Introduction
Conducting and advancing biomedical research has long been and remains an essential part of the mission of academic health centers (AHCs). Recent and ongoing initiatives focused on accelerating clinical, translational, and foundational biomedical research have led AHCs to invest in infrastructure and capabilities that enable and support research activities which are increasingly information and data management-intensive [Reference Stephens1–Reference Smoyer, Embi and Moffatt-Bruce3]. Research informatics and information technology (research IT) encompasses technological, human and organizational resources, systems and methods that manage and analyze data, information and knowledge to improve biomedical and health research [Reference Bernstam4]. The success and growth of institutions’ research enterprise relies upon advanced research IT solutions and capabilities, with investments in such infrastructure steadily rising [Reference Embi and Payne5, Reference Murphy6]. Indeed, research IT services are now at the heart of AHC research capabilities, and are integral to supporting broad and expanding research initiatives in population health, genomics, imaging, personalized medicine, as well as increasingly integrated into comprehensive data security and data sharing strategies. These investments in technology and expertise remain unevenly aligned with clinical mission investments. To be competitive and successful in the current research environment, AHCs require thoughtful research IT investment strategies with measurable outcomes that can align with institutional clinical and operational goals. Increasingly, AHC institutional leaders are feeling pressured to strategically increase investment in research IT due to a number of issues, including, but not limited to:
Institutional competitiveness for national initiatives such as precision health, patient-centered outcomes research that require significant, sustainable investments in research IT skills and resources [7–10].
Health IT systems have a growing role in not only enabling care and operations, but also enabling research and learning health systems, and this can raise new risk and compliance considerations related to security and data sharing strategies.
Programs driving clinical and translational science require more efficient and effective models of access to data and IT systems.
Research funders increasingly expect institutional support for research IT infrastructure and services as prerequisites to funding.
As the demand for such infrastructure and services increases, challenges in how to maintain effective oversight and support for research IT expand at a similar pace, with less clear measures of success. The distributed and variable nature of research funding and productivity often requires investment and deployment without the benefit of predictable funding streams that are core to the strategic development of the clinical and educational missions of AHCs. Without a similar predictable funding stream, many organizations find themselves experimenting with different strategies for implementing research IT services, which makes recruiting and retaining the skilled research IT professionals (e.g., data scientists, research informaticians, and support staff) challenging, given the limited workforce and the growing demand [Reference Bowley11]. Other challenges relate to emerging but not-yet-widespread models for research IT governance at AHCs, ongoing requirements related to leveraging health IT systems and data for secondary research purposes, and mechanisms for incentivizing participation in evidence-generating activities for personnel and organizations not part of the traditional research enterprise [Reference Embi12–Reference Weiner and Embi16]. As institutions address requirements for increasing their research IT investments, there is a need to better characterize their shared value and contributions to the health IT stakeholders. Institutions need guidance on how best to leverage these investments within institutional priorities and strategies, promote their strengths in the context of the national landscape of research IT maturity, and strategically manage external forces such as regulatory requirements, data sharing requirements, and emerging initiatives of sponsors.
Approach
Recent studies show that research IT capabilities and resources are inconsistently implemented across AHCs. This often relates to the differences in overall organization of AHCs [Reference Obeid17–Reference Payne19], such as the difference between a single organization governing all three missions versus one where governance is separated. It can also be seen in the inconsistent presence of a formal aligned department of biomedical informatics or the chief research information officer role [Reference Sanchez-Pinto20].
Maturity models [Reference Nolan21] have been shown to be effective tools in guiding organizational development for prioritization and process improvement in a wide range of areas of information technology [Reference Mutafelija and Stromberg22]. Maturity models assume that organizations, processes, and services develop through a series of stages of increasing quality and predictability [Reference Carvalho, Rocha and Abreu23, Reference Crosby24]. Each stage is modeled to be more efficient and effective than the previous stage. A key tenet of maturity models is that an organization needs to pass through each stage to reach a higher next stage. The path provided by these incrementally improving stages creates achievable steps for improvement as the organization progresses from one stage to the next working towards an ideal future state for the organization, which may or may not be the highest level of maturity due to considerations of costs, culture, and the impact on other missions.
Maturity models are an adaptable framework and may be applied to a single team, across the entire organization or across multiple organizations. They may be used to assess an organization’s capacity to deliver a service—providing insight into organizational culture, policy, and structure—or to measure the degree to which an institution has deployed technologies relative to delivering a service. These two characteristics of maturity models—the ability to enable incremental improvements towards an ideal state and the adaptability of the frameworks—make them a promising tool for helping grapple with the research IT complexities and inconsistent implementations seen in academic medicine.
Maturity models have provided a framework for building indices to look at electronic health record (EHR) deployment [25]. The Health Information Management Systems Society tools have been effective in guiding the implementation of expensive and complex EHRs by establishing a standard for assessing deployment of the EHRs—by measuring levels of service implementation. Maturity has also been applied to various areas of IT service development in higher education [Reference Grajek26]. Educause has developed both a deployment index for various areas of IT but has also created indices that look at organizational capacity for delivering services. These two applications—EHRs and higher Ed IT—inspire the idea of applying maturity to research IT in academic medicine.
