Introduction
Many chronic patients will at some point have end-of-life palliative needs (Gómez-Batiste et al., Reference Gómez-Batiste, Martínez-Muñoz and Blay2014). In order to achieve the best possible quality of life for patients and families, health professionals need to acquire specific skills and have positive attitudes toward palliative care, so that they can respond appropriately to patients’ and their families’ needs (Smith, Reference Smith2003; de Vlieger et al., Reference de Vlieger, Gorchs and Larkin2004; Agusti et al., Reference Agusti, Esquerda and Amorós2018; Jiang et al., Reference Jiang, Lu and Ying2019).
Bandura (Reference Bandura, Sternberg and Kolligian1990) defines competence as the ability to translate secondary skills (cognitive, social, emotional, and sensory-motor), knowledge, values, and attitudes into appropriate actions. Attitudes refer to the positive or negative evaluations that people make about any aspect of reality (Briñol et al., Reference Briñol, Falces, Becerra and Cejudo2007). Traditionally, attitudes have been considered to have three fundamental components: affective (feelings or affective evaluation about the attitude object), cognitive (knowledge, opinion, conviction, or thought about the attitude object) and behavioral (behavior in the presence of the attitude object) (Escámez et al., Reference Escámez, García and Pérez2007). Attitudes are directly related to the thoughts and beliefs one has toward the object of attitude.
The training that health professionals receive in relation to end-of-life care has been found to be deficient: Agusti et al. (Reference Agusti, Esquerda and Amorós2018) showed how medical students showed great concern about the death of patients. On the other hand, Bassah et al. (Reference Bassah, Seymour and Cox2014) conclude in their review on end-of-life attitudes in nursing students that little time is usually devoted to palliative care education or that it is often included in other specialized nursing courses. This can cause stress and anxiety for professionals when caring for patients in end-of-life situations, which can affect their own health in the long term (Cox et al., Reference Cox, Griffiths and Rial-González2000; Mallory, Reference Mallory2003; Caton and Klemm, Reference Caton and Klemm2006; Shoji et al., Reference Shoji, Cieslak and Smoktunowicz2016).
Moreover, training in palliative care and previous experience related to the end of life have an influence on improving the attitude of health professionals toward the care of patients at the end of life (Berndtsson et al., Reference Berndtsson, Karlsson and Rejnö2019; Dimoula et al., Reference Dimoula, Kotronoulas and Katsaragakis2019; Smothers et al., Reference Smothers, Young and Dai2019). At the same time, a more positive attitude to care for these people is also associated with less fear of death and avoidance of death, anxiety, and stress (Espinoza-Venegas et al., Reference Espinoza-Venegas, Luengo-Machuca and Sanhueza-Alvarado2016; Bermejo et al., Reference Bermejo, Villacieros and Hassoun2018; Barnett et al., Reference Barnett, Reed and Adams2020).
Quality palliative care requires both the competence of the health professionals and a positive attitude on their part that promotes dignified care, where in addition to pain relief and symptom control, there is emotional accompaniment (Espinoza-Venegas et al., Reference Espinoza-Venegas, Luengo-Machuca and Sanhueza-Alvarado2016). The attitude of professionals has been found to be one of the most significant predictors of quality of care, which has a positive impact on quality of life at the end of patients’ lives (Ascencio et al., Reference Ascencio, Allende and Verastegui2014). Negative attitudes create barriers to providing comprehensive patient care (Arslan et al., Reference Arslan, Akca and Simsek2014; Sadowska et al., Reference Sadowska, Nowak and Czarkowska-Pączek2020). For this reason, it is important to have tools that allow us to know the attitude of health professionals toward the care of people who are at the end of their lives.
One of the instruments used to assess the attitude of professionals toward end-of-life care is the Frommelt Attitude Toward Care of the Dying Scale (FATCOD). The FATCOD Form A (FATCOD-A) was developed in the United States by Frommelt to assess nurses’ attitudes toward the care of people at the end of life and their families (Murray-Frommelt, Reference Murray-Frommelt1991).
