CVD are the leading cause of all deaths worldwide(Reference Bennett, Stevens and Mathers1). It is estimated that approximately 80 % of CVD deaths occur in low- and middle-income countries, and nearly half of these are premature deaths(Reference Ezzati, Pearson-Stuttard and Bennett2–Reference Yusuf, Rangarajan and Teo4). Importantly, blood lipid management has become a central target to reduce the premature death and disease burden caused by CVD(Reference Climie, van Sloten and Périer5–Reference Michos, McEvoy and Blumenthal8). Previous studies have shown that high levels of total cholesterol (TC), LDL-cholesterol, TAG and TC/HDL-cholesterol and low levels of HDL-cholesterol are all associated with an increased incidence of CVD(Reference Michos, McEvoy and Blumenthal8–Reference Domanski, Tian and Wu12). Thus, the guidelines for preventing primary CVD published by the American College of Cardiology-American Heart Association in 2019 promoted risk assessment and lipid management recommendations(Reference Michos, McEvoy and Blumenthal8). However, in the past few decades, although blood lipid levels have improved in developed countries (DC), such as North America and Europe, they have worsened in less-developed regions, such as East and Southeast Asia(Reference Farzadfar, Finucane and Danaei13,Reference Ezzati, Obermeyer and Tzoulaki14) .
Lipid screening, drug therapy and lifestyle interventions such as diet are all important measures of blood lipid management and prevention. However, the accessibility and affordability of lipid screening and drug treatment are much lower in less-developed regions, especially in populations of low socio-economic status and racial/ethnic minorities, than in DC(Reference Farzadfar, Finucane and Danaei13,Reference Widmer, Flammer and Lerman15) . Therefore, dietary modifications are critical strategies for lipid management and prevention of CVD in those regions(Reference Michos, McEvoy and Blumenthal8,Reference Prabhakaran, Anand and Watkins16–Reference Weber, Knebel and Strassburger18) . Many meta-analyses, cohort studies and randomised controlled trials have explored the associations of healthy dietary patterns, such as well-known Dietary Approaches to Stop Hypertension (DASH) and Mediterranean diet patterns, with blood lipid levels(Reference Chiu, Bergeron and Williams19–Reference Kastorini, Milionis and Esposito24). However, these healthy dietary patterns or dietary guidelines are proposed and updated mainly from developed settings such as Europe and North America. Less-developed ethnic minority regions (LEMR) are substantially different in terms of dietary habits and culinary cultures. Few studies have comprehensively examined the effectiveness of healthy dietary patterns on blood lipid management from LEMR(Reference Chiu, Bergeron and Williams19,Reference Anand, Hawkes and de Souza22) .
The China Multi-Ethnic Cohort (CMEC) study is a large-scale epidemiological study covering nearly 100 000 participants who are substantially different from DC with respect to geographical environment, ethnicity, dietary habits and levels of socio-economic status(Reference Zhao, Hong and Yin25). In this cross-sectional study based on the baseline data of the CMEC study, we aimed to explore the association of DASH and Mediterranean dietary patterns as well as their components with lipid profiles (i.e. TC, LDL-cholesterol, HDL-cholesterol, TAG and TC/HDL-cholesterol).
Methods
Study population
Detailed information about the CMEC study has been reported previously(Reference Zhao, Hong and Yin25). Briefly, the CMEC study recruited 99 556 participants from six ethnic minority groups as well as the majority Han group in less-developed Southwest China. The baseline survey took place between May 2018 and September 2019. All participants first gave informed consent and then underwent a series of assessments that consisted of face-to-face interviews based on electronic questionnaires on tablets, anthropometric measurements, comprehensive medical examinations, and blood and urine tests. The CMEC study was approved by the Sichuan University Medical Ethical Review Board and local ethics committee at each participating site.
For this analysis, we focused on adults aged 30–79 years with complete and plausible diet- and outcome-related data (online Appendix Fig. S1). To minimise reverse causality, we also excluded 6716 participants who self-reported physician-diagnosed hyperlipidaemia. Finally, 83 081 participants were included in the current analysis.
Assessment of the Dietary Approaches to Stop Hypertension and Mediterranean diets
At the baseline survey, the quantitative FFQ was used to assess the intake of main food groups, which covered the most commonly consumed food groups in Southwest China. We collected information on the quantity (average grams per time) and frequency (times per day, week, month or year) of each food group over the last year. Moreover, information on the frequency, quantity and consumption types was recorded for the alcohol, tea and beverages at the individual level and for cooking oil and salt at the family level. Total energy intake was calculated according to the China food exchange lists and the 2018 China food composition tables(26,27) . To assess the FFQ’s reproducibility and validity, FFQ reinterviewing (n 7516) and 3-d non-consecutive 24-h dietary recall (n 1163) were conducted 1 year after the baseline survey from August 2020 to November 2020. In terms of reproducibility, the Spearman rank correlation coefficients for food groups ranged from 0·15 to 0·61. In terms of validity, the deattenuated Spearman rank correlation coefficients for food groups ranged from 0·10 to 0·65.
