- Section I Abortion Training: Workforce, Leadership, Social & Political Impact
- Section II Integration of Abortion into Graduate Medical Education
- Section III Family Planning Curricular Design & Implementation
- Section IV Reproductive Health Services & Abortion Training: Global Examples
- Index
- References
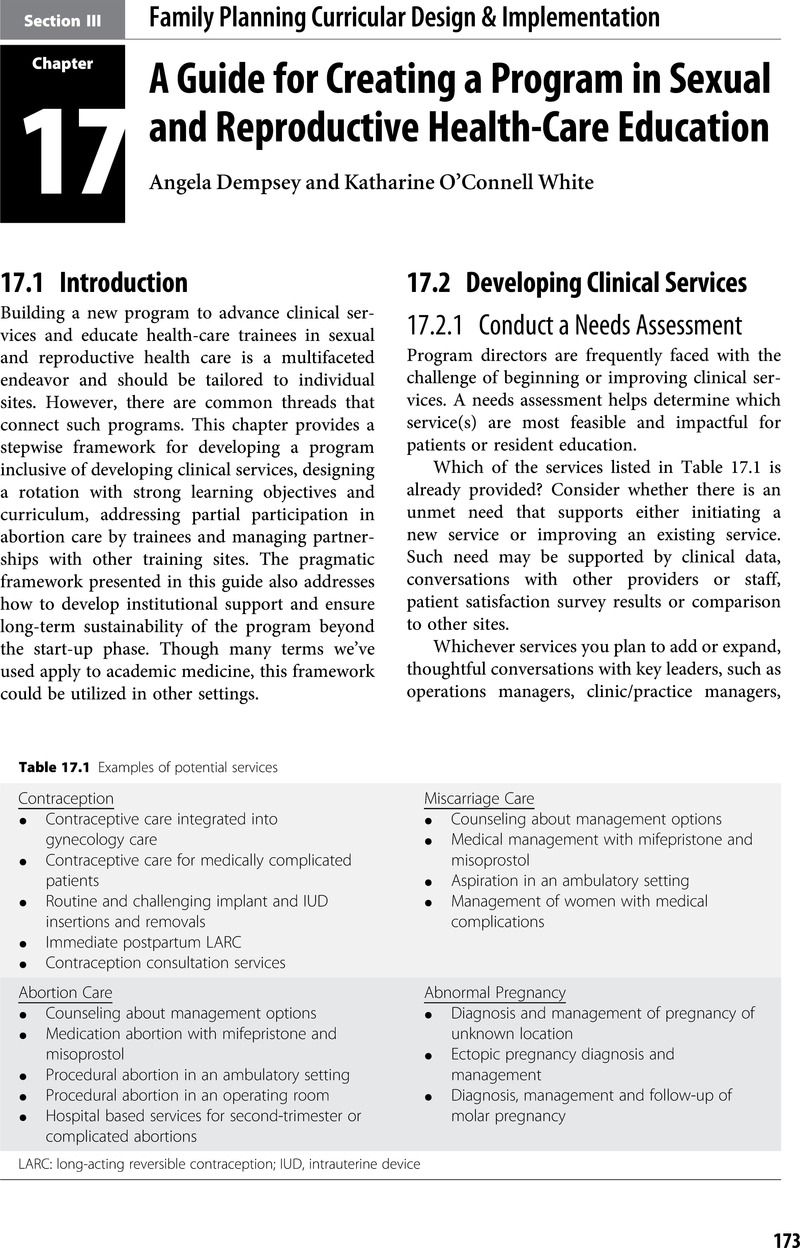
Summary
- Type
- Chapter
- Information
- Advancing Women's Health Through Medical EducationA Systems Approach in Family Planning and Abortion, pp. 173 - 262Publisher: Cambridge University PressPrint publication year: 2021
