Introduction
Stroke is one of the leading causes of disability worldwide (Hebblethwaite & Curley, Reference Hebblethwaite and Curley2015; ‘Stroke in Canada’, n.d.). The sequelae of stroke include motor, sensory, cognitive, visual and communication impairments and can include subsequent mental health impacts such as depression (Lincoln et al., Reference Lincoln, Brinkmann, Cunningham, Dejaeger, de Weerdt, Jenni and De Wit2013; Schöttke & Giabbiconi, Reference Schöttke and Giabbiconi2015). Individuals with stroke may find their ability to participate in meaningful social and leisure activities is hindered due to physical and institutional barriers impacting their community reintegration (Della Vecchia et al., Reference Della Vecchia, Viprey, Haesebaert, Termoz, Giroudon, Dima and Schott2021). For example, an individual with stroke may not be able to participate in a personally meaningful activity such as gardening due to hemiparesis (physical barrier) or no accessible garden spaces, such as raised garden beds (institutional barrier). Rehabilitation programs aim to improve physical and cognitive impairments in order to overcome limitations that may impede community reintegration. Rehabilitation programs may also provide a space for peer-support interactions aimed at addressing activity limitations experienced post-stroke (Clark et al., Reference Clark, MacCrosain, Ward and Jones2020; McKellar et al., Reference McKellar, Cheung, Huijbregts and Cameron2015).
Peer-support involves one individual with lived experience supporting someone else with the same or similar condition (Mead et al., Reference Mead, Hilton and Curtis2001; Shalaby & Agyapong, Reference Shalaby and Agyapong2020). Peer-support programs: (1) utilize the expertise of people with lived experience, (2) integrate peers in health delivery, and (3) focus on patient-directed care (White et al., Reference White, Foster, Marks, Morshead, Goldsmith, Barlow and Gillard2020). Peer-support programs may play an important role in supporting community reintegration post-stroke in an outpatient setting as they promote interpersonal connections from their mutual experiences, which then enables problem solving and increased function (Levy et al., Reference Levy, Luong, Perrier, Bayley and Munce2019; Wijekoon et al., Reference Wijekoon, Wilson, Gowan, Ferreira, Phadke, Udler and Bontempo2020).
Peer-support improves health outcomes such as resiliency and self-efficacy in people with other neurological injuries, spinal cord injury (Barclay & Hilton, Reference Barclay and Hilton2019), mental health issues (Eddie et al., Reference Eddie, Hoffman, Vilsaint, Abry, Bergman, Hoeppner and Kelly2019; White et al., Reference White, Foster, Marks, Morshead, Goldsmith, Barlow and Gillard2020), and diabetes (Houlihan et al., Reference Houlihan, Brody, Everhart-Skeels, Pernigotti, Burnett, Zazula and Jette2017). Peer-support programs offer individualized interventions targeted to the participants’ specific needs and abilities, and can be tailored to specific outcomes (e.g., self-efficacy of diabetes management, wheelchair skills after spinal cord injury). Specific to stroke research, peer-support groups have been found to be beneficial in improving participation and reducing caregiver burden (Christensen et al., Reference Christensen, Golden and Gesell2019; Rotherham et al., Reference Rotherham, Howe and Tillard2015). Moreover, for people with aphasia after stroke, peer-support in the community can improve quality of life and reduce social isolation (Lanyon et al., Reference Lanyon, Worrall and Rose2018; Rotherham et al., Reference Rotherham, Howe and Tillard2015). In particular, a scoping review of 177 studies reported that traditional clinician-led models of aphasia group delivery are limited in scope, whereas peer-led community aphasia groups have an important role in supporting well-being for individuals with chronic aphasia after stroke (Pettigrove et al., Reference Pettigrove, Lanyon, Attard, Vuong and Rose2021).
Peer-support can facilitate development and participation in social roles through the conversation and relationship. Peer-support programs are often conducted in a group setting, but also can be provided as one-to-one support. Peer-support can be related to peer-befriending, as it facilitates connection, shared experience, and belonging, with peer-befriending always involving a one-to-one connection (Hilari et al., Reference Hilari, Behn, James, Northcott, Marshall, Thomas and Goldsmith2021). Peer-befriending can reduce distress and depression in those receiving the support, and has high acceptability from both people providing and receiving support (Hilari et al., Reference Hilari, Behn, James, Northcott, Marshall, Thomas and Goldsmith2021).