This one-dimensional scale consists of 30 items that evaluate by means of a Likert scale from 1 to 5 (strongly disagree to strongly agree) the nurses’ attitude toward the care of people at the end of their lives and their families. Of these items, 15 are written positively, and the rest are written negatively. The total score varies from 30 to 150 points, with a higher score indicating a better attitude toward care. The validity was determined by the Content Validity Index (CVI), finding an interrater agreement of 0.98 among the experts. To determine reliability, a test–retest was conducted first with 18 nurses from an oncology unit, obtaining a Pearson's correlation coefficient of r = 0.94, and secondly with 30 oncology and surgery nurses with a result of r = 0.90 (Murray-Frommelt, Reference Murray-Frommelt1991).
In order to make the scale applicable to different professionals, the author made modifications, resulting in the FATCOD Form B (FATCOD-B) (Murray-Frommelt, Reference Murray-Frommelt2003). The FATCOD-B was administered to students of nursing, psychology and physiotherapy, among others. The CVI obtained was 1.0, and the Pearson correlation coefficient of the test–retest r = 0.93.
The FATCOD has been validated in different languages and countries, and in professionals from different disciplines. FATCOD-A has been validated in Spain, proving to be a valid instrument for assessing attitudes toward end-of-life care in nursing students (Edo-Gual et al., Reference Edo-Gual, Tomás-Sábado and Gómez-Benito2018). However, there is no evidence to indicate that this version of FATCOD is useful for assessing attitudes in other health professionals.
On the other hand, version B has greater use internationally (Japan, Sweden, Italy, China, Palestine, Poland, Turkey) (Nakai et al., Reference Nakai, Miyashita and Sasahara2006; Leombruni et al., Reference Leombruni, Loera and Miniotti2015; Mastroianni et al., Reference Mastroianni, Piredda and Taboga2015; Wang et al., Reference Wang, Li and Yan2016; Henoch et al., Reference Henoch, Melin-Johansson and Bergh2017; Loera et al., Reference Loera, Molinengo and Miniotti2018; Akbolat et al., Reference Akbolat, Ünal and Karakaya2020; Browall et al., Reference Browall, Pakpour and Melin-Johansson2020; Sadowska et al., Reference Sadowska, Nowak and Czarkowska-Pączek2020). This is possibly due to a greater usefulness of version B as it is applicable to a larger number of professionals.
Therefore, the aim of this study was to carry out the adaptation and validation of the FATCOD-B in Spanish professionals and students of medicine, nursing, psychology, and social work, evaluating the validity of appearance, content and construct, reliability, and feasibility.
Methods
Methodological type and design
An adaptation and scale validation was carried out following the process proposed by Ramada et al. (Reference Ramada-Rodilla, Serra-Pujadas and Delclós-Clanchet2013). This includes the translation, revision by a committee of experts (CE), pilot test, retro-translation and comparison with the original version, and validation of the instrument by checking the psychometric properties that determine reliability, validity, and feasibility.
Phase I: Adaptation
With the author's permission, the original scale was translated from English into Spanish by two independent native Spanish bilingual translators. A summary of the translations was made and sent in two rounds to a CE made up of 12 professionals with a minimum of 5 years’ clinical and/or research experience in palliative care, for the review and evaluation of the semantic equivalence, content and appearance validity, and feasibility of the instruments, using a Likert scale. A minimum level of agreement among experts of 80% was established (García and Suárez, Reference García and Suárez2013). Once the recommendations made by the CE had been consolidated, the preliminary version obtained was back-translated by two bilingual translators and compared with the original version.
The pilot test was carried out with 40 professionals who had similar characteristics to the population under study (Ramada-Rodilla et al., Reference Ramada-Rodilla, Serra-Pujadas and Delclós-Clanchet2013). They were given the Spanish version of the FATCOD-B (FATCOD-B-S), a sociodemographic information question form and another form to write down their observations on the scale. The pilot test served to establish whether the questionnaire could be satisfactorily understood and completed by the professionals and to estimate the time required for its completion. Items that were referred to as difficult to understand by 15% or more of the participants would be modified, refining the final version of the instrument (García and Suárez, Reference García and Suárez2013). However, none of the items met this criterion.