We calculated the modified DASH score(Reference Fung, Chiuve and McCullough28) by replacing non-fat and low-fat dairy products with full-fat dairy products(Reference Chiu, Bergeron and Williams19), considering the extremely low intake of non-fat and low-fat dairy in our study population. Moreover, we excluded sweetened beverages in our DASH assessment, considering the low regular intake of sweetened beverages in our study population. Finally, we divided the food components into quintiles according to the participants’ intake and then assigned positive scores (1 points−5 points) to healthy components or reverse scores to red and processed meats and Na (online Appendix Table S1). We then summed seven component scores to obtain a total DASH score ranging from 7 to 35. Similarly, we used the alternative Mediterranean diet (AMED) score, which is modified and adapted to the Mediterranean diet scale(Reference Trichopoulou, Kouris-Blazos and Wahlqvist29–Reference Fung, Rexrode and Mantzoros32). We further excluded nuts in the AMED assessment due to no available information. The scoring criteria for the AMED score in the CMEC study could be seen in online Appendix Table S2. Finally, we summed eight component scores to obtain a total AMED score ranging from 8 to 40.
Assessment of blood lipids
In our study, blood lipid profiles referred to TC, HDL-cholesterol, LDL-cholesterol, TAG and TC/HDL-cholesterol. To assess blood lipids, all participants were required to fast for at least 8 h before drawing venous blood from the antecubital vein. Blood samples were transported through the cold chain to regional central laboratories. Within 24 h after collection, laboratory tests were carried out through a unified standard operating procedure and automated analytical instruments. Fasting blood samples were analysed for TC, LDL-cholesterol, HDL-cholesterol and TAG by an AU5800 automated chemistry analyser (Beckman Coulter Commercial Enterprise).
Statistical analysis
Baseline characteristics were described as the means and standard deviations or percentages according to the quintile of dietary pattern scores, with adjustment for age and sex as appropriate by direct standardisation (using the entire analytic sample as the standard population). Besides, we described baseline characteristics in the CMEC study according to the regions, considering that our previous study(Reference Xiong, Zixiu and Xiaoyan33) has found that both the dietary patterns and baseline characteristics of the ethnic groups were highly related to the geographic regions, which can be clustered into three regions, that is, Sichuan Basin, Yunnan-Kweichow Plateau and Qinghai-Tibet Plateau.
We used multivariable linear regression models to assess the association of the DASH and AMED scores with TC, HDL-cholesterol, LDL-cholesterol, TAG and TC/HDL-cholesterol (as a continuous dependent variable) after adjusting for potential confounders, with the lowest fifth of dietary pattern score as the reference group. To select potential confounders properly, we constructed directed acyclic graphs(Reference Ferguson, McCann and Katikireddi34). According to the directed acyclic graphs and back door criteria(Reference Pearl, Glymour and Jewell35), the final models (online Appendix Text S1 and Appendix Fig. S2) adjusted for sex, age, urbanicity, ethnicity, marital status, education attainment, household income, profession, regular smoking, physical activity, total energy intake, BMI, regular intake of sweetened beverages, regular intake of dietary supplements, regular intake of spicy food, regular intake of pepper food, insomnia symptoms, depressive symptoms, anxiety symptoms, menopause status for women and family history. To test the linear trend across quintiles, we replaced each quintile of dietary scores with its median value and modelled it as a continuous variable. In addition, to facilitate the interpretations of the above results, we evaluated the impact of each dietary component of two dietary patterns on the lipid profile by eliminating one component at a time from the overall score separately (online Appendix Text S2)(Reference Trichopoulou, Bamia and Trichopoulos36). Since we used the electronic questionnaire with built-in quality control, the missing rate of this study was very low. For the missing values of the food group, we used the chain equation method for multiple imputation (with five imputations).
To better inform the target population for subsequent dietary interventions, we conducted subgroup analysis in the non- and high-risk groups (participants with hypertension or diabetes), respectively. To examine effect modification of regions, we conducted stratification analysis among different regions. We also conducted several sensitivity analyses to check the robustness of our findings. First, we further excluded self-reported diagnosis of CVD by a physician (i.e. CHD, stroke) before the main analyses, considering that these diseases may be related to blood lipid levels. Second, we used more stringent inclusion and exclusion criteria based on the first sensitivity analysis by further excluding the self-reported physician-diagnosed cardiometabolic disease (i.e. hypertension, diabetes, CHD and stroke), hepatic and gastrointestinal diseases (i.e. chronic hepatitis, hepatic cirrhosis, gastrointestinal ulcers, gastroenteritis, cholecystitis and gallstones) before the main analyses, given that these diseases may affect dietary habits and blood lipid levels. Third, we ran a complete case analysis instead of the multiple imputation approach. Fourth, we fitted the multivariable model without exclusion of self-reported hyperlipidaemia to examine the magnitude of potential reverse causality. Fifth, we fitted regression models using median instead of expected mean to examine the influence of outcome distributions on the results. Sixth, we did not adjust for regular intake of sweetened beverages to examine its influence on the associations between DASH score with lipids. All analyses were performed with the R Project for Statistical Computing version 4·0·2(Reference Team37).