Most peer-support programs have oversight and management by healthcare professionals or trained volunteers who do not have the same lived experience as those people attending the group (Sadler et al., Reference Sadler, Sarre, Tinker, Bhalla and McKevitt2017; Wijekoon et al., Reference Wijekoon, Wilson, Gowan, Ferreira, Phadke, Udler and Bontempo2020). These programs often incorporate a coupled peer and professional-led approach, where professionals work with individuals with lived experience to provide peer-support interventions (Kessler et al., Reference Kessler, Egan and Kubina2014; Wijekoon et al., Reference Wijekoon, Wilson, Gowan, Ferreira, Phadke, Udler and Bontempo2020). Preliminary evidence from a peer-led brain injury group found it improved social communication better than a staff-led intervention (Howell et al., Reference Howell, Beeke, Pring and Varley2021). However, there is limited research that explores peer-led, peer-support groups for stroke survivors that did not involve a healthcare professional or other outside group.
Building Life After Stroke Together (BLAST) is a community-based, peer-led, peer-support group in Vancouver, British Columbia for individuals who have experienced one or more strokes. There is no healthcare staffing, infrastructure, or healthcare funding supporting the group. The purpose of this group is to form interconnections with people who have similar lived experiences. The BLAST group was founded by a person with stroke who experienced an unmet need in the community, to manage their health and well-being. The founder of BLAST sought to find a space that would accommodate multiple people with varied types and levels of disability for low or no cost. Upon finding a community center, and later a non-profit-housing common area that were available at no cost, the BLAST group commenced. Members of BLAST were informed of the group through word of mouth from the founder, social media, and recommendation from healthcare professionals aware of the group. All members of BLAST collaboratively contribute to the weekly group’s plans and schedule (e.g., deciding on topics for discussion or activities), as well as the activities conducted in the group (e.g., making a meal for the group or facilitating exercises).
The BLAST group meets weekly with the size of group ranging from 8-20 attendees. The BLAST group also organizes an annual weekend camp at an accessible location to facilitate attendance from all participants with any type of disability. The weekly group and camp both focus on social participation through providing a ’safe, accepting, and stress-free environment’ (D Chow, personal communication, May 15, 2020). It is intended for individuals who have experienced a stroke to access leisure activities once other rehabilitation programs have ceased; for example, after discharge from an outpatient stroke program.
The purpose of this study was to explore stroke survivors’ experience of attending a community peer-led, peer-support group. Furthermore, the research examined why individuals choose to participate in the group, the key elements and strengths of the group, and possible areas for improvement.
Materials and methods
Study design
This study used a qualitative description approach with a relativist ontology and a constructivist epistemology (Sandelowski, Reference Sandelowski2000, Reference Sandelowski2010), supplemented by demographic data collected via an online survey, with analysis informed by a constructivist grounded theory (Charmaz, Reference Charmaz2003). Qualitative findings were reported using COnsolidated REporting guidelines for Qualitative studies (Tong et al., Reference Tong, Sainsbury and Craig2007) (see supplemental material). Ethics approval was obtained through the Behaviour Research Ethics Board at the University of British Columbia.
Participants
To be included in the study participants needed to: 1) be members of the peer-led, peer-support group, 2) be adults over 19 years old (legal age of consent in British Columbia, Canada), 3) have the ability to provide informed consent, 4) be able to communicate in English, and 5) have experienced one or more strokes. Convenience sampling was used to recruit participants with criteria of having attended the BLAST group and annual weekend camp.
Recruitment
The research team introduced the study to the group via an initial letter of invitation outlining the purpose of the study, which was distributed by the community research partner (third author). Interested members contacted the first and second authors to participate in the study. Participants were offered a $15.00 honorarium (Canadian dollars) for their participation in this study.
Data collection
All data were collected virtually to abide by the provincial COVID-19 guidelines set out by the British Columbia Ministry of Health. The first and second authors conducted semi-structured individual interviews, between October 2020 and February 2021. The interviews were completed on the phone or through an online platform (Zoom) with a planned duration under 60 min. All interviews were only audio recorded. Although there are disadvantages to undertaking online interviews among people with brain injuries (Topping et al., Reference Topping, Douglas and Winkler2021), our study considered the recommendations from previous literature and patient-partners involved in the design of our study to ensure an ethical and practical delivery of the interview.