Establishing Institutional Metrics and Standards for Research IT
We propose the creation and application of maturity models to guide institutional investment in research IT. There appears to be ample information in the AHC IT and informatics community to build indices that would allow organizations to do their own self-assessments, while also working towards establishing standards from interinstitutional data.
The Need for Two Types of Indices
We suggest a need for two types of tools, a maturity index and a deployment index [Reference Grajek26]. A maturity index measures organizational capacity to deliver a service, considering multiple factors including culture, policy, and organization. A deployment index measures the degree to which an institution has implemented a technology related to delivering a service.
Maturity indices address broader often nontechnical organizational issues and assessments can be completed by multiple offices (e.g., finance, scientific affairs, IT) in an organization to determine variance of perception within an organization and to build consensus on what an organization’s “ideal state” for research IT is. Maturity indices also serve as effective comparators with peer institutions.
Deployment indices allow the assessment of a given technology (e.g., research storage, clinical trials management system) against a classic maturity scale (Fig. 1). In an initial version of a deployment index, people doing the assessment could simply rate their deployment against a maturity scale. In a future version of the index assessment, there could be questions developed to determine quality, comprehensiveness, and complexity levels of a service. As with the maturity index, deployment index results could be effective tools for both internal and external planning. Deployment indices require a higher level of technical familiarity and understanding than maturity indices complete effectively.

Fig. 1 Stages (levels) of maturity.
Development and Initial Experiences
The authors have been involved in developing and testing maturity models for research IT in a number of venues. Embi has led discussions of maturity models at the Clinical Research Forum IT Roundtable where he presented a basic framework for a research IT maturity model. Embi’s framework has been built on by the other authors. One (Anderson) used a variant of this model to engage IT and medical center leadership in a planning exercise about research IT at his institution, building consensus on what research capabilities exist and establishing a common framework for planning. In this work, Anderson tested a maturity index at the University of California Davis to assess the capabilities for development of strategic research IT. To identify both infrastructure capabilities as well as current leverage of these resources for scientific applications, two assessments independently rated research IT and translational informatics capabilities from 22 stakeholders including chief information officer (CIO), associate dean and director-level roles. The study initially sought to test both maturity and deployment indices, but found that the challenges in developing common frameworks across such a broad campus required focusing on the maturity index as an initial framework to socialize the class of resources and stakeholders. UC Davis is intending to extend this work to a regular assessment.
Barnett and Knosp engaged the Association of American Medical Colleges Group on Information Resources to build two indices—a maturity index and a deployment index (online Supplementary Appendix 1 and 2) using methodologies developed by Educause researchers [Reference Grajek26]. They held focus groups and engaged subject matter experts to build a maturity index and a deployment index for research IT at AHCs. A pilot study was performed with members of the Group on Information Resources. The maturity index was used to stimulate a discussion at the 2017 Association of American Medical Colleges Group on Business Affairs Principal Business Officers that includes responses from AHC financial officers, senior research officers and CIOs. Both indices were presented and reviewed at the 2017 Clinical Research Forum IT Roundtable in Chicago.
The maturity index developed was an assessment of organizational characteristics using a Likert scale in seven categories including policies, governance, priority, leadership, supportive culture, integration with other missions and dedication infrastructure (Fig. 2). Fig. 2 shows the category and overall index scores across nine institutions and Fig. 3 shows the counts for Likert responses for one category—leadership. Looking at the data in these two different ways—single scores or raw responses provides insights at different levels of details into how research IT is viewed at these different organizations. The deployment index was a list of technologies with users selecting the maturity level the technology has been deployed at their institutions (Fig. 4). Looking at this data provides a quick assessment of institutional areas of strength or in need of development and could inform communities about topics of interest (e.g., common areas that need development).