Result
Among the 83 081 participants included in this study, the mean age was 51·3 (sd 11·4) years; 61·1 % of participants were women; 34·4 % were urban residences; 53·5 % were ethnic minorities from plateau areas. Age- and sex-standardised baseline characteristics in the CMEC study according to quintiles of DASH and Mediterranean scores are shown in Table 1. Participants in the highest fifth of both the DASH score and Mediterranean score were more likely to be females living in an urban residence from Sichuan Basin, have a high education level and household income, and have a family history of cardiometabolic disease. However, they were less likely to report mental disorders. Besides, baseline characteristics in the CMEC study according to the regions are shown in online Appendix Table S3. Compared with the people in other two regions, the Han majority in Sichuan Basin were more likely to be urban residents, have higher education, socio-economic status levels and dietary scores, and more likely to report a family history of CVD.
Table 1. Age- and sex-standardised baseline characteristics in the CMEC study according to the quintiles of DASH and Mediterranean scores*
(Numbers and percentages; mean values and standard deviations)
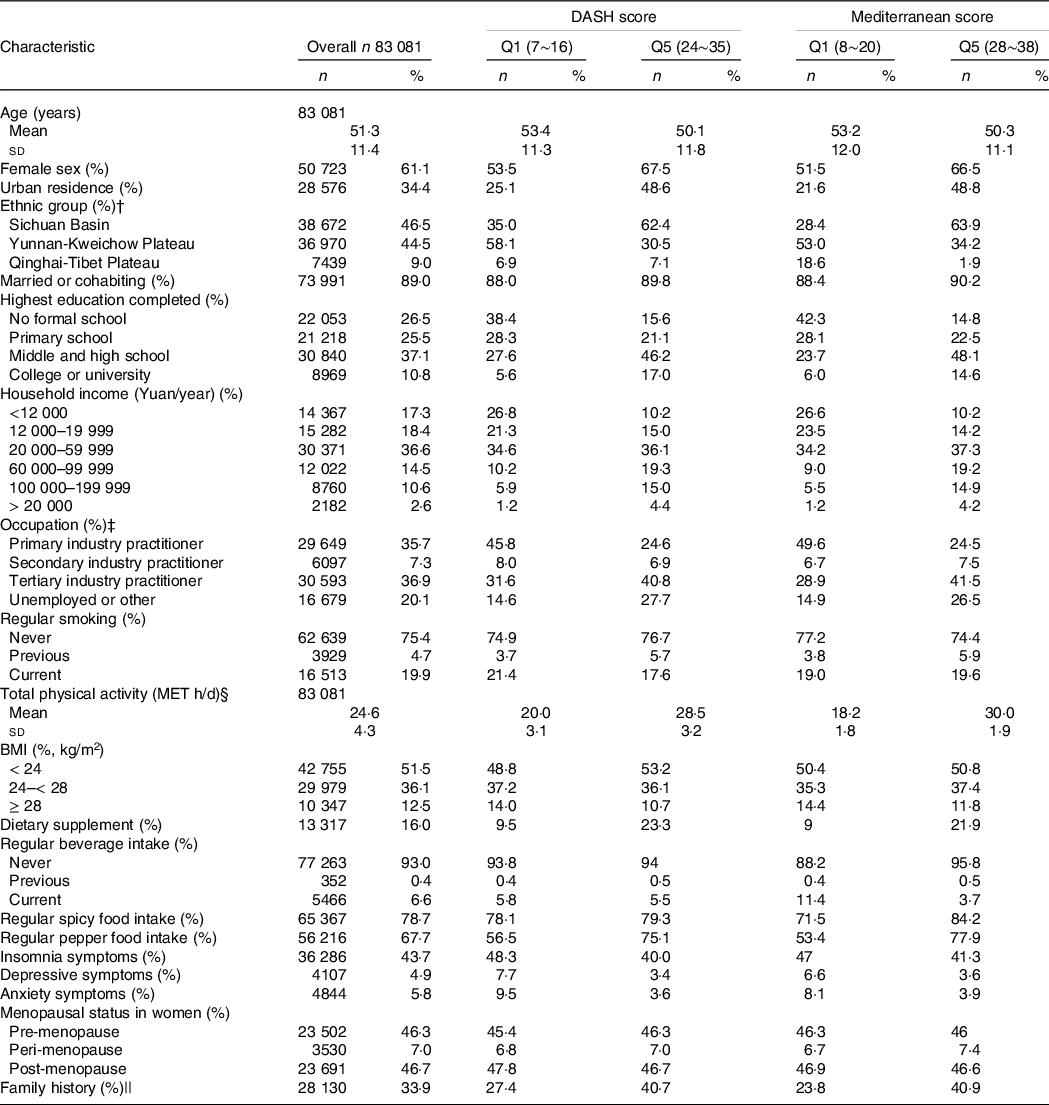
DASH, Dietary Approaches to Stop Hypertension; AMED, alternative Mediterranean diet; MET, metabolic equivalent; Q, quintile.