The interview guide was initially developed using knowledge from past literature on peer-support after stroke (Hughes et al., Reference Hughes, Fleming and Henshall2020) and recommendations from literature on interviewing people with brain injury (Paterson & Scott-Findlay, Reference Paterson and Scott-Findlay2002). The interview guide was further developed with input from key stakeholders (people with lived experience, researchers, clinicians) reviewing the list of questions and discussing the questions with all authors. The interview questions were pilot tested with people with lived experience, then modified in regards to the length and specificity of questions. For participants with aphasia, interviewers provided increased length of time for responses, encouraged use of technology to support communication (e.g., type-to-voice communication, typing responses), and encouraged use of onsite support people if available (e.g., friends or family). Questions asked about participants’ experiences in the group, including, ‘Why did you join the group?’ and ‘What has been your experience post-stroke?’ or ‘How, if at all, has attending the group affected your life after stroke?’ During the interview, questions were adapted based on the previous responses of the participant. The participants completed a brief online survey prior to the semi-structured interview that collected demographic information such as age, current side effects of their stroke, and years of education.
The first two authors conducted the interviews, one facilitated the questions while the other took notes and helped provide follow-up questions. Both authors are female and had previous experience interacting with people with brain injury. Both were enrolled in clinical allied health graduate school (Occupational Therapy) at the University of British Columbia, Canada and received specific training on interviewing people with stroke. The third author was not involved in the interview process; the fourth and fifth authors were involved in the interviews as mentors. The fourth author is male with over 30 years of combined clinical and research experience related to neurological rehabilitation. The fifth author is female with over 15 years combined clinical and research experience in brain injury rehabilitation research. Participants were informed and aware of the interviewer’s backgrounds, as well as the goals of this research project. There were no relationships established between the participants and the authors without lived experience of stroke, prior to this study. Data collection was completed when a sufficient depth of understanding was reached to develop an explanatory model (theoretical sufficiency) (Dey, Reference Dey1999).
Data analysis
Data analysis occurred concurrently with data collection. A self-administered survey was used to obtain demographic information for the eleven participants. Interviews were transcribed verbatim and survey answers were exported from Qualtrics to an Excel file by the first two authors. All proper nouns (participant’s name, names of other people and/or landmarks, etc.) were replaced with pseudonyms during transcription to ensure confidentiality. Analysis of the qualitative data was ongoing and informed by constructivist grounded theory (Charmaz, Reference Charmaz2003). During the coding process, the first and second authors independently coded three interviews to create initial codes through line-by-line coding using active terms (Charmaz, Reference Charmaz2003). The first two authors then collaboratively created focused codes that were used to build a preliminary coding guide with input from the fourth and fifth authors. The first two authors then applied the coding guide to all interviews. Re-evaluation of the coding guide was ongoing, and the data were re-coded as needed to ensure cohesion. During the coding process, the first two authors engaged in memo writing to guide category creation. The first, second, fourth, and fifth authors met as a group to discuss the categories and created concepts that were developed into an explanatory model, using constant comparison and reflection. The third author was not involved in the data analysis process given her membership with the study group.
Three trustworthiness strategies were employed (Morrow, Reference Morrow2005): reflexivity about their positioning and perceived influence on the research process, triangulation of researchers, and member checking. In terms of positioning, the research team consisted of clinical graduate students enrolled in clinical allied health graduate school (Occupational Therapy) (first and second authors), research supervisors with extensive qualitative research experience (authors four and five), and a community research partner with lived experiences of stroke (author three) who was a member of the BLAST group. Interviewers reflected on their identities and their positionality, as well as their biases and beliefs through documenting how they anticipated participants would answer the interview questions which informed probing questions for subsequent interviews to obtain more in-depth data. Complementary triangulation of researchers occurred as the first and second authors were present for the interviews and data analysis occurred as a research team. Lastly, the researchers completed member checking by distributing a poster and video recording, with input from the group founder, to the participants that summarized the preliminary results. Participants were invited to provide feedback to the researchers as a means of knowledge dissemination and an additional opportunity for data collection. All ten of the participants who responded indicated that the summarized findings reflected their experiences. Although no new data or perspectives emerged, the additional feedback was used to further inform the language used within the results section of this study.
Findings
There were 11 participants included in our study (Table 1), from 18 that were invited to participate; no one was excluded after inquiring about participation. The average age of the participants was 65–69 years old (range from 41 to 83 years), and the average time since participants’ first stroke was between 15 and 19 years (range from 3 to 31 years). Ages are presented in range to limit identification of participants. More than half of the participants were female. Four of the participants experienced some expressive aphasia but were able to communicate through technological or with the assistance from caregivers or technology. Interviews lasted between 30 and 60 min.