Phase II: Psychometric validation
Setting
The population under study was made up of Spanish physicians, nurses, psychologists, and social workers who are registered in the respective professional associations, as well as students of these qualifications who are enrolled in the final years of their degree at different universities.
Sample
An intentional sampling was carried out, seeking the participation of Spanish physicians, nurses, psychologists, and social workers who are professionally active, registered in professional associations, who practice in Spain, who have 1 year or more of professional experience, whose mother tongue is Spanish and who have email registered in the database of the corresponding professional association; and students in their 5th and 6th year of the degree in medicine and in their 4th year of nursing, psychology, and social work. The data were collected between January 2017 and December 2018.
Instruments and variables
Together with FATCOD-B-S (Annex 2), a sociodemographic information form was used to obtain data such as age, sex, and previous training and experience at the end of life.
Procedure for data collection
The FATCOD-B-S, together with the sociodemographic information form and the informed consent, was entered into a virtual platform (Google-Forms) with free access to administer online questionnaires. The URL of this platform was sent by email to professionals through the professional associations and professors of the grades that provided it to the students.
Data analysis
Descriptive data analysis was carried out using the Statistical Package for the Social Sciences (SPSS) version 22 for Windows. Descriptive statistics were used to characterize the sample.
The validity of appearance and semantic equivalence was determined with the results obtained in the CE review and the pilot test, and the validity of content from the CE's evaluations with the CVI.
Reliability was determined by assessing internal consistency by Cronbach's α for the full scale and for each subscale; and stability by test–retest, re-administering the scale to a group of 37 students one month after they had first done so.
The Mplus version 8 statistical package was used to perform structural equation modeling. This modeling, specifically the exploratory multi-group factor analysis (EMGFA), allowed the simultaneous evaluation of the validity of FATCOD-B-S in four different disciplines: physicians, nurses, psychologists, and social workers. Since only FATCOD-A had been validated in Spanish nursing students (Edo-Gual et al., Reference Edo-Gual, Tomás-Sábado and Gómez-Benito2018), it was decided to adopt an exploratory rather than confirmatory approach. Through the EMGFA, different degrees of invariance between the groups analyzed can be tested (configuration invariance, mild metric invariance, strong metric invariance) (Kline, Reference Kline2016). The fit of each model was evaluated with the Comparative Fit Index (CFI) and Root Mean Square Error of Approximation (RMSEA) coefficients. The critical values used in these cases were: χ 2 significant, IFC > 0.90 (Bentler, Reference Bentler1990), and RMSEA < 0.08 (Browne and Cudeck, Reference Browne, Cudeck, Bollen and Long1993). In order to compare models with different degrees of invariance, the coefficients ΔCFI and ΔRMSEA were used. Values greater than 0.01 in these coefficients indicate that the model fit has worsened, and therefore, the model with the highest degree of invariance cannot be supported (Cheung and Rensvold, Reference Cheung and Rensvold2002). With regard to factorial loads, for all models the value >0.30 suggested by Hair et al. (Reference Hair, Anderson and Tatham2008) was adopted, for sample sizes above 350 observations. Since the sample was composed by both professionals and students of the four aforementioned disciplines, the authors introduced the dedication variable (professionals/students) in the selected EMGFA.
On the other hand, a correlation was performed between the two subscales, and between each subscale and the FATCOD-B-S using Spearman's Rho correlation coefficient.
To determine the feasibility of the scale, the time needed to complete it, the simplicity of the format and the clarity of the items were assessed.
Ethical considerations
This study meets the basic ethical principles for the responsible conduct of research involving people. Informed consent was sought from all participants and the consent of the scale's author, K. Murray Frommelt, was obtained for the adaptation and validation of the scale in the Spanish context. The approval of the Research Ethics Committee of the University of Granada, Spain, was obtained in act n° 270/CEIH/2017.
Results
Table 1 shows the sociodemographic characteristics of the participants. A total of 2,446 people participated in the study, with 1,134 students and 1,312 professionals.