* Data are presented as the mean values and standard deviations or n (%).
† We aggregated various ethnic groups into three geographic regions due to their high similarity in dietary pattern and baseline characteristics.
‡ Primary industry practitioner is defined as farming, forestry, animal husbandry and fishery labourer. Secondary industry practitioner refers to workers in the processing and manufacturing industry. Tertiary industry practitioner refers to workers in industries other than primary and secondary industries.
§ Physical activity in metabolic equivalent task h/d.
|| Family history refers to the self-reported hypertension, diabetes or CVD from at least one first-degree relative (biological parents, sibling) in the baseline survey.
Associations between DASH and AMED scores and blood lipids are presented in Fig. 1. Generally, DASH scores had negative associations with TC, HDL-cholesterol and TAG, and the AMED score was negatively associated with TC and LDL-cholesterol and HDL-cholesterol. More specifically, comparing the highest quintiles with the lowest DASH scores, TC decreased 0·0708 (95 % CI −0·0923, −0·0493) mmol/l, HDL-cholesterol decreased 0·0380 (95 % CI −0·0462, −0·0299) mmol/l and TAG decreased 0·0668 (95 % CI −0·0994, −0·0341) mmol/l, with all P values for trends < 0·001. We found no significant association between the DASH score with LDL-cholesterol and TC/HDL-cholesterol. For the association between the AMED score and blood lipids, comparing the highest quintiles with the lowest AMED scores, TC decreased 0·0816 (95 % CI −0·1035, −0·0597) mmol/l, LDL-cholesterol decreased 0·0297 (95 % CI −0·0477, −0·0118) mmol/l and HDL-cholesterol decreased 0·0275 (95 % CI −0·0358, −0·0192) mmol/l, with all P values for trends < 0·001. We found no significant association between AMED with TAG and TC/HDL-cholesterol.
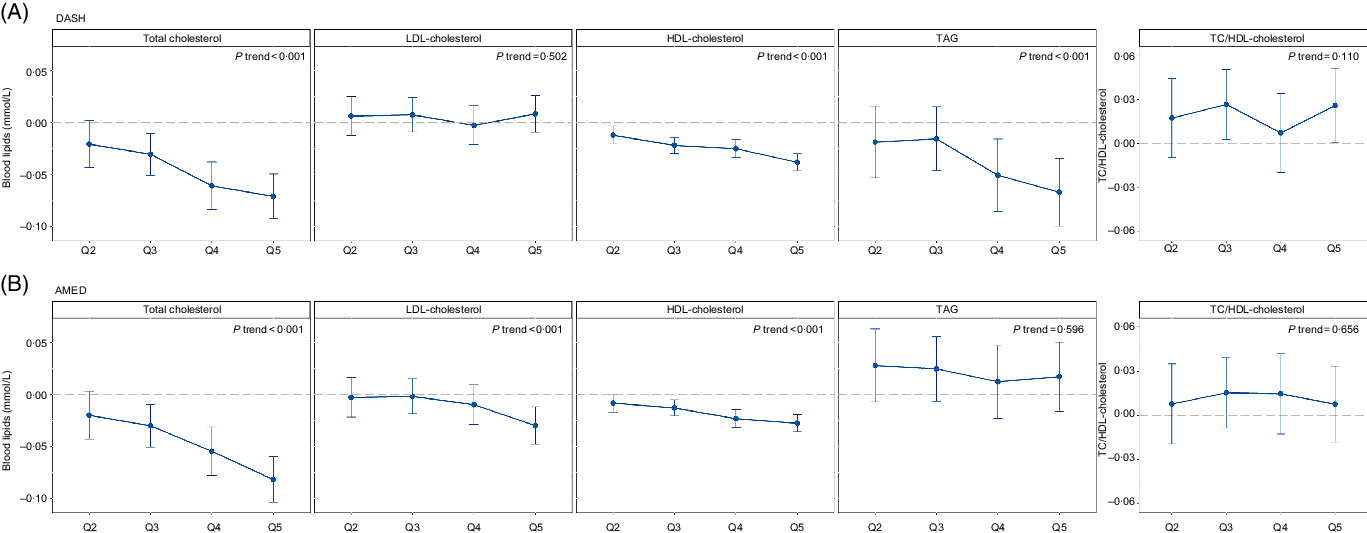
Fig. 1. Association of the DASH and AMED scores with blood lipids. Dots and bars represent regression coefficients and 95 % CI, respectively. DASH, Dietary Approaches to Stop Hypertension; AMED, alternative Mediterranean diet; Q, quintile.