Table 1. Participant demographics

The analysis identified three themes and six subthemes. The first theme Meeting unmet needs after stroke outlined how the group was created by stroke survivors to address feelings of loss through a self-sufficient group that gives back to their community. The second theme Buddies helping buddies highlighted that stroke recovery was a shared process within the group, where members encouraged each other to contribute what they could. The last theme Creating authentic friendships revealed that the group experienced camaraderie within their shared experience and enjoyed spending time together. Together, these themes described what the group offered as a peer-led, peer-support group. When describing individual participants in the results that follow, pseudonyms were used, and participants’ ages were rounded to the nearest multiple of five to help protect their anonymity.
Explanatory model
The explanatory model (Fig. 1) illustrates the nested themes in this study. At its core, the group involves authentic friendships and camaraderie stemming from shared life experiences. Participants described connecting and helping each other with different activities, while providing insight into recovery. Together, the first two themes provided the foundation that met stroke survivors’ needs after stroke by being a space where group members could be independent and give back to their own community. Overall, this model speaks to how a peer-led, peer-support group may support people after stroke.
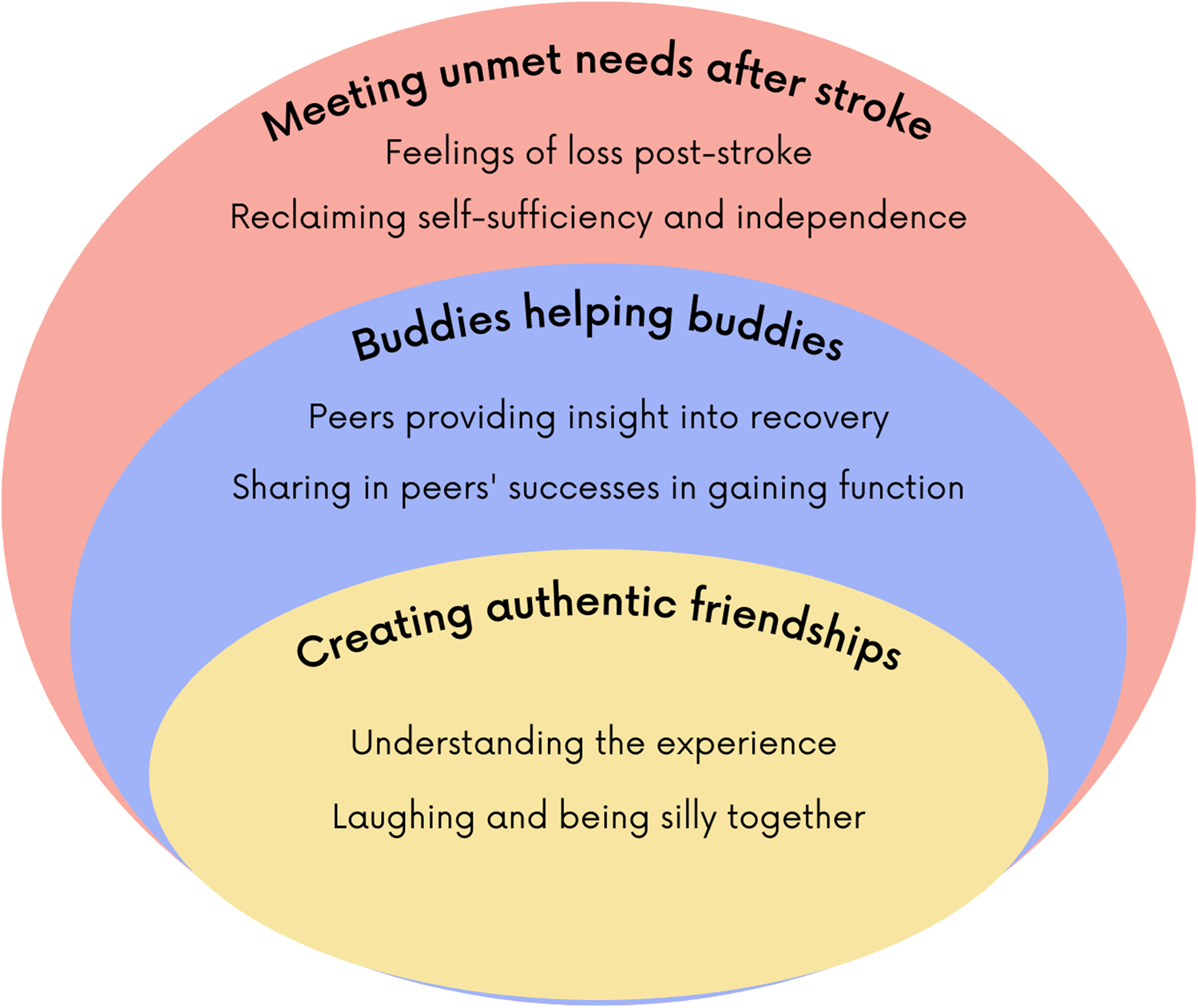
Figure 1. Explanatory model.