Table 1. Sociodemographic characteristics of the participants (n = 2,446)

Source: Sociodemographic information form completed by Spanish students and health professionals.
Among the students, 82.00% were female and the average age was 22.57 years (SD ± 4.320). Among professionals, 75.70% were women and the average age was 40.24 years (SD ± 12.286). 27.80% had a specialty and 43.30% a postgraduate degree. With respect to previous training in palliative or end-of-life care, 31.70% of students and 52.00% of professionals reported having received training in this area. On the other hand, 20.80% and 57.50% respectively indicated having previous professional and/or personal experience related to the end of life.
Linguistic validation
The process of adaptation of the scale to the Spanish context took place between June and October 2016. Adjustments were made according to the recommendations made by the CE, changing some terms so that they were adapted to the context where the scale was to be used (Supplementary Annex 1). The number of items was not changed.
The changes made it possible to determine the semantic equivalence and content validity (CVI = 0.933). There was agreement that, apparently, the scale measured what was intended (100%). The items were relevant and easy to understand.
Feasibility
The average time required by pilot participants to complete the scale was 5.50 min (SD ± 3.289), which was adequate for 100% of the respondents. Comments made by participants indicated that for 97.50% all items were of interest and easily understood. 97.50% of the participants indicated that the FATCOD-B-S has a simple format.
Construct validity
With regard to the adjustment of the invariance models, it should be noted that χ 2 was not significant in any of the cases. However, this coefficient has been the subject of debate because of its sensitivity to sample size. According to the CFI and RMSEA coefficients, the configuration invariance and mild metric invariance models were successfully fitted to the data. In contrast, the strong metric invariance model obtained a satisfactory fit in only one of the coefficients (RMSEA) (Table 2). Despite this, the comparison between the three models was made. When comparing the configuration invariance model and the mild metric invariance model, no significant worsening was noted. According to this result, the model of mild metric invariance was preferred over the model of configuration invariance.
Table 2. Invariance models

The models of mild and strong metric invariance were then compared. Both coefficients (ΔCFI and ΔRMSEA) showed a worsening of the fit. Therefore, the model with mild metric invariance was finally selected over the other two EMGFA models. Although the model of mild invariance does not allow the comparison of means at the level of constructs or factors as the model of strong metric invariance would do, it is possible to conclude from the model of mild invariance that the different groups of participants in the study have a similar understanding or idea about the factors that are being measured by FATCOD-B-S. Figures 1–4 show the specific results of the mild invariance model for groups of student–professionals in medicine, nursing, psychology, and social work.