The differences between the DASH and AMED scores regarding their associations with lipid profiles can be well explained through component analyses (Tables 2 and 3). The component of full-fat dairy products in the DASH (but not in the AMED) contributed the largest proportion to the negative relation with TAG (59·7 %) and showed a strong positive association with LDL-cholesterol. In contrast, the component of the monounsaturated/saturated fat ratio in the AMED (but not in the DASH) contributed a major proportion to the negative associations with HDL-cholesterol (34·2 %) and showed a strong positive association with TAG. For those common food components, higher whole grain intake in both the DASH and AMED contributed a considerable proportion to the negative association with TC, that is, 26·4 % for the DASH and 29·7 % for the AMED. In addition, lower red and processed meat intake in both the DASH and AMED showed a strong association with lower LDL-cholesterol; higher legumes intake in both the DASH and AMED showed a strong association with lower TC/HDL-cholesterol.
Table 2. Blood lipid associations with DASH scores and after alternate subtraction of each of its dietary components
(Coefficient values and 95 % confidence intervals)
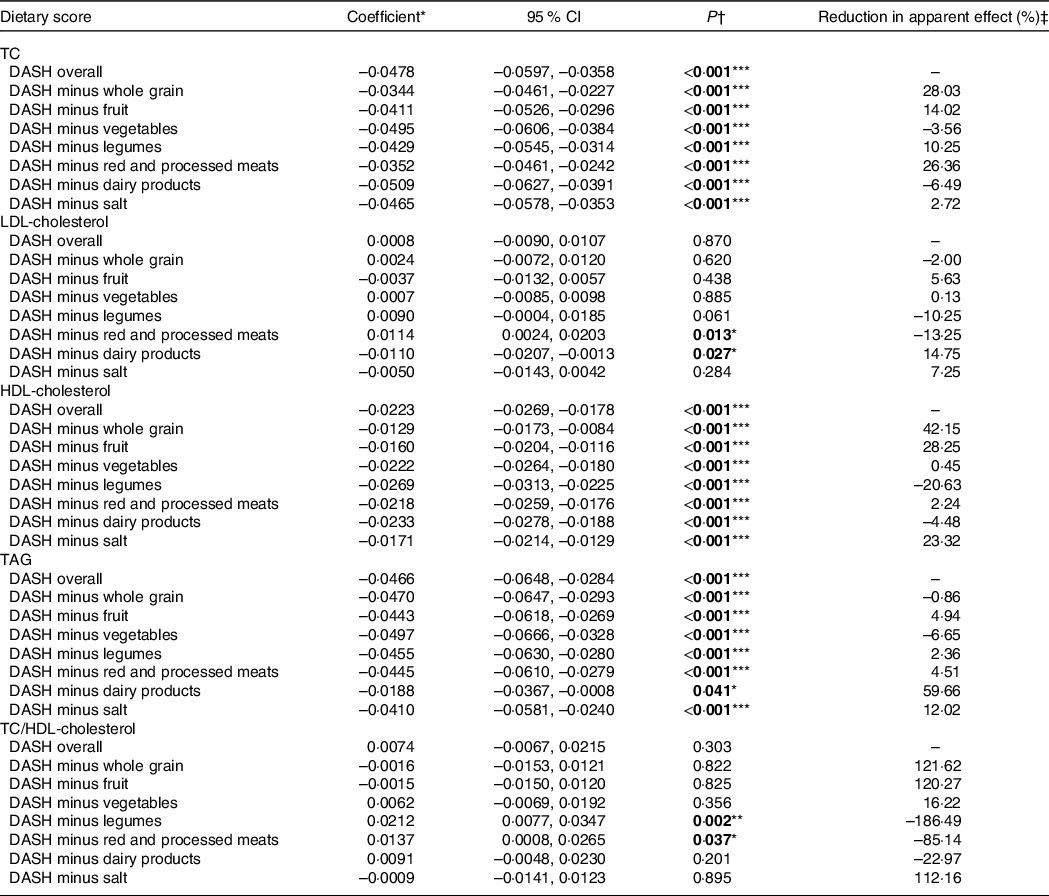
DASH, Dietary Approaches to Stop Hypertension; TC, total cholesterol.
* We assumed a linear relationship with lipid level change per 25 % score range increment.
† Boldface indicates statistical significance (*P < 0·05, **P < 0·01, ***P < 0·001).
‡ Reduction in apparent effect (%) = (Coefficient DASH overall – Coefficient DASH minus component)/Coefficient DASH overall × 100 %.