Theme 1: Meeting unmet needs after stroke
The first theme incorporated two subthemes that explored how participants in the group felt that the peer-led, peer-support group addressed unmet needs after stroke. Subthemes described changes to peoples’ lives after experiencing a stroke and how the group was a space for participants to be independent through their group contributions.
Feelings of loss post-stroke
The first subtheme is temporal as the participants told stories from their first experiences post-stroke. Following acute treatments and rehabilitation interventions, four participants described they were unprepared to adjust to life at home post-stroke. Sylvia (age 75) emphasized that after a stroke, ‘you’re not sure of yourself, you lose everything you have, your confidence’. Sylvia went on to share that she was told by a medical professional that her progress would plateau after two years of rehabilitation. They stated, ‘oh in two years that’s the end of it you won’t get any better…But it took me seven years to feel the way I do, so you can still feel better’. When Sylvia was asked how the medical professional’s prognosis impacted her, she stated, ‘I guess it made me push more or harder to think I am going to get through this. It wasn’t very nice, I thought oh god that this is the end of my life. In fact, I really wanted to die’. All eleven participants expressed similar stories of loss when they reflected on their experience post-stroke.
For many of the participants, decreased confidence in their personal abilities was identified as a reason for avoiding going out into the community. Six participants were hesitant to leave their homes due to vision loss and fear of other people knocking them over. Mary (age 70) recounted, ’Sometimes I feel very frustrated because before I could move around very easily without any problem. Now I am afraid that if I go out, somebody will knock me down without noticing’. Theresa (age 60) reflected on how the lack of confidence to leave her home contributed to feelings of isolation. She disclosed that she had difficulty keeping in contact with previous friends and that her neighbors did not know her because she rarely left the house. All participants detailed similar stories about changes to their social roles and participation in life after their stroke. The participants indicated that BLAST provided a safe opportunity for social engagement and connection to a wider community of people with similar experiences. In this way, feelings of loss of social participation were understood and, in part, addressed by the social experiences and friendships formed within BLAST.
Reclaiming self-sufficiency and independence
The group provided participants the opportunity to find a renewed sense of independence and restore their self-confidence. None of the participants returned to their previous employment and the group was an opportunity for members to use skills from previous employment to benefit the group in a purposeful manner. Michael (age 40) reflected on his role within the group and explained ‘I have a certificate as a healthcare assistant […] I can help them with mobility or whatever they need. So that comes in handy. I guess that’s my role and I enjoy doing it!’ Betty (age 85) offered the following narrative about the separation of the BLAST group to typical healthcare services and professionals:
It is totally volunteer run […] It really stretches your own confidence to say that you can do things. You don’t have to rely on somebody else to do them. It’s a very shared desire to provide this kind of service amongst ourselves. […] Holly took on the banking, depositing of payments that came in and cheques that had to be written. Grace is really the CEO, and everyone else contributes what they can.
Seven other members of the group recounted similar stories where the group provided the opportunity to build confidence through being a self-run organization and helping others within the group. Sylvia described what she thought about the group: ‘It really helps a lot to know that you are useful. You don’t lose everything’.
Although eight of the group members liked that the group was a space to be independent, when asked ‘How could the group improve?’, one member reported that the group would benefit from volunteers to help set-up (moving tables and chairs) and another member expressed it would be beneficial to have healthcare professionals provide guest presentations. In contrast to many of the members’ sentiments regarding the group’s independence, Betty shared her concern about what would happen if the group founder experienced any health concerns:
I know that Grace is the shaker and mover. She has had a few health concerns recently and I would be concerned if she was unable to continue in that role. I just don’t know if she has a team in place that could do what she does.
