Mandatory fortification of bread flour with folic acid is currently being considered by governments of the UK(1) and New Zealand(2). Data from other countries have shown that such fortification programmes can help achieve significant reductions in the incidence of neural tube defects, in particular in high-risk population groups(Reference Hilder3). Despite these confirmed public health benefits, some countries have hesitated to implement mandatory folic acid fortification for a number of reasons, including suggestions of a possible increased incidence of colorectal cancer(Reference Hirsch, Sanchez and Albala4,Reference Mason, Dickstein and Jacques5) , due to potential adenoma-promoting effects of folic acid fortification(Reference Cole, Baron and Sandler6). The timing of increases in colorectal cancer incidence rates in USA and Canada has been provided as evidence supporting the role of folic acid in increasing colorectal cancer risk(Reference Mason, Dickstein and Jacques5). A recent USA expert workshop identified priorities for continued research of the potential adverse health effects of excess folate or folic acid intake(Reference Maruvada, Stover and Mason7).
Bread flour in Australia has been fortified with folic acid since September 2009. Monitoring of this mandatory fortification has shown good compliance(8). While ecological data analyses have obvious limitations with assessing causality, to date Australian trends in colorectal cancer incidence have not been considered in relation to the introduction of mandatory bread flour fortification. We therefore used population-level data to evaluate colorectal cancer incidence patterns before and after introduction of mandatory folic acid fortification of bread flour in Australia.
Methods
We used data from the Australian Cancer Database, published by the Australian Institute of Health and Welfare(9). These data include all new cases of primary invasive colorectal cancers (ICD codes C18-C20) diagnosed between 1999 and 2016 (the most recent data available). We plotted age-standardised incidence of colorectal cancer (cases per 100 000, standardised to the 2001 Australian population) and calculated age-adjusted rate ratios with 95 % CIs (95 % CI) using the method by Fay and Feuer(Reference Fay and Feuer10). Age-group-specific incidence rate ratios with 95 % CI were calculated using a negative binomial regression model. Joinpoint Trend Analysis Software version 4.8.0.1 was used to analyse trends(11).
Results
Age-standardised colorectal cancer incidence generally decreased between 1999 and 2016 (Fig. 1a), although there was a slight increase in rates in 2010 compared with 2009 (62·8 v. 61·6 cases per 100 000, age-adjusted rate ratio 1·02 (95 % CI 0·99, 1·04) (Fig. 1b). Age-specific patterns (Fig. 2) indicated that the slight increase in 2010 v. 2009 was mainly due to a higher incidence in people aged 55–59 years (99·0 v. 88·1 per 100 000; incidence rate ratio 1·12 (95 % CI 1·04, 1·22)) and 65–69 years (229·9 v. 210·9 per 100 000; incidence rate ratio 1·09 (95 % CI 1·02, 1·16)), while other age groups changed very little (data not shown). Trend analysis indicated a joinpoint in 2010, with the significant decrease in incidence observed between 1999 and 2010 (Annual Percent Change: –0·4 % (95 % CI –0·7, 0·0)) becoming more pronounced between 2010 and 2016 (Annual Percent Change: –2·2 % (95 % CI –3·1, –1·3)).