Table 3. Blood lipid associations with AMED scores and after alternate subtraction of each of its dietary components
(Coefficient values and 95 % confidence intervals)
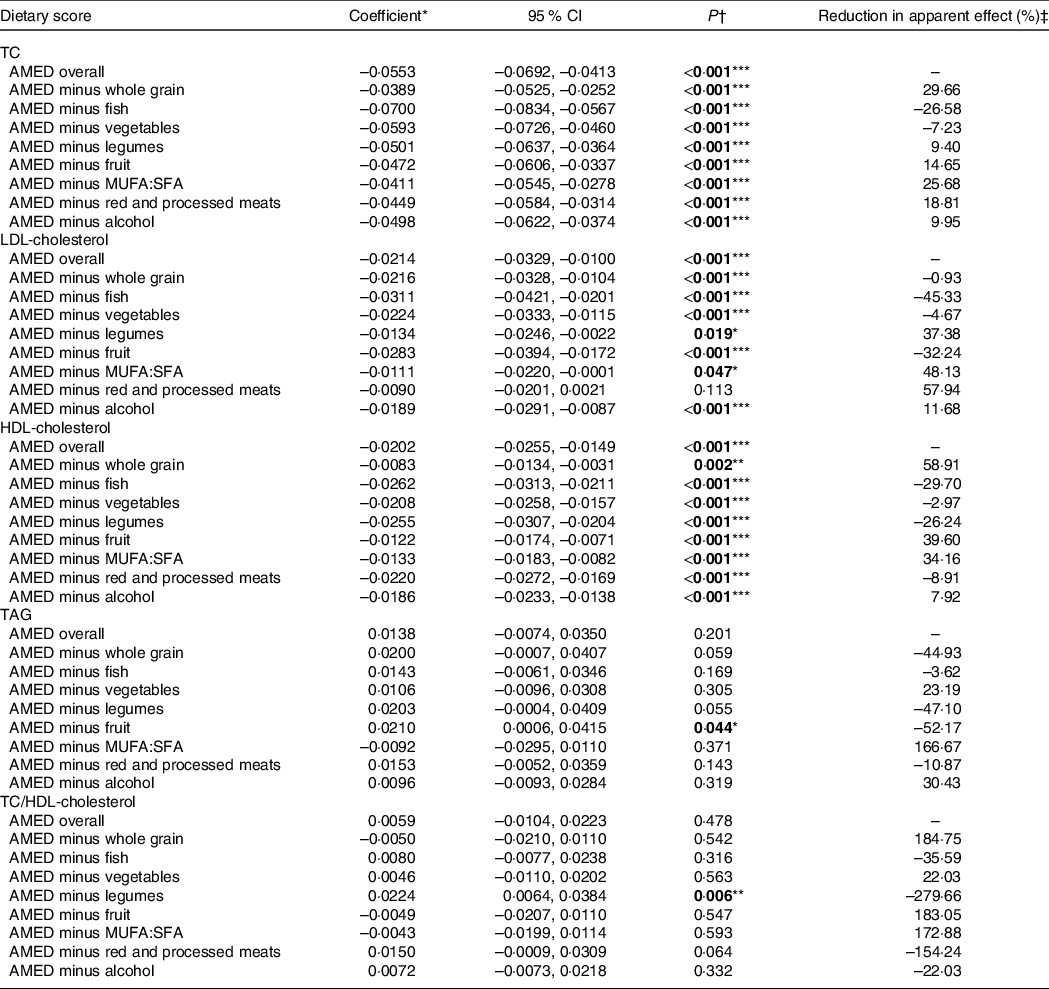
AMED, alternative Mediterranean diet; MUFA:SFA, monounsaturated/saturated fat ratio; TC, total cholesterol.
*We assumed a linear relationship with lipid level change per 25 % score range increment.
† Boldface indicates statistical significance (*P < 0·05, **P < 0·01, ***P < 0·001).
‡ Reduction in apparent effect (%) = (Coefficient AMED overall – Coefficient AMED minus component)/Coefficient AMED overall × 100 %.
Compared with the non-high-risk group, a stronger association between healthy dietary patterns (both DASH and AMED) and lower TC, LDL-cholesterol and TAG levels was found in the high-risk group for both the diabetes and hypertensive groups, although not all subgroups had enough outcomes to establish significant differences. See online Appendix Table S4 for more details. Both DASH and AMED scores showed stronger associations with blood lipids among the Han majority in Sichuan Basin compared with the ethnic minorities in other regions (online Appendix Fig. S3). Further sensitivity analyses did not change our results regarding the associations between the DASH and AMED with blood lipids substantially after we used two more stringent inclusion and exclusion criteria (online Appendix Fig. S4 and Appendix Fig. S5). Our results were robust to the sensitivity analyses of the complete case analysis and the analysis without excluding self-reported hyperlipidaemia (online Appendix Fig. S6 and Appendix Fig. S7). Moreover, our results were relatively robust when we fitted regression models using median instead of expected mean (online Appendix Fig. S8). Lastly, similar associations between DASH scores and blood lipids were found when performing analysis without adjusting for regular intake of sweetened beverages (online Appendix Fig. S9).