Although many of the participants praised the independence they experienced in the group, it was recognized by one of the members that if something happened to the group founder, there may not be a plan in place for someone else to take on their role.
Theme 2: Buddies helping buddies
The second theme included two subthemes that explored how group members helped each other, told their stories about recovery, and showcased peers’ successes.
Peers providing insight into recovery
The first subtheme described the ways that peers benefited both from telling their story and from hearing other peers’ recovery stories. Michael shared, ‘basically [the group] is buddies helping buddies, we just have a good time and heal while helping each other’. Eight group members recounted that they had experienced functional gains more than two years post-stroke, despite being told that most recovery happens in the first six to twenty-four months. The continued recovery they experienced is something they liked to share with newcomers to the group. David (age 70) reflected on his own journey post-stroke and stated: ‘I think of the hardships I went through, I want to help stroke survivors, so that they can see that there is life after stroke’. Seven members responded that they enjoyed telling their recovery story and hearing others’. Different activities throughout the group provided this opportunity as described by James (age 75):
We’ll do what we call a ‘Go Around’, where each person will revisit their journey. It is beneficial for new people coming in to hear somebody else’s story and their progression. I often throw out to people that my stroke was nine years ago, and I am still making improvements. […] There is still the odd person that reads somewhere or is told that that you will only really get better for the next six months […]. And that’s baloney! […] [At the group], they get to hear from people who have had a stroke that it’s not a sprint, it’s a marathon, but you will get better. […] If you have difficulty doing it now, try it again in six months and see how it feels.
Mary, a new member of the group who was three years post-stroke, stated that she enjoyed hearing other members’ perspectives on life post-stroke.
I like people to share with me […] I was quite depressed […] I get frustrated that I have not been able to use my right hand. They told me ‘don’t get frustrated, it might take one or two weeks, it might take a few years […] there is always hope and don’t give up.’
For Mary, one reason she continued to attend the group was to speak with group members like James who shared their experience and perspectives of stroke.
Sharing in peers’ successes in gaining function
The second subtheme highlighted how members celebrated each other’s accomplishments. Michael indicated that they all participated in other members’ successes due to their own personal contributions to the group. Lorraine (65 years) mentioned a story about how Theresa and Robert (age 70) helped each other dance at a weekly lunch:
When Robert first came to BLAST, he didn’t do anything. He’d eat a lot, just sit there and go home when it was over. Theresa has this thing with dancing. Theresa gets him up to dance. […] He has a hard time walking too, so they are both holding each other up. The smile on his face was ear to ear. He has slowly come out of his shell. Which is an amazing thing for all of us to watch! Now he goes there early, sets up all the tables, and makes the coffee. It’s amazing! I think everybody in the group has had an experience like that.
At the group, activities for each meeting are chosen by the members based on their interests and there was no formal structure to the sessions. Michael identified that the flexibility of each meeting allowed for members to do what they wanted without being rushed by a formal schedule. Occasionally, some members would try a new activity that the other group members had not realized they were able to do. Betty described a time when she witnessed a peer with aphasia showcase an unknown skill:
When I first met [David…], he could not speak other than single words, [but] he could sing. It was amazing, nobody even thought of that. He got up and actually sang at a mic. It wasn’t professional but it was a great pleasure because we learned that he could do that.
Eight other members disclosed similar stories about their peers’ successes in different activities in the group, all centered around improved function or new activities they watched another member try.
Theme 3: Creating authentic friendships
In the last theme, there are two subthemes that described how group participants developed authentic friendships and camaraderie as they shared experience of stroke and were able to laugh and have fun together.
Understanding and sharing the experience of stroke
Participants described the atmosphere of the group as welcoming and a place where they could be both understood and understanding of one another. Participants indicated the importance of the friendships made in the group as many members had lost previous friendships because of their stroke. All ten of the other participants provided similar descriptions about the group having a friendly atmosphere. Mary emphasized ‘you can really connect with them [group members] because they are nice people. […] You won’t feel that you are new’.
The group participants indicated that the comfort experienced amongst group members was because everyone had experienced a stroke. Specifically, six participants mentioned that they were comfortable participating in activities even if they looked silly because all members understood the experience of stroke. Specifically, Betty outlined:
I think it is confidence building. You’re not afraid to try things and looking stupid. It’s because everybody else is struggling too, so you build confidence in that respect. Then you go back to your home territory and try to find ways to expand that confidence.