Fig. 1 Age-standardised incidence rates (95 % CIs) for colorectal cancer in Australia. (a) Colorectal cancer incidence per 100 000 in 1999–2016. (b) A non-zero intercept detail of Figure 1a
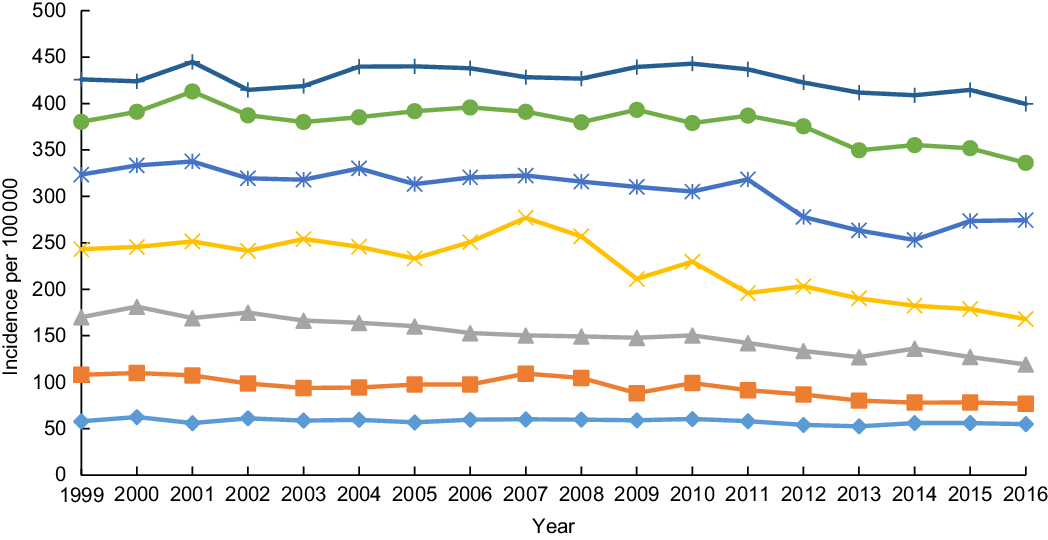
Fig. 2 Colorectal cancer incidence by age group in Australia, 1999–2016. ![]() 50–54 years;
50–54 years; ![]() 55–59 years;
55–59 years; ![]() 60–64 years;
60–64 years; ![]() 65–69 years;
65–69 years; ![]() 70–74 years;
70–74 years; ![]() 75–79 years;
75–79 years; ![]() 80–84 years
80–84 years
Discussion
While causation cannot be assessed from these population-level data, our observations indicate that there is no evidence that introduction of mandatory folic acid fortification of bread flour in 2009 has influenced colorectal cancer incidence in Australia. The two age sub-groups in which colorectal cancer incidence was slightly higher in the year following introduction of mandatory fortification (55–59 and 65–69 years) were affected by suspension of the national bowel cancer screening programme in May 2009, due to faulty faecal occult blood tests(12). At that time, people aged 50, 55 and 65 years were eligible to participate in the bowel cancer screening program. The screening programme was resumed in November 2009, and affected person were reinvited to be screened. Combined this may have had the effect of artificially reducing 2009 incidence and increasing 2010 incidence. This is consistent with other countries where changes in bowel cancer screening participation(Reference Keum and Giovannucci13) had been noted in response to concerns about possible negative effects of folic acid fortification programmes on colorectal cancer incidence.
Thus, the small fluctuations in colorectal cancer incidence around the year of introduction of mandatory folic acid fortification coincide with known variations in screening participation. These variations may also be due to normal, random year-to-year variation of colorectal cancer incidence observed in populations. For most cancer risk factors, there is a lag period between exposure to the risk factor and the subsequent diagnosis of cancer. Indeed, estimates of the latency period between exposure to risk factors and colorectal cancer diagnosis vary widely from 4 to 20 years(Reference Lee, Willett and Fuchs14,Reference Shield, Freisling and Boutron-Ruault15) . Given this, it would be surprising if a fortification-induced increase in the population incidence of colorectal cancer incidence were observed in the year after its introduction. Our trend analysis indicated an acceleration in the rate of decline in colorectal cancer incidence in the seven years following implementation of mandatory folic acid fortification. The continued decrease in colorectal cancer incidence rates after 2010 provides further evidence against a negative impact of folic acid fortification.
These findings appear to contrast with observations in Iran(Reference Moazzen, Dastgiri and Dolatkhah16), though direct comparisons with other countries is difficult, for example, due to differences in fortification regimes and different colorectal cancer surveillance practices.
In conclusion, while definitive evidence likely requires the establishment of large-scale cohort studies or randomised controlled trials, our population-level findings are consistent with the position by Cancer Council Australia and the Cancer Society of New Zealand that folic acid fortification of bread flour for the prevention of neural tube defects does not adversely affect colorectal cancer incidence(17). Increasing the scope of quantitative data at the individual and population level about the impact of folic acid on colorectal cancer internationally should remain a priority, to ensure that decisions made by health agencies are made on the best available evidence.
Acknowledgements
Acknowledgements: N/A. Financial support: This research received no specific grant from any funding agency, commercial or not-for-profit sectors. Conflict of interest: None. Authorship: JCvdP conceived the analyses, PB extracted the data and performed the analyses, LBS and JCvdP created the graphs. All authors contributed to interpretation of the results and writing of the manuscript. Ethics of human subject participation: Ethical approval was not required for this study because it uses population-level aggregate data obtained from cancer registries only.