Fig. 1. Mild metric invariance physicians’ group.

Fig. 2. Mild metric invariance nurses’ group.
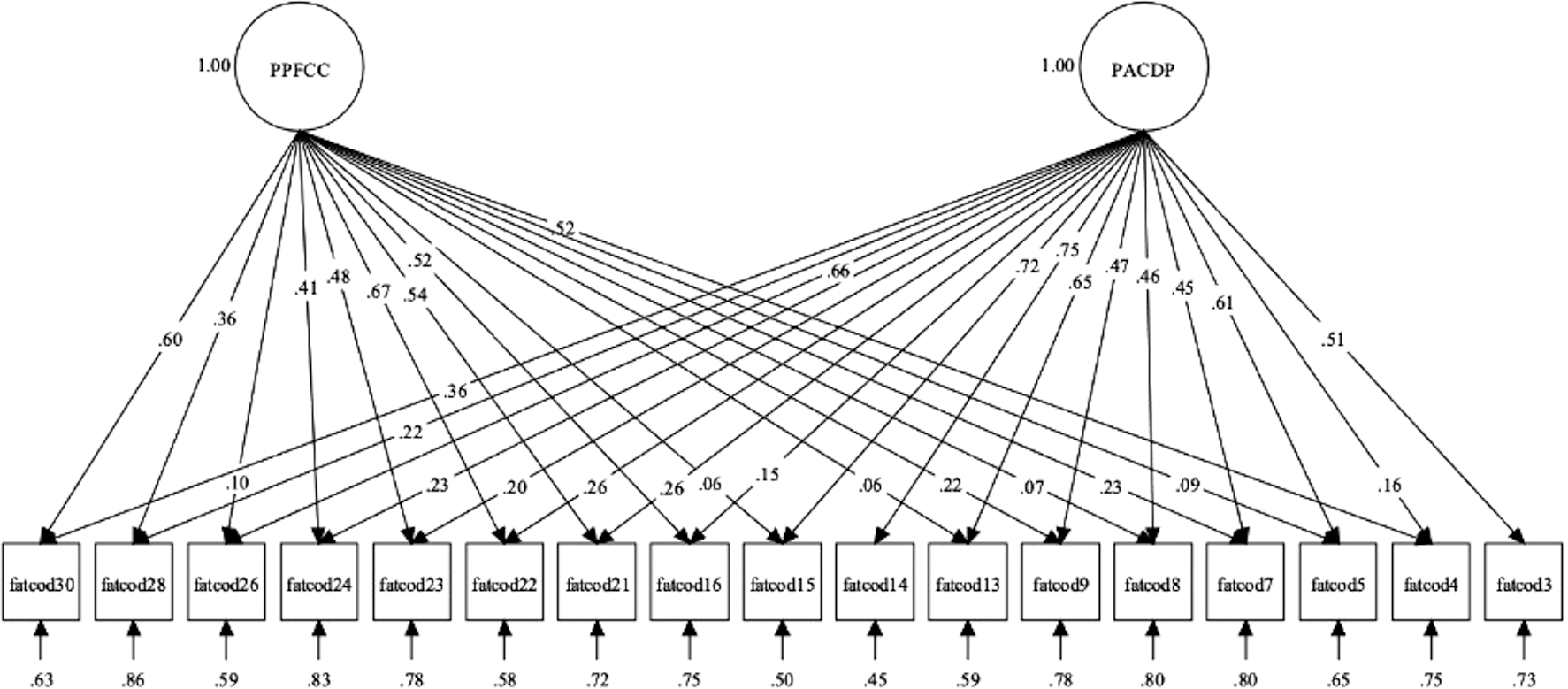
Fig. 3. Mild metric invariance psychologists' group.

Fig. 4. Mild metric invariance social workers’ group.
Seventeen of the 30 items were retained in the model. The remaining items were eliminated because their factorial loads did not reach the limit value or because they had cross-factorial loads. This result is similar to the findings of previous studies (Loera et al., Reference Loera, Molinengo and Miniotti2018).
In the mild invariance model, the nonstandardized factor loads were set equally across all groups. The standardized factor loads are shown in the figures. The acceptance of the mild metric invariance model indicates that the same reagents measure the same constructs in all analyzed groups. The model also suggests that the participants of the different groups interpret the FATCOD-B-S reagents in the same way. Put another way, regardless of which group the participants belong to, the PACDP (Positive Attitudes toward Caring for Dying Patients) and PPFCC (Perceptions of Patient and Family-Centered Care) factors have the same meaning.
When repeating the analyses introducing the dedication variable (professionals/students), it was found that the factor structure and nonstandardized factor loads remain the same in all groups.
On the other hand, a Spearman's Rho correlation coefficient was found between the two subscales (PACDP–PPFCC) of 0.296 (p < 0.001), and between the PACDP subscale and the FATCOD-B-S of 0.909 (p < 0.001), and between the PPFCC subscale and the FATCOD-B-S of 0.641 (p < 0.001).
Reliability
Once the invariance of the instrument was established, Cronbach's α was calculated for each of the factors, taking into account only the items retained. For the PACDP factor, the values were the following: physicians 0.74, nurses 0.79, psychologists 0.82, and social workers 0.76. For the PPFCC factor, the coefficients were as follows: physicians 0.72, nurses 0.70, psychologists 0.70, and social workers 0.66. Cronbach's α for total retained items is 0.79. It should be noted that for exploratory studies, values higher than 0.60 are considered acceptable (Hair et al., Reference Hair, Page and Brunsveld2019). Consequently, the results suggest that the instrument factors are reliable in each of the groups examined in this study. The results of the test–retest showed good results in relation to the stability of the scale (ICC = 0.843, p < 0.001).