Participants described their enjoyment in being able to try activities without concerns about being judged by others regarding their disability(ies). Laura (age 79) described a memorable experience:
Play[ing] games together. It is really stimulating to do that with somebody who is at the same level of function as you are, because if I were to play scrabble with a normal person, it would drive them crazy because I would be doing 2, 3, 4, letter words and they would want to be more challenged.
By taking part in activities with other people who have had the same experience, members described acceptance to be themselves.
Conversely, there was one negative case. One participant reported that she did not enjoy playing the games with other members of the group. Mary explained that because everyone had different issues, there were different reaction times while playing games:
So, you’ll be bored if you sit there, when you are much better than others, and have to wait for them to be ready. I am not the person that has the patience to wait too long. I don’t find that interesting.
However, she did acknowledge that she found value in talking with the members during and after the games which is why she continued to attend the group.
Laughing and being silly together
Participants highlighted that the friendships they developed in the group were formed through acceptance of one’s self and others; this facilitated the group member’s ability to have fun together. When Grace responded to a question that asked what she liked about the group, she exclaimed:
They are fun! They are relaxed! Stress-free! They are accepting! We are accepting of all our little issues. There are a few people who are crabby, but they get off it and come back. And we can laugh at each other. I think that there is more laughter in our group than any other group.
Laura described that at the group, ‘it is amazing camaraderie. Just amazing. I think that is the number one thing about it’. Mary spoke of her continued attendance and attributed it to the welcoming atmosphere built by friendships: ‘They treat you like their friends right away […]. Right away, you know that you are welcome with this group of people and that is why I joined them’. Betty emphasized the social benefits of meeting with one another, ‘It’s a social opportunity to get together. It’s like a family reunion, we are not strangers from different places’. All members described the group as being more than a peer-support group for people who have had a stroke. Four participants reported that they liked having access to a group of friends to connect with over Facebook, Zoom, email, or the phone.
Discussion
This study explored the experiences of stroke survivors attending a peer-led, peer-support group and identified that stroke survivors in the community experience unmet needs, enjoy having a space to be independent, and create authentic and permanent friendships while having a good time. The discussion is organized by the three themes.
Participants in this study described both the physical bodily experience of disability and the social constructs that cause barriers and how they interconnect, similar to the social-relational model of disability (Cologon, Reference Cologon2016). The social-relational model of disability postulates that disability includes both the lived experience of an individual’s body and its relationship with the social environment and barriers experienced (Cologon, Reference Cologon2016). Findings from this study are consistent with this theory as participants described how they navigated socially imposed barriers and sought out opportunities in their community to increase social connections, which led them to the group. Participants’ view on life after stroke provided opportunities where members explored their potential without social pressures while still acknowledging their corporeal limitations. This study found that the group was a space where participants were self-sufficient without concerns of external constraints as reflected in Betty’s anecdote regarding their ability to independently facilitate the group.
Although many of the participants praised the independence they experienced in the group, it was recognized by one of the members that if the group’s founder was no longer engaged in the group, there may not be a plan in place for someone else to take on their role. There are potential sustainability issues in peer-led peer-support groups that may be more pronounced than in institutionally led peer-support programs. Findings from our study extend earlier knowledge of sustainability in peer-led groups identifying the barrier of limited permanence in leadership roles (Howell et al., Reference Howell, Beeke, Pring and Varley2021). However, the limitation of groups or programs initiated and led by health service institutions is the potential to lack an independence and self-sufficiency as experienced in this study. Findings from this study indicate an added benefit of the peer-led component of the group, which expands knowledge from previous work on traditional peer-support groups. It is possible that a collaborative, co-development approach may guide the formation and implementation of peer-support programs to engage key stakeholders and facilitate the similar unique benefits as described in this study (Dams-O’Connor et al., Reference Dams-O’Connor, Landau, Hoffman and St De Lore2018; Jull et al., Reference Jull, Giles and Graham2017).