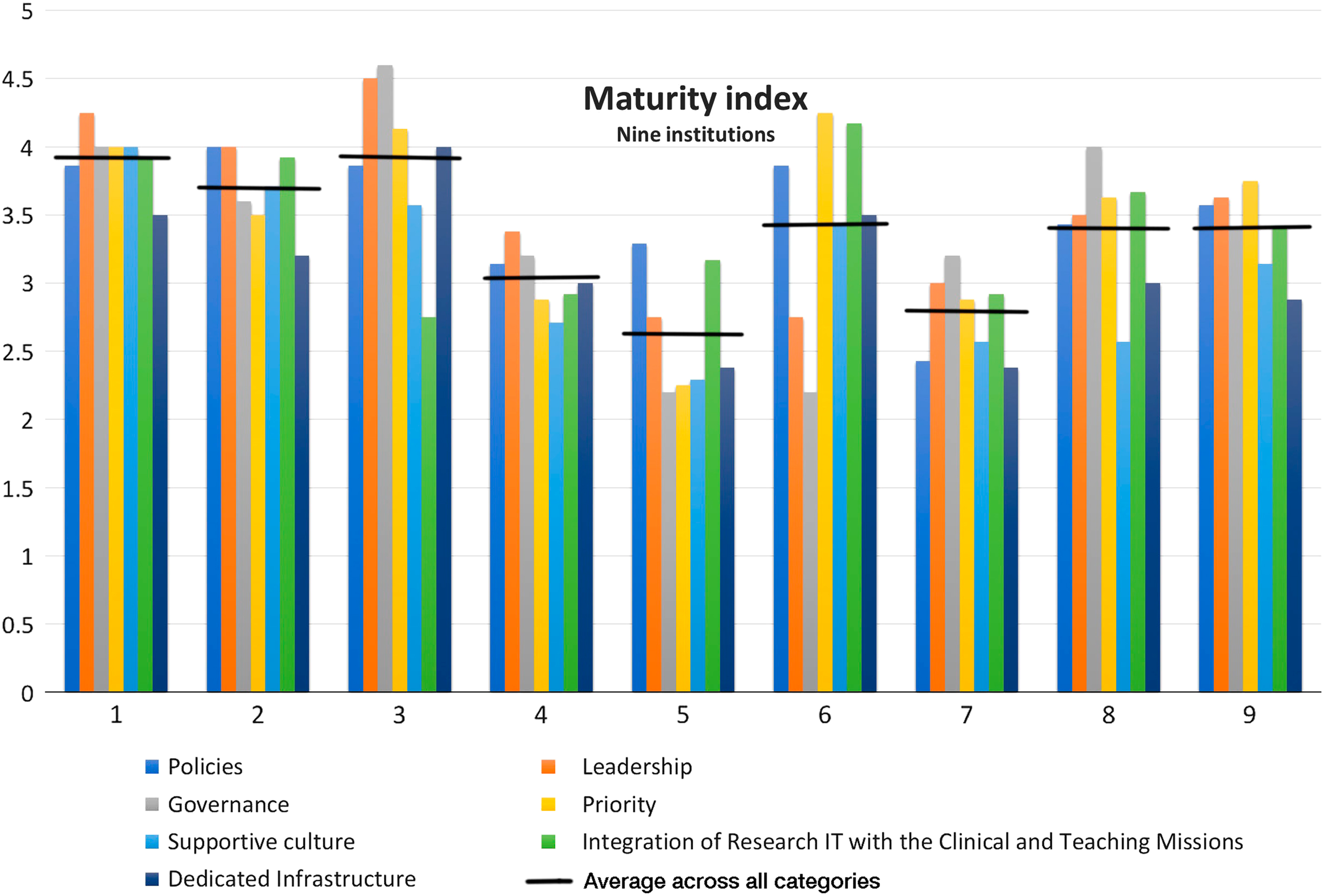
Fig. 2 Example of maturity index results for seven categories of maturity. Horizontal line indicates average across all categories. IT, information technology.

Fig. 3 Example of maturity index results for leadership category showing counts of Likert response for each question in the category. CIO, chief information officer; CRIO, chief research information officer; IT, information technology.

Fig. 4 Deployment index results. Each color is a different institution.
Value Proposition and Impact
Ultimately, once fully refined, validated and widely implemented, the value proposition of research IT maturity and deployment indices will be demonstrated by their use enabling AHCs to define strategic investment into and development of research IT services and capabilities. Indeed, when put into widespread use, such maturity and deployment models would serve the greater biomedical research community in a variety of ways. Some potential examples and impacts include:
Single enterprise identification of gaps and readiness in aligning clinical needs with research.
Enabling and optimizing research environments that cross organizational boundaries (e.g., computational biology and clinical imaging, patient-centered mobile health, and practice networks).
Providing comparable metrics for funding organizations to allow for review of institutional research IT readiness against aggregated community measures.
Developing guidelines for specific readiness and deployment indices as part of emerging communities of practice (e.g., multi-site clinical/research networks, precision health, or artificial intelligence in medicine initiatives).
Establishing effective representation of local expertise and infrastructure capabilities for strategic review, academic recruitment, or development of public-private partnerships.
Conclusions
Based on this pilot work, maturity models applied to research IT have shown the potential to inform a range of leadership stakeholders within institutions in a number of ways, including creating a guide for implementation and evaluation, providing a platform and context for internal discussion and planning, and defining organizational best practices for research IT support within academic medicine.
Next steps include establishing common open source indices for institutions to use across the value categories described above and to create objective maturity and deployment indices for specific services aligned with strategic needs.
Across these activities, it will be critical to continuously improve indices through building on the feedback from institutions and groups that use them and through establishing means to share and validate data and outcomes. As we move beyond pilot initiatives to broader data collection and use, we hope to be able to correlate output of these indices with other markers of maturity such as research productivity and emerging metrics for research IT.
Funding/Support
This project was supported by the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Awards including grant numbers UL1TR001860, U54TR001356, and UL1TR001108.
Disclosures
The authors have no conflicts of interest to declare.
Acknowledgments
The authors would like to thank colleagues in the Association for American Medical Colleges and the Clinical Research Forum IT Roundtable for their feedback and assistance with initial efforts to develop maturity models.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/cts.2018.339