Discussion
Palliative care is a field of interdisciplinary practice. The involvement of different health professionals in care of patients at the end of life and their families is essential. It is important that health professionals, not only nurses, demonstrate positive skills and attitudes toward palliative care in order to respond appropriately to patients’ and families’ needs. In Spain, FATCOD-A had only been validated in nurses, which prevented the use of the instrument to assess the attitude toward the care of people at the end of their lives in different health professionals.
The translation of an instrument is a necessary process, but it is not sufficient to guarantee its validity in a different context for which it was designed (Sousa and Rojjanasrirat, Reference Sousa and Rojjanasrirat2011). For this reason, the methodological process for the adaptation and validation of FATCOD-B in the Spanish context was carried out in this study, as a strategy to ensure its validity and reliability. To do so, it is necessary to look for the adaptation of it to the specific conditions of the population to which it is going to be applied.
This scale has been used in different countries, administered to professionals in different areas, validated by different statistical methods, and with different results in relation to the factor structure of the scale. The great variability in the validation results can make us think of possible failures since the original construction of the instrument, making it necessary to revise the items that make it up. However, it is an instrument that since its publication (Murray-Frommelt, Reference Murray-Frommelt1991, Reference Murray-Frommelt2003) has been widely used in different contexts. In this study, the validation of FATCOD-B-S was carried out simultaneously in Spanish physicians, nurses, psychologists, and social workers, and students of these disciplines.
The factorial distribution of FATCOD found in previous studies varies from the one-dimensional distribution reported in the original validation study (Murray-Frommelt, Reference Murray-Frommelt1991, Reference Murray-Frommelt2003) and in the short version validated by Browall et al. (Reference Browall, Pakpour and Melin-Johansson2020) up to a maximum of 7 factors found in the Chinese version (Wang et al., Reference Wang, Li and Yan2016). Most studies found a two-dimensional structure (Nakai et al., Reference Nakai, Miyashita and Sasahara2006; Leombruni et al., Reference Leombruni, Loera and Miniotti2015; Edo-Gual et al., Reference Edo-Gual, Tomás-Sábado and Gómez-Benito2018; Loera et al., Reference Loera, Molinengo and Miniotti2018; Sadowska et al., Reference Sadowska, Nowak and Czarkowska-Pączek2020). However, the distribution of items in the factors and the number of items retained vary. The distribution of items obtained in this study, although with a lower number of items retained, is very similar to that found by other authors (Nakai et al., Reference Nakai, Miyashita and Sasahara2006; Leombruni et al., Reference Leombruni, Loera and Miniotti2015; Edo-Gual et al., Reference Edo-Gual, Tomás-Sábado and Gómez-Benito2018; Loera et al., Reference Loera, Molinengo and Miniotti2018; Sadowska et al., Reference Sadowska, Nowak and Czarkowska-Pączek2020).
The data analysis technique used in this study allows the inclusion of measurement errors in the validation model. It is a technique that involves greater constraints than traditional factor analyses, and even more demanding than the principal component analysis used by Edo-Gual et al. (Reference Edo-Gual, Tomás-Sábado and Gómez-Benito2018) to analyze the data provided by a sample of Spanish nursing students. The major restrictions of the technique used in this study, the restriction to equality of the number of factors and nonstandardized factor loads, plus the inclusion of residual variances, may explain the reduction with respect to the original number of items in the FATCOD-B. However, if comparisons between health professionals are to be made using this instrument, only reagents subjected to multi-group analysis such as those used in this study should be used for this purpose. In this sense, although a greater quantity of reagents was eliminated through the analyses reported in this study, the value of these results is to suggest that only those items of the FATCOD-B-S should be used to make comparisons between physicians, nurses, psychologists, and social workers. It is also important to point out that it is not convenient to use a validated instrument in nurses to make measurements in other types of professionals. With the validation made in this study, the interested parties can use the extracted items to make measurements in the groups examined here.