Discussion
This study investigated the association of the DASH and Mediterranean-style dietary patterns with blood lipids in a population of LEMR. Both the DASH and Mediterranean diets were negatively associated with blood lipids in LEMR. More specifically, DASH scores had negative associations with TC, HDL-cholesterol and TAG, while AMED scores were negatively associated with TC, LDL-cholesterol and HDL-cholesterol.
Compared with the results of previous studies mainly coming from DC, the DASH diet was associated with different lipid patterns in our study. Previous clinical trials, systematic reviews and meta-analyses have shown that the DASH is negatively related to TC and LDL-cholesterol but has no significant association with TAG and TC/HDL-cholesterol(Reference Obarzanek, Sacks and Vollmer20,Reference Anand, Hawkes and de Souza22,Reference Siervo, Lara and Chowdhury38,Reference Chiavaroli, Viguiliouk and Nishi39) . In contrast, DASH scores were found to be negatively associated with TC and TAG, but there was no significant association with LDL-cholesterol and TC/HDL-cholesterol in our study with the setting of LEMR. For HDL-cholesterol, the relationship between DASH and HDL-cholesterol is not consistent at present(Reference Chiu, Bergeron and Williams19,Reference Obarzanek, Sacks and Vollmer20,Reference Siervo, Lara and Chowdhury38) , and our research found that the DASH diet was negatively associated with HDL-cholesterol, which was consistent with some clinical trials(Reference Chiu, Bergeron and Williams19,Reference Obarzanek, Sacks and Vollmer20) . Similar to the results in the setting of DC, a negative association between DASH scores and TC was also found in our study, which was largely driven by the whole grain component (contributing a considerable proportion of 26·4 %). Of note, low whole grain consumption is one of the three leading dietary risk factors for death and disability adjusted life year worldwide, while refined grain intake is increasing in LEMR(Reference Hu, Pan and Malik40,Reference Afshin, Sur and Fay41) . Besides, consistent with the evidence from DC(Reference Obarzanek, Sacks and Vollmer20), there was no significant association between DASH scores and TC/HDL-cholesterol in our study, which was largely related to the negative association between DASH and HDL-cholesterol. Different from the results in DC, the DASH diet in our study showed no significant association with LDL-cholesterol but a strong negative association with TAG levels, which was largely due to the high intake of full-fat dairy products. In contrast to DC, almost all of the dairy product consumption in LEMR is full-fat dairy products(Reference Dehghan, Mente and Rangarajan42). For LDL-cholesterol, although the individual full-fat dairy product component in the DASH showed a strong positive association with LDL-cholesterol, the whole DASH dietary pattern did not show a detrimental association with LDL-cholesterol, which was similar to clinical trials(Reference Chiu, Bergeron and Williams19). For TAG, the strong negative association between the DASH and TAG seen in our study was mainly due to the high intake of full-fat dairy products, which contributed the largest proportion of their negative association (59·7 %). The beneficial effect of full-fat dairy product intake on TAG may be related to Ca, some specific amino acids from whey protein, SFA and other combined and synergic effects of various nutrients in full-fat dairy products(Reference Ricci-Cabello, Herrera and Artacho43–Reference Louie, Flood and Rangan48). Especially for SFA, previous studies have shown that the replacement of carbohydrates with an equivalent amount of SFA could lead to a significant reduction of TAG(Reference Mensink49). TAG is not only a biomarker for increased concentrations of remnant lipoprotein cholesterol concentrations(Reference Simha50,Reference Nordestgaard and Varbo51) but is also involved in the causal pathway of arteriosclerotic CVD by which it plays a pathogenic role in directly promoting atherogenesis(Reference Simha50,Reference Jacobson, Ito and Maki52,Reference Budoff53) . Moreover, compared with other lipid abnormalities, TAG management is more difficult for LEMR with low accessibility and affordability of drug treatment, given that some TAG-lowering agents additionally need to be added to conventional statin therapy(Reference Budoff53). Given this, TAG could be used as an important target of the DASH diet to manage lipids and prevent CVD in low- and middle-income country settings. In summary, compared with the results mainly from DC, although the DASH diet was associated with different lipid patterns in our study in LEMR, it may also be beneficial for lipid management.