Our second theme described the strengths of a community-based peer-led, peer-support group for stroke survivors and was agreeable with social identity theory. Social identity theory describes how an individual’s social identity helps to guide how they view their behavior, actions, values, interactions, and goal setting abilities (Haslam, Reference Haslam2014). The welcoming environment of the group fostered a strength-based approach where members were encouraged to contribute during activities, learn from one another, and explore their abilities. Secondly, social identity theory postulates that social identities are not well supported by external sources (Dennis, Reference Dennis2003), such as a paid volunteer or a healthcare professional, as seen in other stroke support groups (Sadler et al., Reference Sadler, Sarre, Tinker, Bhalla and McKevitt2017; Wijekoon et al., Reference Wijekoon, Wilson, Gowan, Ferreira, Phadke, Udler and Bontempo2020). In our study, peers guided the group’s behavior through cultivating a safe environment, sharing recovery stories, and celebrating peers’ successes, which is similar to previous studies on peer-support (Della Vecchia et al., Reference Della Vecchia, Viprey, Haesebaert, Termoz, Giroudon, Dima and Schott2021; Jellema et al., Reference Jellema, van Hees, Zajec, van der Sande, Nijhuis-Van Der Sanden and Steultjens2017; Northcott et al., Reference Northcott, Moss, Harrison and Hilari2016). Similarly, in study describing the co-design of a peer-led coaching intervention, preliminary findings from the intervention testing showed supportive re-engagement in social participation and benefits to one’s life quality (Masterson-Algar et al., Reference Masterson-Algar, Williams, Burton, Arthur, Hoare, Morrison and Elghenzai2020). As such, peer-led, peer-support groups, such as BLAST, may be as beneficial as current community-based programs for stroke survivors.
The third theme, Creating authentic friendships, described how all participants valued the relationships and social connection of the peer-led, peer-support group. This theme aligns to previous research on befriending after stroke, which indicates that people with stroke can experience well-being, self-acceptance, and improved quality of life from friendships (Hilari et al., Reference Hilari, Behn, James, Northcott, Marshall, Thomas and Goldsmith2021).
In the subtheme, Laughing and being silly together, participants experienced playfulness, which is a concept where activities are approached with an openness grounded in creativity and curiosity, which allows for capacities to be explored and unsuccessful attempts to be re-framed as learning opportunities (Guitard et al., Reference Guitard, Ferland and Dutil2005). Additional positive outcomes of playfulness identified in stroke rehabilitation is the contribution to motivation and positive impact on mood and engagement in activities (Pallesen et al., Reference Pallesen, Andersen, Hansen, Lundquist and Brunner2018). In this study, playfulness was a key element of the group and was experienced when members encouraged peers to be open-minded, try their best, and laugh during activities knowing the experience is shared. The findings add to the existing peer-support group literature by illustrating how playfulness and fun may foster engagement in activities leading to greater group participation amongst stroke survivors.
This study had two main limitations. First, our study was completed during the COVID-19 pandemic; therefore, the interviews were completed virtually, which may have been a barrier for potential participants. By potentially excluding participants who were not comfortable or did not have access to the Internet and necessary technology (e.g., smartphones or computers), there may have been decreased participation in the study. Additionally, given the prevalence of cognitive communication issues in people with brain injury, there may have been reduced understanding and engagement during virtual interviews (Topping et al., Reference Topping, Douglas and Winkler2021); however, we considered participant preference when conducting virtual interviews. Finally, although we incorporated participants’ feedback through member checking, follow-up interviews with the participants were not completed. Follow-up interviews would have provided an opportunity for additional information to arise through theoretical sampling.
This study suggests the need for future research in three main areas. First, experimental research to determine the efficacy of peer-led, peer-support groups on stroke recovery and community integration. Future policy research is needed to explore potential funding for peer-led, peer-support groups for stroke survivors. Finally, further qualitative research is needed to explore the experiences of attending peer-led, peer-support groups for other neurological conditions.
Conclusion
This study explored the experiences of stroke survivors attending BLAST, a community-based peer-led, peer-support group. Findings indicated that attending BLAST provided the opportunity for stroke survivors to connect with people in a safe and playful environment that promoted exploring their abilities through group engagement and contributed to participants’ recognition of self-sufficiency and independence. This research extends previous knowledge of peer-support in stroke rehabilitation by describing the experiences from those attending a peer-led group. These included the potential complication of limited permanence in leadership roles, the importance of self-determination of group content, development of authentic friendships, and playfulness contributed to group participation.
Supplementary materials
For supplementary material for this article, please visit https://doi.org/10.1017/BrImp.2023.3
Acknowledgement
We would like to acknowledge and thank our participants and members of BLAST for contributing to this research through sharing their time and experiences with us.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of interest
DC (third author) is a member of the peer-led peer-support group studied in this research.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.