The scale has proven to be a reliable tool for assessing health professionals’ attitudes to end-of-life care, with a Cronbach α ranging from 0.74 to 0.82 for different professionals in the PACDP subscale and from 0.66 to 0.72 in the PPFCC subscale. In the previous studies, the lowest values in reliability were those reported by Mastroiani in the validation of the scale with Italian nursing students, where they found 6 factors with a Cronbach α between 0.47 and 0.69 (Mastroianni et al., Reference Mastroianni, Piredda and Taboga2015) and the highest found in the short version of the scale, one-dimensional, validated in Sweden with nurses, with a 0.87 Cronbach α (Browall et al., Reference Browall, Pakpour and Melin-Johansson2020).
The basic palliative care teams are made up of physicians and nurses, with the support of psychologists and social workers (Ministry of Health, 2011). Although FATCOD has been used with physicians and nurses from different countries, no reports have been found in the literature of its use with psychologists and social workers. It is considered important to have an instrument that allows us to know the attitudes of these professionals since they are all directly involved with the care of patients at the end of life and their families. This study allows us to have a validated instrument to evaluate the attitude of health professionals, which will allow, on the one hand, to select the professionals who have the best attitude toward the care of people who are at the end of their lives in order to carry out their care work in these areas, and on the other hand, to implement the necessary actions to improve the attitude of the professionals, which is related to an improvement in the quality of care (Ascencio et al., Reference Ascencio, Allende and Verastegui2014; Jiang et al., Reference Jiang, Lu and Ying2019) and a decrease in the negative side effects of this care on professionals (Agusti et al., Reference Agusti, Esquerda and Amorós2018; Bermejo et al., Reference Bermejo, Villacieros and Hassoun2018; Dimoula et al., Reference Dimoula, Kotronoulas and Katsaragakis2019).
Limitations
The selection of the sample was intentional. However, the sample size is larger than that used in previous studies. However, results may vary when using another sample selection method, so results obtained in other studies will need to be confirmed.
The FATCOD-B-S was administered virtually. Although the response format has not been modified, it is unknown whether there may be differences with respect to paper administration.
Conclusion
The linguistic and psychometric validation of FATCOD-B-S in Spanish physicians, nurses, psychologists, and social workers provides a valid instrument for determining attitudes toward the care of people at the end of their lives. The number of items in FATCOD-B-S is lower than in the original version. However, the results show that only these items should be used to make comparisons between health professionals in the different disciplines where it has been validated.
FATCOD-B-S demonstrates its validity of appearance, since the items, in appearance, measure what they are proposed to; and it also demonstrates its validity of content, since the content of each item is relevant in the context in which it is intended to be applied and the aspects which are relevant to the construction of attitudes toward the care of people at the end of their lives are included in it. The scale has proven to be useful in relation to the time required and the ease of completion of the format.
The Spanish version of the scale is made up of two subscales in the four professional groups: “Positive attitudes toward caring for dying patients” and “Perceptions of patient and family-centered care,” and a high internal consistency index is obtained that demonstrates the validity and reliability of the instrument.
Being able to know the attitudes of physicians, nurses, psychologists, and social workers toward the care of people who are at the end of their lives will make it possible to implement the necessary actions to improve the attitude of the professionals, which is related to an improvement in the quality of care and a reduction in the negative side effects of this care on the professionals.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951521001504.
Acknowledgments
The authors would like to thank K. Murray Frommelt for her support throughout the process as well as the study participants and members of the expert committee: Adoración Muñoz, Ana Carvajal, Claudio Calvo, Francisco Moltó, Isabel Ródenas, M. Carmen Ortega, M. José Cabañero, Marisa Velasco, Moisés Leyva, Rafael Gómez, Susan Hannam, and Victoria Espinar.
Funding
The present study has been supported by the Spanish Ministry of Education through a University Faculty Training contract granted to R.H.H. (FPU15/02487).
Conflict of interests
The authors declare that there is no conflict of interest.