Compared with previous studies mainly coming from DC, the Mediterranean diet was also associated with different lipid patterns in our study. Previous studies have shown that a Mediterranean diet is associated with lower TC, LDL-cholesterol, and TAG and higher HDL-cholesterol, which implies beneficial effects for lipid management(Reference Anand, Hawkes and de Souza22–Reference Kastorini, Milionis and Esposito24). In contrast, we found that the AMED scores were negatively associated with TC, LDL-cholesterol and HDL-cholesterol in the setting of LEMR. Similar to the results for DC, our study also found negative associations between the AMED score and TC and LDL-cholesterol levels, which was mainly due to the high intake of whole grains (contributing a considerable proportion of 29·7 % for TC) and low intake of red and processed meats (contributing the largest proportion of 57·9 % for LDL-cholesterol). However, the Mediterranean diet did not show a positive association with HDL-cholesterol and a negative association with TAG levels in our study, which was contrary to the findings of a meta-analysis of fifty studies and 534 906 individuals mainly from DC(Reference Kastorini, Milionis and Esposito24). The Mediterranean diet did not show a negative association with TC/HDL-cholesterol in our study, which was different with the findings of some research from DC(Reference Mertens, Mullie and Deforche54,Reference Yang, Farioli and Korre55) . The Mediterranean diet is largely dependent on the dietary habits of the population from developed northern Europe, one of whose major features is a high monounsaturated/saturated fat ratio (mainly due to the use of olive oil as the main fat in food preparation)(Reference Trichopoulou, Costacou and Bamia30,Reference Trichopoulou, Bamia and Trichopoulos36,Reference Park, Steck and Fung56) . However, the monounsaturated/saturated fat ratio component included in the AMED in our study contributed a major proportion to the negative associations with HDL-cholesterol (34·2 %) and showed a strong positive association with TAG, which did not show the expected beneficial effects(Reference Anand, Hawkes and de Souza22,Reference Mensink, Zock and Kester57,Reference Willett58) on lipid levels. This component may represent other types of oil in less-developed settings rather than the expected healthy olive oil(Reference Gardener, Wright and Gu59). A high monounsaturated/saturated fat ratio in our study only reflects the high intake of vegetable oil. In addition, the different culinary cultures (e.g. deep-fried cooking) in these areas may further undermine the beneficial effects of the monounsaturated/saturated fat ratio(Reference Yamashima, Ota and Mizukoshi60). Therefore, although the Mediterranean diet shows a favourable association with all four blood lipids in DC, our findings suggest that the AMED may not function adequately for lipid management in LEMR.
The limitations of the present study warrant mention. First, the FFQ used in our study included only thirteen commonly consumed food groups. Although those food groups can be used to calculate the DASH and Mediterranean scores, the coarse food groups may impair the accuracy of calculations of specific dietary components (such as the monounsaturated/saturated fat ratio in the AMED scores) and total energy intake. However, the differences in total energy intake between the calculation based on crude food groups in the FFQ and that based on specific food items in the 24-h dietary recall were small and roughly randomly distributed around zero. Given the most participants in the CMEC study are illiterate, speaking different local languages and consuming distinct foods which are not included in any existing food database, this food group-based food questionnaire may be the only option for large-scale survey that can ensure the efficiency of communication, the cooperation of participants and the comparability among various regions. Second, although we have carefully adjusted for potential confounders under the guidance of directed acyclic graphs, there may still be some residual confounding. Third, this study is a cross-sectional study. Although we excluded self-reported hyperlipidaemia, it still limited the reliability of causality.
Conclusion
Based on the baseline data of the CMEC study, both the DASH and AMED scores were associated with different lipid patterns in LEMR compared with previous evidence mainly coming from DC. DASH scores had strong negative associations with TC and TAG, which may be beneficial for lipid management. Full-fat dairy intake, which is encouraged in the modified DASH, may produce a favourable effect on lowering TAG. For the AMED, although higher AMED scores were associated with lower TC and LDL-cholesterol levels, they did not show a favourable association with HDL-cholesterol levels, TAG levels and TC/HDL-cholesterol, suggesting that the AMED may not function adequately for lipid management in LEMR.
Acknowledgements
The authors thank all the team members and participants involved in the China Multi-Ethnic Cohort (CMEC). The authors are grateful to Prof. Xiaosong Li at Sichuan University for his leadership and fundamental contribution to the establishment of the CMEC. Prof. Li was the former principal investigator of the CMEC study who passed away in 2019.
This work was funded by the National Key R&D Program of China (Grant No. 2017YFC0907303, 2017YFC0907300). XX was supported by the National Natural Science Foundation of China (Grant No. 81903415), the Key R&D Project of Sichuan Province Science and Technology Support Program (Grant No. 2020YFS0215) and CNS-ZD Tizhi and Health Fund (Grant No. CNS-ZD2020-149). JY was supported by the National Natural Science Foundation of China (Grant No. 81860597). XZ was supported by the National Natural Science Foundation of China (Grant No. 81973151).
N. Z., X. X., D, J. Y. and X. Z. contributed to the design of the present study. X. Z. was the principal investigator of the CMEC study. D. and J. Y. the coprincipal investigator of the CMEC study. N. Z. and X. X. wrote the analysis plan, and the first and final draft of the paper. D., J. Y. and X. Z. reviewed and commented on the data analysis, all drafts and the final paper. All other authors were involved in conduct of the study, analysis of data, interpretation of results and provided critical comments on all drafts of the report.
No potential conflict of interest was reported by the authors.
Supplementary material
For supplementary material referred to in this article, please visit https://doi.org/10.1017/S0007114521004013






